Formulation and Evaluation of Diclofenac Potassium Gel in Sports Injuries with and without Phonophoresis
Abstract
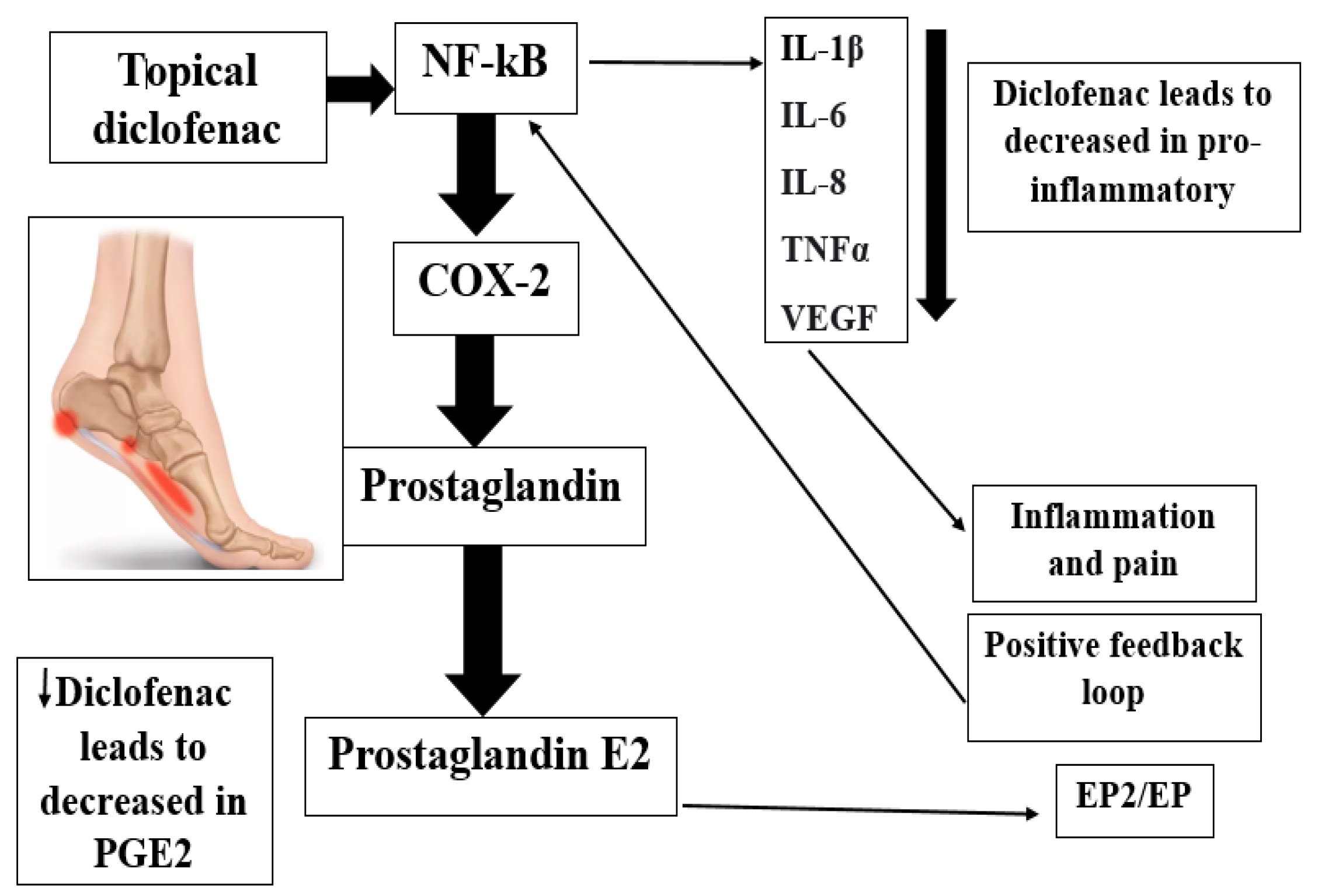
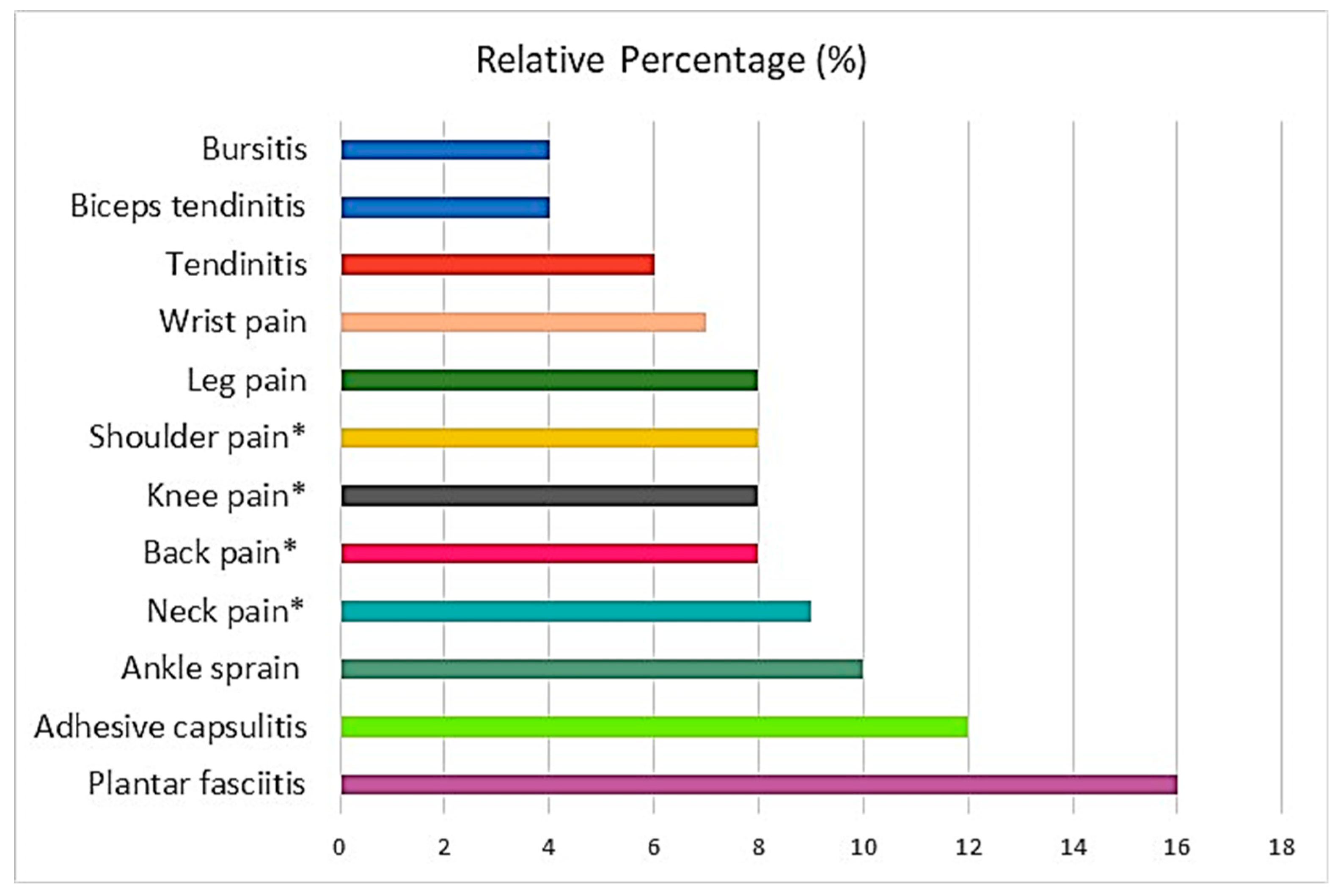
1. Introduction
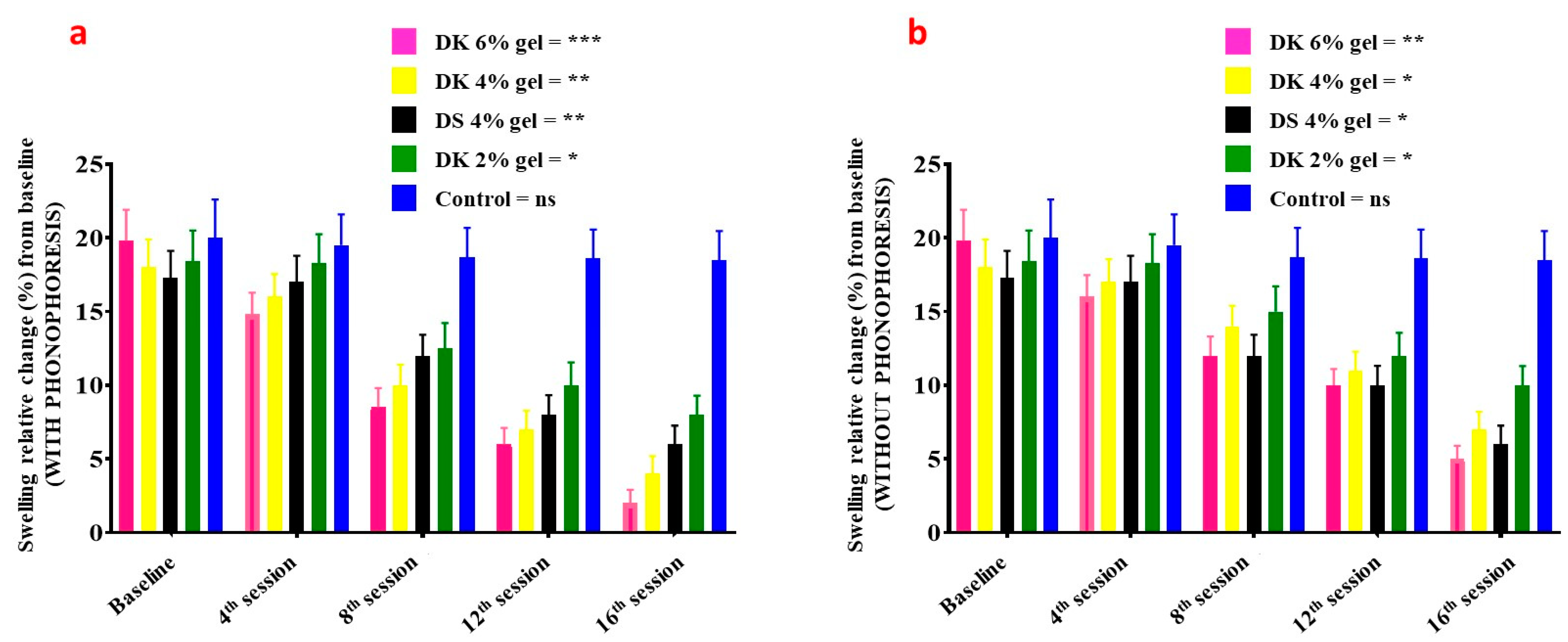
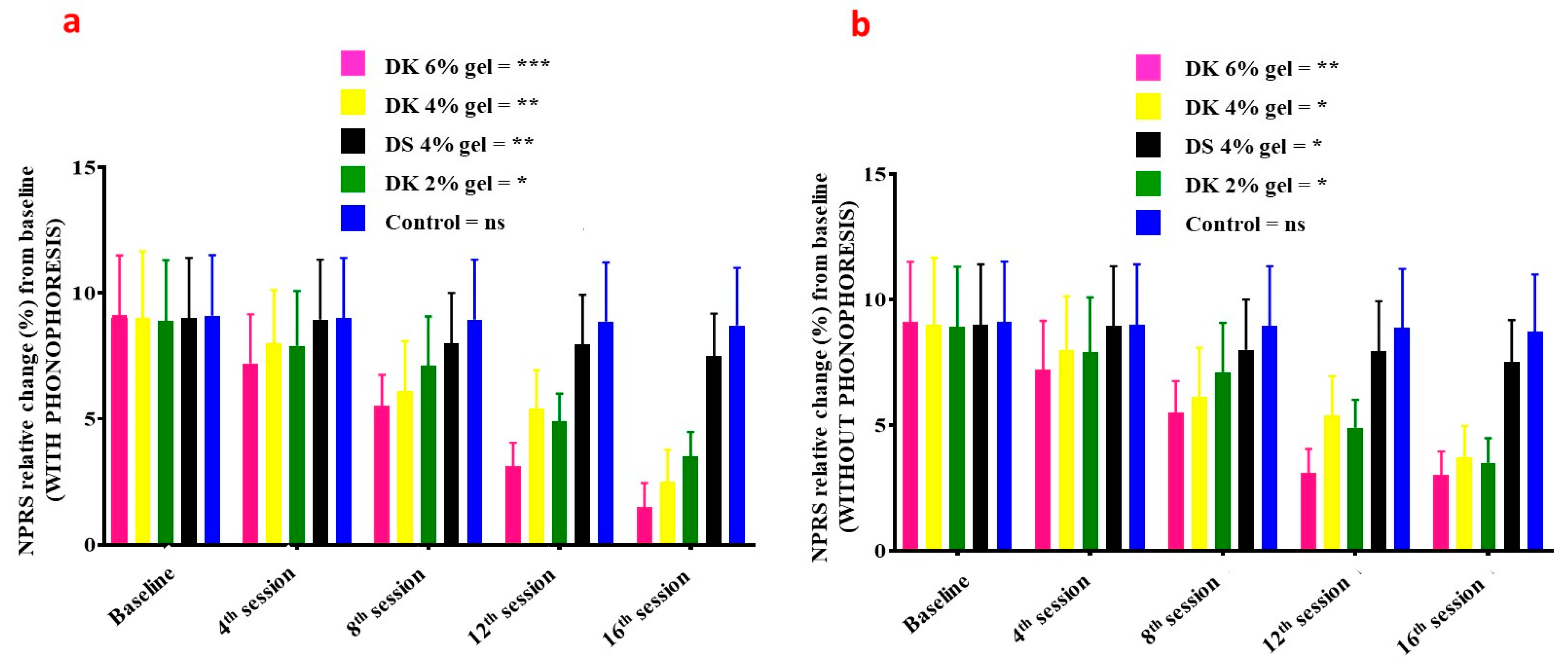
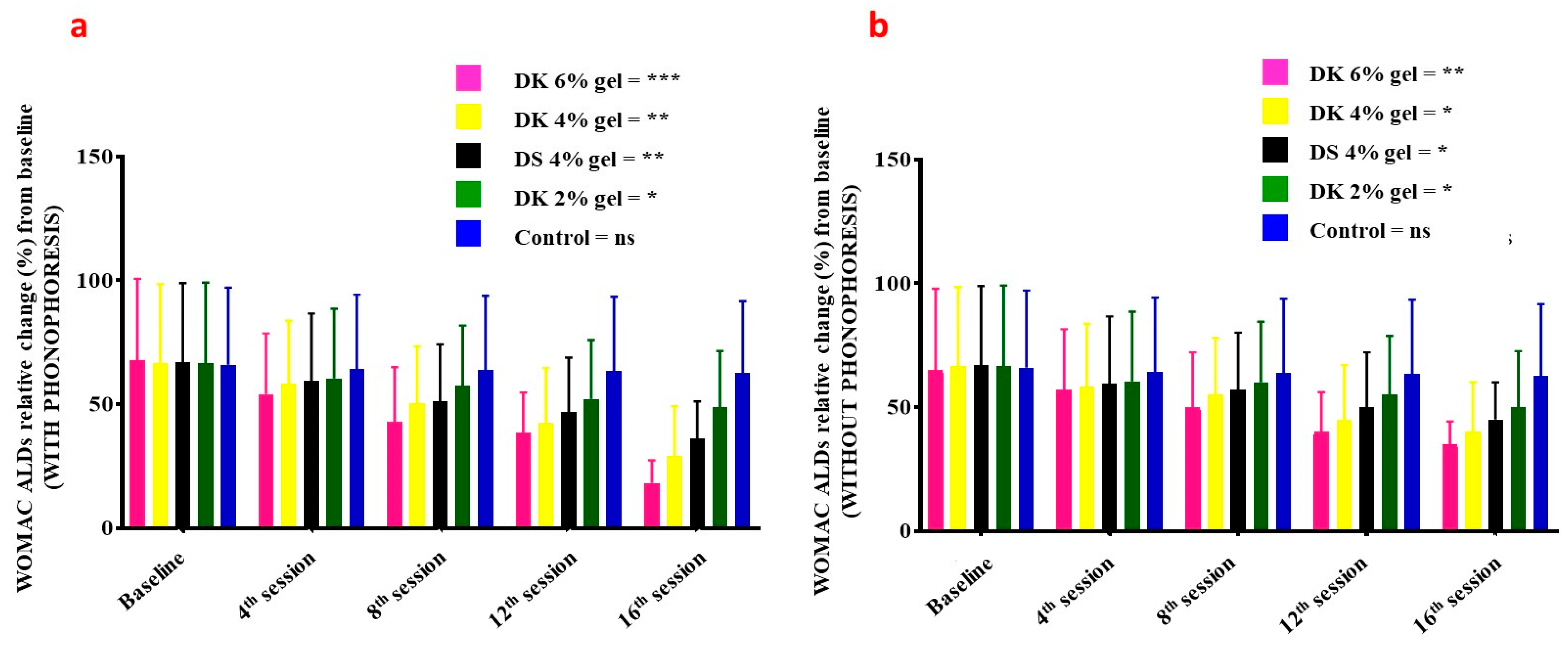
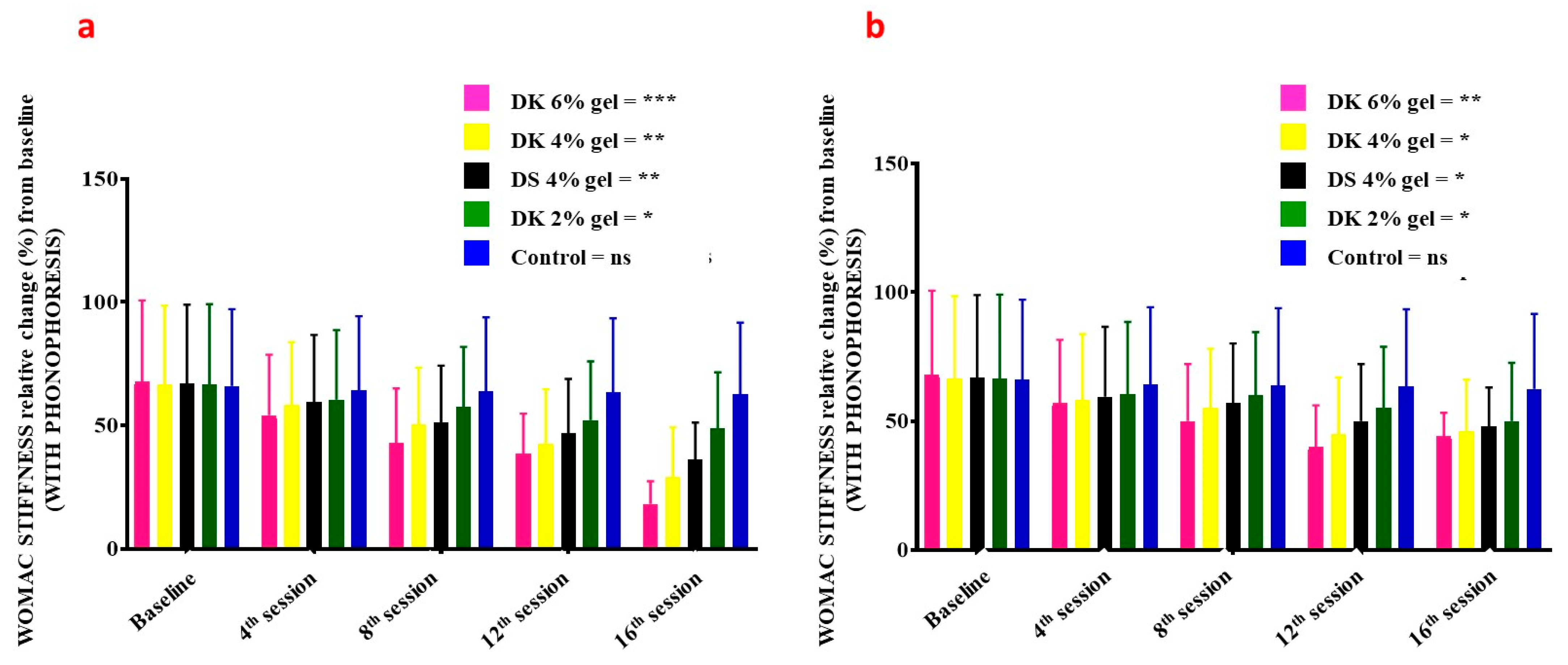
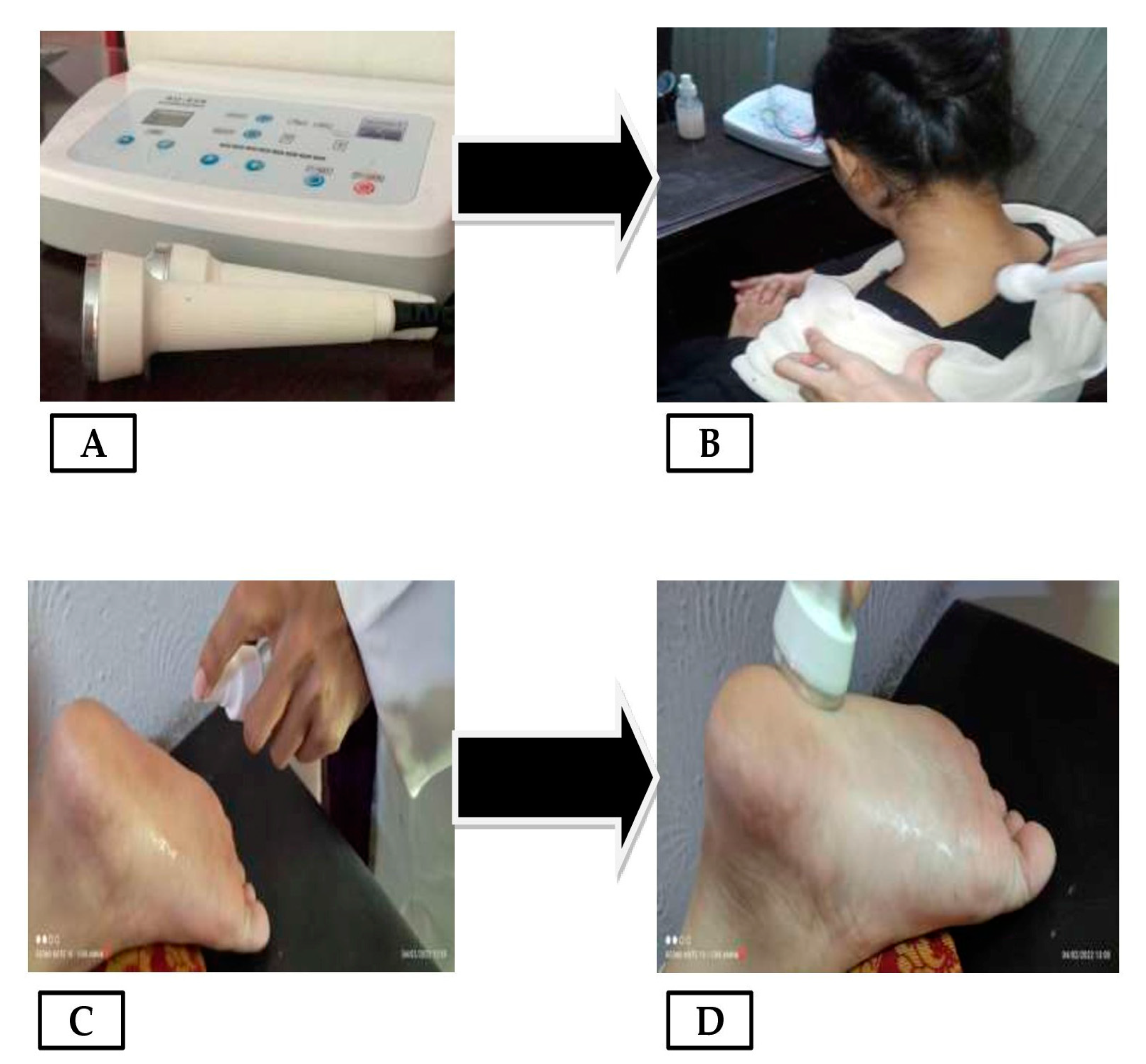
2. Results and Discussion
3. Conclusions
4. Materials and Methods
4.1. Study, Patients, and Ethics
4.2. Statistical Analysis
4.3. Preparation of Diclofenac Potassium Gel
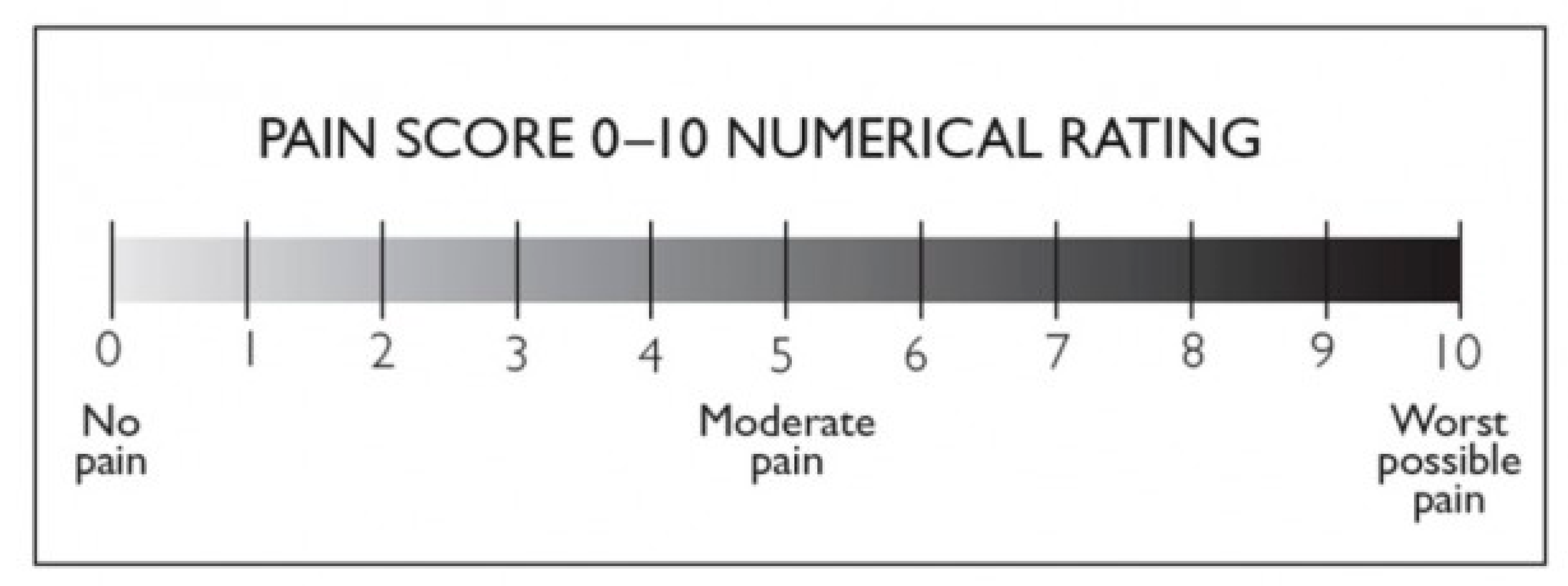
4.4. Numerical Pain Rating Scale
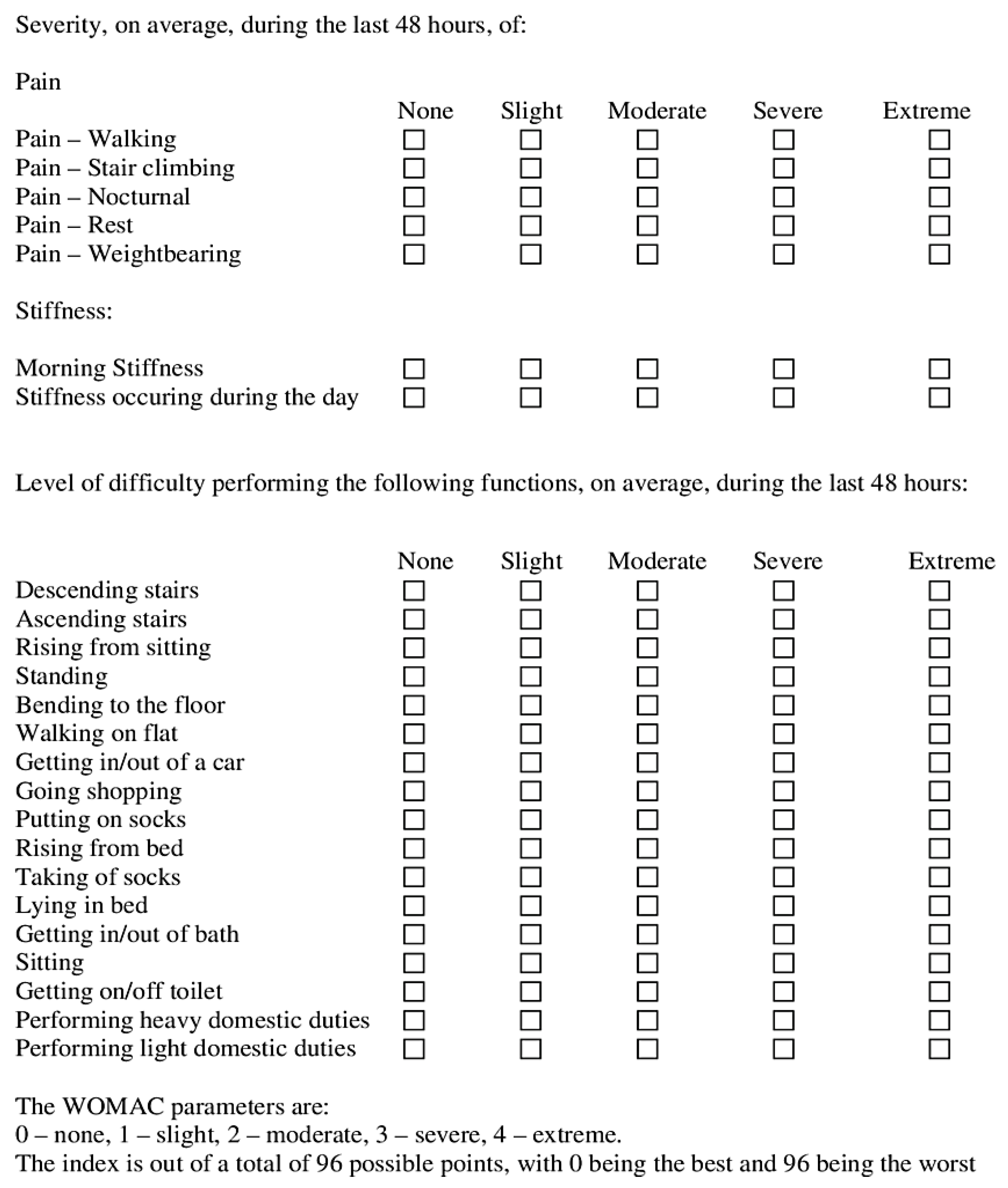
4.5. WOMAC Index
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ivins, D. Acute ankle sprain: An update. Am. Fam. Physician 2006, 74, 1714–1720. [Google Scholar] [PubMed]
- Kerkhoffs, G.M.; Rowe, B.H.; Assendelft, W.J.; Kelly, P.A.; Struijs, C.N. Immobilisation and functional treatment for acute lateral ankle ligament injuries in adults. Cochrane Database Syst. Rev. 2002, 3, CD003762. [Google Scholar] [CrossRef]
- Zacher, J.; Altman, R.; Bellamy, N.; Brühlmann, J.P.; Da Silva, E.; Huskisson, R.S. Topical diclofenac and its role in pain and inflammation: An evidence-based review. Curr. Med. Res. Opinion 2008, 24, 925–950. [Google Scholar] [CrossRef]
- Osteoarthritis: The care and management of osteoarthritis in adults. Inst. Clin. Excell. Clin. Guidel. 2008. Available online: http://guidance.nice.org.uk/CG59 (accessed on 24 June 2013).
- Massey, T.; Derry, S.; Moore, R.A.; McQuay, H.J. Topical NSAIDs for acute pain in adults. Cochrane Database Syst. Rev. 2010, 16, CD007402. [Google Scholar] [CrossRef]
