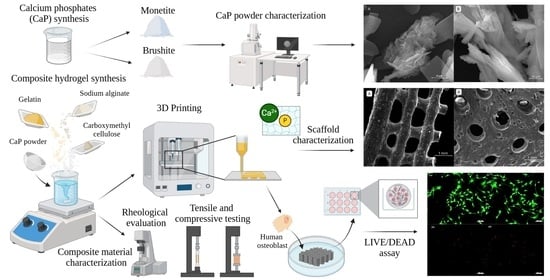
Effect of Phosphate Phase Incorporation on 3D-Printed Hydrogel Scaffolds: Towards Customizable Bone Graft Materials
Abstract
1. Introduction
2. Results and Discussion
2.1. CaP Powders Characterization
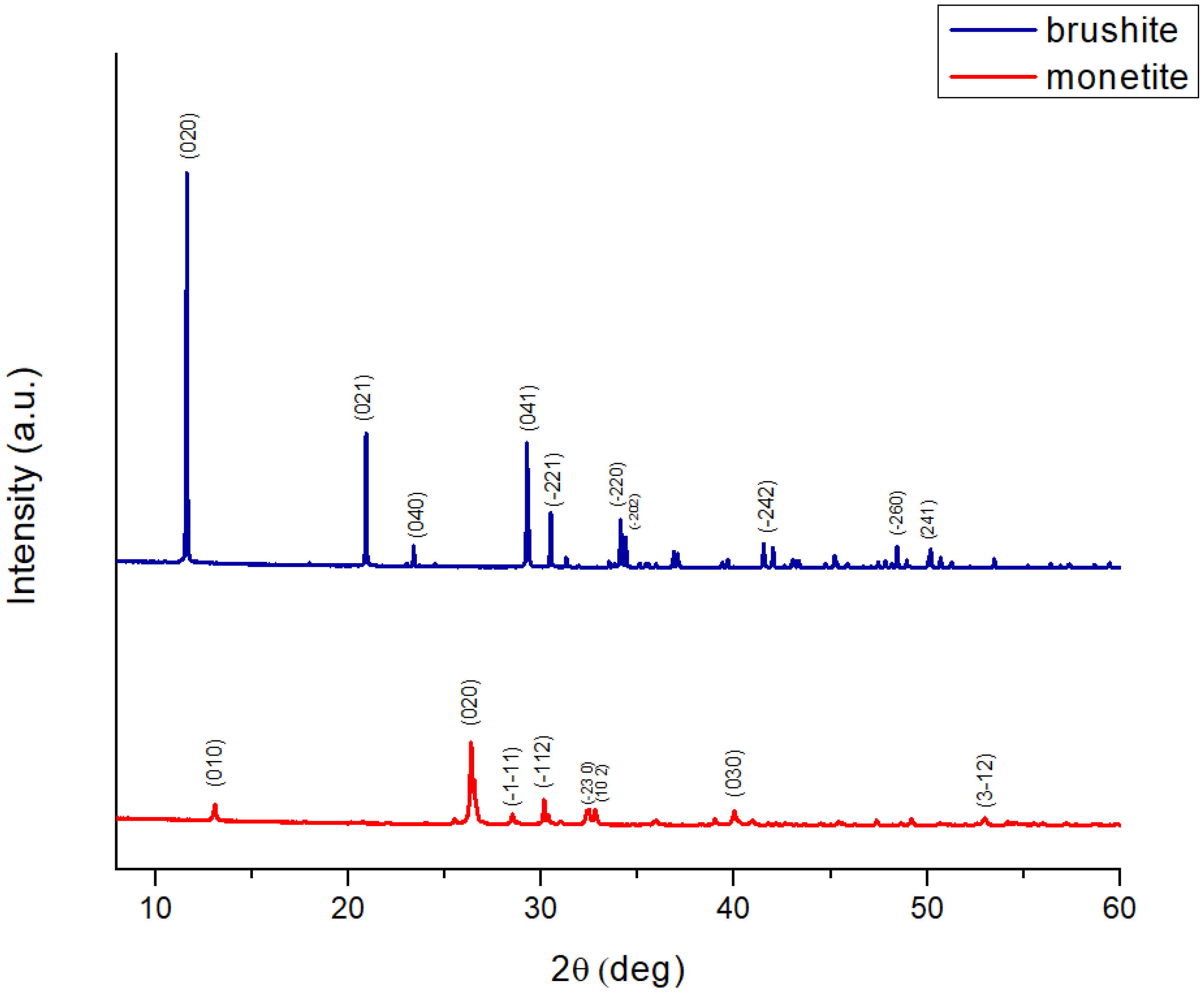
2.1.1. X-Ray Diffraction
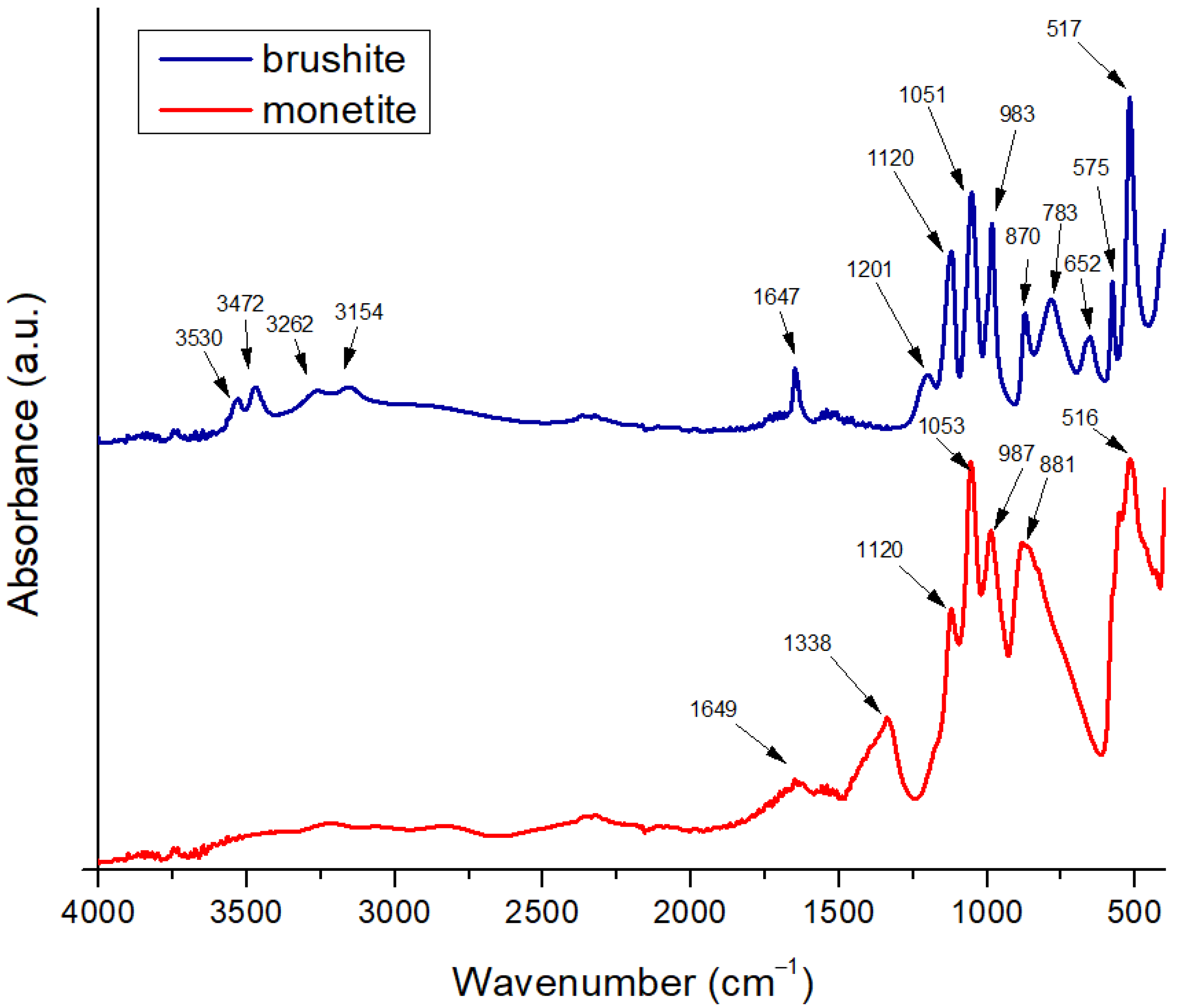
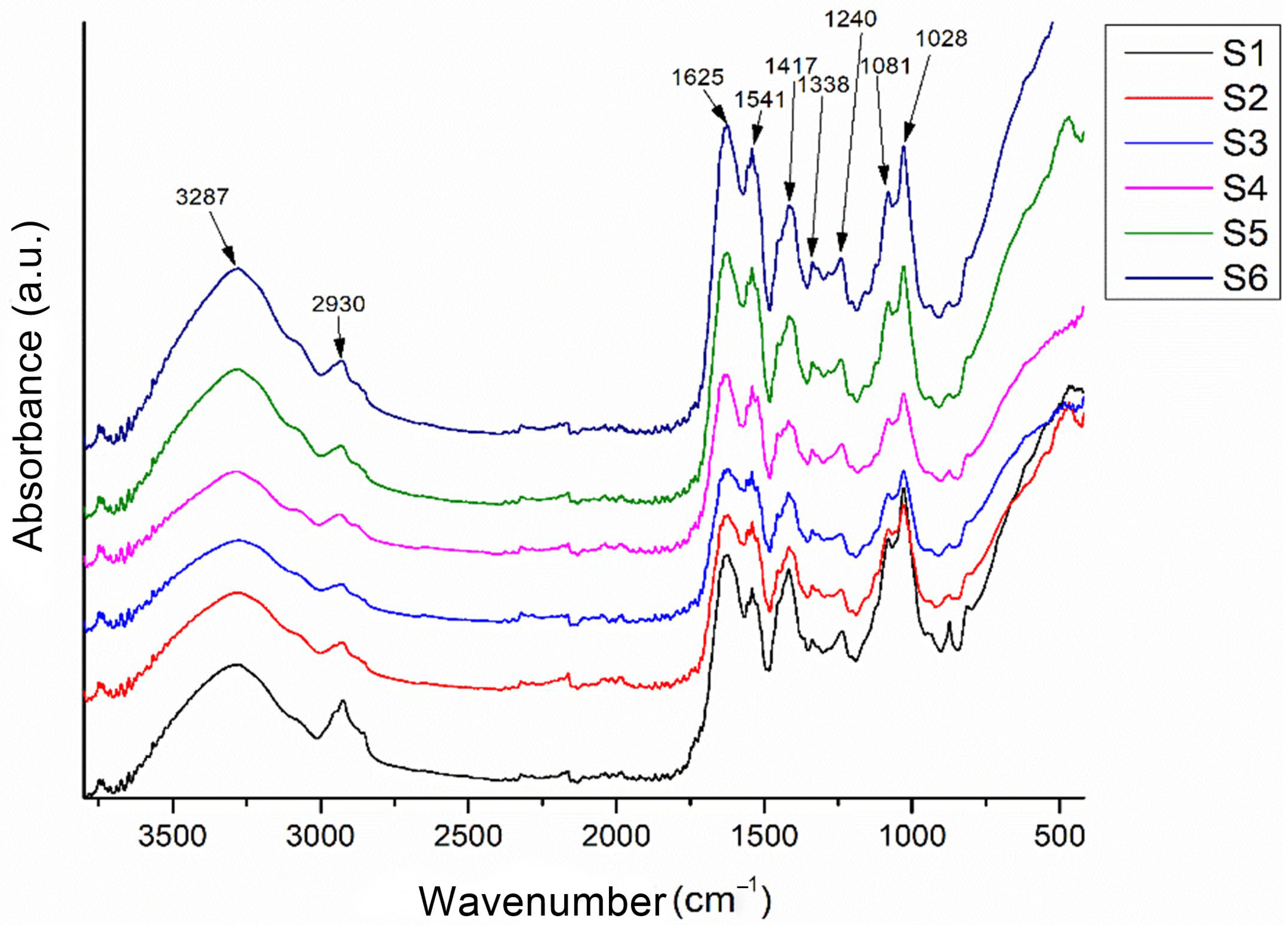
2.1.2. Fourier Transform Infrared Spectroscopy
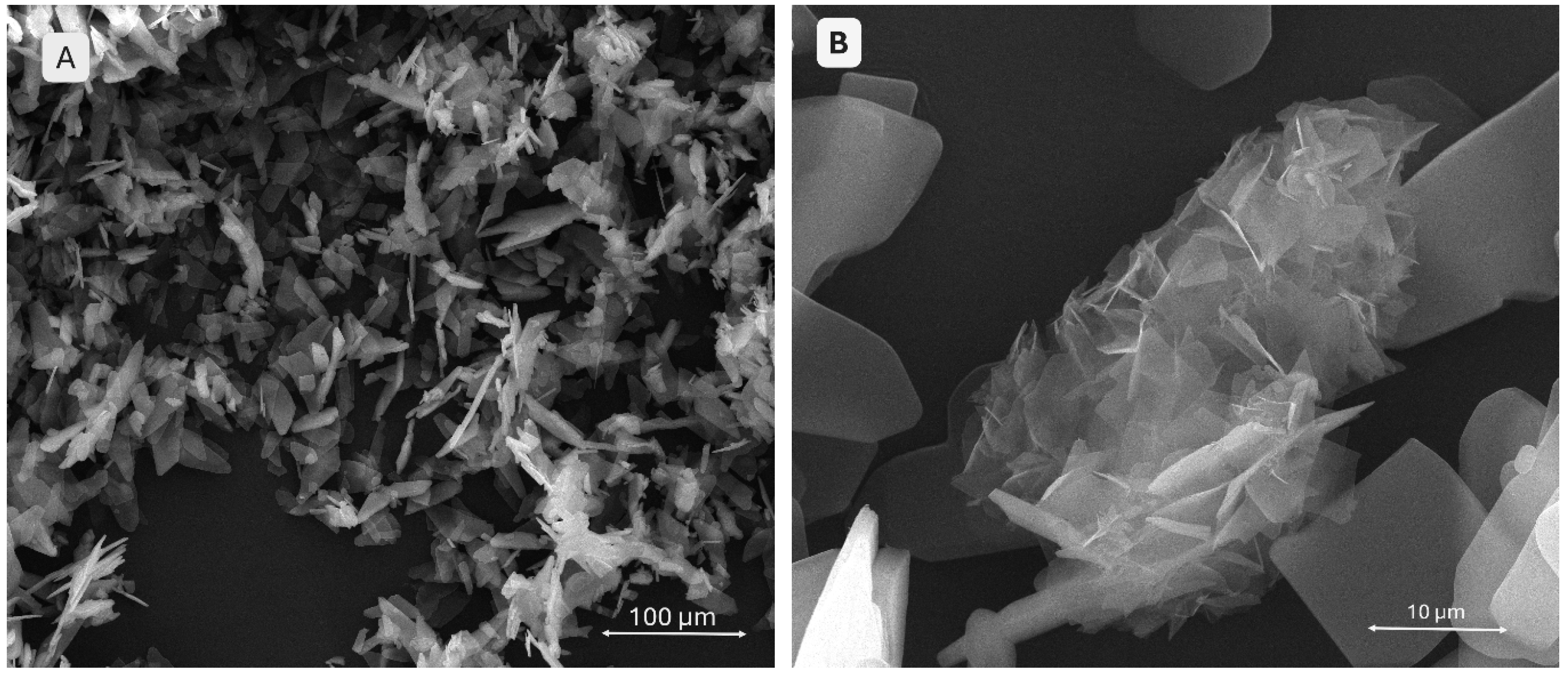
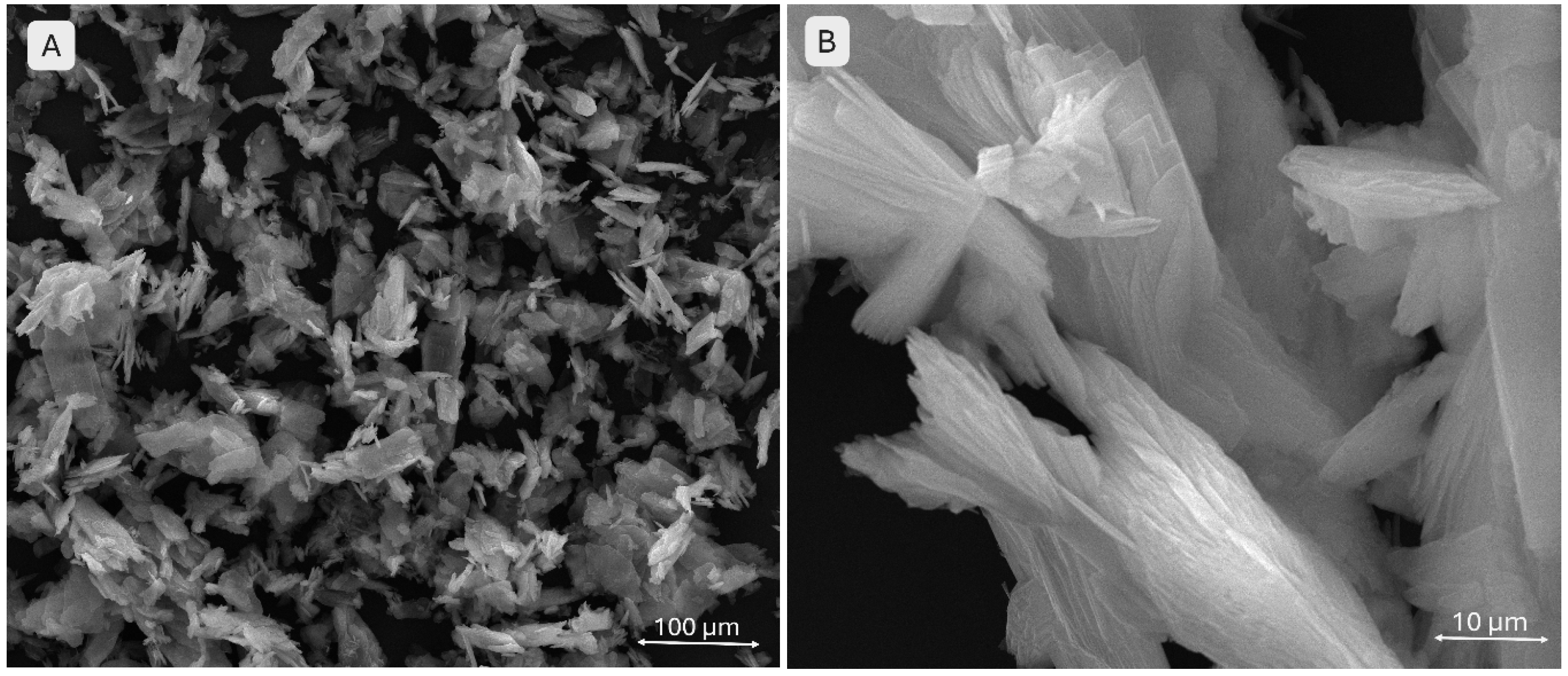
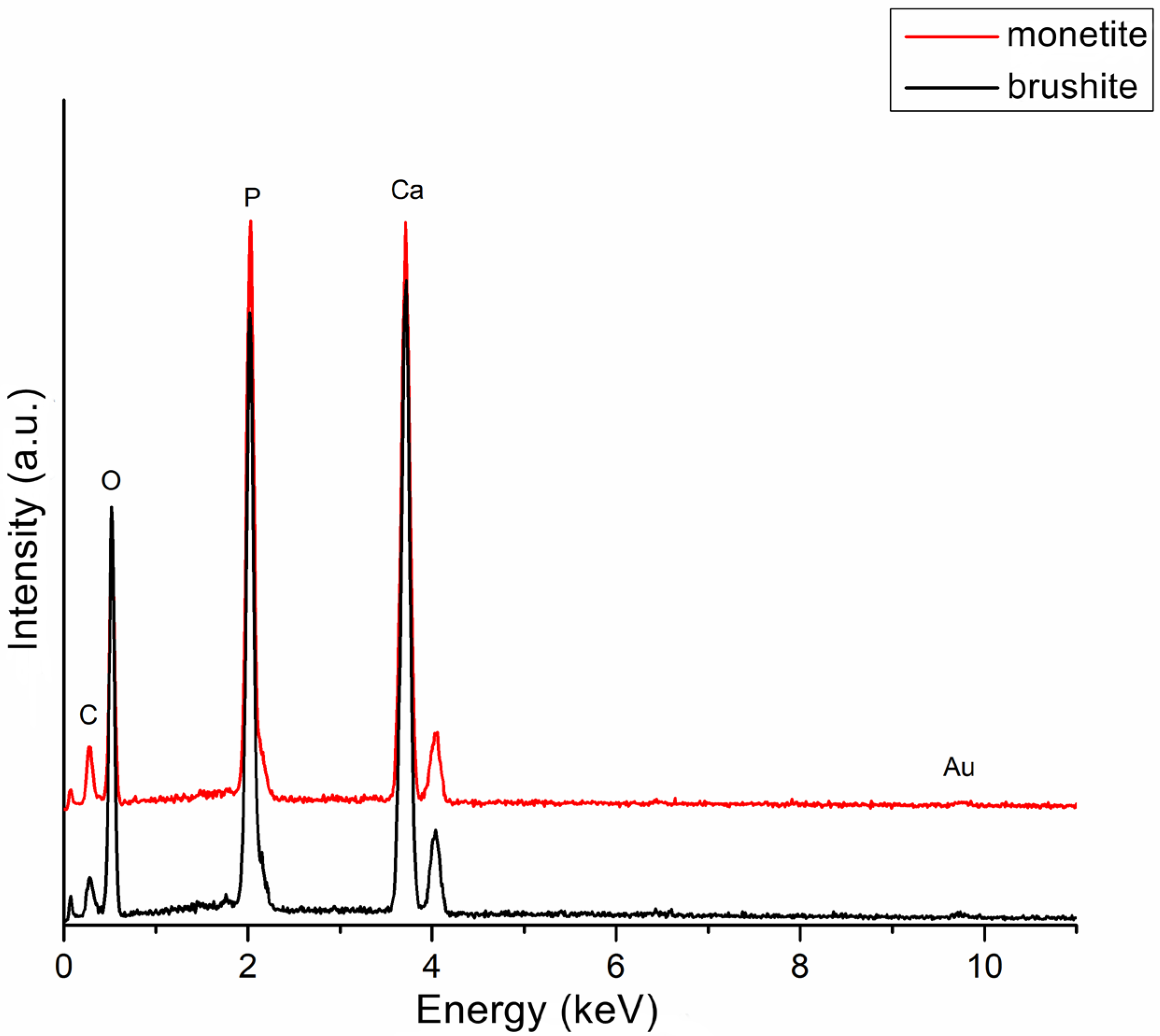
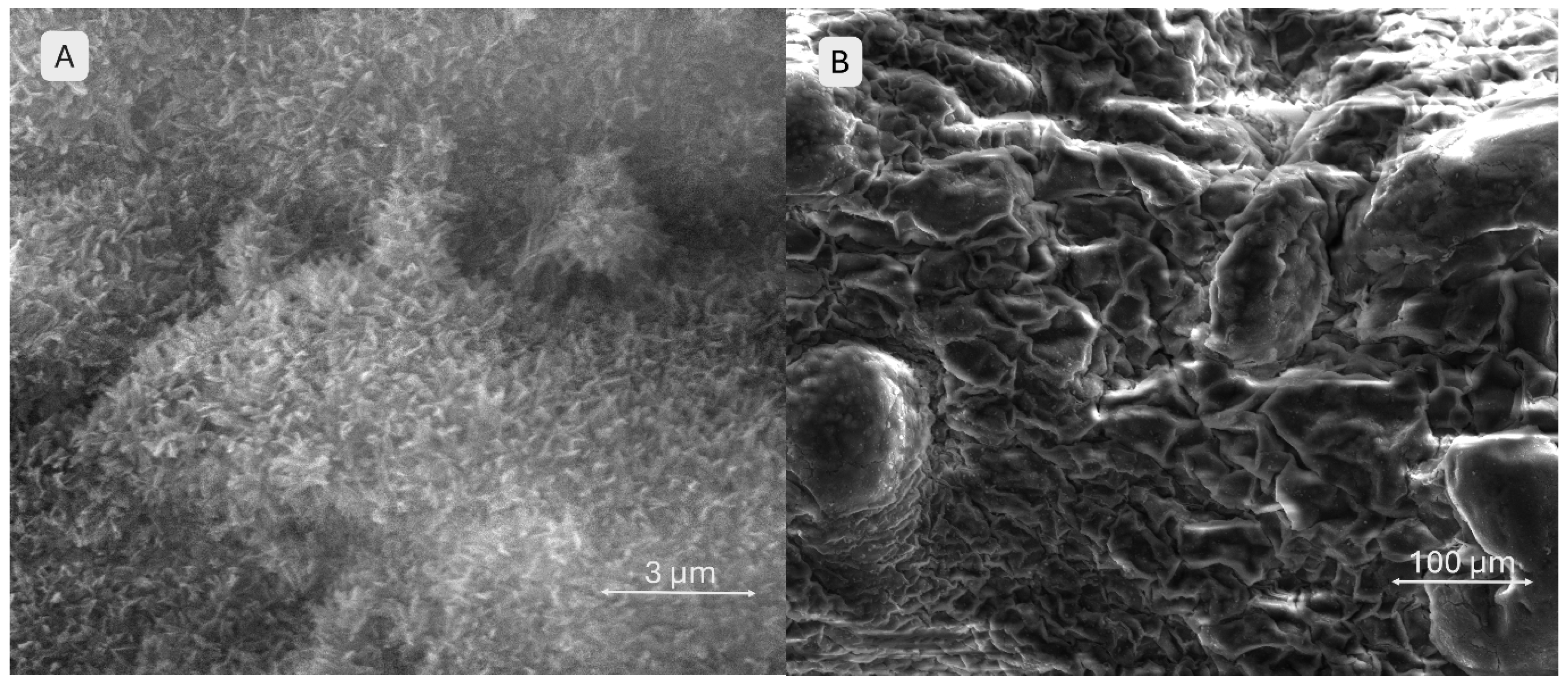
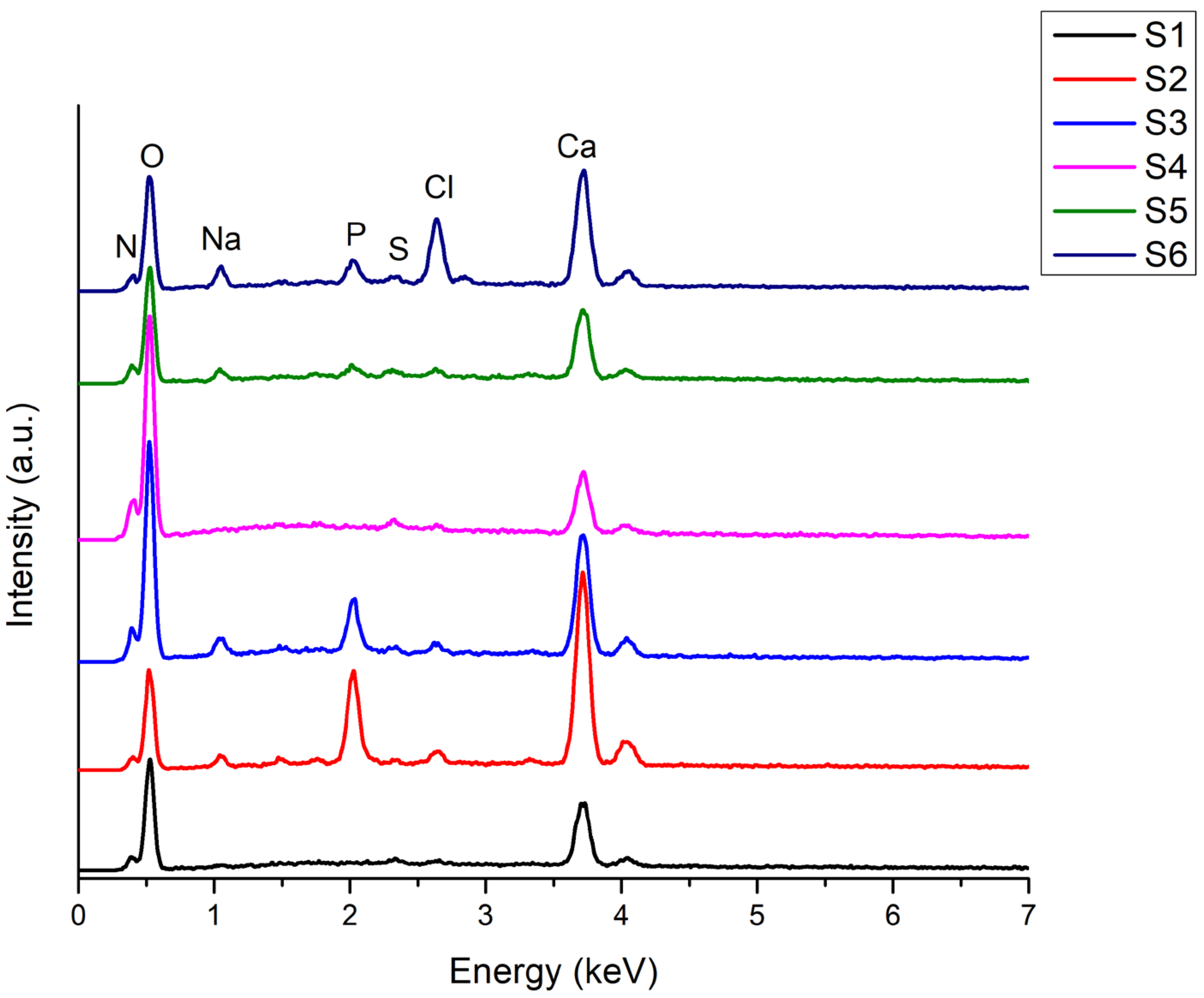
2.1.3. Scanning Electron Microscopy and X-Ray Energy-Dispersive Spectroscopy
2.2. Composite Hydrogel Characterization
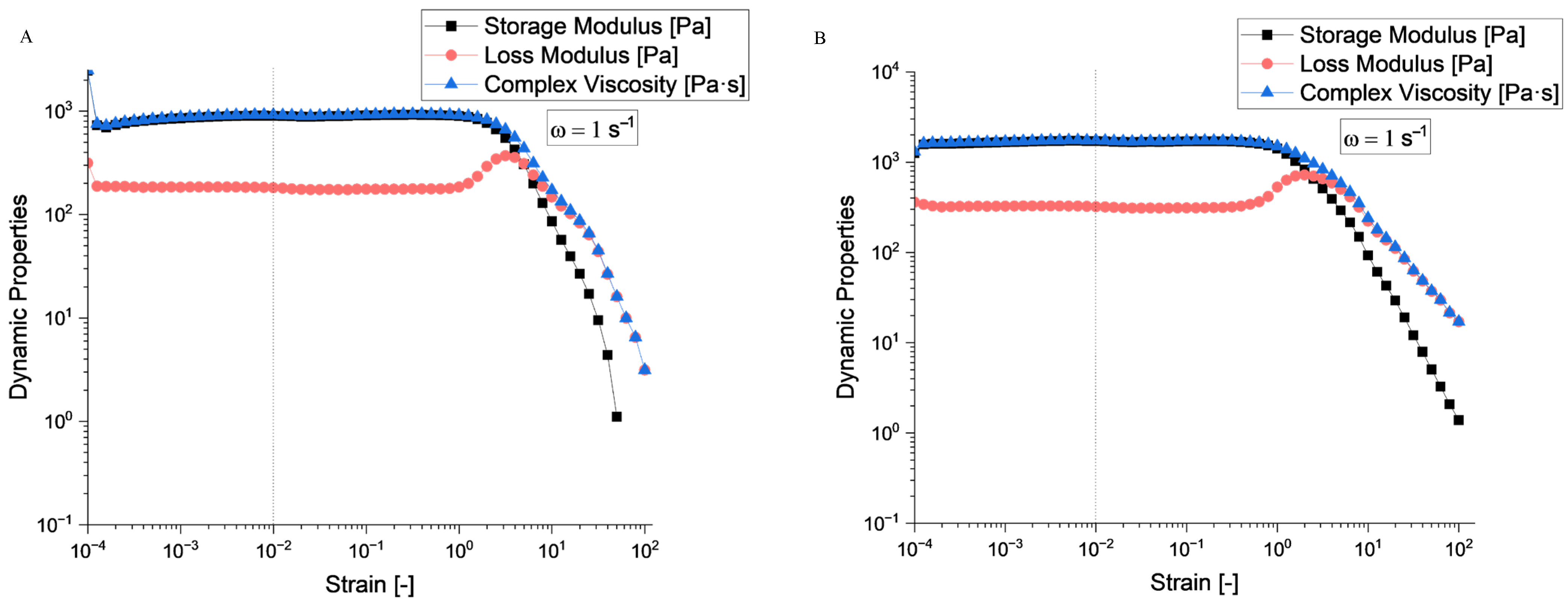
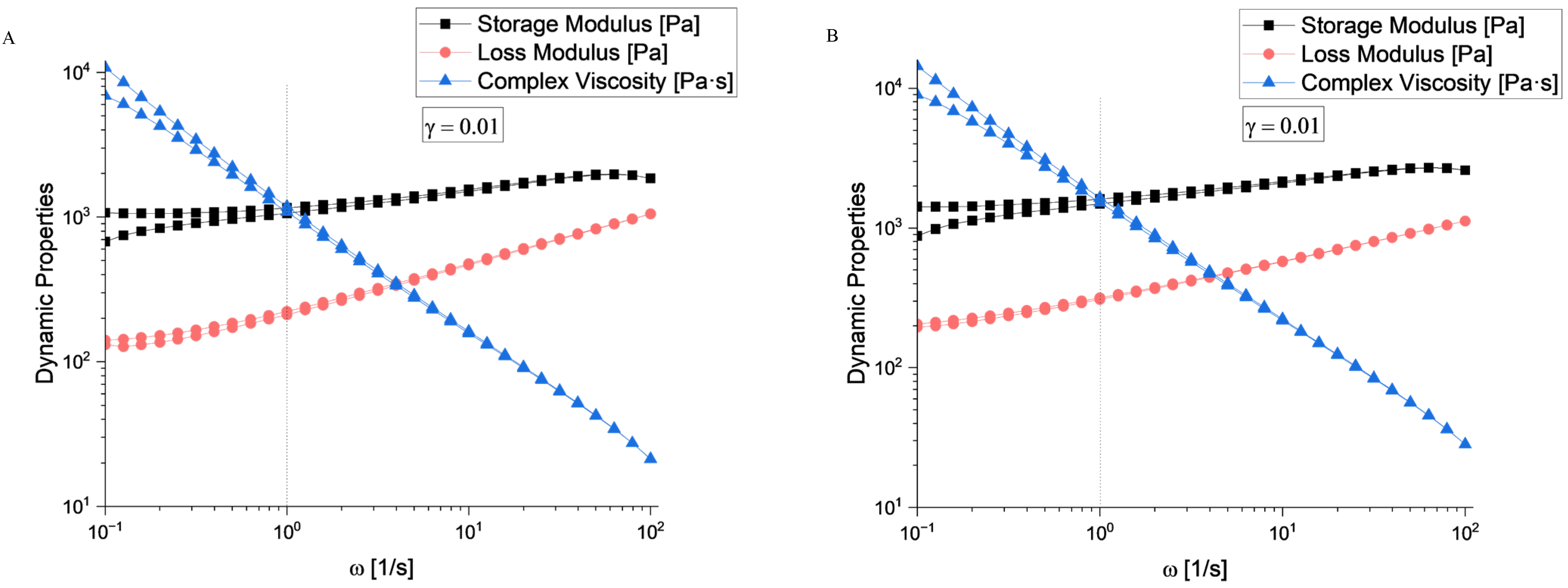
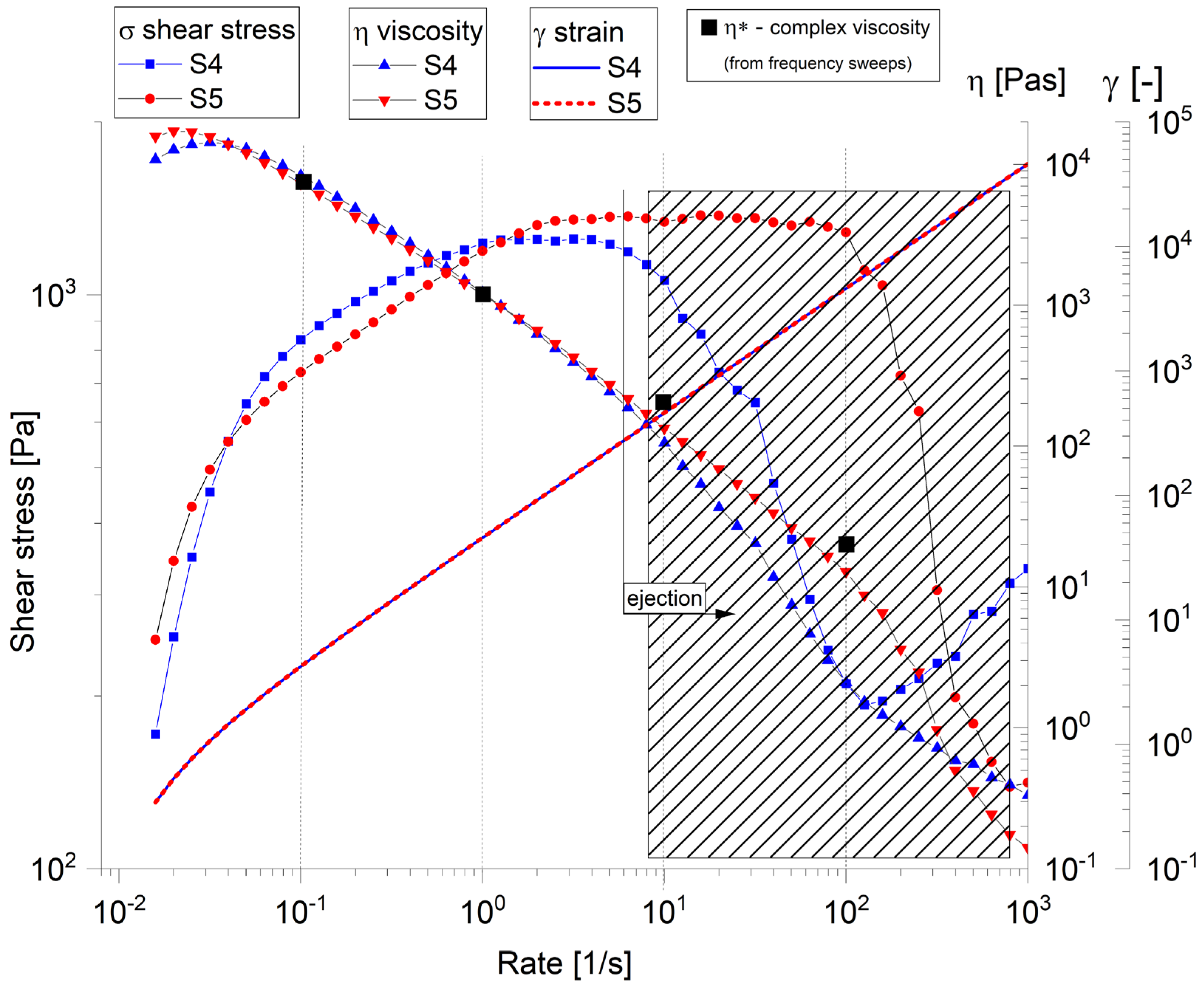
2.2.1. Rheological Evaluation
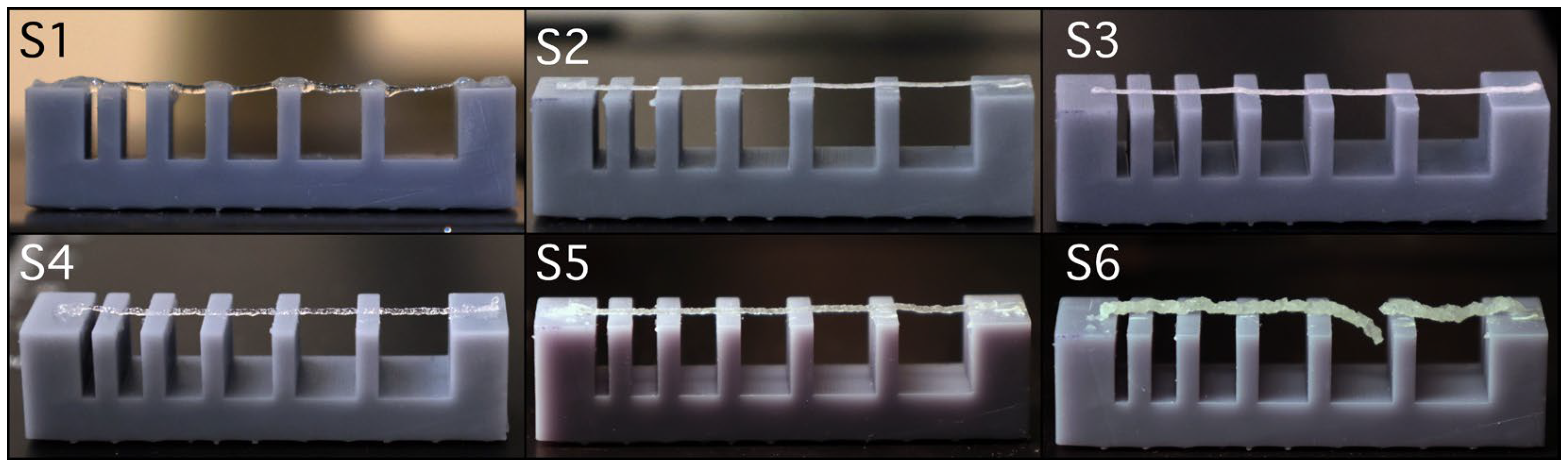
2.2.2. Filament Collapse Testing
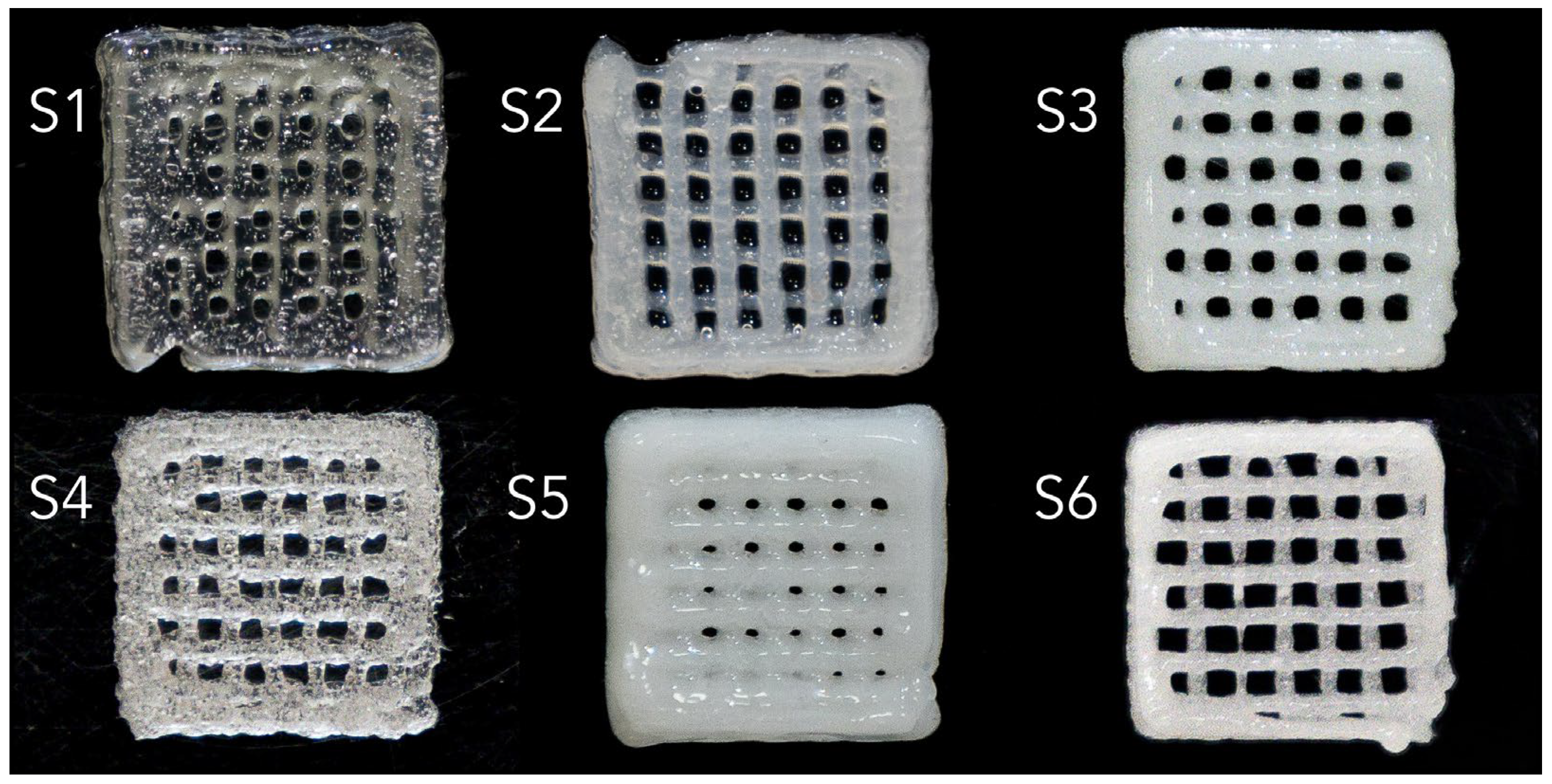
2.2.3. Extrusion-Based 3D Bioprinting
