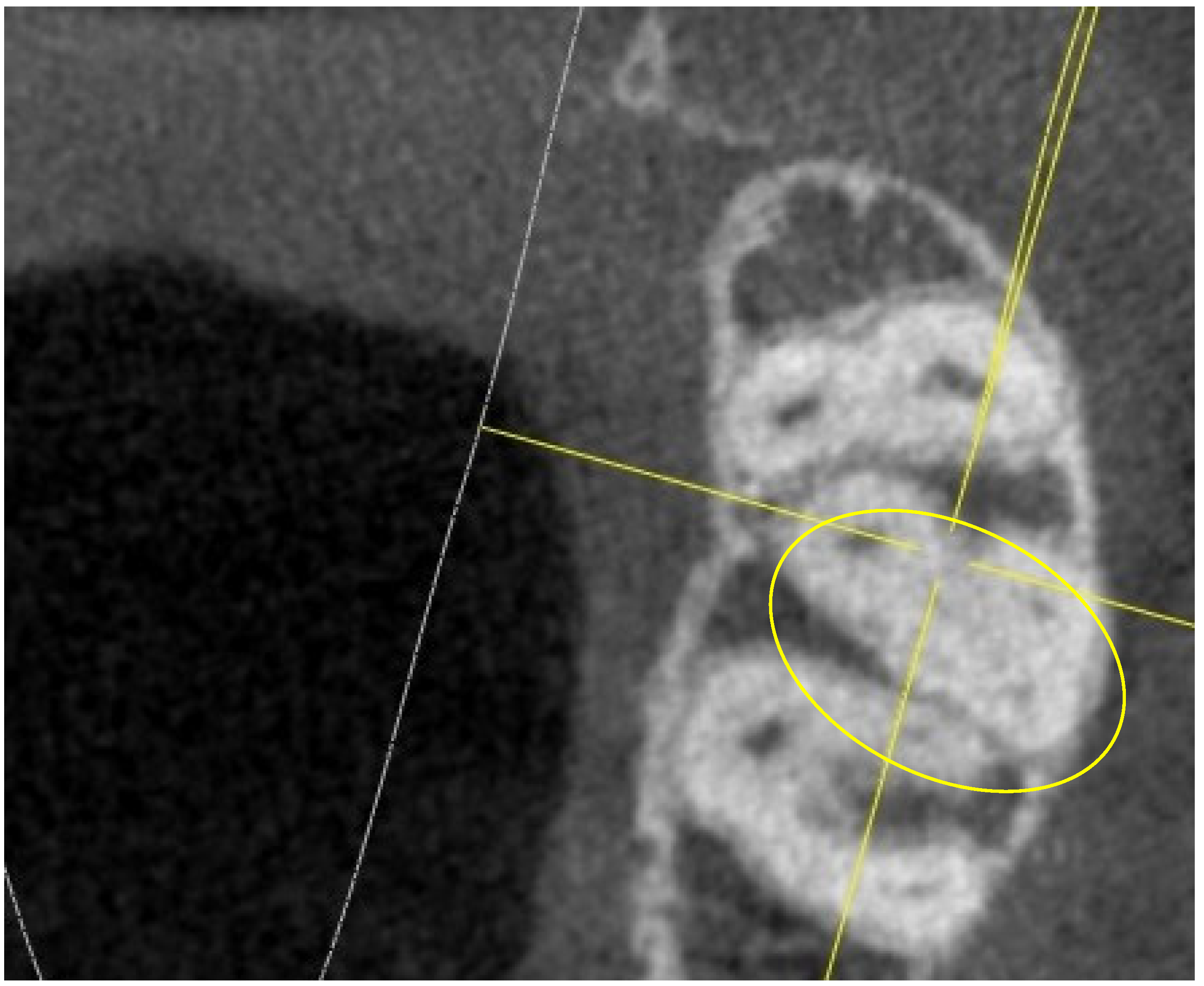
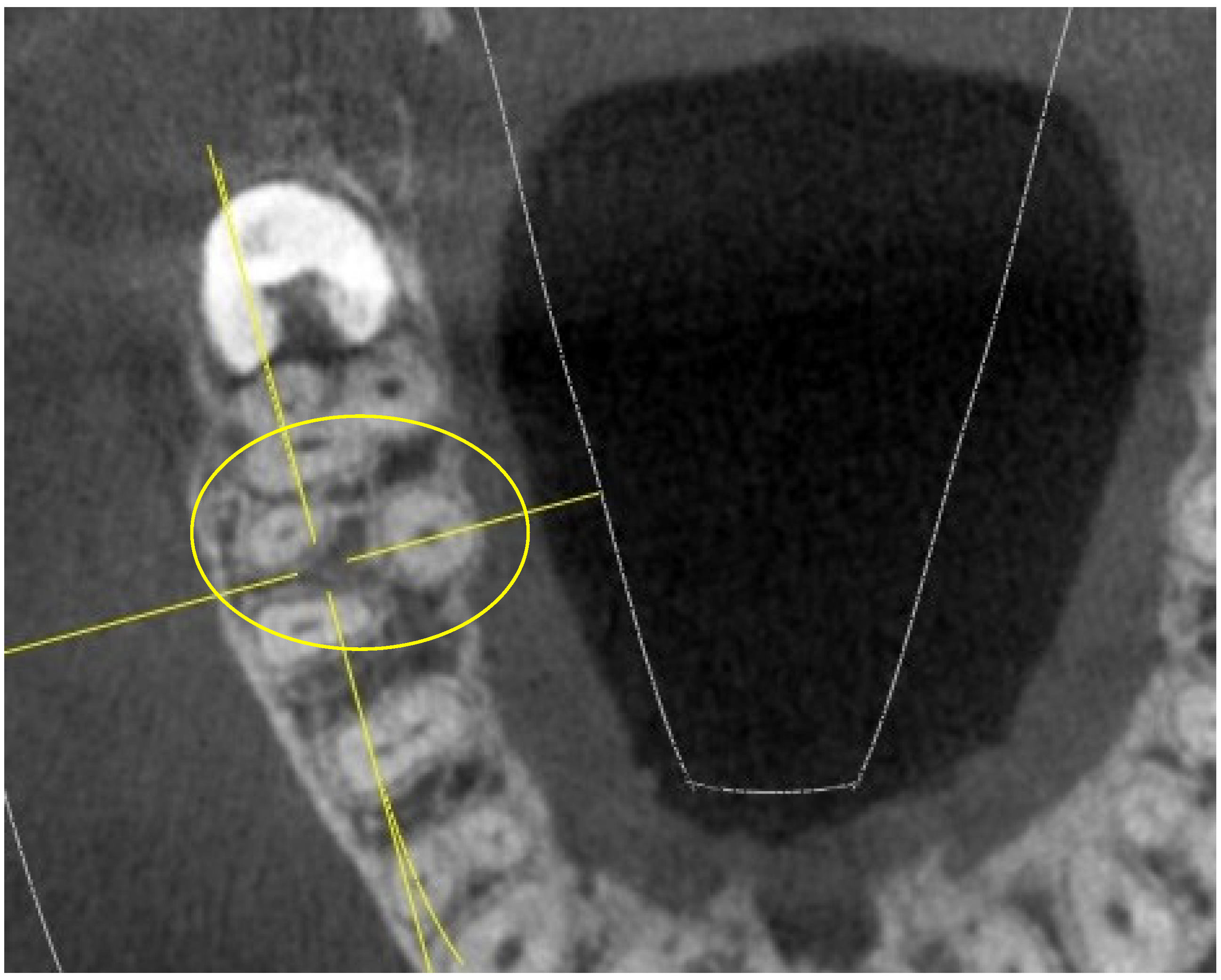
Upper First and Second Molar Pulp Chamber Endodontic Anatomy Evaluation According to a Recent Classification: A Cone Beam Computed Tomography Study
Abstract
:1. Introduction
2. Materials and Methods
- the presence of four maxillary molars (including jus first and second);
- no previous conservative or endodontic treatment;
- absence of coronal restorations;
- complete root formation;
- absence of root canal calcification—root canals should be visible from the pulp chamber to the apical part;
- absence of conditions that could limit the possibility of identifying the structures being studied, such as neoplasms, cysts, large periradicular lesions, artifacts, or internal or external root resorptions;
- no influence of the wisdom tooth on the shape of the roots and canals of the seventh due to the close position;
- older than 18;
- patients of Caucasian origin.
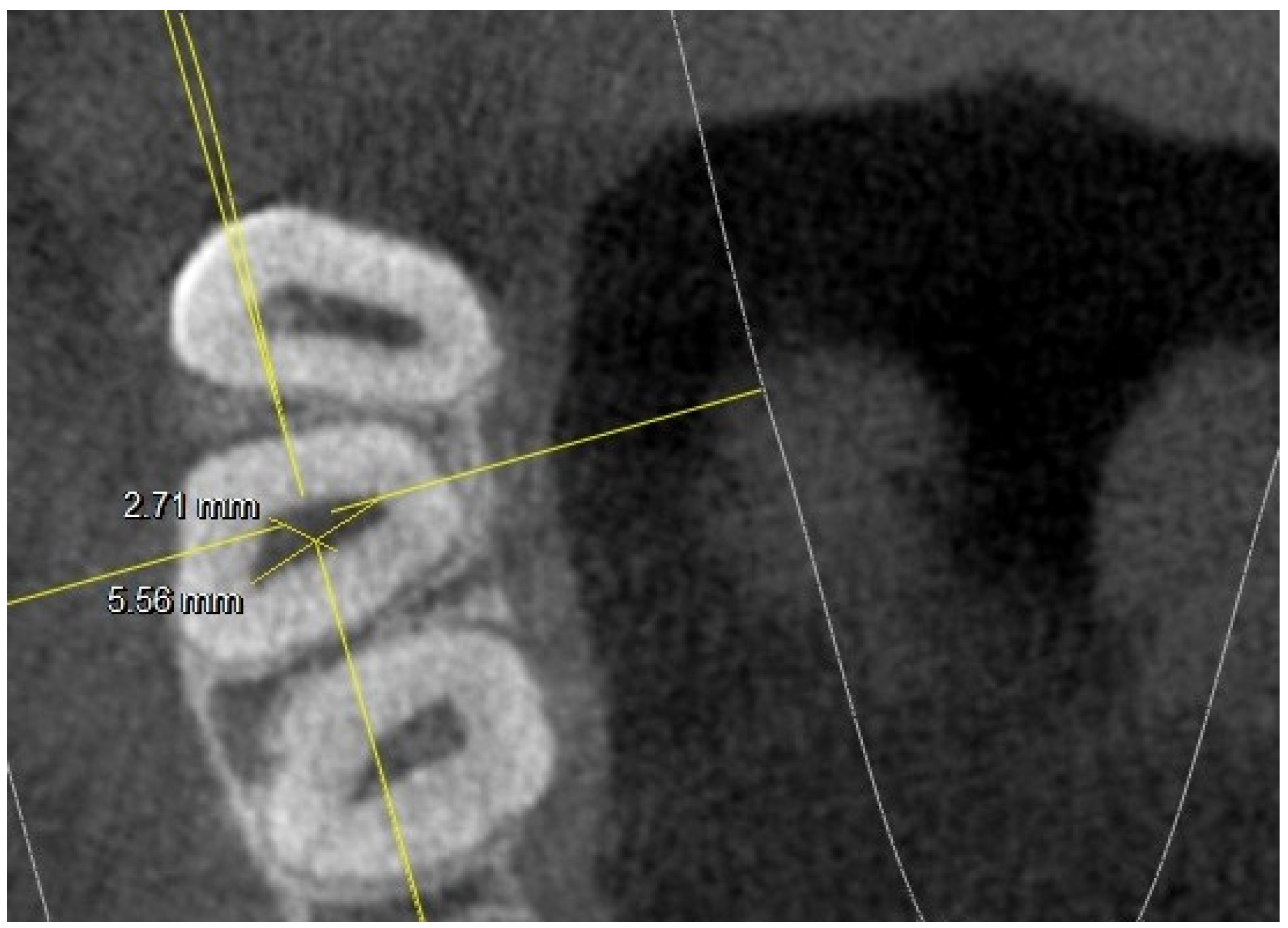
- long and short diameter of the pulp chamber floor;
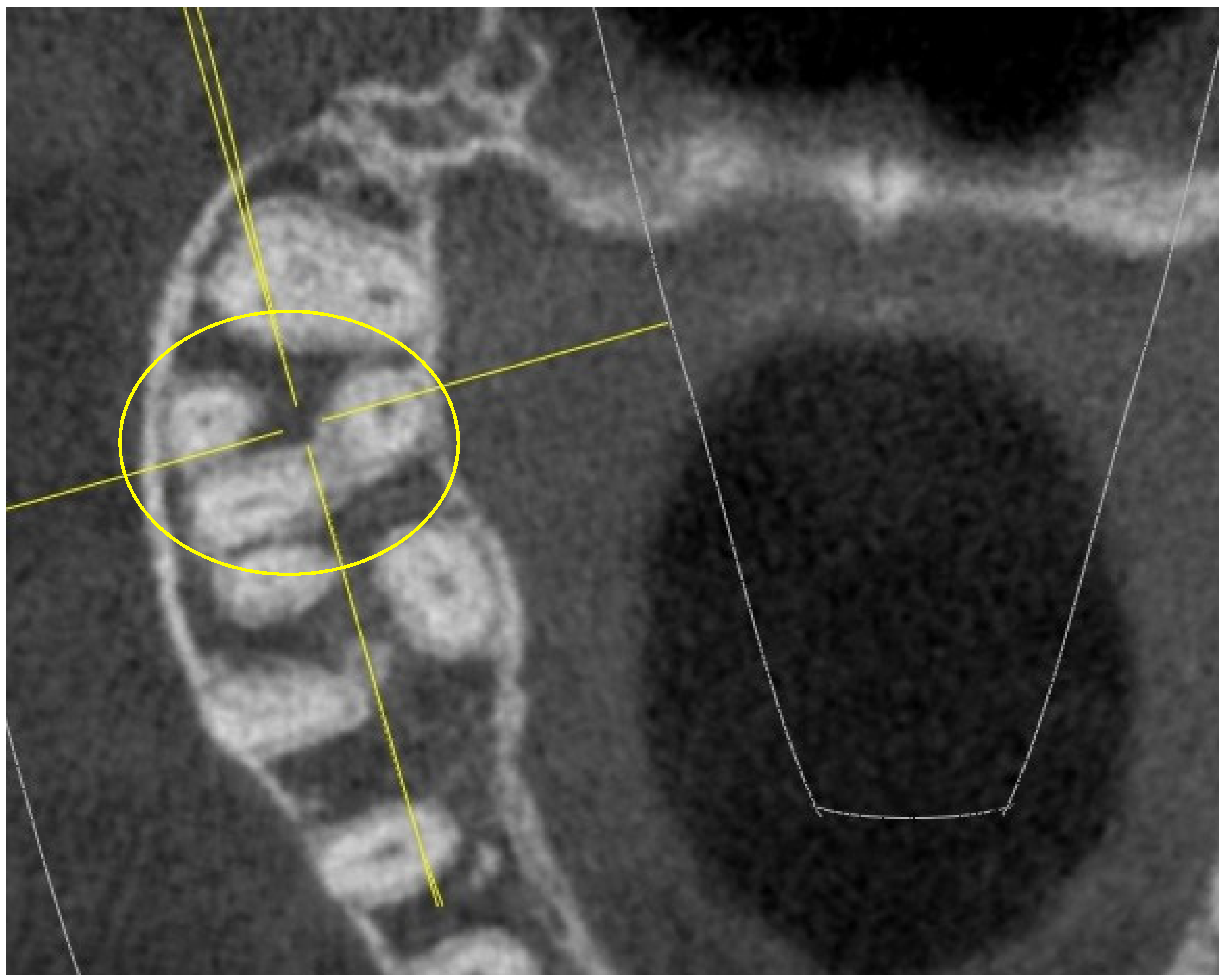
- shape of the pulp chamber associated with a letter of the alphabet (in relation to the number and arrangement of canal orifices);
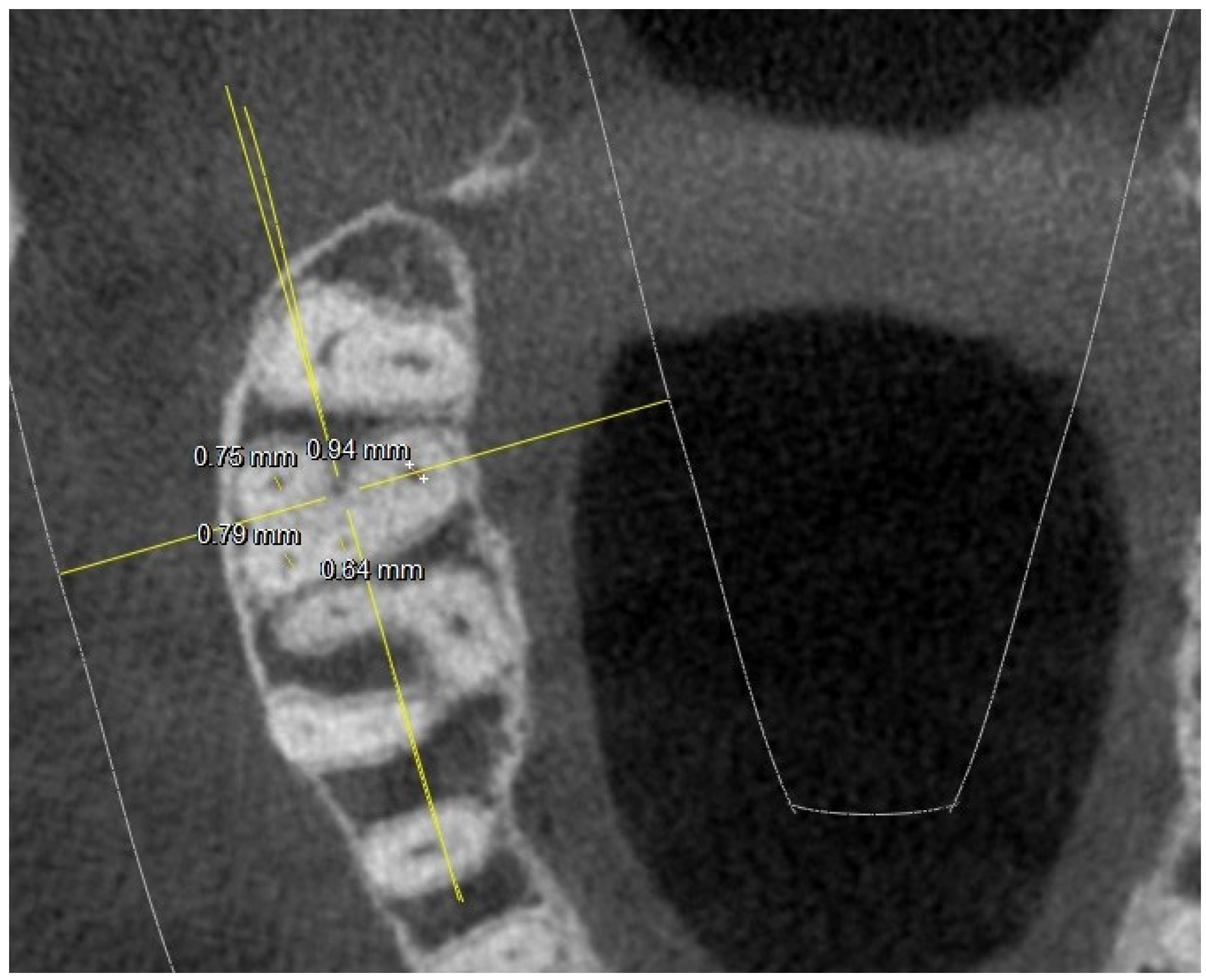
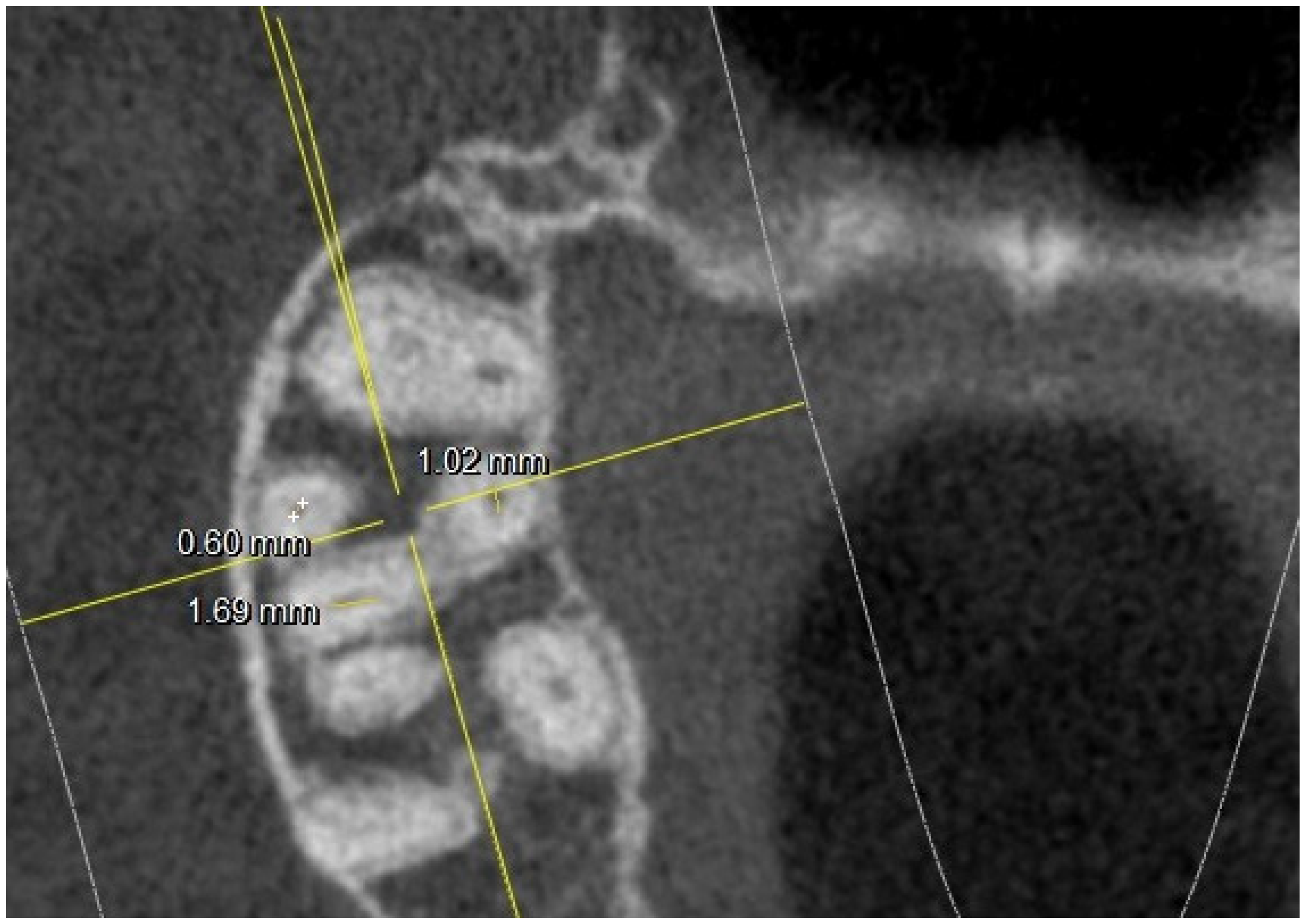
- diameter of root canal orifices;
- distance between intra- and inter-root canals;
- possible fusion of the roots;
- root diameter.
- K: in maxillary molars with the presence of four canal orifices: MB, MB-2, disto-buccal and palatal; a line joining the disto-buccal and palatal and two other lines radiating from the center of this line to MB and MB-2, forming the letter “K” of the alphabet.