- Brune, K. Persistence of NSAIDs at effect sites and rapid disappearance from side-effect compartments contributes to tolerability. Curr. Med. Res. Opin. 2007, 23, 2985–2995. [Google Scholar] [CrossRef] [PubMed]
- Bandolier: Evidence-Based Health Care. Topical Analgesics: A Review Of reviews and a Bit of Perspective. 2005. Available online: https://www.medi-cine.ox.ac.uk/bandolier/Extraforbando/Topextra3.pdf (accessed on 20 January 2013).
- Davies, N.M.; Anderson, K.E. Clinical pharmacokinetics of diclofenac. Therapeutic insights and pitfalls. Clin. Pharmacokinet 1997, 33, 184–213. [Google Scholar] [CrossRef] [PubMed]
- Riess, W.; Schmid, K.; Bott, L.; Kobayashi, J.K.; Moppert, W.; Schneider, A.; Sioufi, A.; Strusberg, M. The percutaneous absorption of diclofenac. Arzneim. Schung. 1986, 36, 1092–1096. [Google Scholar]
- Bjordal, M.; Ljunggren, A.E.; Klovning, A.; Moppert, J.; Schneider, W.; Sioufi, A.; Strusberg, A.; Tomasi, M. Non-steroidal anti-inflammatory drugs, including cyclo-oxygenase-2 inhibitors, in osteoarthritic knee pain: Meta-analysis of randomised placebo-controlled trials. BMJ 2004, 329, 1317. [Google Scholar] [CrossRef]
- Jordan, K.; Arden, N.; Doherty, M.; Bannwarth, B.; Bijlsma, J.W.J.; Dieppe, P.; Gunther, K.; Hauselmann, H.; Herrero-Beaumont, G.; Kaklamanis, P.; et al. EULAR recommendations 2003: An evidence-based approach to the management of knee osteoarthritis: Report of a task force of the standing committee for international clinical studies including therapeutic trials (ESCISIT). Ann. Rheum. Dis. 2003, 62, 1145–1155. [Google Scholar] [CrossRef]
- Mason, L.; Moore, R.A.; Edwards, J.E.; Moore, A.R. Topical NSAIDs for acute pain: A meta- analysis. BMC Fam. Pract. 2004, 5, 10. [Google Scholar] [CrossRef] [PubMed]
- Moore, R.A.; Tramer, M.R.; Carroll, D.; Wiffen, P.J.; McQuay, H.J. Quantitative systematic review of topically applied non-steroidal anti-inflammatory drugs. BMJ 1998, 316, 333–338. [Google Scholar] [CrossRef] [PubMed]