2.2.4. Fourier Transform Infrared Spectroscopy
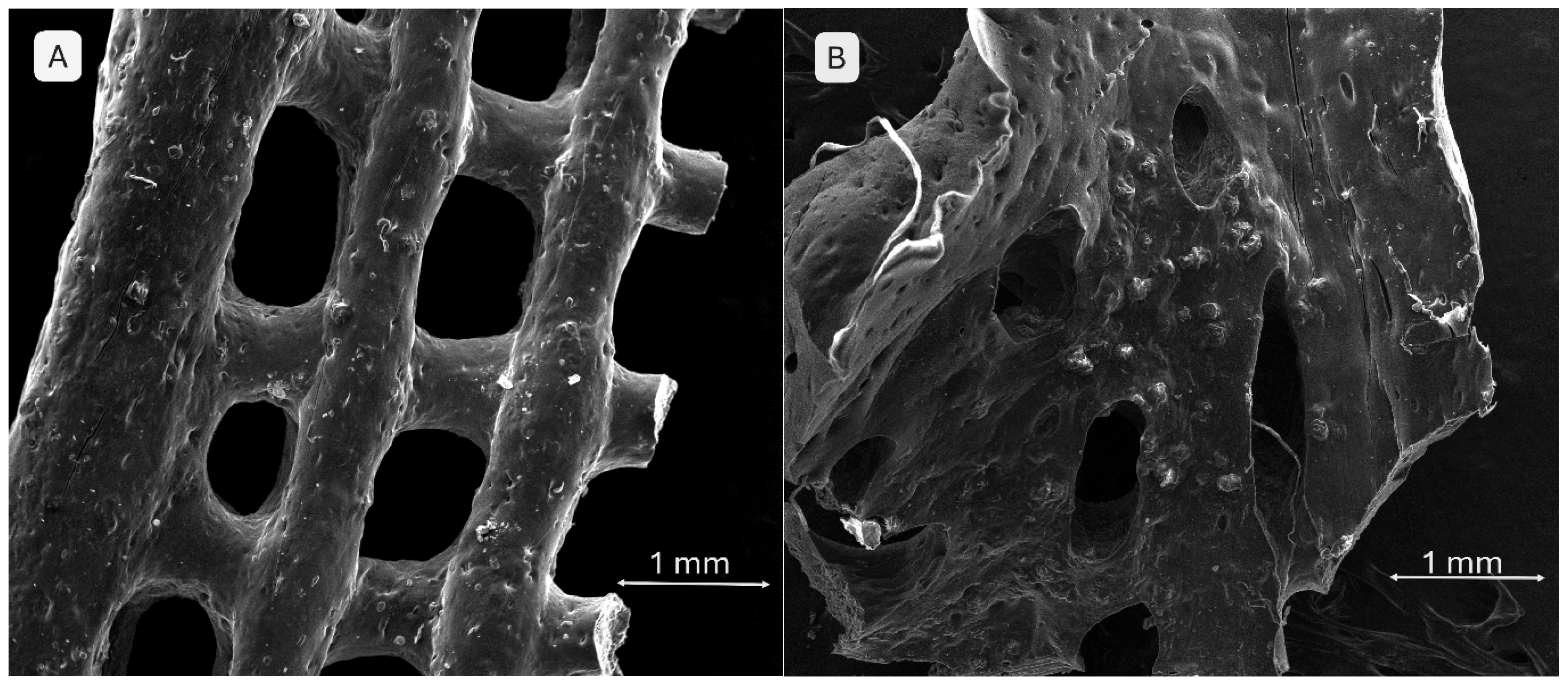
2.2.5. Scanning Electron Microscopy and X-Ray Energy-Dispersive Spectroscopy
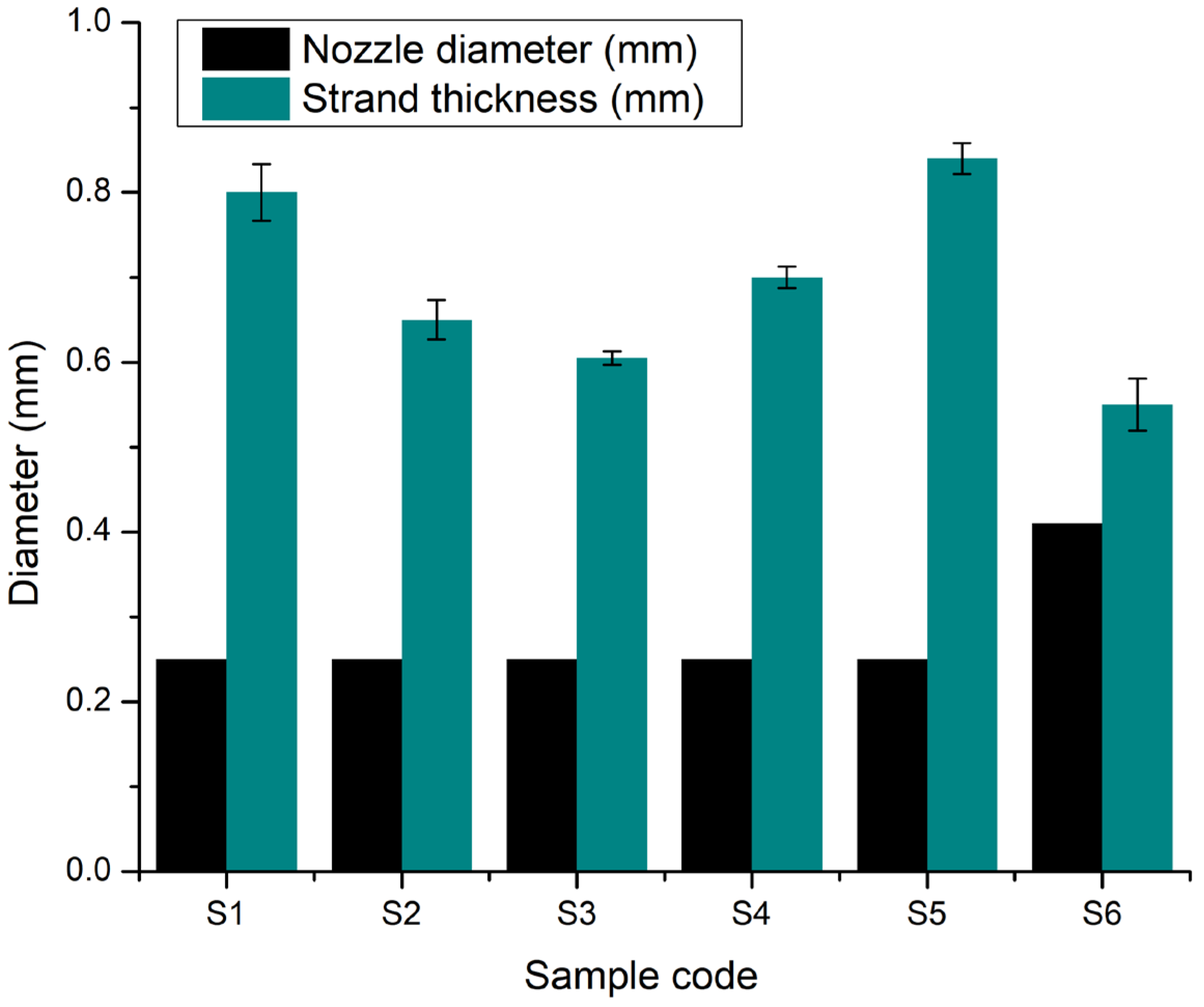
2.2.6. Printing Accuracy
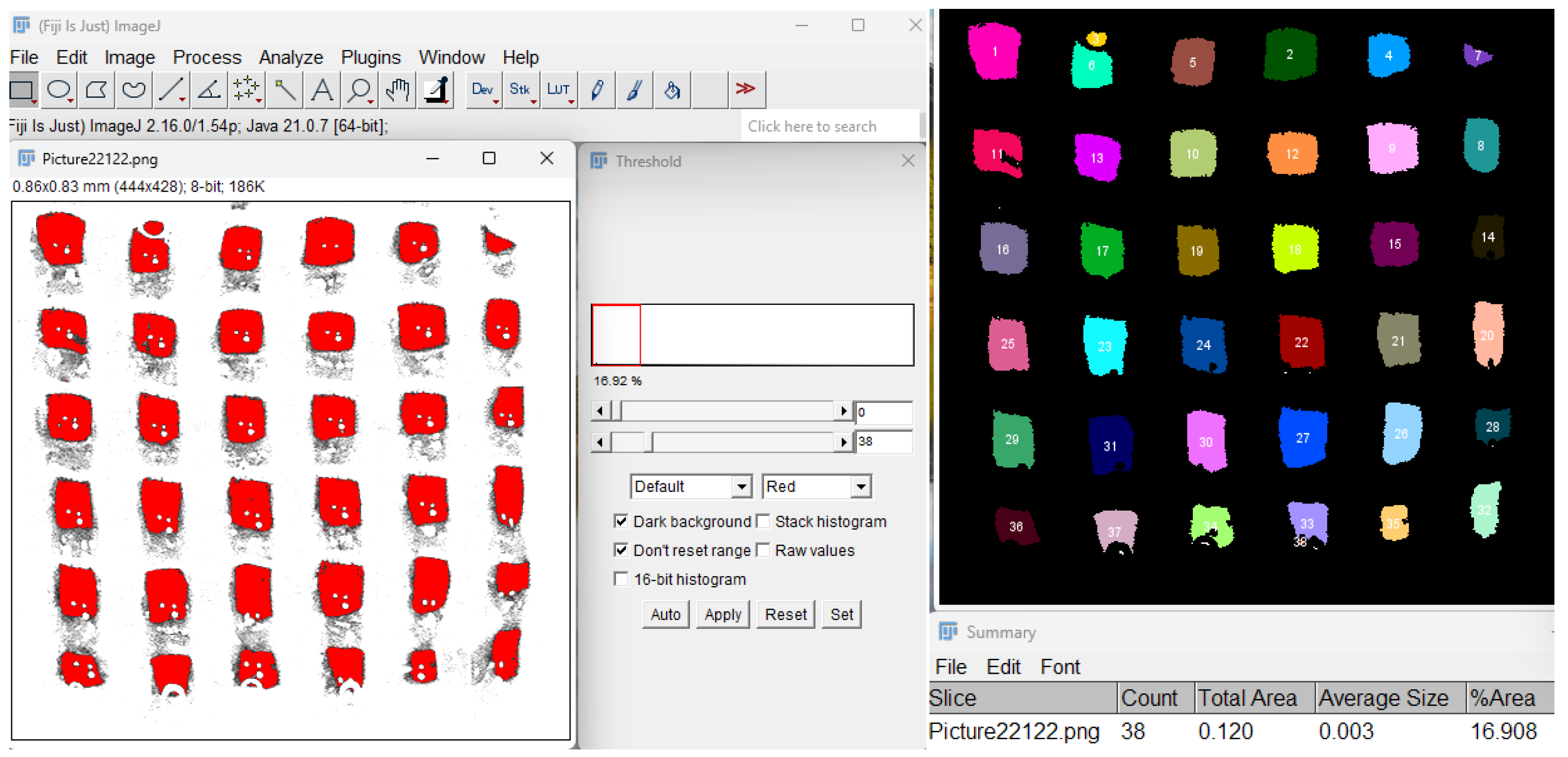
2.2.7. Porosity Evaluation
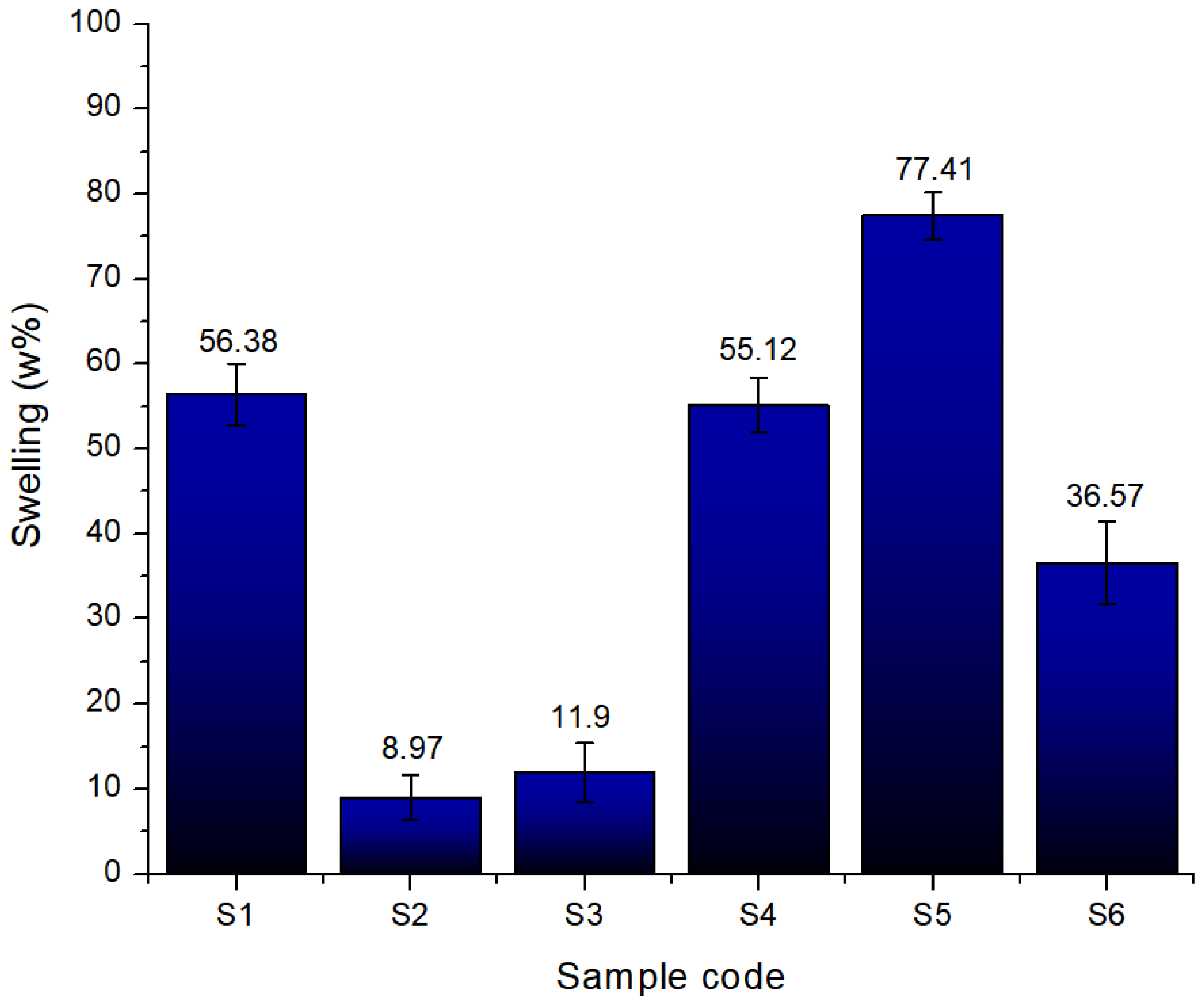
2.2.8. Swelling Degree
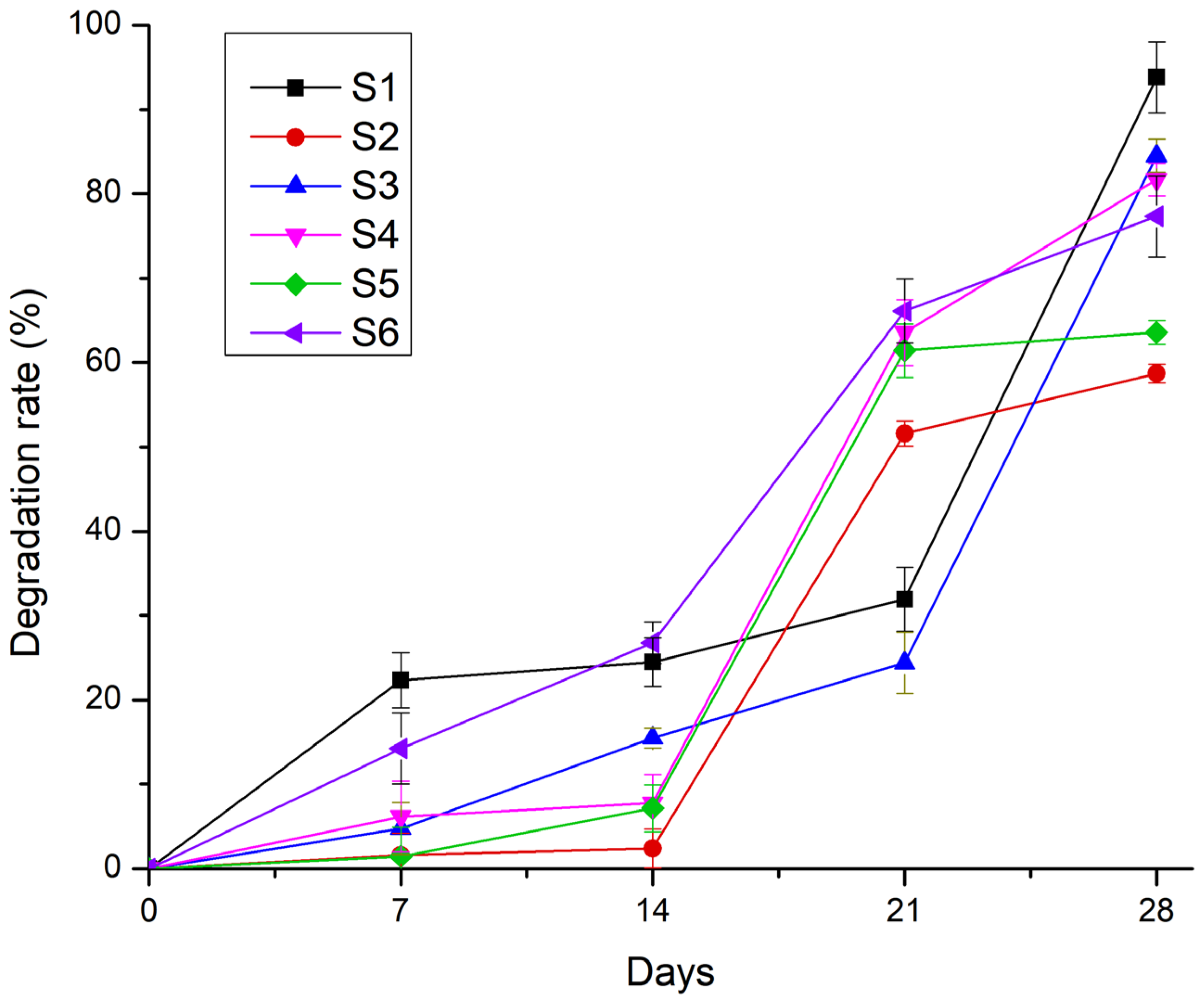
2.2.9. Degradation Rate
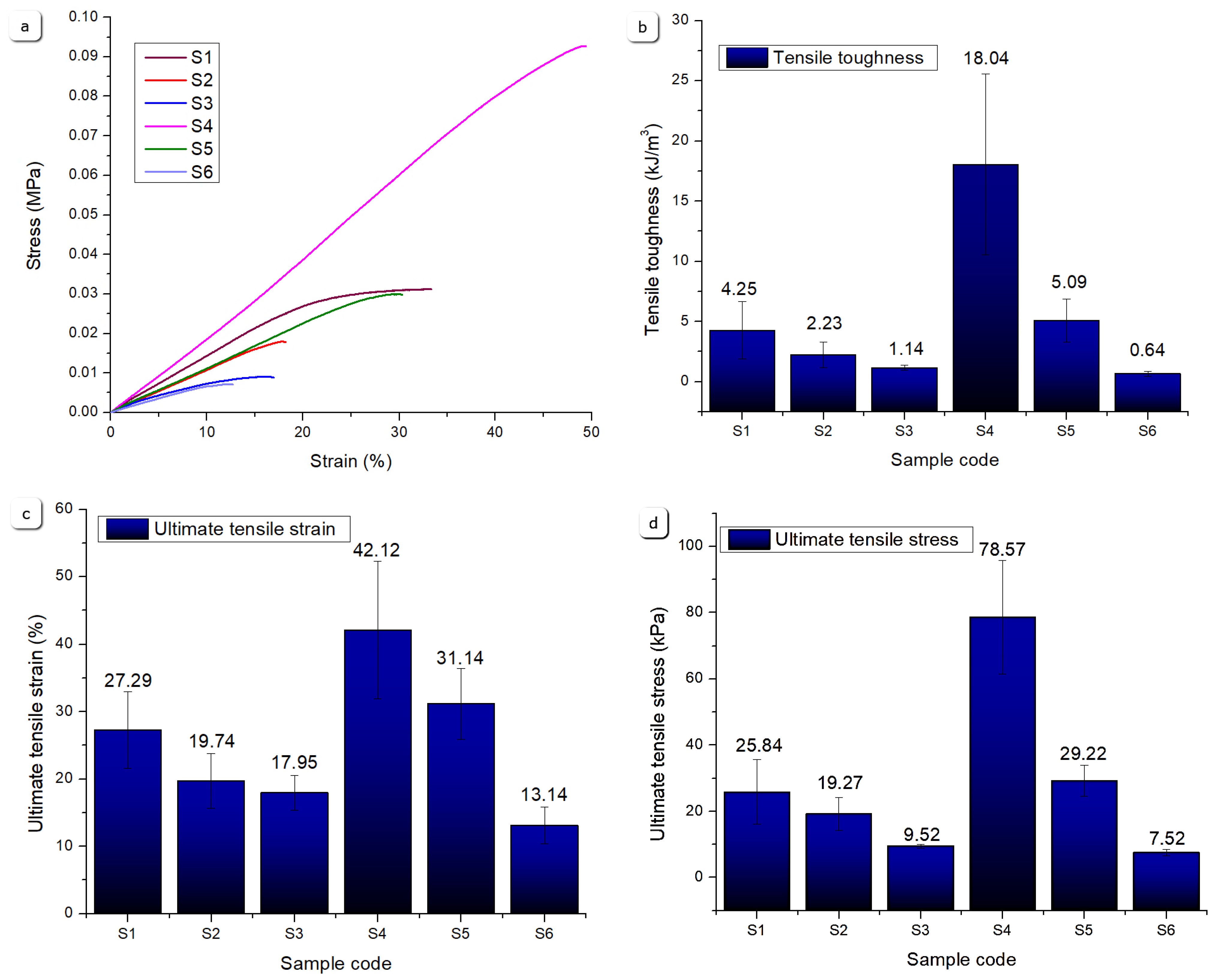
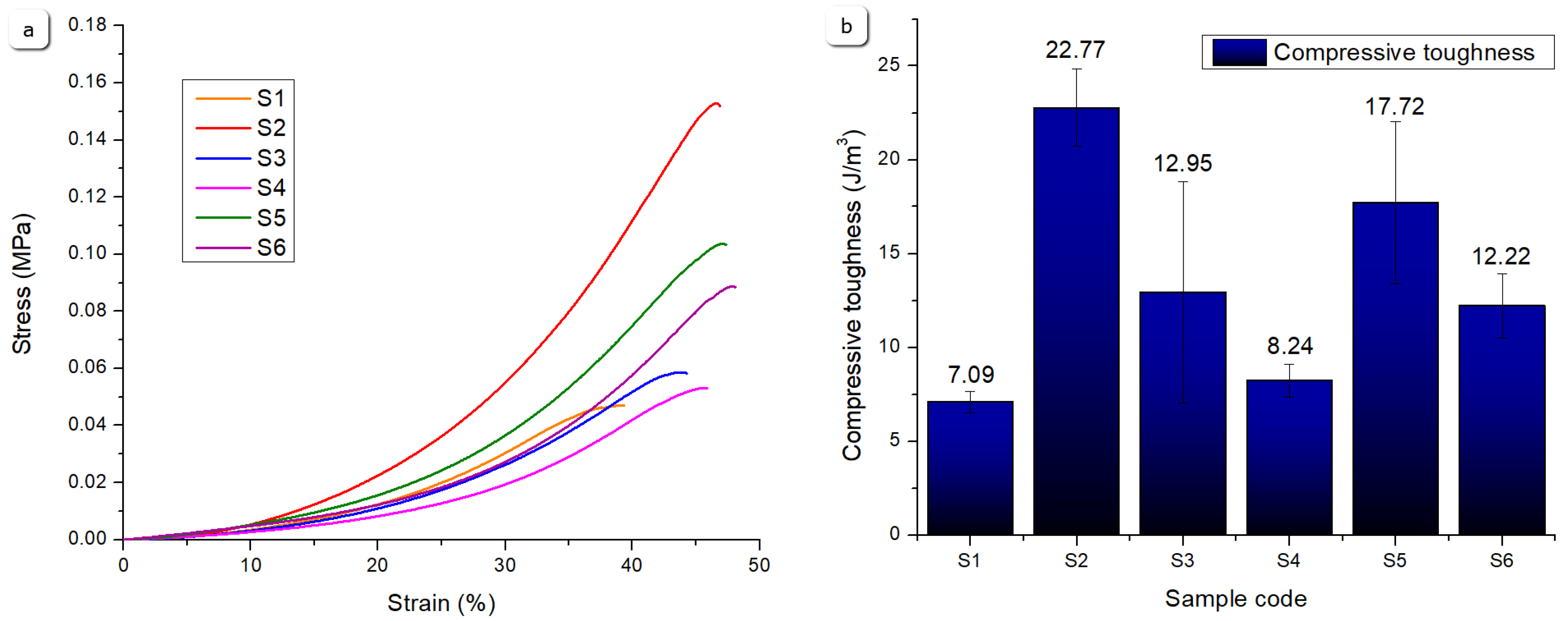
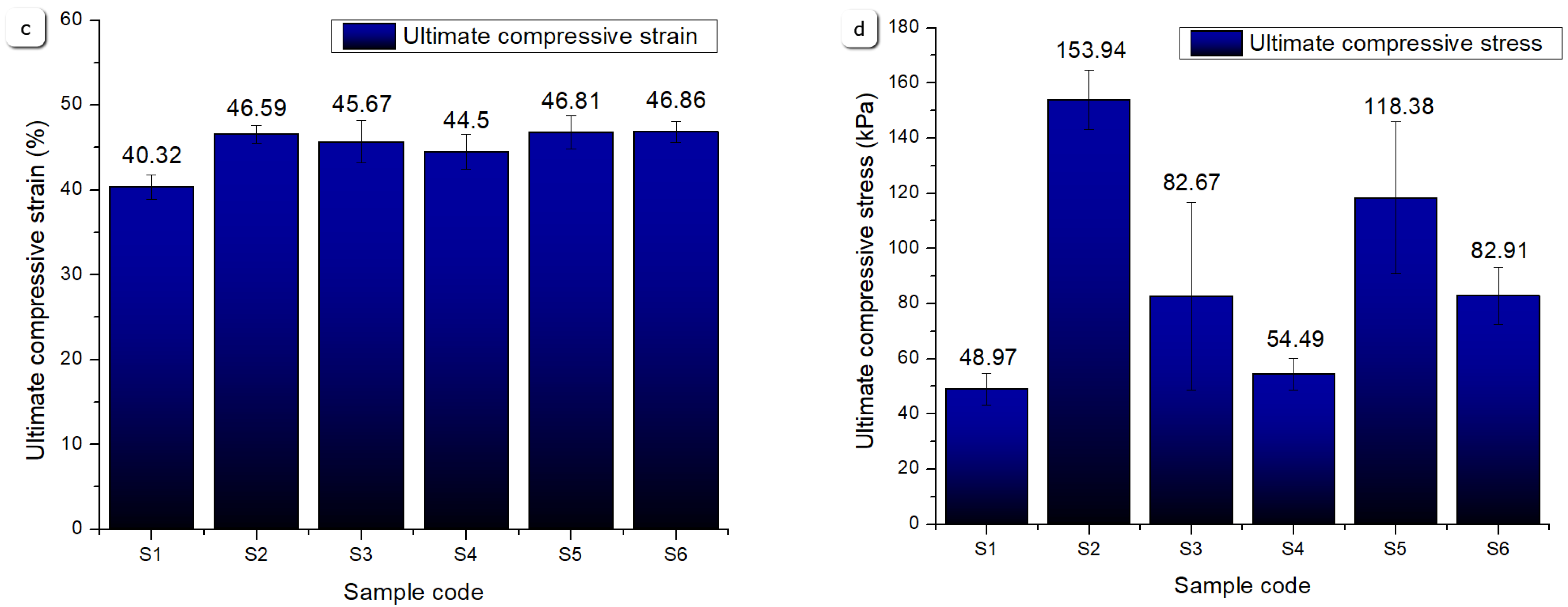
2.2.10. Mechanical Properties
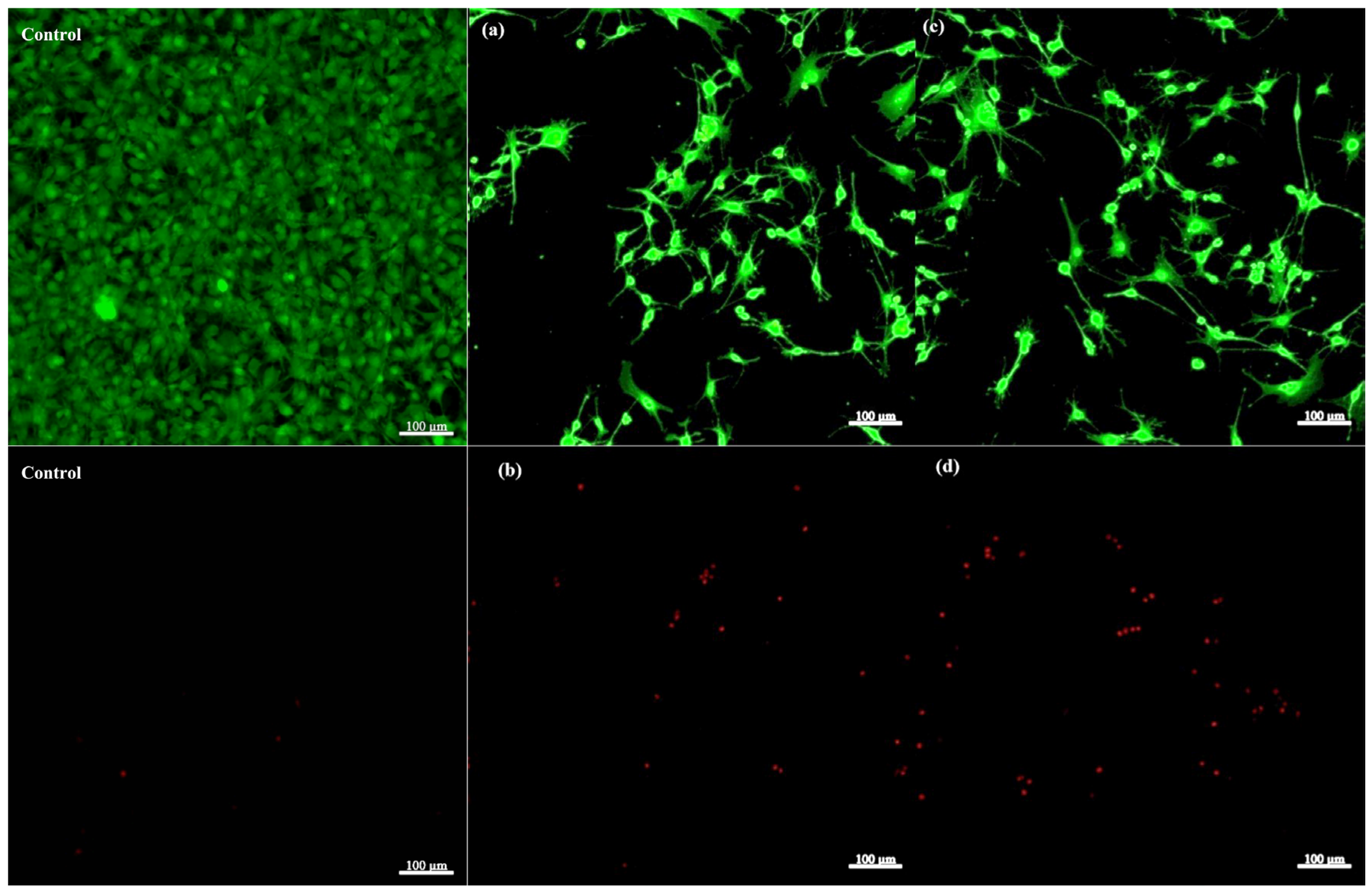
2.2.11. LIVE/DEAD Viability Assay
3. Conclusions
4. Materials and Methods
4.1. Materials
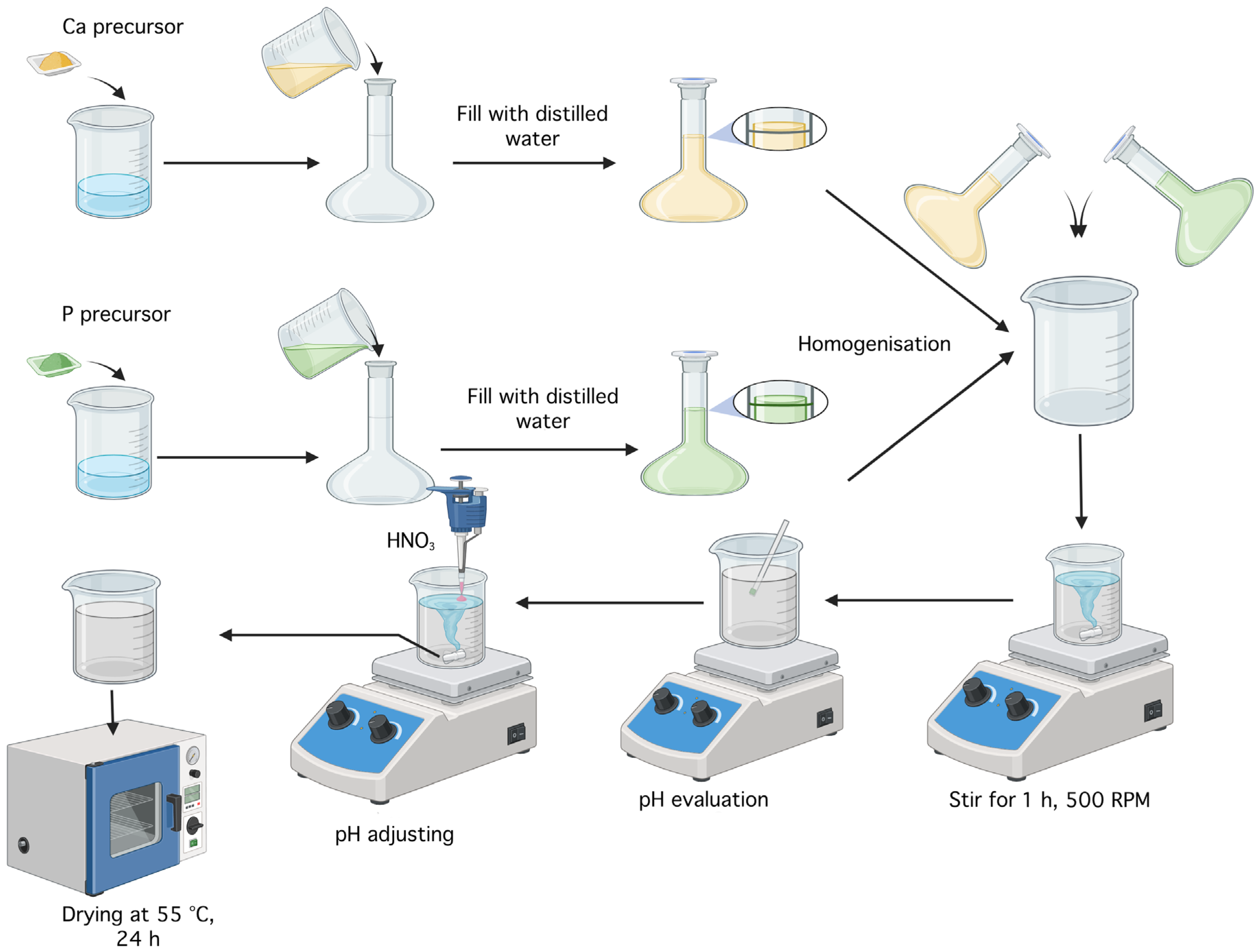
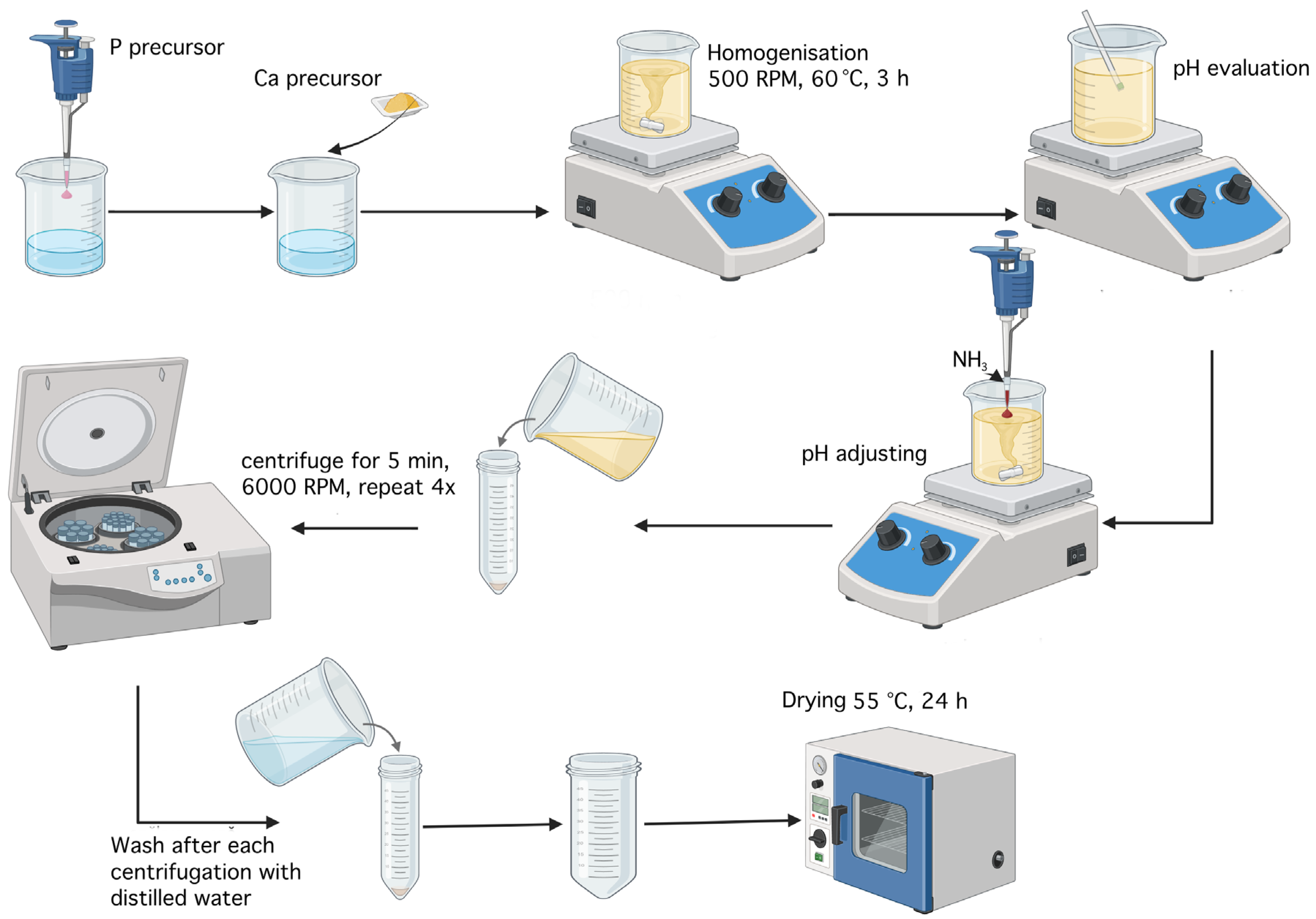
4.2. Synthesis of Calcium Phosphate Powders
4.2.1. Synthesis of Monetite
4.2.2. Synthesis of Brushite
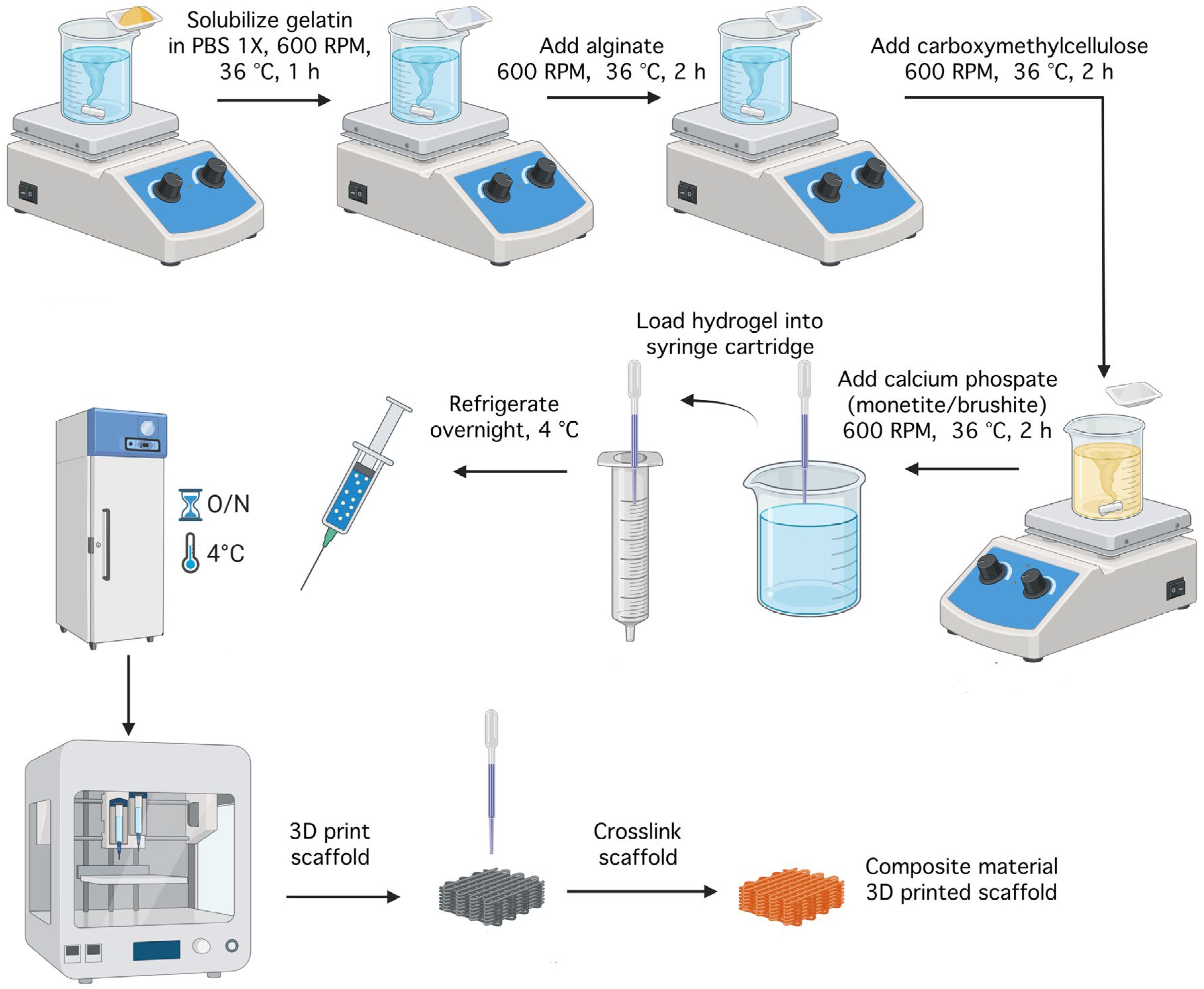
4.3. Synthesis of Hydrogel Compositions
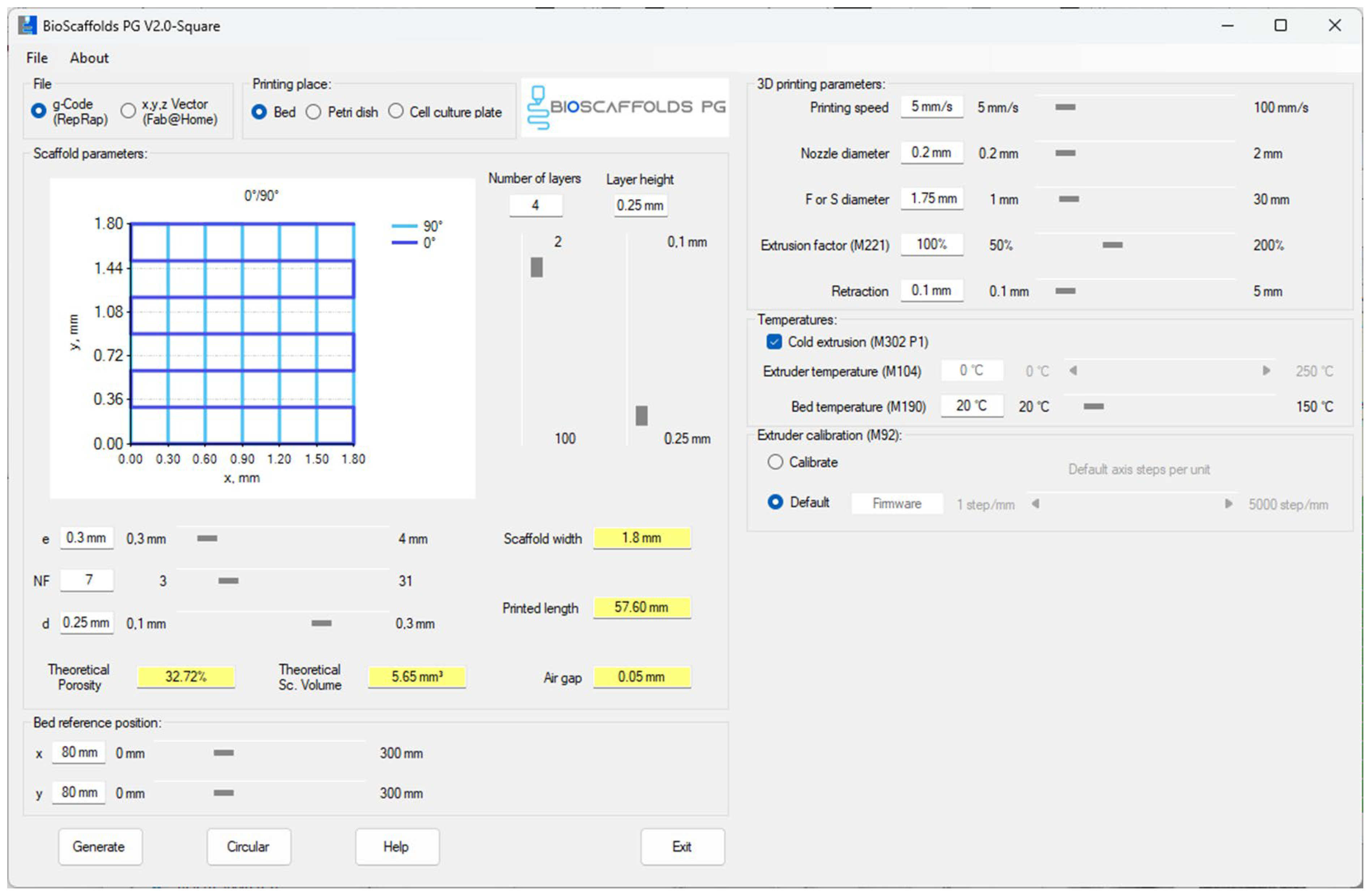
4.4. Three-Dimensional Printing Process
4.5. Characterization Methods
4.5.1. X-Ray Diffraction
