Dental Whitening Gels: Strengths and Weaknesses of an Increasingly Used Method
Abstract
1. Introduction
2. Results
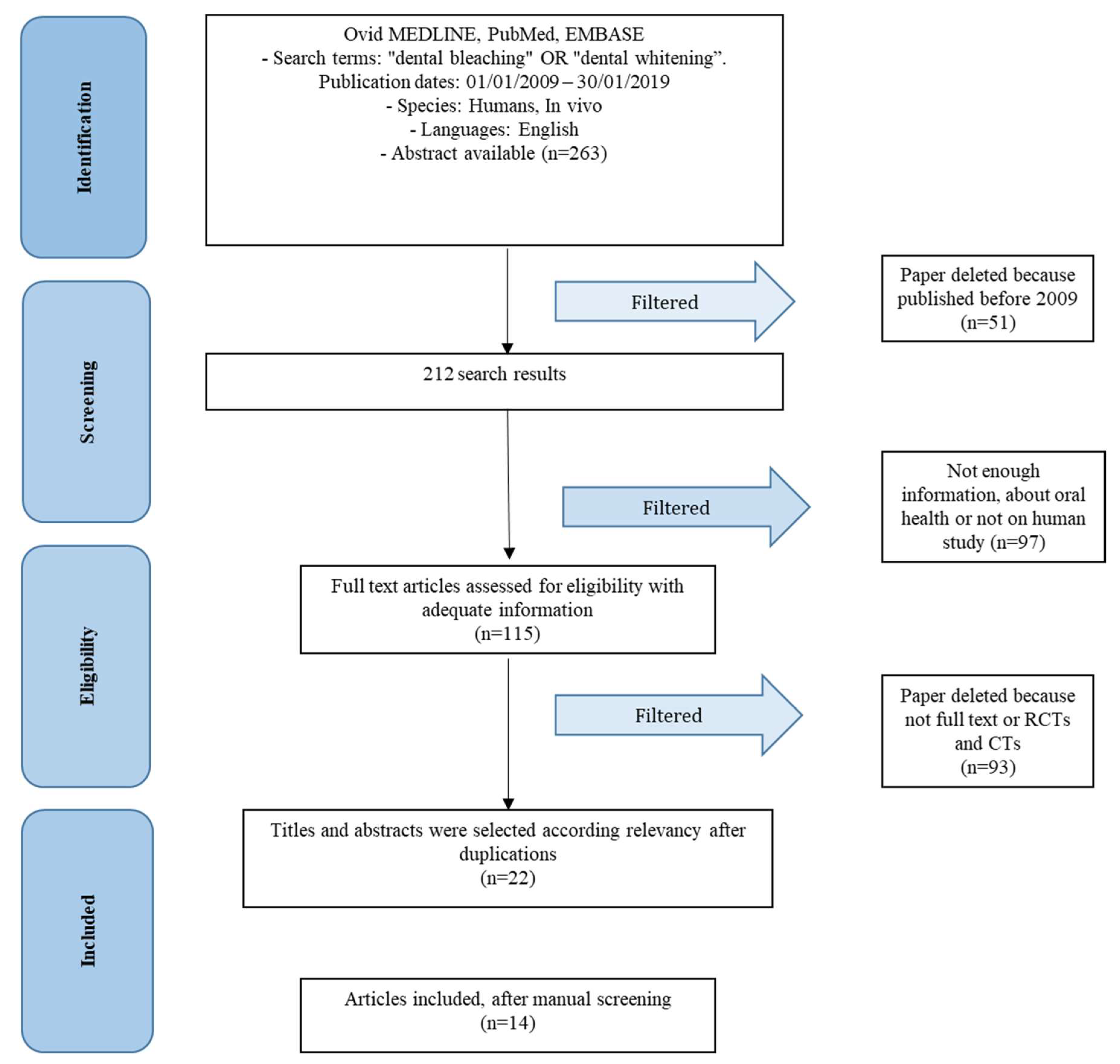
2.1. Study Selection
2.2. Study Characteristics
2.3. Synthesis of Results
- Tooth sensitivity
- Skin cold sensation
- Pain
- Difficulty in oral hygiene
