Advances in Nanogels for Topical Drug Delivery in Ocular Diseases
Abstract
:1. Introduction
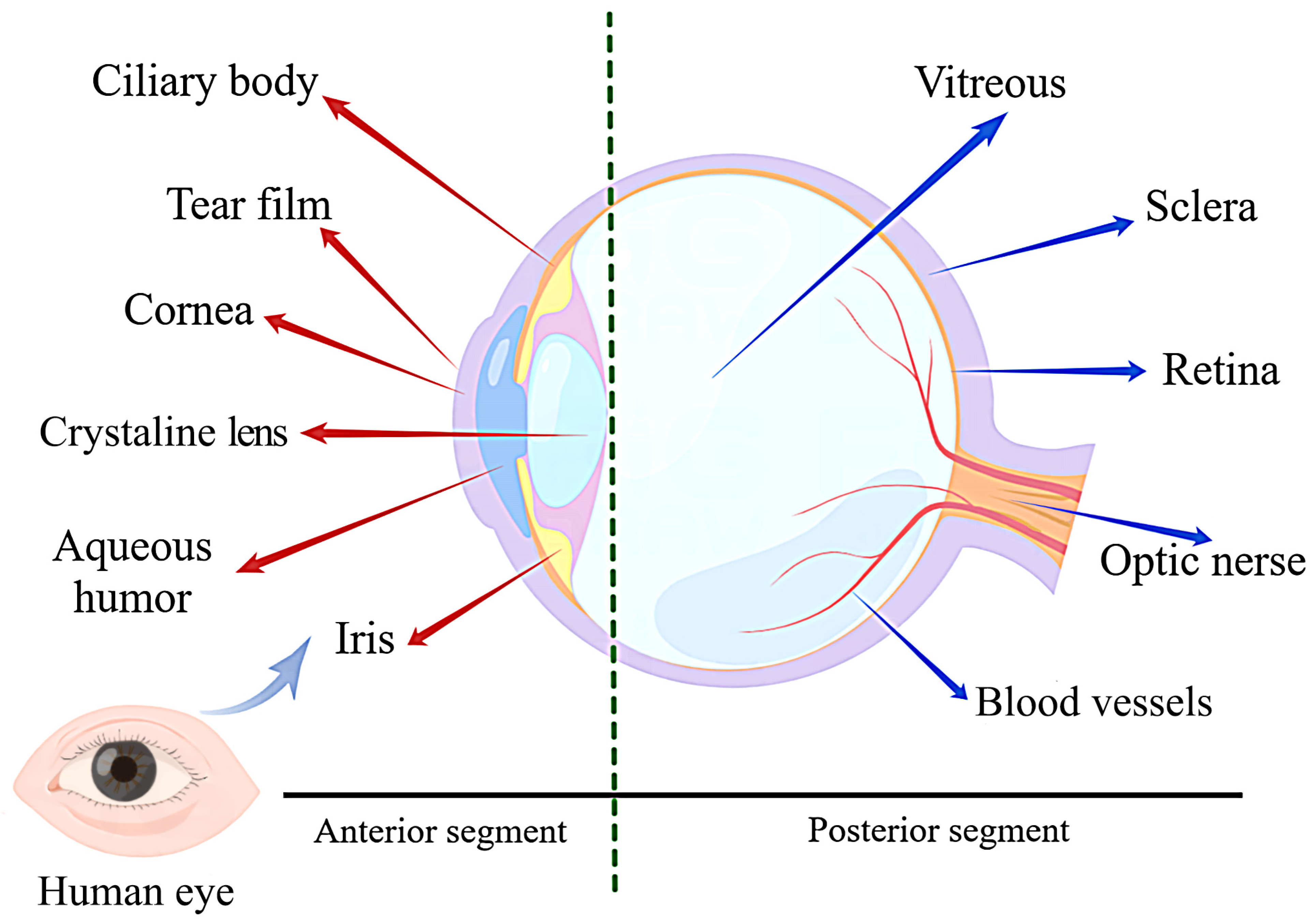
2. Ocular Structure and Barriers
3. Nanogels System
3.1. Concept and Properties of Nanogels
3.2. Preparations of Nanogels
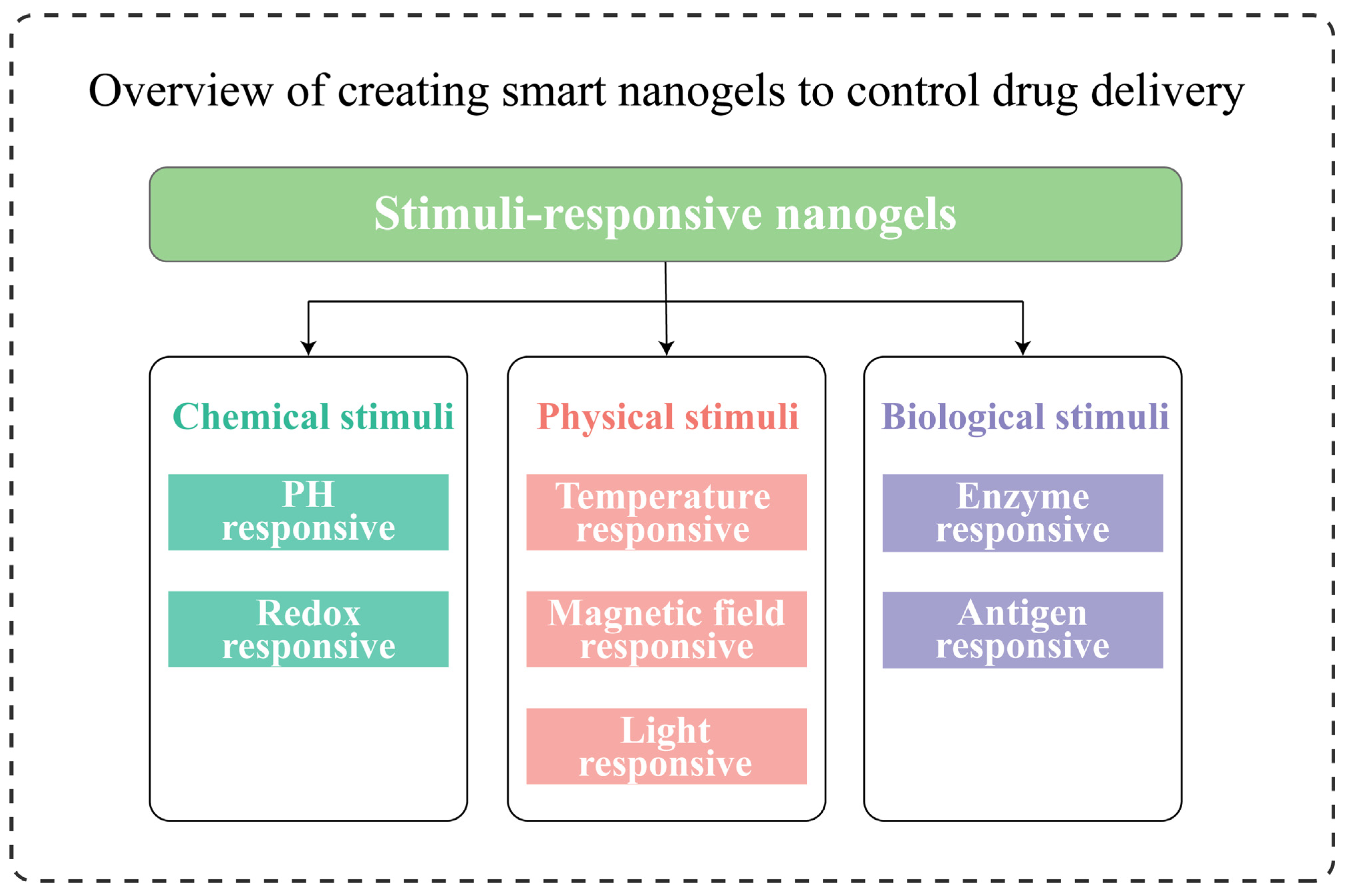
3.3. Stimuli-Responsive Nanogels
4. Advances in Nanogels for Ocular Diseases
4.1. Glaucoma
4.2. Cataract
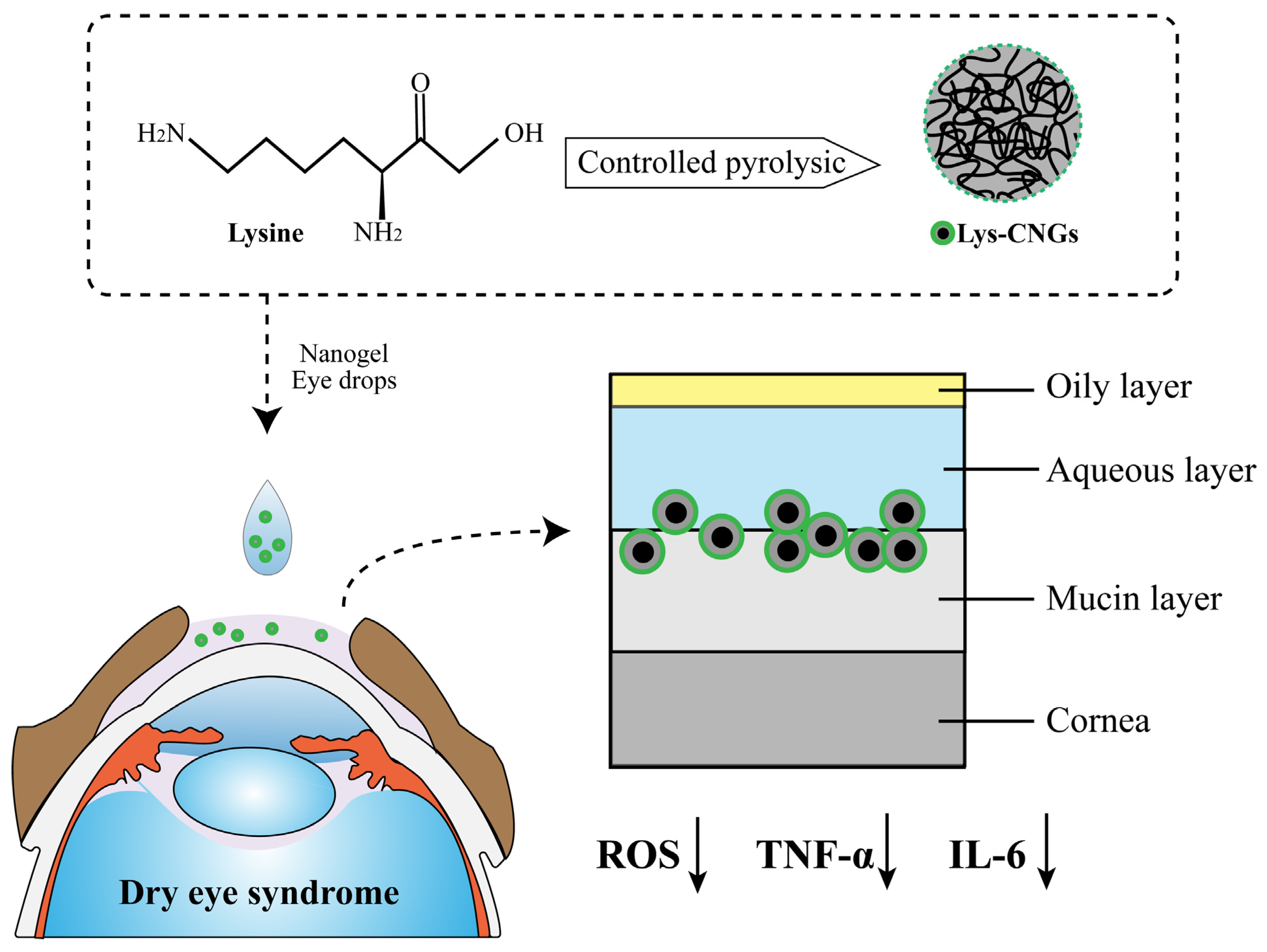
4.3. Dry Eye Syndrome
4.4. Bacterial Keratitis
4.5. Nanogel Contact Lenses
4.6. Other Ocular Applications
5. Conclusions and Future Prospects
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bourne, R.; Steinmetz, J.D.; Flaxman, S.; Briant, P.S.; Taylor, H.R.; Resnikoff, S.; Casson, R.J.; Abdoli, A.; Abu-Gharbieh, E.; Afshin, A.; et al. Vision Loss Expert Group of the Global Burden of Disease Study Trends in Prevalence of Blindness and Distance and near Vision Impairment over 30 Years: An Analysis for the Global Burden of Disease Study. Lancet Glob. Health 2021, 9, e130–e143. [Google Scholar]
- Awwad, S.; Mohamed Ahmed, A.H.A.; Sharma, G.; Heng, J.S.; Khaw, P.T.; Brocchini, S.; Lockwood, A. Principles of Pharmacology in the Eye. Br. J. Pharmacol. 2017, 174, 4205–4223. [Google Scholar] [PubMed] [Green Version]
- Jumelle, C.; Gholizadeh, S.; Annabi, N.; Dana, R. Advances and Limitations of Drug Delivery Systems Formulated as Eye Drops. J. Control. Release Off. J. Control. Release Soc. 2020, 321, 1–22. [Google Scholar]
- Zhu, M.; Wang, J.; Li, N. A Novel Thermo-Sensitive Hydrogel-Based on Poly(N-Isopropylacrylamide)/Hyaluronic Acid of Ketoconazole for Ophthalmic Delivery. Artif. Cells Nanomed. Biotechnol. 2018, 46, 1282–1287. [Google Scholar] [PubMed] [Green Version]
- Sánchez-López, E.; Espina, M.; Doktorovova, S.; Souto, E.B.; García, M.L. Lipid Nanoparticles (SLN, NLC): Overcoming the Anatomical and Physiological Barriers of the Eye—Part I—Barriers and Determining Factors in Ocular Delivery. Eur. J. Pharm. Biopharm. Off. J. Arbeitsgem. Pharm. Verfahr. EV 2017, 110, 70–75. [Google Scholar]
- Bisht, R.; Mandal, A.; Jaiswal, J.K.; Rupenthal, I.D. Nanocarrier Mediated Retinal Drug Delivery: Overcoming Ocular Barriers to Treat Posterior Eye Diseases. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2018, 10, e1473. [Google Scholar]
- Kour, J.; Kumari, N.; Sapra, B. Ocular Prodrugs: Attributes and Challenges. Asian J. Pharm. Sci. 2021, 16, 175–191. [Google Scholar]
- Müller, L.; Jensen, B.P.; Bachmann, L.M.; Wong, D.; Wells, A.P. New Technique to Reduce Systemic Side Effects of Timolol Eye Drops: The Tissue Press Method-Cross-over Clinical Trial. Clin. Exp. Ophthalmol. 2020, 48, 24–30. [Google Scholar]
- Akhter, M.H.; Ahmad, I.; Alshahrani, M.Y.; Al-Harbi, A.I.; Khalilullah, H.; Afzal, O.; Altamimi, A.S.A.; Najib Ullah, S.N.M.; Ojha, A.; Karim, S. Drug Delivery Challenges and Current Progress in Nanocarrier-Based Ocular Therapeutic System. Gels 2022, 8, 82. [Google Scholar]
- Ahmed, S.; Amin, M.M.; Sayed, S. Ocular Drug Delivery: A Comprehensive Review. AAPS PharmSciTech 2023, 24, 66. [Google Scholar]
- Li, Q.; Li, Z.; Zeng, W.; Ge, S.; Lu, H.; Wu, C.; Ge, L.; Liang, D.; Xu, Y. Proniosome-Derived Niosomes for Tacrolimus Topical Ocular Delivery: In Vitro Cornea Permeation, Ocular Irritation, and in Vivo Anti-Allograft Rejection. Eur. J. Pharm. Sci. Off. J. Eur. Fed. Pharm. Sci. 2014, 62, 115–123. [Google Scholar] [CrossRef]
- Yang, Y.; Lockwood, A. Topical Ocular Drug Delivery Systems: Innovations for an Unmet Need. Exp. Eye Res. 2022, 218, 109006. [Google Scholar] [CrossRef] [PubMed]
- Onugwu, A.L.; Nwagwu, C.S.; Onugwu, O.S.; Echezona, A.C.; Agbo, C.P.; Ihim, S.A.; Emeh, P.; Nnamani, P.O.; Attama, A.A.; Khutoryanskiy, V.V. Nanotechnology Based Drug Delivery Systems for the Treatment of Anterior Segment Eye Diseases. J. Control. Release Off. J. Control. Release Soc. 2023, 354, 465–488. [Google Scholar] [CrossRef]
- Mauri, E.; Giannitelli, S.M.; Trombetta, M.; Rainer, A. Synthesis of Nanogels: Current Trends and Future Outlook. Gels 2021, 7, 36. [Google Scholar] [CrossRef]
- Soni, K.S.; Desale, S.S.; Bronich, T.K. Nanogels: An Overview of Properties, Biomedical Applications and Obstacles to Clinical Translation. J. Control. Release Off. J. Control. Release Soc. 2016, 240, 109–126. [Google Scholar]
- Yin, Y.; Hu, B.; Yuan, X.; Cai, L.; Gao, H.; Yang, Q. Nanogel: A Versatile Nano-Delivery System for Biomedical Applications. Pharmaceutics 2020, 12, 290. [Google Scholar] [CrossRef] [Green Version]
- Neamtu, I.; Rusu, A.G.; Diaconu, A.; Nita, L.E.; Chiriac, A.P. Basic Concepts and Recent Advances in Nanogels as Carriers for Medical Applications. Drug Deliv. 2017, 24, 539–557. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Narayanan, K.B.; Bhaskar, R.; Han, S.S. Recent Advances in the Biomedical Applications of Functionalized Nanogels. Pharmaceutics 2022, 14, 2832. [Google Scholar] [CrossRef]