- van Tulder, M.W.; Scholten, R.J.; Koes, B.W. Non-steroidal anti-inflammatory drugs for low-back pain. Cochrane Database Syst. Rev. 2000, 2, 31. [Google Scholar] [CrossRef]
- Cordero, J.A.; Alarcon, L.; Escribano, E.; Obach, R.; Domenech, J. A comparative study of the transdermal penetration of a series of nonsteroidal antiinflammatory drugs. J. Pharm. Sci. 1997, 86, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Brunner, M.; Dehghanyar, P.; Seigfried, B.; Wolfgang, M.; Georg, M.; Markus, M. Favourable dermal penetration of diclofenac after administration to the skin using a novel spray gel formulation. Br. J. Clin. Pharmacol. 2005, 60, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Lionberger, D.R.; Joussellin, E.; Lanzarotti, A.; Yanchick, J.; Magelli, M. Diclofenac epolamine topical patch relieves pain associated with ankle sprain. J. Pain Res. 2011, 4, 47–53. [Google Scholar] [PubMed]
- van Rijn, R.M.; van Os, A.G.; Bernsen, R.M.; Luijsterburg, P.A.; Koes, B.W.; Bierma-Zeinstra, S.M. What is the clinical course of acute ankle sprains? A systematic literature review. Am. J. Med. 2008, 121, 324–331.e6. [Google Scholar] [CrossRef] [PubMed]
- Purves, R.D. Optimum numerical integration methods for estimation of area-under-the- curve (AUC) and area-under-the-moment- curve (AUMC). J. Pharmacokinet Biopharm. 1992, 20, 211–226. [Google Scholar] [CrossRef]
- Schermer, R. Topical therapy for sprains of the ankle joint. A double-blind study of the efficacy of diclofenac diethylammonium in an emulsion-gel. Wehrmed Mschr. 1991, 9, 415–419. [Google Scholar]