- Y: in maxillary molars with three canal orifices: MB, disto-buccal and palatal; when a line is formed joining the three canals in the center of the access cavity, it resembles the letter “Y” of the alphabet.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dablanca-Blanco, A.-B.; Castelo-Baz, P.; Miguéns-Vila, R.; Álvarez-Novoa, P.; Martín-Biedma, B. Endodontic Rotary Files, What Should an Endodontist Know? Medicina 2022, 58, 719. [Google Scholar] [CrossRef]
- Karamifar, K.; Samavi, S.; Saghiri, M.A. Topographic changes in NiTi rotary instruments after the clinical use. Aust. Endod. J. 2020, 46, 315–322. [Google Scholar] [CrossRef]
- Pedullà, E.; Kharouf, N.; Caruso, S.; La Rosa, G.R.M.; Jmal, H.; Haikel, Y.; Mancino, D. Torsional, Static, and Dynamic Cyclic Fatigue Resistance of Reciprocating and Continuous Rotating Nickel-Titanium Instruments. J Endod. 2022, 48, 1421–1427. [Google Scholar] [CrossRef]
- Antony, D.P.; Thomas, T.; Nivedhitha, M.S. Two-dimensional Periapical, Panoramic Radiography Versus Three-dimensional Cone-beam Computed Tomography in the Detection of Periapical Lesion After Endodontic Treatment: A Systematic Review. Cureus 2020, 12, e7736. [Google Scholar] [CrossRef]
- Reda, R.; Zanza, A.; Bhandi, S.; De Biase, A.; Testarelli, L.; Miccoli, G. Surgical-anatomical evaluation of mandibular premolars by CBCT among the Italian population. Dent. Med. Probl. 2022, 59, 209–216. [Google Scholar] [CrossRef]
- Elbarbary, M.; Sgro, A.; Khazaei, S.; Goldberg, M.; Tenenbaum, H.C.; Azarpazhooh, A. The applications of ultrasound, and ultrasonography in dentistry: A scoping review of the literature. Clin. Oral Investig. 2022, 26, 2299–2316. [Google Scholar] [CrossRef]
- Kazemipoor, M.; Sabaghzadegan, F.; Ezoddini Ardakani, F. Pattern of Endodontic Periapical Lesion Extension in Anterior Teeth: A CBCT Study in an Iranian Population. Iran Endod J. 2019, 14, 259–264. [Google Scholar] [CrossRef]