- Bhaladhare, S.; Bhattacharjee, S. Chemical, Physical, and Biological Stimuli-Responsive Nanogels for Biomedical Applications (Mechanisms, Concepts, and Advancements): A Review. Int. J. Biol. Macromol. 2023, 226, 535–553. [Google Scholar] [CrossRef]
- Oh, J.K.; Drumright, R.; Siegwart, D.J.; Matyjaszewski, K. The Development of Microgels/Nanogels for Drug Delivery Applications. Prog. Polym. Sci. 2008, 33, 448–477. [Google Scholar] [CrossRef]
- Laha, B.; Das, S.; Maiti, S.; Sen, K.K. Novel Propyl Karaya Gum Nanogels for Bosentan: In Vitro and in Vivo Drug Delivery Performance. Colloids Surf. B Biointerfaces 2019, 180, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Han, Y.; Zhu, T.; Wu, X.; Yu, W.; Zhu, J.; Shang, Y.; Lin, X.; Zhao, T. Targeting Delivery and Minimizing Epidermal Diffusion of Tranexamic Acid by Hyaluronic Acid-Coated Liposome Nanogels for Topical Hyperpigmentation Treatment. Drug Deliv. 2021, 28, 2100–2107. [Google Scholar] [CrossRef] [PubMed]
- Rosso, A.P.; Martinelli, M. Nanogels and Dendritic Molecules Combined to Form a Smart Nanomaterial. Eur. Polym. J. 2022, 162, 110874. [Google Scholar] [CrossRef]
- Wen, Y.; Jia, H.; Mo, Z.; Zheng, K.; Chen, S.; Ding, Y.; Zhang, Y.; Wen, Y.; Xie, Q.; Qiu, J.; et al. Cross-Linked Thermosensitive Nanohydrogels for Ocular Drug Delivery with a Prolonged Residence Time and Enhanced Bioavailability. Mater. Sci. Eng. C 2021, 119, 111445. [Google Scholar] [CrossRef]
- Alshaikh, R.A.; Waeber, C.; Ryan, K.B. Polymer Based Sustained Drug Delivery to the Ocular Posterior Segment: Barriers and Future Opportunities for the Treatment of Neovascular Pathologies. Adv. Drug Deliv. Rev. 2022, 187, 114342. [Google Scholar] [CrossRef]
- Alami-Milani, M.; Zakeri-Milani, P.; Valizadeh, H.; Salehi, R.; Salatin, S.; Naderinia, A.; Jelvehgari, M. Novel Pentablock Copolymers as Thermosensitive Self-Assembling Micelles for Ocular Drug Delivery. Adv. Pharm. Bull. 2017, 7, 11–20. [Google Scholar] [CrossRef] [Green Version]
- DelMonte, D.W.; Kim, T. Anatomy and Physiology of the Cornea. J. Cataract Refract. Surg. 2011, 37, 588–598. [Google Scholar] [CrossRef]
- Barar, J.; Javadzadeh, A.R.; Omidi, Y. Ocular Novel Drug Delivery: Impacts of Membranes and Barriers. Expert Opin. Drug Deliv. 2008, 5, 567–581. [Google Scholar] [CrossRef]
- Huang, D.; Chen, Y.-S.; Rupenthal, I.D. Overcoming Ocular Drug Delivery Barriers through the Use of Physical Forces. Adv. Drug Deliv. Rev. 2018, 126, 96–112. [Google Scholar] [CrossRef]
- Huang, H.S.; Schoenwald, R.D.; Lach, J.L. Corneal Penetration Behavior of Beta-Blocking Agents II: Assessment of Barrier Contributions. J. Pharm. Sci. 1983, 72, 1272–1279. [Google Scholar] [CrossRef] [PubMed]
- Cholkar, K.; Patel, S.P.; Vadlapudi, A.D.; Mitra, A.K. Novel Strategies for Anterior Segment Ocular Drug Delivery. J. Ocul. Pharmacol. Ther. Off. J. Assoc. Ocul. Pharmacol. Ther. 2013, 29, 106–123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nelson, J.D.; Craig, J.P.; Akpek, E.K.; Azar, D.T.; Belmonte, C.; Bron, A.J.; Clayton, J.A.; Dogru, M.; Dua, H.S.; Foulks, G.N.; et al. TFOS DEWS II Introduction. Ocul. Surf. 2017, 15, 269–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaneev, A.; Tikhomirova, V.; Chesnokova, N.; Popova, E.; Beznos, O.; Kost, O.; Klyachko, N. Nanotechnology for Topical Drug Delivery to the Anterior Segment of the Eye. Int. J. Mol. Sci. 2021, 22, 12368. [Google Scholar] [CrossRef] [PubMed]
- Watsky, M.A.; Jablonski, M.M.; Edelhauser, H.F. Comparison of Conjunctival and Corneal Surface Areas in Rabbit and Human. Curr. Eye Res. 1988, 7, 483–486. [Google Scholar] [CrossRef]
- Lawrence, M.S.; Miller, J.W. Ocular Tissue Permeabilities. Int. Ophthalmol. Clin. 2004, 44, 53–61. [Google Scholar] [CrossRef]
- Achouri, D.; Alhanout, K.; Piccerelle, P.; Andrieu, V. Recent Advances in Ocular Drug Delivery. Drug Dev. Ind. Pharm. 2013, 39, 1599–1617. [Google Scholar] [CrossRef]
- Alamouti, B.; Funk, J. Retinal Thickness Decreases with Age: An OCT Study. Br. J. Ophthalmol. 2003, 87, 899–901. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, H. Ocular Barriers as a Double-Edged Sword: Preventing and Facilitating Drug Delivery to the Retina. Drug Deliv. Transl. Res. 2023, 13, 547–567. [Google Scholar] [CrossRef]
- Liu, Z.; Huang, S.; Zheng, Y.; Zhou, T.; Hu, L.; Xiong, L.; Li, D.W.-C.; Liu, Y. The Lens Epithelium as a Major Determinant in the Development, Maintenance, and Regeneration of the Crystalline Lens. Prog. Retin. Eye Res. 2023, 92, 101112. [Google Scholar] [CrossRef]
- Cui, W.; Li, J.; Decher, G. Self-Assembled Smart Nanocarriers for Targeted Drug Delivery. Adv. Mater. Deerfield Beach Fla 2016, 28, 1302–1311. [Google Scholar] [CrossRef]