- Yamaguchi, S.; Terahara, T.; Okawa, K.; Inakura, H. A multicenter, randomized, double-blind, placebo-controlled, comparative study to evaluate the efficacy and safety of newly developed diclofenac patches in patients with cancer pain. Pain 2021. [Google Scholar] [CrossRef]
- Benaouda, F.; Inacio, R.; Lim, C.H.; Park, H.; Pitcher, T.; Alhnan, M.A.; Aly, M.M.S.; Al-Jamal, K.T.; Chan, K.L.; Gala, R.P.; et al. Needleless administration of advanced therapies into the skin via the appendages using a hypobaric patch. Proc. Natl. Acad. Sci. USA 2022, 119, e2120340119. [Google Scholar] [CrossRef] [PubMed]
- Tabosa, M.A.M.; Cordery, S.F.; Jane White, K.A.; Bunge, A.L.; Guy, R.H.; Delgado-Charro, M.B. Skin pharmacokinetics of diclofenac and co-delivered functional excipients. Int. J. Pharm. 2022, 612, 121469. [Google Scholar]
- Ahmad, M.; Iqbal, M.; Murtaza, G. Comparison of bioavailability and pharmacokinetics of diclofenac sodium and diclofenac potassium in normal and dehydrated rabbits. Yao Xue Xue Bao 2009, 44, 80–84. [Google Scholar] [PubMed]
- Hinz, B.; Chevts, J.; Renner, B.; Wuttke, H.; Rau, T.; Schmidt, A.; Szelenyi, I.; Brune, K.; Werner, U. Bioavailability of diclofenac potassium at low doses. Br. J. Clin. Pharmacol. 2005, 59, 80–84. [Google Scholar] [CrossRef]
- Chuasuwan, B.; Binjesoh, V.; Polli, J.E.; Zhang, H.; Amidon, G.L.; Junginger, H.E.; Midha, K.K.; Shah, V.P.; Stavchansky, S.; Dressman, J.B.; et al. Biowaiver monographs for immediate release solid oral dosage forms: Diclofenac sodium and diclofenac potassium. J. Pharm. Sci. 2009, 98, 1209–1219. [Google Scholar] [CrossRef] [PubMed]
- LEHMANN, J.F. The biophysical basis of biologic ultrasonic reactions with special reference to ultrasonic therapy. Arch. Phys. Med. Rehabil. 1953, 34, 39–52. [Google Scholar]
- Kamel, M.; Eid, H.; Mansour, R.J.T. Ultrasound detection of heel enthesitis: A comparison with magnetic resonance imaging. J. Rheumatol. 2003, 30, 774–778. [Google Scholar]