3. Discussion
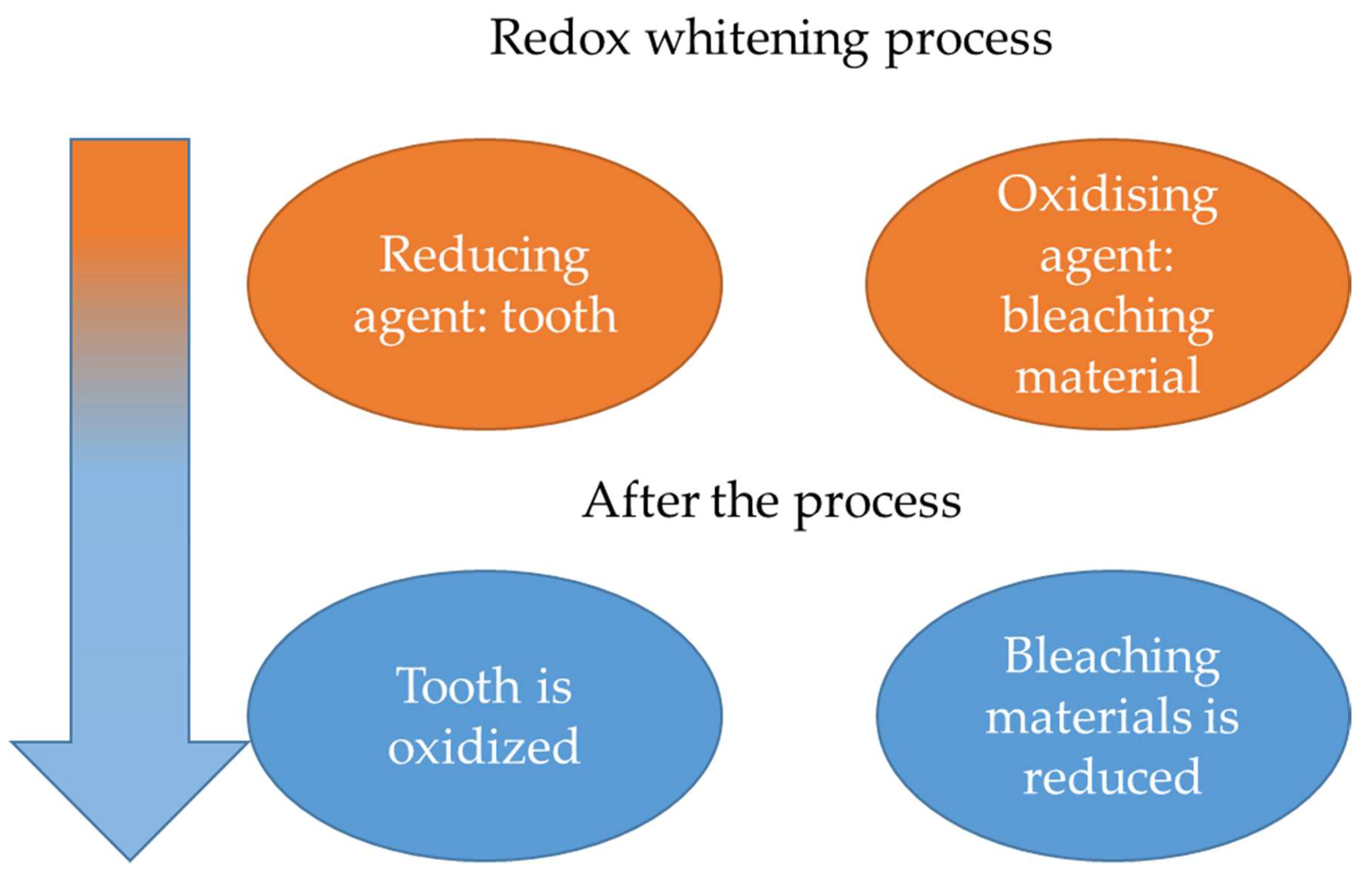
3.1. Type of Dental Bleaching
3.2. Office or Home Techniques
3.3. Summary of Evidence
3.4. Limitation
4. Conclusions
5. Materials and Methods
5.1. Information Sources
5.2. Search
- Are dental patients who have dental bleaching at increased risk of teeth damage?