- Seracchiani, M.; Reda, R.; Zanza, A.; D’angelo, M.; Russo, P.; Luca, T. Mechanical Performance and Metallurgical Characteristics of 5 Different Single-file Reciprocating Instruments: A Comparative In Vitro and Laboratory Study. J. Endod. 2022, 48, 1073–1080. [Google Scholar] [CrossRef] [PubMed]
- Ashkar, I.; Sanz, J.L.; Forner, L. Cyclic Fatigue Resistance of Glide Path Rotary Files: A Systematic Review of in Vitro Studies. Materials (Basel). 2022, 15, 6662. [Google Scholar] [CrossRef] [PubMed]
- McGuigan, M.B.; Louca, C.; Duncan, H.F. Endodontic instrument fracture: Causes and prevention. Br. Dent. J. 2013, 214, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Bhagabati, N.; Yadav, S.; Talwar, S. An In Vitro Cyclic Fatigue Analysis of Different Endodontic Nickel-Titanium Rotary Instruments. J. Endod. 2012, 38, 515–518. [Google Scholar] [CrossRef] [PubMed]
- Pawar, A.M.; Singh, S. New classification for pulp chamber floor anatomy of human molars. J. Conserv. Dent. 2020, 23, 430–435. [Google Scholar] [CrossRef] [PubMed]
- Pirani, C.; Camilleri, J. Effectiveness of root canal filling materials and techniques for treatment of apical periodontitis: A systematic review. Int Endod J. 2023, 56, 436–454. [Google Scholar] [CrossRef] [PubMed]
- Krasner, P.; Rankow, H.J. Anatomy of the pulp-chamber floor. J Endod. 2004, 30, 5–16. [Google Scholar] [CrossRef] [PubMed]
- Lertchirakarn, V.; Timyam, A.; Messer, H. Effects of Root Canal Sealers on Vertical Root Fracture Resistance of Endodontically Treated Teeth. J. Endod. 2002, 28, 217–219. [Google Scholar] [CrossRef]
- Alrahabi, M.; Zafar, M.S.; Adanir, N. Aspects of Clinical Malpractice in Endodontics. Eur. J. Dent. 2019, 13, 450–458. [Google Scholar] [CrossRef]
- Rodrigues, F.B.; Paranhos, M.P.G.; Spohr, A.M.; Oshima, H.M.S.; Carlini, B.; Burnett, L.H., Jr. Fracture resistance of root filled molar teeth restored with glass fibre bundles. Int. Endod. J. 2010, 43, 356–362. [Google Scholar] [CrossRef]