- Argerakis, N.G.; Positano, R.G.; Positano, R.C.; Boccio, A.K.; Adler, R.S.; Saboeiro, G.R.; Joshua, S.D. Ultrasound diagnosis and evaluation of plantar heel pain. J. Am. Podiatr. Med. Assoc. 2015, 105, 135–140. [Google Scholar] [CrossRef]
- McNally, E.G.; Shetty, S. Plantar fascia: Imaging diagnosis and guided treatment. Semin. Musculoskelet Radiol. 2010, 14, 334–343. [Google Scholar] [CrossRef]
- Cheing, G.; Chang, H.; Lo, S.K.J.S.W. A comparison of the effectiveness of extracorporeal shock wave and ultrasound therapy in the management of heel pain. Medicine 2007, 17, 195–201. [Google Scholar] [CrossRef]
- Babatunde, O.O.; Legha, A.; Littlewood, C.; Chesterton, L.S.; Thomas, M.J.; Menz, H.B.; Danielle, W.; Edward, R. Comparative effectiveness of treatment options for plantar heel pain: A systematic review with network meta-analysis. Meta-Analyst 2019, 53, 182–194. [Google Scholar] [CrossRef]
- Crawford, F.; Snaith, M.J. How effective is therapeutic ultrasound in the treatment of heel pain? Ann. Rheum. Dis. 1996, 55, 265–267. [Google Scholar] [CrossRef] [PubMed]
- Shanks, P.; Curran, M.; Fletcher, P.; Thompson, R.J.T.F. The effectiveness of therapeutic ultrasound for musculoskeletal conditions of the lower limb: A literature review. Foot 2010, 20, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Katzap, Y.; Haidukov, M.; Berland, O.M.; Itzhak, R.B.; Kalichman, L.J. Additive effect of therapeutic ultrasound in the treatment of plantar fasciitis: A randomized controlled trial. Randomized Control Trial 2018, 48, 847–855. [Google Scholar] [CrossRef]