4.5.2. Fourier Transform Infrared Spectroscopy
4.5.3. Scanning Electron Microscopy and Energy-Dispersive X-Ray Spectroscopy
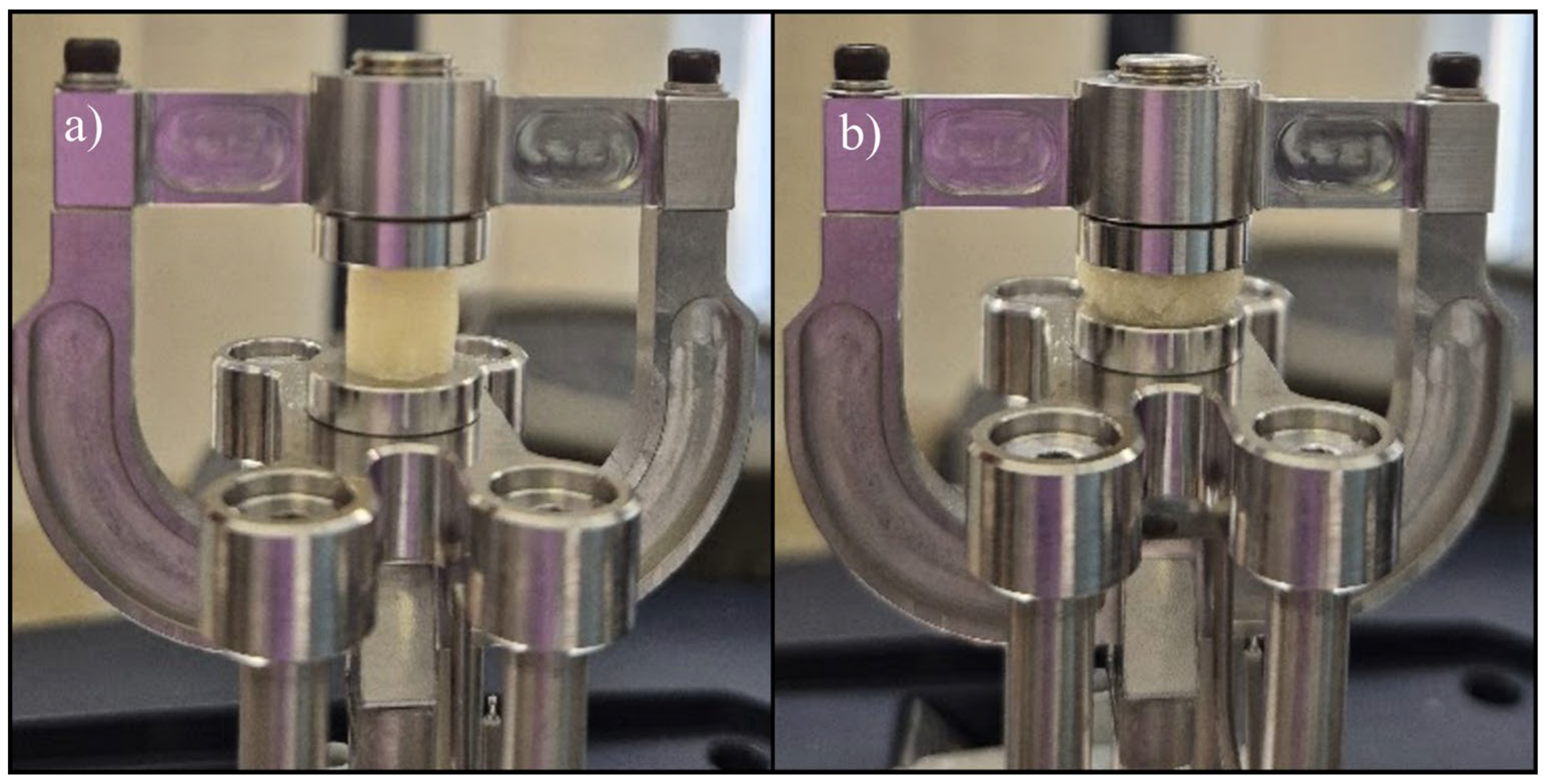
4.5.4. Uniaxial Tensile Test
4.5.5. Uniaxial Compression Test
4.5.6. Rheological Evaluation
4.5.7. Filament Collapse Testing
4.5.8. Three-Dimensional Printing Accuracy
4.5.9. Porosity Evaluation
4.5.10. Swelling Degree
4.5.11. Degradation Rate
4.5.12. In Vitro Mineralization
4.5.13. LIVE/DEAD Viability Assay
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| CaP | Calcium Phosphate |
| Alg | Alginate |
| Gel | Gelatine |
| CMC | Carboxymethylcellulose |
| FTIR | Fourier Transform Infrared Spectroscopy |
| SEM | Scanning Electron Microscopy |
| EDS | Energy-dispersive X-ray Spectroscopy |
| PBS | Phosphate-buffered Saline |
| SBF | Simulated Body Fluid |
| hFOB 1.19 | Human Foetal Osteoblastic Cells |
| DMEM | Dulbecco’s Modified Eagle’s Medium |
References
- Liu, J.; Yang, L.; Liu, K.; Gao, F. Hydrogel scaffolds in bone regeneration: Their promising roles in angiogenesis. Front. Pharmacol. 2023, 14, 1050954. [Google Scholar] [CrossRef] [PubMed]