- Patel, S.; Brown, J.; Pimentel, T.; Kelly, R.D.; Abella, F.; Durack, C. Cone beam computed tomography in Endodontics—A review of the literature. Int. Endod. J. 2019, 52, 1138–1152. [Google Scholar] [CrossRef]
- Gambarini, G.; Plotino, G.; Grande, N.M.; Testarelli, L.; Prencipe, M.; Messineo, D.; Fratini, L.; D’ambrosio, F. Differential diagnosis of endodontic-related inferior alveolar nerve paraesthesia with cone beam computed tomography: A case report. Int. Endod. J. 2011, 44, 176–181. [Google Scholar] [CrossRef]
- Corte-Real, A.; Nunes, T.; Caetano, C.; Almiro, P.A. Cone Beam Computed Tomography (CBCT) Technology and Learning Outcomes in Dental Anatomy Education: E-Learning Approach. Anat. Sci. Educ. 2021, 14, 711–720. [Google Scholar] [CrossRef]
- Mufadhal, A.A.; Madfa, A.A. The morphology of permanent maxillary first molars evaluated by cone-beam computed tomography among a Yemeni population. BMC Oral Health 2023, 23, 46. [Google Scholar] [CrossRef] [PubMed]
- Swimberghe, R.C.D.; Buyse, R.; Meire, M.A.; De Moor, R.J.G. Efficacy of different irrigation technique in simulated curved root canals. Lasers Med Sci. 2021, 36, 1317–1322. [Google Scholar] [CrossRef] [PubMed]
- Boutsioukis, C.; Arias-Moliz, M.T. Present status and future directions-irrigants and irrigation methods. Int. Endod. J. 2022, 55 (Suppl. S3), 588–612. [Google Scholar] [CrossRef] [PubMed]
- Gavini, G.; Santos, M.D.; Caldeira, C.L.; Machado, M.E.L.; Freire, L.G.; Iglecias, E.F.; Peters, O.A.; Candeiro, G.T.M. Nickel-titanium instruments in endodontics: A concise review of the state of the art. Braz Oral Res. 2018, 32, e67. [Google Scholar] [CrossRef] [PubMed]