- Dorji, K.; Graham, N.; Macedo, L.; Gravesande, J.; Goldsmith, C.H.; Gelley, G.; Rice, M.; Solomon, P. The effect of ultrasound or phonophoresis as an adjuvant treatment for non-specific neck pain: Systematic review of randomised controlled trials. Disabil Rehabil. 2002, 44, 2968–2974. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.L.; Smith, N.B.; Bailey, M.R.; Czarnota, G.J.; Hynynen, K.; Makin, I.R.; Bioeffects Committee of the American Institute of Ultrasound in Medicine. Overview of therapeutic ultrasound applications and safety considerations. J. Ultrasound Med. 2012, 31, 623–634. [Google Scholar] [CrossRef]
- Ahn, J.H.; Lee, C.W.; Park, C.; Kim, Y.C. Ultrasonographic examination of plantar fasciitis: A comparison of patient positions during examination. J. Foot Ankle Res. 2016, 9, 38. [Google Scholar] [CrossRef]
- Cameron, M.H.; Monro, L.G. Relative transmission of ultrasound by media customarily used for phonophoresis. Phys. Ther. 1992, 72, 142–148. [Google Scholar] [CrossRef]
- D'vaz, A.; Ostor, A.J.; Speed, C.; Jenner, J.; Bradley, M.; Prevost, A.; Hazleman, B.L. Pulsed low-intensity ultrasound therapy for chronic lateral epicondylitis: A randomized controlled trial. Bmj 2006, 45, 566–570. [Google Scholar] [CrossRef]
- Tolu, S.; Köse, M.M.; Korkmaz, M.C.; Üşen, A.; Rezvani, A. Comparison of the Efficacy of Different Concentrations of Diclofenac Sodium Phonophoresis (1.16% vs 2.32%) in Patients with Knee Osteoarthritis: A Randomized Double-Blind Controlled Trial. Acta Chir. Orthop. Traumatol. Cech. 2021, 88, 117–123. [Google Scholar]
- Wang, X.; Dan, W.; Wenzhao, L.; Lei, Y. Emerging biomaterials for reproductive medicine. Eng. Regen. 2021, 2, 230–245. [Google Scholar] [CrossRef]
- Khan, Z.U.; Razzaq, A.; Khan, A.; Rehman, N.U.; Khan, H.; Khan, T.; Khan, A.U.; Althobaiti, N.A.; Menaa, F.; Iqbal, H.; et al. Physicochemical Characterizations and Pharmacokinetic Evaluation of Pentazocine Solid Lipid Nanoparticles against Inflammatory Pain Model. Pharmaceutics 2022, 14, 409. [Google Scholar] [CrossRef] [PubMed]