- Zhang, J.; Jiao, J.; Niu, M.; Gao, X.; Zhang, G.; Yu, H.; Yang, X.; Liu, L. Ten Years of Knowledge of Nano-Carrier Based Drug Delivery Systems in Ophthalmology: Current Evidence, Challenges, and Future Prospective. Int. J. Nanomed. 2021, 16, 6497–6530. [Google Scholar] [CrossRef] [PubMed]
- Rezaei, A.; Fathi, M.; Jafari, S.M. Nanoencapsulation of Hydrophobic and Low-Soluble Food Bioactive Compounds within Different Nanocarriers. Food Hydrocoll. 2019, 88, 146–162. [Google Scholar] [CrossRef]
- Shi, Y.; van der Meel, R.; Chen, X.; Lammers, T. The EPR Effect and beyond: Strategies to Improve Tumor Targeting and Cancer Nanomedicine Treatment Efficacy. Theranostics 2020, 10, 7921–7924. [Google Scholar] [CrossRef]
- Gowd, V.; Ahmad, A.; Tarique, M.; Suhail, M.; Zughaibi, T.A.; Tabrez, S.; Khan, R. Advancement of Cancer Immunotherapy Using Nanoparticles-Based Nanomedicine. Semin. Cancer Biol. 2022, 86, 624–644. [Google Scholar] [CrossRef]
- Torchilin, V.P. Multifunctional, Stimuli-Sensitive Nanoparticulate Systems for Drug Delivery. Nat. Rev. Drug Discov. 2014, 13, 813–827. [Google Scholar] [CrossRef] [Green Version]
- Vinogradov, S.; Batrakova, E.; Kabanov, A. Poly(Ethylene Glycol)–Polyethyleneimine NanoGelTM Particles: Novel Drug Delivery Systems for Antisense Oligonucleotides. Colloids Surf. B Biointerfaces 1999, 16, 291–304. [Google Scholar] [CrossRef]
- Suhail, M.; Rosenholm, J.M.; Minhas, M.U.; Badshah, S.F.; Naeem, A.; Khan, K.U.; Fahad, M. Nanogels as Drug-Delivery Systems: A Comprehensive Overview. Ther. Deliv. 2019, 10, 697–717. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Maciel, D.; Rodrigues, J.; Shi, X.; Tomás, H. Biodegradable Polymer Nanogels for Drug/Nucleic Acid Delivery. Chem. Rev. 2015, 115, 8564–8608. [Google Scholar] [CrossRef]
- Xu, H.; Li, S.; Liu, Y.-S. Nanoparticles in the Diagnosis and Treatment of Vascular Aging and Related Diseases. Signal Transduct. Target. Ther. 2022, 7, 231. [Google Scholar] [CrossRef]
- Hamidi, M.; Azadi, A.; Rafiei, P. Hydrogel Nanoparticles in Drug Delivery. Adv. Drug Deliv. Rev. 2008, 60, 1638–1649. [Google Scholar] [CrossRef] [PubMed]
- Destruel, P.-L.; Zeng, N.; Maury, M.; Mignet, N.; Boudy, V. In Vitro and in Vivo Evaluation of in Situ Gelling Systems for Sustained Topical Ophthalmic Delivery: State of the Art and Beyond. Drug Discov. Today 2017, 22, 638–651. [Google Scholar] [CrossRef] [PubMed]
- Al-Kinani, A.A.; Zidan, G.; Elsaid, N.; Seyfoddin, A.; Alani, A.W.G.; Alany, R.G. Ophthalmic Gels: Past, Present and Future. Adv. Drug Deliv. Rev. 2018, 126, 113–126. [Google Scholar] [CrossRef] [Green Version]
- Makhathini, S.S.; Mdanda, S.; Kondiah, P.J.; Kharodia, M.E.; Rumbold, K.; Alagidede, I.; Pathak, Y.; Bulbulia, Z.; Rants’o, T.A.; Kondiah, P.P.D. Biomedicine Innovations and Its Nanohydrogel Classifications. Pharmaceutics 2022, 14, 2839. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zhai, Y.; Wang, J.; Zhai, G. New Progress and Prospects: The Application of Nanogel in Drug Delivery. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 60, 560–568. [Google Scholar] [CrossRef]
- Sasaki, Y.; Akiyoshi, K. Nanogel Engineering for New Nanobiomaterials: From Chaperoning Engineering to Biomedical Applications. Chem. Rec. N. Y. N 2010, 10, 366–376. [Google Scholar] [CrossRef]
- Hajebi, S.; Rabiee, N.; Bagherzadeh, M.; Ahmadi, S.; Rabiee, M.; Roghani-Mamaqani, H.; Tahriri, M.; Tayebi, L.; Hamblin, M.R. Stimulus-Responsive Polymeric Nanogels as Smart Drug Delivery Systems. Acta Biomater. 2019, 92, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Obireddy, S.R.; Lai, W.-F. Preparation and Use of Nanogels as Carriers of Drugs. Drug Deliv. 2021, 28, 1594–1602. [Google Scholar] [CrossRef] [PubMed]
- Bonetti, L.; De Nardo, L.; Farè, S. Thermo-Responsive Methylcellulose Hydrogels: From Design to Applications as Smart Biomaterials. Tissue Eng. Part B Rev. 2021, 27, 486–513. [Google Scholar] [CrossRef] [PubMed]
- Fakhari, A.; Berkland, C. Applications and Emerging Trends of Hyaluronic Acid in Tissue Engineering, as a Dermal Filler and in Osteoarthritis Treatment. Acta Biomater. 2013, 9, 7081–7092. [Google Scholar] [CrossRef] [Green Version]
- Yao, Y.; Xia, M.; Wang, H.; Li, G.; Shen, H.; Ji, G.; Meng, Q.; Xie, Y. Preparation and Evaluation of Chitosan-Based Nanogels/Gels for Oral Delivery of Myricetin. Eur. J. Pharm. Sci. Off. J. Eur. Fed. Pharm. Sci. 2016, 91, 144–153. [Google Scholar] [CrossRef]
- Silva, D.; Pinto, L.F.V.; Bozukova, D.; Santos, L.F.; Serro, A.P.; Saramago, B. Chitosan/Alginate Based Multilayers to Control Drug Release from Ophthalmic Lens. Colloids Surf. B Biointerfaces 2016, 147, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Dubashynskaya, N.; Poshina, D.; Raik, S.; Urtti, A.; Skorik, Y.A. Polysaccharides in Ocular Drug Delivery. Pharmaceutics 2019, 12, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, H.-Q.; Fan, Y.; Hu, Y.; Cheng, G.; Xu, F.-J. Polysaccharide–Peptide Conjugates: A Versatile Material Platform for Biomedical Applications. Adv. Funct. Mater. 2021, 31, 2005978. [Google Scholar] [CrossRef]