- Betancourt, P.; Navarro, P.; Cantín, M.; Fuentes, R. Cone-beam computed tomography study of prevalence and location of MB2 canal in the mesiobuccal root of the maxillary second molar. Int. J. Clin. Exp. Med. 2015, 8, 9128–9134. [Google Scholar] [PubMed]
- Zhuk, R.; Taylor, S.; Johnson, J.D.; Paranjpe, A. Locating the MB2 canal in relation to MB1 in Maxillary First Molars using CBCT imaging. Aust. Endod. J. 2020, 46, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Adhikari, H. Efficacy of cone beam computed tomography in the detection of MB2 canals in the mesiobuccal roots of maxillary first molars: An in vitro study. J. Conserv. Dent. 2017, 20, 332–336. [Google Scholar] [CrossRef]
- Shen, Y.; Gu, Y. Assessment of the presence of a second mesiobuccal canal in maxillary first molars according to the location of the main mesiobuccal canal–a micro-computed tomographic study. Clin. Oral Investig. 2021, 25, 3937–3944. [Google Scholar] [CrossRef]
- Martins, J.N.; Marques, D.; Silva, E.J.N.L.; Caramês, J.; Mata, A.; Versiani, M.A. Second mesiobuccal root canal in maxillary molars—A systematic review and meta-analysis of prevalence studies using cone beam computed tomography. Arch. Oral Biol. 2020, 113, 104589. [Google Scholar] [CrossRef]
- Polineni, S.; Bolla, N.; Mandava, P.; Vemuri, S.; Mallela, M.; Gandham, V.M. Marginal adaptation of newer root canal sealers to dentin: A SEM study. J Conserv Dent. 2016, 19, 360. [Google Scholar] [CrossRef]
- Arroyo-Bote, S. Use of cbct in the endodontic management of a second mandibular premolar with three roots: Clinical case. J. Clin. Exp. Dent. 2022, 14, e107–e113. [Google Scholar] [CrossRef] [PubMed]
- Jing, Y.N.; Ye, X.; Liu, D.G.; Zhang, Z.Y.; Ma, X.C. Cone-beam computed tomography was used for study of root and canal morphology of maxillary first and second molars. Beijing Da Xue Xue Bao Yi Xue Ban 2014, 46, 958–962. [Google Scholar] [PubMed]