- Ding, W.; Ge, Y.; Zhang, T.; Zhang, C.; Yin, X. Advanced construction strategies to obtain nanocomposite hydrogels for bone repair and regeneration. NPG Asia Mater. 2024, 16, 14. [Google Scholar] [CrossRef]
- Chen, X.; Wu, T.; Bu, Y.; Yan, H.; Lin, Q. Fabrication and Biomedical Application of Alginate Composite Hydrogels in Bone Tissue Engineering: A Review. Int. J. Mol. Sci. 2024, 25, 7810. [Google Scholar] [CrossRef] [PubMed]
- Ameli, S.; Nourani, M.; Bakhshi, N.; Salemi, B.; Assadpour, E.; Jafari, S.M. Alginate-gelatin composite hydrogels for encapsulating Aloe vera extract; optimization, characterization, and release kinetics. Carbohydr. Polym. Technol. Appl. 2025, 9, 100717. [Google Scholar] [CrossRef]
- Hernández-González, A.C.; Téllez-Jurado, L.; Rodríguez-Lorenzo, L.M. Alginate hydrogels for bone tissue engineering, from injectables to bioprinting: A review. Carbohydr. Polym. 2020, 229, 115514. [Google Scholar] [CrossRef]
- Rather, J.A.; Akhter, N.; Ashraf, Q.S.; Mir, S.A.; Makroo, H.A.; Majid, D.; Barba, F.J.; Khaneghah, A.M.; Dar, B.N. A comprehensive review on gelatin: Understanding impact of the sources, extraction methods, and modifications on potential packaging applications. Food Packag. Shelf Life 2022, 34, 100945. [Google Scholar] [CrossRef]
- Kaliampakou, C.; Lagopati, N.; Pavlatou, E.; Charitidis, C.A. Alginate–Gelatin Hydrogel Scaffolds; An Optimization of Post-Printing Treatment for Enhanced Degradation and Swelling Behavior. Gels 2023, 9, 857. [Google Scholar] [CrossRef]
- Oruc, M.E.; Evcimen Duygulu, N.; Onder, B.; Yelkenci, A.; Ustündag, C.B.; Ciftci, F. Nano-Hydroxyapatite/Poly(methyl methacrylate) Composite Bone Scaffold: Surfactant Surface Effects. Polymers 2025, 17, 1148. [Google Scholar] [CrossRef]
- Boanini, E.; Pagani, S.; Tschon, M.; Rubini, K.; Fini, M.; Bigi, A. Monetite vs. Brushite: Different Influences on Bone Cell Response Modulated by Strontium Functionalization. J. Funct. Biomater. 2022, 13, 65. [Google Scholar] [CrossRef]
- Arif, Z.U.; Khalid, M.Y.; Zolfagharian, A.; Bodaghi, M. 4D bioprinting of smart polymers for biomedical applications: Recent progress, challenges, and future perspectives. React. Funct. Polym. 2022, 179, 105374. [Google Scholar] [CrossRef]