- Luckanagul, J.A.; Pitakchatwong, C.; Ratnatilaka Na Bhuket, P.; Muangnoi, C.; Rojsitthisak, P.; Chirachanchai, S.; Wang, Q.; Rojsitthisak, P. Chitosan-Based Polymer Hybrids for Thermo-Responsive Nanogel Delivery of Curcumin. Carbohydr. Polym. 2018, 181, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Fathi, M.; Entezami, A.A.; Arami, S.; Rashidi, M.-R. Preparation of N-Isopropylacrylamide/Itaconic Acid Magnetic Nanohydrogels by Modified Starch as a Crosslinker for Anticancer Drug Carriers. Int. J. Polym. Mater. Polym. Biomater. 2015, 64, 541–549. [Google Scholar] [CrossRef]
- Ahmed, S.; Alhareth, K.; Mignet, N. Advancement in Nanogel Formulations Provides Controlled Drug Release. Int. J. Pharm. 2020, 584, 119435. [Google Scholar] [CrossRef]
- Shen, Y.; An, C.; Jiang, J.; Huang, B.; Li, N.; Sun, C.; Wang, C.; Zhan, S.; Li, X.; Gao, F.; et al. Temperature-Dependent Nanogel for Pesticide Smart Delivery with Improved Foliar Dispersion and Bioactivity for Efficient Control of Multiple Pests. ACS Nano 2022, 16, 20622–20632. [Google Scholar] [CrossRef]
- Soriano Pérez, M.L.; Funes, J.A.; Flores Bracamonte, C.; Ibarra, L.E.; Forrellad, M.A.; Taboga, O.; Cariddi, L.N.; Salinas, F.J.; Ortega, H.H.; Alustiza, F.; et al. Development and Biological Evaluation of PNIPAM-Based Nanogels as Vaccine Carriers. Int. J. Pharm. 2023, 630, 122435. [Google Scholar] [CrossRef]
- Recent Developments in Stimuli-Responsive Polymer Nanogels for Drug Delivery and Diagnostics: A Review. Eur. J. Pharm. Biopharm. 2020, 157, 121–153. [CrossRef]
- Bordat, A.; Boissenot, T.; Nicolas, J.; Tsapis, N. Thermoresponsive Polymer Nanocarriers for Biomedical Applications. Adv. Drug Deliv. Rev. 2019, 138, 167–192. [Google Scholar] [CrossRef]
- Cook, M.T.; Haddow, P.; Kirton, S.B.; McAuley, W.J. Polymers Exhibiting Lower Critical Solution Temperatures as a Route to Thermoreversible Gelators for Healthcare. Adv. Funct. Mater. 2021, 31, 2008123. [Google Scholar] [CrossRef]
- Chaudhari, P.; Shetty, D.; Lewis, S.A. Recent Progress in Colloidal Nanocarriers Loaded in Situ Gel in Ocular Therapeutics. J. Drug Deliv. Sci. Technol. 2022, 71, 103327. [Google Scholar] [CrossRef]
- Lee, C.H.; Moturi, V.; Lee, Y. Thixotropic Property in Pharmaceutical Formulations. J. Control. Release Off. J. Control. Release Soc. 2009, 136, 88–98. [Google Scholar] [CrossRef]
- Zha, L.; Banik, B.; Alexis, F. Stimulus Responsive Nanogels for Drug Delivery. Soft Matter 2011, 7, 5908–5916. [Google Scholar] [CrossRef]
- Hartmann, V.; Keipert, S. Physico-Chemical, in Vitro and in Vivo Characterisation of Polymers for Ocular Use. Pharmazie 2000, 55, 440–443. [Google Scholar] [PubMed]
- Kim, Y.K.; Kim, E.-J.; Lim, J.H.; Cho, H.K.; Hong, W.J.; Jeon, H.H.; Chung, B.G. Dual Stimuli-Triggered Nanogels in Response to Temperature and PH Changes for Controlled Drug Release. Nanoscale Res. Lett. 2019, 14, 77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ilka, R.; Mohseni, M.; Kianirad, M.; Naseripour, M.; Ashtari, K.; Mehravi, B. Nanogel-Based Natural Polymers as Smart Carriers for the Controlled Delivery of Timolol Maleate through the Cornea for Glaucoma. Int. J. Biol. Macromol. 2018, 109, 955–962. [Google Scholar] [CrossRef]
- Cuggino, J.C.; Tártara, L.I.; Gugliotta, L.M.; Palma, S.D.; Alvarez Igarzabal, C.I. Mucoadhesive and Responsive Nanogels as Carriers for Sustainable Delivery of Timolol for Glaucoma Therapy. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 118, 111383. [Google Scholar] [CrossRef]
- Abd El-Rehim, H.A.; Swilem, A.E.; Klingner, A.; Hegazy, E.-S.A.; Hamed, A.A. Developing the Potential Ophthalmic Applications of Pilocarpine Entrapped into Polyvinylpyrrolidone-Poly(Acrylic Acid) Nanogel Dispersions Prepared by γ Radiation. Biomacromolecules 2013, 14, 688–698. [Google Scholar] [CrossRef]
- Abdel-Rashid, R.S.; Helal, D.A.; Omar, M.M.; El Sisi, A.M. Nanogel Loaded with Surfactant Based Nanovesicles for Enhanced Ocular Delivery of Acetazolamide. Int. J. Nanomed. 2019, 14, 2973–2983. [Google Scholar] [CrossRef] [Green Version]
- Nibourg, L.M.; Gelens, E.; de Jong, M.R.; Kuijer, R.; van Kooten, T.G.; Koopmans, S.A. Nanofiber-Based Hydrogels with Extracellular Matrix-Based Synthetic Peptides for the Prevention of Capsular Opacification. Exp. Eye Res. 2016, 143, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Gautam, D.; Pedler, M.G.; Nair, D.P.; Petrash, J.M. Nanogel-Facilitated In-Situ Delivery of a Cataract Inhibitor. Biomolecules 2021, 11, 1150. [Google Scholar] [CrossRef]