- Hung, K.F.; Hui, L.; Yeung, A.W.K.; Jacobs, R.; Leung, Y.Y.; Bornstein, M.M. An analysis of patient dose received during cone-beam computed tomography in relation to scan settings and imaging indications as seen in a dental institution in order to establish institutional diagnostic reference levels. Dentomaxillofac Radiol. 2022, 51, 20200529. [Google Scholar] [CrossRef]




| 16 | 17 | 26 | 27 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean Value | SD | MeanValue | SD | Mean Value | SD | Mean Value | SD | |||
| Long diameter | 5.89 | 1.01 | 5.74 | 0.98 | 5.98 | 1.05 | 5.62 | 0.99 | ||
| Short diameter | 3.74 | 1.51 | 3.25 | 1.42 | 3.18 | 1.62 | 3.2 | |||
| Shape | K(20), Y(4), I(2) | K(16), Y(9), I(1) | K(23), Y(2), I(1) | K(11), Y(12), I(3) | ||||||
| At the orifice: M-B diameter | 0.65 | 0.21 | 0.81 | 0.17 | 0.74 | 0.24 | 0.67 | 0.21 | ||
| D-B diameter | 0.69 | 0.11(2 NO) | 0.72 | 0.14 (1 NO) | 0.65 | 0.12 (1 NO) | 0.69 | 0.15 (3 NO) | ||
| Palatal diameter | 0.89 | 0.18 | 0.89 | 0.21 | 1.12 | 0.16 | 0.89 | 0.18 | ||
| Mb2 diameter | 0.38 | 0.12 (6 NO) | 0.3 | 0.8 (10 NO) | 0.39 | 0.9 (3 NO) | 0.34 | 0.8 (15 NO) | ||
| At the orifice: MB-DB distance | 2.33 | 0.22 | 2.35 | 0.21 | 2.22 | 0.2 | 2.19 | 0.2 | ||
| DB-P distance | 2.96 | 0.44 | 3.25 | 0.2 | 3.32 | 0.41 | 3.67 | 0.2 | ||
| P-MB2 distance | 3.65 | 0.52 | 3.39 | 0.42 | 3.62 | 0.48 | 3.68 | 0.39 | ||
| MB1-MB2 distance | 1.54 | 0.21 | 1.67 | 0.21 | 1.63 | 0.19 | 1.45 | 0.22 | ||
| MB-P distance | 4.91 | 0.3 | 5.03 | 0.36 | 5.02 | 0.26 | 4.87 | 0.31 | ||
| 5 mm from the CEJ: MB diameter | 0.74 | 0.26 | 0.85 | 0.21 | 0.74 | 0.24 | 0.8 | 0.22 | ||
| DB diameter | 0.79 | 0.14 (2 NO) | 0.65 | 0.11 (1 NO) | 0.75 | 0.12 (1 NO) | 0.68 | 0.12 (3 NO) | ||
| Palatal diameter | 1.19 | 0.07 | 1.1 | 0.06 | 1.35 | 0.06 | 1.19 | 0.06 | ||