- Khademi, A.; Khandan, A.; Iranmanesh, P.; Heydari, M. Development of a 3D Bioprinted Alginate-Gelatin Hydrogel Scaffold Loaded with Calcium Phosphates for Dental Pulp Tissue Regeneration. Iran. J. Chem. Chem. Eng. 2025, 44, 1–16. [Google Scholar] [CrossRef]
- Cong, B.; Zhang, H. Innovative 3D printing technologies and advanced materials revolutionizing orthopedic surgery: Current applications and future directions. Front. Bioeng. Biotechnol. 2025, 13, 1542179. [Google Scholar] [CrossRef] [PubMed]
- Charbonnier, B.; Hadida, M.; Marchat, D. Additive Manufacturing Serving Bone: Hopes, Reality and Future Challenges for Clinical Applications. Soc. Sci. Res. Netw. 2020, 1, 3674059. [Google Scholar] [CrossRef]
- Rayed, E.; Islam, S.M.; Niha, S.; Jim, J.; Kabir, M.; Mridha, M.F. Deep learning for medical image segmentation: State-of-the-art advancements and challenges. Inform. Med. Unlocked 2024, 47, 101504. [Google Scholar] [CrossRef]
- Bharadwaj, T.; Thomas, A.; Verma, D. Bioprinting. In Applications of 3D Printing in Biomedical Engineering; Springer: Berlin/Heidelberg, Germany, 2021; pp. 45–96. [Google Scholar] [CrossRef]
- Kühl, J.; Gorb, S.; Kern, M.; Klüter, T.; Kühl, S.; Seekamp, A.; Fuchs, S. Extrusion-based 3D printing of osteoinductive scaffolds with a spongiosa-inspired structure. Front. Bioeng. Biotechnol. 2023, 11, 2–5. [Google Scholar] [CrossRef]
- Ma, P.; Wu, W.; Wei, Y.; Ren, L.; Lin, S.; Wu, J. Biomimetic gelatin/chitosan/polyvinyl alcohol/nano-hydroxyapatite scaffolds for bone tissue engineering. Mater. Des. 2021, 207, 109865. [Google Scholar] [CrossRef]
- Laubach, M.; Whyte, S.; Chan, H.F.; Frankenbach-Désor, T.; Mayer-Wagner, S.; Hildebrand, F.; Holzapfel, B.M.; Kneser, U.; Dulleck, U.; Hutmacher, D.W. Lost in translation: The lack of agreement between surgeons and scientists regarding biomaterials research and innovation for treating bone defects. BMC Med. 2024, 22, 517. [Google Scholar] [CrossRef]
- Musculoskeletal Health. Available online: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions (accessed on 18 July 2025).