- Does dental bleaching influence tooth sensitivity or alterations in patients?
5.3. Eligibility Criteria
- Study on dental bleaching gels or dental whitening technique.
- Study on post-operative, bleaching or whitening gels, unwanted effect and side
- Study on human trial (randomized controlled trial and clinical trial)
- Studies involving patients with disease.
- Not enough information about dental bleaching, conservative or preventive dentistry.
- Experimental dental material
- Animal studies
- Not full text articles
5.4. Risk of Bias Assessment
Author Contributions
Funding
Conflicts of Interest
Appendix A
Visual Analogue Scale
References
- Kwon, S.R.; Wertz, P.W. Review of the Mechanism of Tooth Whitening. J. Estet. Restor. Dent. 2015, 27, 240–257. [Google Scholar] [CrossRef]
- Maran, B.M.; Burey, A.; de Paris Matos, T.; Loguercio, A.D.; Reis, A. In-office dental bleaching with light vs. without light: A systematic review and meta-analysis. J. Dent. 2018, 70, 1–13. [Google Scholar] [CrossRef]
- Qin, T.; Mellgren, T.; Jefferies, S.; Xia, W.; Engqvist, H. A Study for Tooth Bleaching via Carbamide Peroxide-Loaded Hollow Calcium Phosphate Spheres. Dent. J. 2017, 5, 3. [Google Scholar] [CrossRef]
- Haywood, V.B.; Sword, R.J. Tooth bleaching questions answered. Br. Dent. J. 2017, 223, 369. [Google Scholar] [CrossRef]
- De Moor, R.J.G.; Verheyen, J.; Verheyen, P.; Diachuk, A.; Meire, M.A.; De Coster, P.J.; De Bruyne, F.; Keulemans, F. Laser Teeth Bleaching: Evaluation of Eventual Side Effects on Enamel and the Pulp and the Efficiency In Vitro and In Vivo. Sci. World J. 2015, 2015. [Google Scholar] [CrossRef]
- Presoto, C.D.; Bortolatto, J.F.; de Carvalho, P.P.F.; Trevisan, T.C.; Floros, M.C.; Junior, O.B.D.O. New Parameter for In-Office Dental Bleaching. Case Rep. Dent. 2016, 2016. [Google Scholar] [CrossRef]
- Lago, A.D.N.; de Freitas, P.M.; Araújo, E.M.D.S.; Matos, A.B.; Garone-Netto, N. Is It Necessary to Prepare the Enamel before Dental Bleaching? Int. J. Dent. 2017, 2017. [Google Scholar] [CrossRef]
- Lo Giudice, R.; Pantaleo, G.; Lizio, A.; Romeo, U.; Castiello, G.; Spagnuolo, G.; Lo Giudice, G. Clinical and Spectrophotometric Evaluation of LED and Laser Activated Teeth Bleaching. Open Dent. J. 2016, 10, 242–250. [Google Scholar] [CrossRef]
- Cochrane Training. Available online: https://methods.cochrane.org/bias/sites/methods.cochrane.org.bias/files/public/uploads/6.%20Assessing%20risk%20of%20bias%20in%20included%20studies%20v1.0%20Standard%20author%20slides.pdf (accessed on 6 May 2019).