| MB2 diameter | 0.42 | 0.6 (2 NO) | 0.47 | 0.5 (7 NO) | 0.47 | 0.7 (3 NO) | 0.42 | 0.4 (11 NO) | ||
| 5 mm from the CEJ: MB-DB distance | 4.35 | 0.82 | 2.88 | 0.62 | 4.13 | 0.78 | 2.97 | 0.64 | ||
| DB-P distance | 5.65 | 1.03 | 5.42 | 1.12 | 5.44 | 1.23 | 5.1 | 0.98 | ||
| P-MB2 distance | 5.94 | 1.45 | 4.94 | 1.44 | 5.61 | 1.65 | 3.28 | 1.12 | ||
| MB1-MB2 distance | 1.98 | 0.62 | 1.52 | 0.44 | 1.9 | 0.4 | 1.32 | 0.42 | ||
| MB-P distance | 7.56 | 1.7 | 6.55 | 1.55 | 7.14 | 1.52 | 5.68 | 1.49 | ||
| 5 mm from the CEJ: MB root diameter | 6.78 2.64 | 1.76 0.68 | 6 2.8 | 1.35 0.70 | 6.46 2.75 | 2.02 1.12 | 5.96 2.8 | 1.68 0.56 | ||
| DB root diameter | 5.04 2.94 | 1.43 1.12 (3 NO) | 4.49 3 | 1.06 0,89 (8 NO) | 5.15 2.98 | 1.12 0.68 | 4.33 3.3 | 1.21 0.88 4 NO | ||
| Palatal root diameter | 5.62 4.63 | 1.12 0.58 | 5.25 4.45 | 1.06 0.89 | 5.7 | 4.53 | 1.12 0.98 | 4.99 4.41 | 1.12 0.86 | |
| Roots fusions | 8 | 19 | 7 | 18 | ||||||
| 3 mm from the apex: MB diameter | 0.54 | 0.22 | 0.69 | 0.18 | 0.66 | 0.12 | 0.55 | 0.11 | ||
| DB diameter | 0.54 | 0.21 (2 NO) | 0.54 | 0.17 (1 NO) | 0.58 | 0.18 (1 NO) | 0.53 | 0.16 (3 NO) | ||
| Palatal diameter | 0.87 | 0.12 | 0.86 | 0.12 | 0.82 | 0.16 | 0.59 | 0.17 | ||
| MB2 diameter | 0.39 | 0.08 (8 NO) | 0.28 | 0.06 (9 NO) | 0.44 | 0.12 (5 NO) | 0.19 | 0.07 (7 NO) | ||
| 3 mm from the apex: MB-DB distance | 4.93 | 1.89 | 2.82 | 0.67 | 4.07 | 1.76 | 3.06 | 1.99 | ||
| DB-P distance | 8.6 | 2 | 7.12 | 1.9 | 8.12 | 2.6 | 6.64 | 1.89 | ||
| P-MB2 distance | 8.48 | 2.42 | 5.7 | 1.88 | 7.6 | 2.43 (12 NO) | 5.55 | 1.68 | ||
| MB1-MB2 distance | 1.48 | 0.41 | 0.87 | 0.22 | 1.72 | 0.41 | 1.76 | 0.45 | ||
| MB-P distance | 9.13 | 2.12 | 7.23 | 1.99 | 8.85 | 2.43 | 6.48 | 1.88 | ||
| 3 mm from the apex: MB root diameter | 5.03 2.6 | 1.23 0.86 (3 NO) | 4.26 2.14 | 1.18 0.64 (1 NO) | 2.7 4.9 | 1.23 0.58 (2 NO) | 4.6 2.94 | 1.55 0.66 (7 NO) | ||