- Swilem, A.E.; Elshazly, A.H.M.; Hamed, A.A.; Hegazy, E.-S.A.; Abd El-Rehim, H.A. Nanoscale Poly(Acrylic Acid)-Based Hydrogels Prepared via a Green Single-Step Approach for Application as Low-Viscosity Biomimetic Fluid Tears. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 110, 110726. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.-H.; Jian, H.-J.; Li, Y.-J.; Huang, Y.-F.; Anand, A.; Huang, C.-C.; Lin, H.-J.; Lai, J.-Y. Alleviation of Dry Eye Syndrome with One Dose of Antioxidant, Anti-Inflammatory, and Mucoadhesive Lysine-Carbonized Nanogels. Acta Biomater. 2022, 141, 140–150. [Google Scholar] [CrossRef]
- Davaran, S.; Lotfipour, F.; Sedghipour, N.; Sedghipour, M.R.; Alimohammadi, S.; Salehi, R. Preparation and in Vivo Evaluation of in Situ Gel System as Dual Thermo-/PH-Responsive Nanocarriers for Sustained Ocular Drug Delivery. J. Microencapsul. 2015, 32, 511–519. [Google Scholar]
- Obuobi, S.; Mayandi, V.; Nor, N.A.M.; Lee, B.J.; Lakshminarayanan, R.; Ee, P.L.R. Nucleic Acid Peptide Nanogels for the Treatment of Bacterial Keratitis. Nanoscale 2020, 12, 17411–17425. [Google Scholar] [CrossRef]
- Lin, H.-Y.; Wang, S.-W.; Mao, J.-Y.; Chang, H.-T.; Harroun, S.G.; Lin, H.-J.; Huang, C.-C.; Lai, J.-Y. Carbonized Nanogels for Simultaneous Antibacterial and Antioxidant Treatment of Bacterial Keratitis. Chem. Eng. J. 2021, 411, 128469. [Google Scholar] [CrossRef]
- Kim, H.-J.; Zhang, K.; Moore, L.; Ho, D. Diamond Nanogel-Embedded Contact Lenses Mediate Lysozyme-Dependent Therapeutic Release. ACS Nano 2014, 8, 2998–3005. [Google Scholar] [CrossRef]
- Lee, S.-H.; Kim, H.-J.; Kim, D.-H.; Chang, W.-S.; Vales, T.P.; Kim, J.-W.; Kim, K.-H.; Kim, J.-K. Thermo-Sensitive Nanogel-Laden Bicontinuous Microemulsion Drug-Eluting Contact Lenses. J. Biomed. Mater. Res. B Appl. Biomater. 2019, 107, 1159–1169. [Google Scholar] [CrossRef]
- Wang, Z.; Li, X.; Zhang, X.; Sheng, R.; Lin, Q.; Song, W.; Hao, L. Novel Contact Lenses Embedded with Drug-Loaded Zwitterionic Nanogels for Extended Ophthalmic Drug Delivery. Nanomaterials 2021, 11, 2328. [Google Scholar] [CrossRef]
- Jamard, M.; Hoare, T.; Sheardown, H. Nanogels of Methylcellulose Hydrophobized with N-Tert-Butylacrylamide for Ocular Drug Delivery. Drug Deliv. Transl. Res. 2016, 6, 648–659. [Google Scholar] [CrossRef] [PubMed]
- Zoratto, N.; Forcina, L.; Matassa, R.; Mosca, L.; Familiari, G.; Musarò, A.; Mattei, M.; Coviello, T.; Di Meo, C.; Matricardi, P. Hyaluronan-Cholesterol Nanogels for the Enhancement of the Ocular Delivery of Therapeutics. Pharmaceutics 2021, 13, 1781. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Sun, L.; Fang, S.; Wang, S.; Chen, J.; Xiao, X.; Liu, C. Thermosensitive in Situ Nanogel as Ophthalmic Delivery System of Curcumin: Development, Characterization, in Vitro Permeation and in Vivo Pharmacokinetic Studies. Pharm. Dev. Technol. 2016, 21, 576–582. [Google Scholar] [CrossRef]
- Buosi, F.S.; Alaimo, A.; Di Santo, M.C.; Elías, F.; García Liñares, G.; Acebedo, S.L.; Castañeda Cataña, M.A.; Spagnuolo, C.C.; Lizarraga, L.; Martínez, K.D.; et al. Resveratrol Encapsulation in High Molecular Weight Chitosan-Based Nanogels for Applications in Ocular Treatments: Impact on Human ARPE-19 Culture Cells. Int. J. Biol. Macromol. 2020, 165, 804–821. [Google Scholar] [CrossRef] [PubMed]
- Grimaudo, M.A.; Amato, G.; Carbone, C.; Diaz-Rodriguez, P.; Musumeci, T.; Concheiro, A.; Alvarez-Lorenzo, C.; Puglisi, G. Micelle-Nanogel Platform for Ferulic Acid Ocular Delivery. Int. J. Pharm. 2020, 576, 118986. [Google Scholar] [CrossRef]
- Gooch, N.; Molokhia, S.A.; Condie, R.; Burr, R.M.; Archer, B.; Ambati, B.K.; Wirostko, B. Ocular Drug Delivery for Glaucoma Management. Pharmaceutics 2012, 4, 197–211. [Google Scholar] [CrossRef] [Green Version]
- Tham, Y.-C.; Li, X.; Wong, T.Y.; Quigley, H.A.; Aung, T.; Cheng, C.-Y. Global Prevalence of Glaucoma and Projections of Glaucoma Burden through 2040: A Systematic Review and Meta-Analysis. Ophthalmology 2014, 121, 2081–2090. [Google Scholar] [CrossRef]
- Fea, A.M.; Novarese, C.; Caselgrandi, P.; Boscia, G. Glaucoma Treatment and Hydrogel: Current Insights and State of the Art. Gels 2022, 8, 510. [Google Scholar] [CrossRef]
- Quigley, H.A. 21st Century Glaucoma Care. Eye Lond. Engl. 2019, 33, 254–260. [Google Scholar] [CrossRef] [Green Version]
- Yellepeddi, V.K.; Palakurthi, S. Recent Advances in Topical Ocular Drug Delivery. J. Ocul. Pharmacol. Ther. Off. J. Assoc. Ocul. Pharmacol. Ther. 2016, 32, 67–82. [Google Scholar] [CrossRef]
- Dickmann, L. Ocular Therapeutics: Drug Delivery and Pharmacology. Mol. Pharm. 2016, 13, 2875–2876. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Esteban-Pérez, S.; Andrés-Guerrero, V.; López-Cano, J.J.; Molina-Martínez, I.; Herrero-Vanrell, R.; Bravo-Osuna, I. Gelatin Nanoparticles-HPMC Hybrid System for Effective Ocular Topical Administration of Antihypertensive Agents. Pharmaceutics 2020, 12, 306. [Google Scholar] [CrossRef] [Green Version]