- Chemin, K.; Rezende, M.; Loguercio, A.D.; Reis, A.; Kossatz, S. Effectiveness of and Dental Sensitivity to At-home Bleaching With 4% and 10% Hydrogen Peroxide: A Randomized, Triple-blind Clinical Trial. Oper. Dent. 2018, 43, 232–240. [Google Scholar] [CrossRef]
- Rossi, B.; Freitas, P.M.; Tedesco, T.K.; Gonçalves, F.; Ferreira, L.S. Tooth color changes and sensitivity in patients undergoing dental bleaching with 10% hydrogen peroxide using customized trays or strips: A randomized clinical trial. Minerva Stomatol. 2018, 67, 55–61. [Google Scholar] [CrossRef]
- Coppla, F.M.; Rezende, M.; de Paula, E.; Farago, P.V.; Loguercio, A.D.; Kossatz, S.; Reis, A. Combination of Acetaminophen/Codeine Analgesics Does Not Avoid Bleaching-Induced Tooth Sensitivity: A Randomized, Triple-Blind Two-Center Clinical Trial. Oper. Dent. 2018, 43, E53–E63. [Google Scholar] [CrossRef] [PubMed]
- Rahal, V.; Gallinari, M.O.; Barbosa, J.S.; Martins-Junior, R.L.; Santos, P.H.D.; Cintra, L.T.A.; Briso, A.L.F. Influence of skin cold sensation threshold in the occurrence of dental sensitivity during dental bleaching: A placebo controlled clinical trial. J. Appl. Oral Sci. 2018, 26. [Google Scholar] [CrossRef] [PubMed]
- Briso, A.L.F.; Rahal, V.; Azevedo, F.A.; Gallinari, M.O.; Gonçalves, R.S.; Frascino, S.M.B.; Santos, P.H.D.; Cintra, L.T.A. Neurosensory analysis of tooth sensitivity during at-home dental bleaching: A randomized clinical trial. J. Appl. Oral Sci. 2018, 26. [Google Scholar] [CrossRef] [PubMed]
- Mondelli, R.; Rizzante, F.; Rosa, E.R.; Borges, A.; Furuse, A.Y.; Bombonatti, J. Effectiveness of LED/Laser Irradiation on In-Office Dental Bleaching after Three Years. Oper. Dent. 2018, 43, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Nie, J.; Tian, F.C.; Wang, Z.H.; Yap, A.U.; Wang, X.Y. Comparison of efficacy and outcome satisfaction between in-office and home teeth bleaching in Chinese patients. J. Oral Sci. 2017, 59, 527–532. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Montenegro-Arana, A.; Arana-Gordillo, L.A.; Farana, D.; Davila-Sanchez, A.; Jadad, E.; Coelho, U.; Gomes, O.; Loguercio, A.D. Randomized Double-blind Clinical Trial of Bleaching Products in Patients Wearing Orthodontic Devices. Oper. Dent. 2016, 41, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Meireles, S.S.; Goettems, M.L.; Dantas, R.V.; Bona, Á.D.; Santos, I.S.; Demarco, F.F. Changes in oral health related quality of life after dental bleaching in a double-blind randomized clinical trial. J. Dent. 2014, 42, 114–121. [Google Scholar] [CrossRef]
- Moncada, G.; Sepúlveda, D.; Elphick, K.; Contente, M.; Estay, J.; Bahamondes, V.; Fernandez, E.; Oliveira, O.B.; Martin, J. Effects of light activation, agent concentration, and tooth thickness on dental sensitivity after bleaching. Oper. Dent. 2013, 38, 467–476. [Google Scholar] [CrossRef]
- Bonafé, E.; Bacovis, C.L.; Iensen, S.; Loguercio, A.D.; Reis, A.; Kossatz, S. Tooth sensitivity and efficacy of in-office bleaching in restored teeth. J. Dent. 2013, 41, 363–369. [Google Scholar] [CrossRef]
- Kossatz, S.; Martins, G.; Loguercio, A.D.; Reis, A. Tooth sensitivity and bleaching effectiveness associated with use of a calcium-containing in-office bleaching gel. J. Am. Dent. Assoc. 2012, 143, e81–e87. [Google Scholar] [CrossRef]