- Current Advances of Three-Dimensional Bioprinting Application in Dentistry: A Scoping Review. Available online: https://www.mdpi.com/1996-1944/15/18/6398 (accessed on 18 July 2025).
- Nguyen, M.N.-H.; Vu, B.T.; Truong, D.M.; Le, T.D.; Vo, T.-T.T.; Vo, T.V.; Nguyen, T.-H. Fabrication of 3-Dimensional-Printed Bilayered Scaffold Carboxymethyl Chitosan/Oxidized Xanthan Gum, Biphasic Calcium Phosphate for Osteochondral Regeneration. Biomater. Res. 2025, 29, 0186. [Google Scholar] [CrossRef]
- Baniameri, S.; Aminianfar, H.; Gharehdaghi, N.; Yousefi-Koma, A.-A.; Mohaghegh, S.; Nokhbatolfoghahaei, H.; Khojasteh, A. Tissue Engineering 3D-Printed Scaffold Using Allograft/Alginate/Gelatin Hydrogels Coated With Platelet-Rich Fibrin or Adipose Stromal Vascular Fraction Induces Osteogenesis In Vitro. J. Cell. Physiol. 2025, 240, e31497. [Google Scholar] [CrossRef]
- Kotlarz, M.; Ferreira, A.M.; Gentile, P.; Dalgarno, K. Bioprinting of Cell-Laden Hydrogels onto Titanium Alloy Surfaces to Produce a Bioactive Interface. Macromol. Biosci. 2022, 22, 2200071. [Google Scholar] [CrossRef]
- Han, Y.; Jia, X.; Yang, Y.; Guo, P.; Li, C.; Zhang, Y.; Yin, L.; Jia, B.; Wang, H. Study of bioactive 3D-printed scaffolds incorporating zinc-based MOF for bone defect repair and anti-inflammatory applications. Mater. Today Bio 2025, 32, 101884. [Google Scholar] [CrossRef] [PubMed]
- Tharakan, S.; Khondkar, S.; Lee, S.; Ahn, S.; Mathew, C.; Gresita, A.; Hadjiargyrou, M.; Ilyas, A. 3D Printed Osteoblast–Alginate/Collagen Hydrogels Promote Survival, Proliferation and Mineralization at Low Doses of Strontium Calcium Polyphosphate. Pharmaceutics 2022, 15, 11. [Google Scholar] [CrossRef] [PubMed]
- Probing the Structure, Cytocompatibility, and Antimicrobial Efficacy of Silver-, Strontium-, and Zinc-Doped Monetite. ACS Applied Bio Materials. Available online: https://pubs.acs.org/doi/10.1021/acsabm.2c00047 (accessed on 18 July 2025).
- Mukasheva, F.; Moazzam, M.; Yernaimanova, B.; Shehzad, A.; Zhanbassynova, A.; Berillo, D.; Akilbekova, D. Design and Characterization of 3D Printed Pore Gradient Hydrogel Scaffold for Bone Tissue Engineering. Bioprinting 2024, 39, e00341. [Google Scholar] [CrossRef]
- Frontiers. 3D Printed Hybrid Scaffolds for Bone Regeneration Using Calcium Methoxyethoxide as a Calcium Source. Available online: https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1224596/full (accessed on 18 July 2025).
- Ng, P.; Pinho, A.R.; Gomes, M.C.; Demidov, Y.; Krakor, E.; Grume, D.; Herb, M.; Lê, K.; Mano, J.; Mathur, S.; et al. Fabrication of Antibacterial, Osteo-Inductor 3D Printed Aerogel-Based Scaffolds by Incorporation of Drug Laden Hollow Mesoporous Silica Microparticles into the Self-Assembled Silk Fibroin Biopolymer. Macromol. Biosci. 2022, 22, e2100442. [Google Scholar] [CrossRef]
- Peng, B.-Y.; Ou, K.-L.; Liu, C.-M.; Chu, S.-F.; Huang, B.-H.; Cho, Y.-C.; Saito, T.; Tsai, C.-H.; Hung, K.-S.; Lan, W.-C. A Three-Dimensional Bioprinted Copolymer Scaffold with Biocompatibility and Structural Integrity for Potential Tissue Regeneration Applications. Polymers 2022, 14, 3415. [Google Scholar] [CrossRef]
- Hollister, S.; Lin, C.-Y.; Kang, H.; Adachi, T. Computational Design and Simulation of Tissue Engineering Scaffolds. In Virtual Prototyping Bio Manufacturing in Medical Applications; Springer: Berlin/Heidelberg, Germany, 2007; pp. 113–127. [Google Scholar] [CrossRef]
- Wu, Y.; Fuh, J.; Ozbolat, I. Ethical and regulatory concerns of bioprinting. In 3D Bioprinting in Tissue and Organ Regeneration; Academic Press: Cambridge, MA, USA, 2023; pp. 265–288. [Google Scholar] [CrossRef]
- Effect of Temperature and pH on Calcium Phosphate Precipitation. Available online: https://www.researchgate.net/publication/355564100_Effect_of_Temperature_and_pH_on_Calcium_Phosphate_Precipitation (accessed on 18 July 2025).
- Mevellec, J.-Y.; Quillard, S.; Deniard, P.; Mekmene, O.; Gaucheron, F.; Bouler, J.-M.; Buisson, J.-P. Polarized infrared reflectance spectra of brushite (CaHPO4·2H2O) crystal investigation of the phosphate stretching modes. Spectrochim. Acta. A Mol. Biomol. Spectrosc. 2013, 111, 7–13. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Calcium orthophosphates (CaPO4): Occurrence and properties. Prog. Biomater. 2016, 5, 9–70. [Google Scholar] [CrossRef]
- X-Ray Diffraction and Infrared Spectroscopy Data Review Analyses of the Calcium Phosphates. Biointerface Res. Appl. Chem. 2021, 12, 732–755. [CrossRef]
- Xie, J.; Riley, C.; Kumar, M.; Chittur, K. FTIR/ATR study of protein adsorption and brushite transformation to hydroxyapatite. Biomaterials 2002, 23, 3609–3616. [Google Scholar] [CrossRef]
- Trifan, A.; Liciu, E.; Busuioc, C.; Stancu, I.-C.; Banciu, A.; Nicolae, C.; Dragomir, M.; Cristea, D.-D.; Sabău, R.-E.; Nițulescu, D.-A.; et al. Developing Bioengineered 3D-Printed Composite Scaffolds with Antimicrobial Potential for Bone Tissue Regeneration. J. Funct. Biomater. 2025, 16, 227. [Google Scholar] [CrossRef]
- Cooke, M.E.; Rosenzweig, D.H. The rheology of direct and suspended extrusion bioprinting. APL Bioeng. 2021, 5, 011502. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Xu, Y.; Cao, L.; Xiong, L.; Shang, D.; Cong, Y.; Zhao, D.; Wei, X.; Li, J.; Fu, D.; et al. Mechanical and biological properties of 3D printed bone tissue engineering scaffolds. Front. Bioeng. Biotechnol. 2025, 13. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Lian, H.; Huang, Y.; Zhao, D.; Wang, H.; Wang, C.; Li, J.; Ke, L. In vitro genotoxicity evaluation and metabolic study of residual glutaraldehyde in animal-derived biomaterials. Regen. Biomater. 2020, 7, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Teterina, A.Y.; Smirnov, I.V.; Fadeeva, I.S.; Fadeev, R.S.; Smirnova, P.V.; Minaychev, V.V.; Kobyakova, M.I.; Fedotov, A.Y.; Barinov, S.M.; Komlev, V.S. Octacalcium Phosphate for Bone Tissue Engineering: Synthesis, Modification, and In Vitro Biocompatibility Assessment. Int. J. Mol. Sci. 2021, 22, 12747. [Google Scholar] [CrossRef]
- Yokoi, T.; Watanabe, M.; Goto, T.; Meng, S.; Sekino, T.; Shimabukuro, M.; Kawashita, M. Synthesis of Octacalcium Phosphate Containing Glutarate Ions with a High Incorporation Fraction. Materials 2023, 16, 64. [Google Scholar] [CrossRef]
- Dávila, J.L.; Manzini, B.M.; Lopes da Fonsêca, J.H.; Mancilla Corzo, I.J.; Neto, P.I.; Aparecida de Lima Montalvão, S.; Annichino-Bizzacchi, J.M.; Akira d’Ávila, M.; Lopes da Silva, J.V. A parameterized g-code compiler for scaffolds 3D bioprinting. Bioprinting 2022, 27, e00222. [Google Scholar] [CrossRef]
- Feyissa, Z.; Edossa, G.D.; Gupta, N.K.; Negera, D. Development of double crosslinked sodium alginate/chitosan based hydrogels for controlled release of metronidazole and its antibacterial activity. Heliyon 2023, 9, e20144. [Google Scholar] [CrossRef]
- D3039/D3039M Standard Test Method for Tensile Properties of Polymer Matrix Composite Materials. Available online: https://store.astm.org/d3039_d3039m-08.html (accessed on 18 July 2025).
- Schindelin, J.; Arganda-Carreras, I.; Frise, E.; Kaynig, V.; Longair, M.; Pietzsch, T.; Preibisch, S.; Rueden, C.; Saalfeld, S.; Schmid, B.; et al. Fiji: An open-source platform for biological-image analysis. Nat. Methods 2012, 9, 676–682. [Google Scholar] [CrossRef]
- Baino, F.; Yamaguchi, S. The Use of Simulated Body Fluid (SBF) for Assessing Materials Bioactivity in the Context of Tissue Engineering: Review and Challenges. Biomimetics 2020, 5, 57. [Google Scholar] [CrossRef]
- Kokubo, T.; Kushitani, H.; Sakka, S.; Kitsugi, T.; Yamamuro, T. Solutions able to reproduce in vivo surface-structure changes in bioactive glass-ceramic A-W3. J. Biomed. Mater. Res. 1990, 24, 721–734. [Google Scholar] [CrossRef]
- GEO Accession Viewer. Available online: https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSM7026701 (accessed on 18 July 2025).
- LIVE/DEAD Viability/Cytotoxicity Kit for Mammalian Cells—RO. Available online: https://www.thermofisher.com/tr/en/home/references/protocols/cell-and-tissue-analysis/protocols/live-dead-viability-cytotoxicity-kit-for-mammalian-cells.html (accessed on 18 July 2025).





| Sample | Gelatine (%) | Alginate (%) | CMC (%) | Monetite (%) | Brushite (%) | Printing Pressure (kPa) | Printing Speed (mm/s) | Nozzle Diameter | Crosslinking |
|---|---|---|---|---|---|---|---|---|---|
| S1 | 8 | 7 | 1 | 0 | 0 | 220 | 5 | 25G (260 µm) | 1.66% CaCl2 0.5% glutaraldehyde 3% citric acid–15 min |
| S2 | 8 | 7 | 1 | 5 | 0 | 263 | |||
| S3 | 8 | 7 | 1 | 0 | 5 | 195 | |||
| S4 | 12 | 5 | 1 | 0 | 0 | 283 | |||
| S5 | 12 | 5 | 1 | 3 | 0 | 274 | |||
| S6 | 12 | 5 | 1 | 0 | 3 | 231 | 22G (400 µm) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trifan, A.; Liciu, E.; Nedelcu, A.-S.; Dragomir, M.; Cristea, D.-D.; Mateescu, C.-Ș.; Nițulescu, D.-A.; Cîrstea, C.-A.-M.; Banciu, A.; Toader, G.; et al. Effect of Phosphate Phase Incorporation on 3D-Printed Hydrogel Scaffolds: Towards Customizable Bone Graft Materials. Gels 2025, 11, 665. https://doi.org/10.3390/gels11080665
Trifan A, Liciu E, Nedelcu A-S, Dragomir M, Cristea D-D, Mateescu C-Ș, Nițulescu D-A, Cîrstea C-A-M, Banciu A, Toader G, et al. Effect of Phosphate Phase Incorporation on 3D-Printed Hydrogel Scaffolds: Towards Customizable Bone Graft Materials. Gels. 2025; 11(8):665. https://doi.org/10.3390/gels11080665
Chicago/Turabian StyleTrifan, Andreea, Eduard Liciu, Andrei-Silviu Nedelcu, Mihai Dragomir, Doru-Daniel Cristea, Ciprian-Ștefan Mateescu, David-Andrei Nițulescu, Cătălina-Ana-Maria Cîrstea, Adela Banciu, Gabriela Toader, and et al. 2025. "Effect of Phosphate Phase Incorporation on 3D-Printed Hydrogel Scaffolds: Towards Customizable Bone Graft Materials" Gels 11, no. 8: 665. https://doi.org/10.3390/gels11080665
APA StyleTrifan, A., Liciu, E., Nedelcu, A.-S., Dragomir, M., Cristea, D.-D., Mateescu, C.-Ș., Nițulescu, D.-A., Cîrstea, C.-A.-M., Banciu, A., Toader, G., Diacon, A., & Busuioc, C. (2025). Effect of Phosphate Phase Incorporation on 3D-Printed Hydrogel Scaffolds: Towards Customizable Bone Graft Materials. Gels, 11(8), 665. https://doi.org/10.3390/gels11080665