- Bigdeli, A.; Makhmalzadeh, B.S.; Feghhi, M.; SoleimaniBiatiani, E. Cationic Liposomes as Promising Vehicles for Timolol/Brimonidine Combination Ocular Delivery in Glaucoma: Formulation Development and in Vitro/in Vivo Evaluation. Drug Deliv. Transl. Res. 2022, 13, 1035–1047. [Google Scholar] [CrossRef]
- Huang, J.; Peng, T.; Li, Y.; Zhan, Z.; Zeng, Y.; Huang, Y.; Pan, X.; Wu, C.-Y.; Wu, C. Ocular Cubosome Drug Delivery System for Timolol Maleate: Preparation, Characterization, Cytotoxicity, Ex Vivo, and In Vivo Evaluation. AAPS PharmSciTech 2017, 18, 2919–2926. [Google Scholar] [CrossRef] [PubMed]
- Abd El Wahab, L.M.; Essa, E.A.; El Maghraby, G.M.; Arafa, M.F. The Development and Evaluation of Phase Transition Microemulsion for Ocular Delivery of Acetazolamide for Glaucoma Treatment. AAPS PharmSciTech 2022, 24, 1. [Google Scholar] [CrossRef]
- Lee, C.M.; Afshari, N.A. The Global State of Cataract Blindness. Curr. Opin. Ophthalmol. 2017, 28, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Konopińska, J.; Młynarczyk, M.; Dmuchowska, D.A.; Obuchowska, I. Posterior Capsule Opacification: A Review of Experimental Studies. J. Clin. Med. 2021, 10, 2847. [Google Scholar] [CrossRef]
- Thrimawithana, T.R.; Rupenthal, I.D.; Räsch, S.S.; Lim, J.C.; Morton, J.D.; Bunt, C.R. Drug Delivery to the Lens for the Management of Cataracts. Adv. Drug Deliv. Rev. 2018, 126, 185–194. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, C.; Chen, S.; Hu, J.; Shen, L.; Yu, Y. Research Progress Concerning a Novel Intraocular Lens for the Prevention of Posterior Capsular Opacification. Pharmaceutics 2022, 14, 1343. [Google Scholar] [CrossRef]
- Topete, A.; Saramago, B.; Serro, A.P. Intraocular Lenses as Drug Delivery Devices. Int. J. Pharm. 2021, 602, 120613. [Google Scholar] [CrossRef]
- Shen Lee, B.; Toyos, M.; Karpecki, P.; Schiffbauer, J.; Sheppard, J. Selective Pharmacologic Therapies for Dry Eye Disease Treatment: Efficacy, Tolerability, and Safety Data Review from Preclinical Studies and Pivotal Trials. Ophthalmol. Ther. 2022, 11, 1333–1369. [Google Scholar] [CrossRef]
- Pucker, A.D.; Ng, S.M.; Nichols, J.J. Over the Counter (OTC) Artificial Tear Drops for Dry Eye Syndrome. Cochrane Database Syst. Rev. 2016, 2, CD009729. [Google Scholar] [CrossRef] [Green Version]
- Michaelov, E.; McKenna, C.; Ibrahim, P.; Nayeni, M.; Dang, A.; Mather, R. Sjögren’s Syndrome Associated Dry Eye: Impact on Daily Living and Adherence to Therapy. J. Clin. Med. 2022, 11, 2809. [Google Scholar] [CrossRef]
- Seen, S.; Tong, L. Dry Eye Disease and Oxidative Stress. Acta Ophthalmol. 2018, 96, e412–e420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dogru, M.; Kojima, T.; Simsek, C.; Tsubota, K. Potential Role of Oxidative Stress in Ocular Surface Inflammation and Dry Eye Disease. Invest. Ophthalmol. Vis. Sci. 2018, 59, DES163–DES168. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.-J.; Luo, L.-J.; Harroun, S.G.; Wei, S.-C.; Unnikrishnan, B.; Chang, H.-T.; Huang, Y.-F.; Lai, J.-Y.; Huang, C.-C. Synergistically Dual-Functional Nano Eye-Drops for Simultaneous Anti-Inflammatory and Anti-Oxidative Treatment of Dry Eye Disease. Nanoscale 2019, 11, 5580–5594. [Google Scholar] [CrossRef]
- Christensen, I.L.; Sun, Y.-P.; Juzenas, P. Carbon Dots as Antioxidants and Prooxidants. J. Biomed. Nanotechnol. 2011, 7, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Tuft, S.; Somerville, T.F.; Li, J.-P.O.; Neal, T.; De, S.; Horsburgh, M.J.; Fothergill, J.L.; Foulkes, D.; Kaye, S. Bacterial Keratitis: Identifying the Areas of Clinical Uncertainty. Prog. Retin. Eye Res. 2022, 89, 101031. [Google Scholar] [CrossRef] [PubMed]
- Asbell, P.; Stenson, S. Ulcerative Keratitis. Survey of 30 Years’ Laboratory Experience. Arch. Ophthalmol. Chic. Ill 1960 1982, 100, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Liu, Y.; Li, X.; Kebebe, D.; Zhang, B.; Ren, J.; Lu, J.; Li, J.; Du, S.; Liu, Z. Research Progress of In-Situ Gelling Ophthalmic Drug Delivery System. Asian J. Pharm. Sci. 2019, 14, 1–15. [Google Scholar] [CrossRef]
- Khan, N.; Aqil, M.; Imam, S.S.; Ali, A. Development and Evaluation of a Novel in Situ Gel of Sparfloxacin for Sustained Ocular Drug Delivery: In Vitro and Ex Vivo Characterization. Pharm. Dev. Technol. 2015, 20, 662–669. [Google Scholar] [CrossRef]
- Lichtinger, A.; Yeung, S.N.; Kim, P.; Amiran, M.D.; Iovieno, A.; Elbaz, U.; Ku, J.Y.F.; Wolff, R.; Rootman, D.S.; Slomovic, A.R. Shifting Trends in Bacterial Keratitis in Toronto: An 11-Year Review. Ophthalmology 2012, 119, 1785–1790. [Google Scholar] [CrossRef] [PubMed]