- Mondelli, R.F.; Azevedo, J.F.; Francisconi, A.C.; Almeida, C.M.; Ishikiriama, S.K. Comparative clinical study of the effectiveness of different dental bleaching methods—Two year follow-up. J. Appl. Oral Sci. 2012, 20, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Franz-Montan, M.; Ramacciato, J.C.; Rodrigues, J.A.; Marchi, G.M.; Rosalen, P.L.; Groppo, F.C. The effect of combined bleaching techniques on oral microbiota. Indian J. Dent. Res. 2009, 20, 304–307. [Google Scholar] [CrossRef] [PubMed]
- Cogo, E.; Sibilla, P.; Turrini, R. Sbiancamento Dentale. Metodi per il Successo; Quintessence: Chicago, IL, USA, 2011; ISBN 88-7492-157-8. [Google Scholar]
- Joiner, A. Tooth colour: A review of the literature. J. Dent. 2004, 32 (Suppl. 1), 3–12. [Google Scholar] [CrossRef] [PubMed]
- Llena, C.; Martínez-Galdón, O.; Forner, L.; Gimeno-Mallench, L.; Rodríguez-Lozano, F.J.; Gambini, J. Hydrogen Peroxide Diffusion through Enamel and Dentin. Materials 2018, 11, 1694. [Google Scholar] [CrossRef] [PubMed]
- Casado, B.G.; Moraes, S.L.; Souza, G.F.; Guerra, C.M.; Souto-Maior, J.R.; Lemos, C.A.; Vasconcelos, B.C.E.; Pellizzer, E.P. Efficacy of Dental Bleaching with Whitening Dentifrices: A Systematic Review. Int. J. Dent. 2018, 2018. [Google Scholar] [CrossRef] [PubMed]
- Oldoini, G.; Bruno, A.; Genovesi, A.M.; Parisi, L. Effects of Amorphous Calcium Phosphate Administration on Dental Sensitivity during In-Office and At-Home Interventions. Dent. J. 2018, 6, 52. [Google Scholar] [CrossRef]
- Troiano, G.; Laino, L.; Cicciù, M.; Cervino, G.; Fiorillo, L.; D’amico, C.; Zhurakivska, K.; Lo Muzio, L. Comparison of Two Routes of Administration of Dexamethasone to Reduce the Postoperative Sequelae After Third Molar Surgery: A Systematic Review and Meta-Analysis. Open Dent. J. 2018, 12, 181. [Google Scholar] [CrossRef]
- Cervino, G.; Fiorillo, L.; Spagnuolo, G.; Bramanti, E.; Laino, L.; Lauritano, F.; Cicciù, M. Interface Between MTA and Dental Bonding Agents: Scanning Electron Microscope Evaluation. J. Int. Soc. Prev. Community Dent. 2017, 7, 64–68. [Google Scholar] [CrossRef]
- Boruziniat, A.; Atoufi, A.; Chehreli, Z.; Akbari, M.; Gifani, M. Effect of Non-Vital Bleaching on the Durability of Resin–Dentin Bond with an Ethanol-Based Etch-And-Rinse Adhesive. Biomimetics 2018, 3, 35. [Google Scholar] [CrossRef]
- Cervino, G.; Fiorillo, L.; Herford, A.S.; Laino, L.; Troiano, G.; Amoroso, G.; Crimi, S.; Matarese, M.; D’Amico, C.; Nastro Siniscalchi, E.; et al. Alginate Materials and Dental Impression Technique: A Current State of the Art and Application to Dental Practice. Mar. Drugs 2018, 17, 18. [Google Scholar] [CrossRef]
- Cervino, G.; Fiorillo, L.; Laino, L.; Herford, A.S.; Lauritano, F.; Giudice, G.L.; Fama, F.; Santoro, R.; Troiano, G.; Iannello, G.; et al. Oral Health Impact Profile in Celiac Patients: Analysis of Recent Findings in a Literature Review. Gastroenterol. Res. Pract. 2018, 2018, 7848735. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, T.; Bernardello, F.; Berton, F.; Porrelli, D.; Rapani, A.; Camurri Piloni, A.; Fiorillo, L.; Di Lenarda, R.; Stacchi, C. Efficacy of Alveolar Ridge Preservation after Maxillary Molar Extraction in Reducing Crestal Bone Resorption and Sinus Pneumatization: A Multicenter Prospective Case-Control Study. BioMed Res. Int. 2018, 2018, 9352130. [Google Scholar] [CrossRef] [PubMed]