- Sa'adon, S.; Ansari, M.N.M.; Razak, S.I.A.; Yusof, A.H.M.; Faudzi, A.A.M.; Sagadevan, S.; Nayan, N.H.M.; Anand, J.S.; Amin, K.A.M. Electrospun Nanofiber and Cryogel of Polyvinyl Alcohol Transdermal Patch Containing Diclofenac Sodium: Preparation, Characterization, and In Vitro Release Studies. Pharmaceutics 2021, 13, 1900. [Google Scholar] [CrossRef] [PubMed]
- Branco, A.C.; Oliveira, A.S.; Monteiro, I.; Nolasco, P.; Silva, D.C.; Figueiredo-Pina, C.G.; Colaço, R.; Serro, A.P. PVA-Based Hydrogels Loaded with Diclofenac for Cartilage Replacement. Gels 2022, 8, 143. [Google Scholar] [CrossRef] [PubMed]
- Petersen, B.; Rovati, S. Diclofenac epolamine (Flector®) patch. Clin. Drug Investig. 2009, 29, 1–9. [Google Scholar] [CrossRef]
- Hu, Y.; Hui, Z.; Hao, W.; Hong, C.; Jiaying, C.; Xiaoyan, C.; Lin, X.; Huan, W.; Renjie, C. Scaffolds with Anisotropic Structure for Neural Tissue Engineering. Eng. Regen. 2022, 3, 154–162. [Google Scholar] [CrossRef]
- Yang, L.; Lingyu, S.; Han, Z.; Feika, B.; Yuanjin, Z. Ice-inspired lubricated drug delivery particles from microfluidic electrospray for osteoarthritis treatment. ACS Nano 2021, 12, 20600–20606. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Zhu, Y.; Xing, C.; Li, S.; Bao, Z.; Lei, L.; Lin, D.; Wang, Y.; Chen, H.; Xu, X. An injectable thermosensitive hydrogel for dual delivery of diclofenac and Avastin® to effectively suppress inflammatory corneal neovascularization. Int. J. Pharm. 2022, 625, 122081. [Google Scholar] [CrossRef]
- Borkowf, C.B. A New Method for Approximating the Asymptotic Variance of Spearman’s Rank Correlation. Stat. Sin. 1999, 9, 535–558. [Google Scholar]