- Ni, N.; Nam, E.M.; Hammersmith, K.M.; Nagra, P.K.; Azari, A.A.; Leiby, B.E.; Dai, Y.; Cabrera, F.A.; Ma, J.F.; Lambert, C.E.; et al. Seasonal, Geographic, and Antimicrobial Resistance Patterns in Microbial Keratitis: 4-Year Experience in Eastern Pennsylvania. Cornea 2015, 34, 296–302. [Google Scholar] [CrossRef]
- Andersson, D.I.; Hughes, D.; Kubicek-Sutherland, J.Z. Mechanisms and Consequences of Bacterial Resistance to Antimicrobial Peptides. Drug Resist. Updat. Rev. Comment. Antimicrob. Anticancer Chemother. 2016, 26, 43–57. [Google Scholar] [CrossRef] [PubMed]
- Khara, J.S.; Obuobi, S.; Wang, Y.; Hamilton, M.S.; Robertson, B.D.; Newton, S.M.; Yang, Y.Y.; Langford, P.R.; Ee, P.L.R. Disruption of Drug-Resistant Biofilms Using de Novo Designed Short α-Helical Antimicrobial Peptides with Idealized Facial Amphiphilicity. Acta Biomater. 2017, 57, 103–114. [Google Scholar] [CrossRef]
- Obuobi, S.; Tay, H.K.-L.; Tram, N.D.T.; Selvarajan, V.; Khara, J.S.; Wang, Y.; Ee, P.L.R. Facile and Efficient Encapsulation of Antimicrobial Peptides via Crosslinked DNA Nanostructures and Their Application in Wound Therapy. J. Control. Release Off. J. Control. Release Soc. 2019, 313, 120–130. [Google Scholar] [CrossRef]
- Wang, S.; Yao, J.; Zhou, B.; Yang, J.; Chaudry, M.T.; Wang, M.; Xiao, F.; Li, Y.; Yin, W. Bacteriostatic Effect of Quercetin as an Antibiotic Alternative In Vivo and Its Antibacterial Mechanism In Vitro. J. Food Prot. 2018, 81, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Creech, J.L.; Chauhan, A.; Radke, C.J. Dispersive Mixing in the Posterior Tear Film Under a Soft Contact Lens. Ind. Eng. Chem. Res. 2001, 40, 3015–3026. [Google Scholar] [CrossRef]
- Jung, H.J.; Abou-Jaoude, M.; Carbia, B.E.; Plummer, C.; Chauhan, A. Glaucoma Therapy by Extended Release of Timolol from Nanoparticle Loaded Silicone-Hydrogel Contact Lenses. J. Control. Release Off. J. Control. Release Soc. 2013, 165, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Fan, X.; Torres-Luna, C.; Azadi, M.; Domszy, R.; Hu, N.; Yang, A.; David, A.E. Evaluation of Commercial Soft Contact Lenses for Ocular Drug Delivery: A Review. Acta Biomater. 2020, 115, 60–74. [Google Scholar] [CrossRef]
- Wong, A.; Fallon, M.; Celiksoy, V.; Ferla, S.; Varricchio, C.; Whitaker, D.; Quantock, A.J.; Heard, C.M. A Composite System Based upon Hydroxypropyl Cyclodextrins and Soft Hydrogel Contact Lenses for the Delivery of Therapeutic Doses of Econazole to the Cornea, In Vitro. Pharmaceutics 2022, 14, 1631. [Google Scholar] [CrossRef]
- Li, C.-C.; Abrahamson, M.; Kapoor, Y.; Chauhan, A. Timolol Transport from Microemulsions Trapped in HEMA Gels. J. Colloid Interface Sci. 2007, 315, 297–306. [Google Scholar] [CrossRef]
- Lu, C.; Yoganathan, R.B.; Kociolek, M.; Allen, C. Hydrogel Containing Silica Shell Cross-Linked Micelles for Ocular Drug Delivery. J. Pharm. Sci. 2013, 102, 627–637. [Google Scholar] [CrossRef]
- Gulsen, D.; Li, C.-C.; Chauhan, A. Dispersion of DMPC Liposomes in Contact Lenses for Ophthalmic Drug Delivery. Curr. Eye Res. 2005, 30, 1071–1080. [Google Scholar] [CrossRef] [PubMed]
- Dixon, P.; Fentzke, R.C.; Bhattacharya, A.; Konar, A.; Hazra, S.; Chauhan, A. In Vitro Drug Release and in Vivo Safety of Vitamin E and Cysteamine Loaded Contact Lenses. Int. J. Pharm. 2018, 544, 380–391. [Google Scholar] [CrossRef] [PubMed]
- Chu, Z.; Xue, C.; Shao, K.; Xiang, L.; Zhao, X.; Chen, C.; Pan, J.; Lin, D. Photonic Crystal-Embedded Molecularly Imprinted Contact Lenses for Controlled Drug Release. ACS Appl. Bio Mater. 2022, 5, 243–251. [Google Scholar] [CrossRef]
- Maulvi, F.A.; Soni, T.G.; Shah, D.O. A Review on Therapeutic Contact Lenses for Ocular Drug Delivery. Drug Deliv. 2016, 23, 3017–3026. [Google Scholar] [CrossRef] [PubMed]
- Lanier, O.L.; Christopher, K.G.; Macoon, R.M.; Yu, Y.; Sekar, P.; Chauhan, A. Commercialization Challenges for Drug Eluting Contact Lenses. Expert Opin. Drug Deliv. 2020, 17, 1133–1149. [Google Scholar] [CrossRef]
- Jung, H.J.; Chauhan, A. Temperature Sensitive Contact Lenses for Triggered Ophthalmic Drug Delivery. Biomaterials 2012, 33, 2289–2300. [Google Scholar] [CrossRef]
- Lee, S.-H.; Shin, K.-S.; Kim, J.-W.; Kang, J.-Y.; Kim, J.-K. Stimulus-Responsive Contact Lens for IOP Measurement or Temperature-Triggered Drug Release. Transl. Vis. Sci. Technol. 2020, 9, 1. [Google Scholar] [CrossRef] [Green Version]
- Men, Y.; Peng, S.; Yang, P.; Jiang, Q.; Zhang, Y.; Shen, B.; Dong, P.; Pang, Z.; Yang, W. Biodegradable Zwitterionic Nanogels with Long Circulation for Antitumor Drug Delivery. ACS Appl. Mater. Interfaces 2018, 10, 23509–23521. [Google Scholar] [CrossRef] [PubMed]
- Lei, M.; Zhang, W.; Yi, C.; Yan, L.; Tian, Y. Zwitterionic Nanogels with Temperature Sensitivity and Redox-Degradability for Controlled Drug Release. Colloids Surf. B Biointerfaces 2021, 206, 111959. [Google Scholar] [CrossRef] [PubMed]