- Cervino, G.; Fiorillo, L.; Herford, A.S.; Romeo, U.; Bianchi, A.; Crimi, S.; De Stefano, R.; Troiano, G.; Santoro, R.; Laino, L.; et al. Molecular Biomarkers Related to Oral Carcinoma: Clinical Trial Outcome Evaluation in a Literature Review. Dis. Mark. 2019, 2019. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, L.; De Stefano, R.; Cervino, G.; Crimi, S.; Bianchi, A.; Campagna, P.; Herford, A.C.; Laino, L.; Cicciù, M. Oral and Psychological Alterations in Haemophiliac Patients. Biomedicines 2019, 7, 33. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, L. Chlorhexidine gel use in the oral district: A systematic review. Gels 2019, 5, 31. [Google Scholar] [CrossRef]
- Cervino, G.; Fiorillo, L.; Arzukanyan, A.V.; Spagnuolo, G.; Cicciù, M. Dental Restorative Digital Workflow: Digital Smile Design from Aesthetic to Function. Dent. J. 2019, 7, 30. [Google Scholar] [CrossRef] [PubMed]
- Crespi, R.; Capparè, P.; Gherlone, E. Magnesium-enriched hydroxyapatite compared to calcium sulfate in the healing of human extraction sockets: Radiographic and histomorphometric evaluation at 3 months. J. Periodontol. 2009, 80, 210–218. [Google Scholar] [CrossRef]
- Crespi, R.; Capparè, P.; Gherlone, E. Osteotome sinus floor elevation and simultaneous implant placement in grafted biomaterial sockets: 3 years of follow-up. J. Periodontol. 2010, 81, 344–349. [Google Scholar] [CrossRef]
- De Rosa, C.; Sampogna, G.; Luciano, M.; Del Vecchio, V.; Fabrazzo, M.; Fiorillo, A. Social versus biological psychiatry: It’s time for integration! Int. J. Soc. Psychiatry 2018, 64, 617–621. [Google Scholar] [CrossRef]
- Machado, A.W. 10 commandments of smile esthetics. Dent. Press J. Orthod. 2014, 19, 136–157. [Google Scholar] [CrossRef]
- Lecocq, G.; Trung, L.T.T. Smile esthetics: Calculated beauty? Int. Orthod. 2014, 12, 149–170. [Google Scholar] [CrossRef] [PubMed]
- Flytström, I.; Stenberg, B.; Svensson, Å.; Bergbrant, I.M. Patients’ visual analogue scale: A useful method for assessing psoriasis severity. Acta Derm. Venereol. 2012, 92, 347–348. [Google Scholar] [CrossRef] [PubMed]

| Author | Year | Bleaching Techniques | Side Effects | Results |
|---|---|---|---|---|
| Chemin et al. [10] | 2018 | 4% HP (Hydrogen Peroxide) 10% HP | Tooth sensitivity | The absolute risk and intensity of tooth sensitivity was higher in the group that used HP 10 than the one that used HP 4 |
| Rossi et al. [11] | 2018 | 10% HP tray 10% HP strip | Tooth sensitivity | Strips were associated with a lower frequency of dental sensitivity (Table 2). |
| Coppla et al. [12] | 2018 | 35% HP | Tooth sensitivity | The use of an acetaminophen/codeine combination prior to in-office bleaching does not reduce the risk and intensity of bleaching-induced TS (Tooth Sensitivity). |
| Rahal et al. [13] | 2018 | 35% HP | Tooth sensitivity Skin cold sensation | Bleaching treatment increased dental sensitivity and skin cold sensation |
| Briso et al. [14] | 2018 | 10% CP (Carbamide Plus) | Tooth sensitivity | We concluded that the bleaching treatment sensitized the teeth |
| Over 20% of the teeth presented spontaneous sensitivity | ||||
| Mondelli et al. [15] | 2018 | LPS 35% + LPS (Lase Peroxide) 35% + HL (Hybrid Light) WHP (Whiteness Hydrogen Peroxide) 35% + LPS 25% + HL | Tooth sensitivity | The sensitivity decreased after 24 h for all groups |