- Lin, J.; Fessell, D.P.; Jacobson, J.A.; Weadock, W.J.; Hayes, C.W.J. An illustrated tutorial of musculoskeletal sonography: Part 3, lower extremity. AJR Am. J. Roentgenol. 2000, 175, 1313–1321. [Google Scholar] [CrossRef]
- Provenzano, A.H.; Åström, E.; Löwing, K. Exploring pain interference and self-perceived health status in children with osteogenesis imperfecta—A cross-sectional study. BMC Musculoskelet Disord. 2022, 23, 876. [Google Scholar] [CrossRef]
- Li, L.; Zeng, Z.; Zhang, H.; Xu, L.; Lin, Y.; Zhang, Y.; Deng, M.; Fan, P. Different Prevalence of Neuropathic Pain, and Risk Factors in Patients with Knee Osteoarthritis at Stages of Outpatient, Awaiting and after Total Knee Arthroplasty. Orthop Surg. 2020. Epub ahead of print. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bukhari, K.A.; Khan, I.A.; Ishaq, S.; Iqbal, M.O.; Alqahtani, A.M.; Alqahtani, T.; Menaa, F. Formulation and Evaluation of Diclofenac Potassium Gel in Sports Injuries with and without Phonophoresis. Gels 2022, 8, 612. https://doi.org/10.3390/gels8100612
Bukhari KA, Khan IA, Ishaq S, Iqbal MO, Alqahtani AM, Alqahtani T, Menaa F. Formulation and Evaluation of Diclofenac Potassium Gel in Sports Injuries with and without Phonophoresis. Gels. 2022; 8(10):612. https://doi.org/10.3390/gels8100612
Chicago/Turabian StyleBukhari, Komal Ammar, Imran Ahmad Khan, Shahid Ishaq, Muhammad Omer Iqbal, Ali M. Alqahtani, Taha Alqahtani, and Farid Menaa. 2022. "Formulation and Evaluation of Diclofenac Potassium Gel in Sports Injuries with and without Phonophoresis" Gels 8, no. 10: 612. https://doi.org/10.3390/gels8100612
APA StyleBukhari, K. A., Khan, I. A., Ishaq, S., Iqbal, M. O., Alqahtani, A. M., Alqahtani, T., & Menaa, F. (2022). Formulation and Evaluation of Diclofenac Potassium Gel in Sports Injuries with and without Phonophoresis. Gels, 8(10), 612. https://doi.org/10.3390/gels8100612