- Bayer, I.S. Hyaluronic Acid and Controlled Release: A Review. Molecules 2020, 25, 2649. [Google Scholar] [CrossRef]
- Bongiovì, F.; Di Prima, G.; Palumbo, F.S.; Licciardi, M.; Pitarresi, G.; Giammona, G. Hyaluronic Acid-Based Micelles as Ocular Platform to Modulate the Loading, Release, and Corneal Permeation of Corticosteroids. Macromol. Biosci. 2017, 17, 1700261. [Google Scholar] [CrossRef]
- Kao, Y.-W.; Hsu, S.-K.; Chen, J.Y.-F.; Lin, I.-L.; Chen, K.-J.; Lee, P.-Y.; Ng, H.-S.; Chiu, C.-C.; Cheng, K.-C. Curcumin Metabolite Tetrahydrocurcumin in the Treatment of Eye Diseases. Int. J. Mol. Sci. 2020, 22, 212. [Google Scholar] [CrossRef]
- Delmas, D.; Cornebise, C.; Courtaut, F.; Xiao, J.; Aires, V. New Highlights of Resveratrol: A Review of Properties against Ocular Diseases. Int. J. Mol. Sci. 2021, 22, 1295. [Google Scholar] [CrossRef]
- Romeo, A.; Musumeci, T.; Carbone, C.; Bonaccorso, A.; Corvo, S.; Lupo, G.; Anfuso, C.D.; Puglisi, G.; Pignatello, R. Ferulic Acid-Loaded Polymeric Nanoparticles for Potential Ocular Delivery. Pharmaceutics 2021, 13, 687. [Google Scholar] [CrossRef] [PubMed]
- Razavi, M.S.; Ebrahimnejad, P.; Fatahi, Y.; D’Emanuele, A.; Dinarvand, R. Recent Developments of Nanostructures for the Ocular Delivery of Natural Compounds. Front. Chem. 2022, 10, 850757. [Google Scholar] [CrossRef]
- Grimaudo, M.A.; Pescina, S.; Padula, C.; Santi, P.; Concheiro, A.; Alvarez-Lorenzo, C.; Nicoli, S. Topical Application of Polymeric Nanomicelles in Ophthalmology: A Review on Research Efforts for the Noninvasive Delivery of Ocular Therapeutics. Expert Opin. Drug Deliv. 2019, 16, 397–413. [Google Scholar] [CrossRef]



| Author/Year | Applications | Polymers | Drug-Loaded | Preparations |
|---|---|---|---|---|
| Ilka/2018 [77] | Glaucoma | Chitosan, Sodium alginate | Timolol Maleate | Pregelation method |
| Cuggino/2021 [78] | Glaucoma | N-Isopropylacrylamide, Acrylic acid | Timolol Maleate | Free-radical polymerization |
| Abd El-Rehim/2013 [79] | Glaucoma | Polyvinylpyrrolidone, Acrylic acid | Pilocarpine | γ radiation-induced polymerization |
| Abdel-Rashid/2019 [80] | Glaucoma | Chitosan, Tripolyphosphate | Acetazolamide | Ionic-gelation method |
| Nibourg/2016 [81] | Cataract | Nanofibers, Synthetic peptides | / | Chemical crosslinking/selfassembly |
| Gautam/2021 [82] | Cataract | Acrylic acid, MethAcrylic acid | Sorbinil | Photo-induced aggregation |
| Swilem/2020 [83] | Dry eye syndrome | Polyvinylpyrrolidone, Acrylic acid | / | Ionizing-radiation method |
| Lin/2022 [84] | Dry eye syndrome | Lysine hydrochloride | / | Pyrolysis |
| Davaran/2015 [85] | Bacterial keratitis | N-Isopropylacrylamide, Methacrylic acid, Vinylpyrrolidone | Ciprofloxacin | Free-radical polymerization |
| Obuobi/2020 [86] | Bacterial keratitis | Deoxyribonucleic acid, L12 antimicrobial peptides | L12 antimicrobial peptides | Physical crosslinking/selfassembly |
| Lin/2021 [87] | Bacterial keratitis | Quercetin, Lysine | / | Pyrolysis |
| Kim/2014 [88] | Contact lenses | Nanodiamond-Polyethyleneimine, Chitosan | Timolol Maleate | Pyrolysis |
| Lee/2019 [89] | Contact lenses | N-Isopropylacrylamide, N,N′-methylenebis (acrylamide) | Timolol Maleate | Emulsion polymerization |
| Wang/2021 [90] | Contact lenses | Hydroxyethyl methacrylate, N-vinyl pyrrolidinone | Levofloxacin | Reflux-precipitation polymerization |
| Jamard/2016 [91] | Ocular Delivery | N-tert-butylacrylamide, Methylcellulose | Dexamethasone | Chemical crosslinking/selfassembly |
| Zoratto/2021 [92] | Ocular Delivery | Hyaluronan, Cholesterol | Tobramycin/Diclofenac sodium salt/Dexamethasone/Piroxicam | Chemical crosslinking/selfassembly |
| Liu/2016 [93] | Ocular Delivery | Cationic nanostructured lipid carriers, Poloxamer | Curcumin | Pregelation method |
| Buosi/2020 [94] | Ocular Delivery | High molecular weight chitosan, Sodium tripolyphosphate | Resveratrol | Ionic-gelation method |
| Grimaudo/2020 [95] | Ocular Delivery | Hyaluronan, ε-polylysine | Ferulic acid | Ionic-gelation method |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, Y.; Tao, Q.; Xie, J.; Lu, L.; Xie, X.; Zhang, Y.; Jin, Y. Advances in Nanogels for Topical Drug Delivery in Ocular Diseases. Gels 2023, 9, 292. https://doi.org/10.3390/gels9040292
Wu Y, Tao Q, Xie J, Lu L, Xie X, Zhang Y, Jin Y. Advances in Nanogels for Topical Drug Delivery in Ocular Diseases. Gels. 2023; 9(4):292. https://doi.org/10.3390/gels9040292
Chicago/Turabian StyleWu, Yongkang, Qing Tao, Jing Xie, Lili Lu, Xiuli Xie, Yang Zhang, and Yong Jin. 2023. "Advances in Nanogels for Topical Drug Delivery in Ocular Diseases" Gels 9, no. 4: 292. https://doi.org/10.3390/gels9040292
APA StyleWu, Y., Tao, Q., Xie, J., Lu, L., Xie, X., Zhang, Y., & Jin, Y. (2023). Advances in Nanogels for Topical Drug Delivery in Ocular Diseases. Gels, 9(4), 292. https://doi.org/10.3390/gels9040292