| Nie et al. [16] | 2017 | In-office bleaching (OB) Take-home bleaching (HB) | Tooth sensitivity | Visual analogue scale (VAS) scores were greater for HB |
| Montenegro-Arana et al. [17] | 2016 | 8% HP 10% HP | Tooth sensitivity | The number of patients with sensitivity was 58.8% and 73.3% |
| Meireles et al. [18] | 2014 | 10% CP 16% CP | Oral health related quality of life Difficult in oral hygiene and pain | Positive impact of the dental bleaching was detected, with patients showing more their teeth without embarrassment. |
| Moncada et al. [19] | 2013 | 15% HP 35% HP + Light 35% HP | Tooth sensitivity | Increases in the concentration of bleaching agents directly affect tooth sensitivity, and LED/laser activation and tooth thickness are not correlated |
| Bonafé et al. [20] | 2013 | 35% HP | Tooth sensitivity Restoration interactions | Bleaching can promote higher intensity of sensitivity |
| Kossatz et al. [21] | 2012 | 35% HP 35% HP + calcium | Tooth sensitivity | The results of this study support the findings that a CC 35 percent hydrogen peroxide gel can reduce sensitivity |
| Mondelli et al. [22] | 2012 | 35% HP + HL 35% HP 38% HP | Tooth sensitivity | All techniques and bleaching gels used were effective in teeth bleaching |
| Franz-Montan et al. [23] | 2009 | 10% CP 37% CP 10% CP + 37% CP | Oral antimicrobial activity | The carbamide peroxide when used at 37%, 10%, or in combination, did not affect human salivary microorganisms. |
| VAS Tooth Sensitivity | Score 1 | Score 2 | Score 3 |
|---|---|---|---|
| Strip bleaching (SB) | 37.3% | 9.8% | 2.7% |
| Tray bleaching (TB) | 20.9% | 8.4% | 0.5% |
| Author | Year | Risk of Bias | |||
|---|---|---|---|---|---|
| Unclear | Low | Moderate | High | ||
| Chemin et al. [10] | 2018 | ✓ | |||
| Rossi et al. [11] | 2018 | ✓ | |||
| Coppla et al. [12] | 2018 | ✓ | |||
| Rahal et al. [13] | 2018 | ✓ | |||
| Briso et al. [14] | 2018 | ✓ | |||
| Mondelli et al. [15] | 2018 | ✓ | |||
| Nie et al. [16] | 2017 | ✓ | |||
| Montenegro-Arana et al. [17] | 2016 | ✓ | |||
| Meireles et al. [18] | 2014 | ✓ | |||
| Moncada et al. [19] | 2013 | ✓ | |||
| Bonafé et al. [20] | 2013 | ✓ | |||
| Kossatz et al. [21] | 2012 | ✓ | |||
| Mondelli et al. [22] | 2012 | ✓ | |||
| Franz-Montan et al. [23] | 2009 | ✓ | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fiorillo, L.; Laino, L.; De Stefano, R.; D’Amico, C.; Bocchieri, S.; Amoroso, G.; Isola, G.; Cervino, G. Dental Whitening Gels: Strengths and Weaknesses of an Increasingly Used Method. Gels 2019, 5, 35. https://doi.org/10.3390/gels5030035
Fiorillo L, Laino L, De Stefano R, D’Amico C, Bocchieri S, Amoroso G, Isola G, Cervino G. Dental Whitening Gels: Strengths and Weaknesses of an Increasingly Used Method. Gels. 2019; 5(3):35. https://doi.org/10.3390/gels5030035
Chicago/Turabian StyleFiorillo, Luca, Luigi Laino, Rosa De Stefano, Cesare D’Amico, Salvatore Bocchieri, Giulia Amoroso, Gaetano Isola, and Gabriele Cervino. 2019. "Dental Whitening Gels: Strengths and Weaknesses of an Increasingly Used Method" Gels 5, no. 3: 35. https://doi.org/10.3390/gels5030035
APA StyleFiorillo, L., Laino, L., De Stefano, R., D’Amico, C., Bocchieri, S., Amoroso, G., Isola, G., & Cervino, G. (2019). Dental Whitening Gels: Strengths and Weaknesses of an Increasingly Used Method. Gels, 5(3), 35. https://doi.org/10.3390/gels5030035