| DB root diameter | 4.08 2.91 | 1.21 0.68 (5 NO) | 3.5 2.44 | 0.9 0.66 (10 NO) | 3.65 2.4 | 1.44 0.54 (5 NO) | 3.58 2.58 | 1.23 0.66 (9 NO) | ||
| Palatal root diameter | 4.9 3.7 | 1.77 1.01 | 3.38 1.95 | 1.12 0.66 | 4.8 3.5 | 1.23 0.88 | 4 3.15 | 1.12 0.99 (2 NO) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reda, R.; Di Nardo, D.; Zanza, A.; Bellanova, V.; Abbagnale, R.; Pagnoni, F.; D’Angelo, M.; Pawar, A.M.; Galli, M.; Testarelli, L. Upper First and Second Molar Pulp Chamber Endodontic Anatomy Evaluation According to a Recent Classification: A Cone Beam Computed Tomography Study. J. Imaging 2024, 10, 9. https://doi.org/10.3390/jimaging10010009
Reda R, Di Nardo D, Zanza A, Bellanova V, Abbagnale R, Pagnoni F, D’Angelo M, Pawar AM, Galli M, Testarelli L. Upper First and Second Molar Pulp Chamber Endodontic Anatomy Evaluation According to a Recent Classification: A Cone Beam Computed Tomography Study. Journal of Imaging. 2024; 10(1):9. https://doi.org/10.3390/jimaging10010009
Chicago/Turabian StyleReda, Rodolfo, Dario Di Nardo, Alessio Zanza, Valentina Bellanova, Rosemary Abbagnale, Francesco Pagnoni, Maurilio D’Angelo, Ajinkya M. Pawar, Massimo Galli, and Luca Testarelli. 2024. "Upper First and Second Molar Pulp Chamber Endodontic Anatomy Evaluation According to a Recent Classification: A Cone Beam Computed Tomography Study" Journal of Imaging 10, no. 1: 9. https://doi.org/10.3390/jimaging10010009
APA StyleReda, R., Di Nardo, D., Zanza, A., Bellanova, V., Abbagnale, R., Pagnoni, F., D’Angelo, M., Pawar, A. M., Galli, M., & Testarelli, L. (2024). Upper First and Second Molar Pulp Chamber Endodontic Anatomy Evaluation According to a Recent Classification: A Cone Beam Computed Tomography Study. Journal of Imaging, 10(1), 9. https://doi.org/10.3390/jimaging10010009











