Hydrogels in Veterinary Vaccine Development: Types, Mechanisms, and Applications
Abstract
1. Background
2. Hydrogel
2.1. Types and Applications of Hydrogels
2.2. Loading of the Hydrogel
2.3. The Physicochemical Properties of Hydrogels
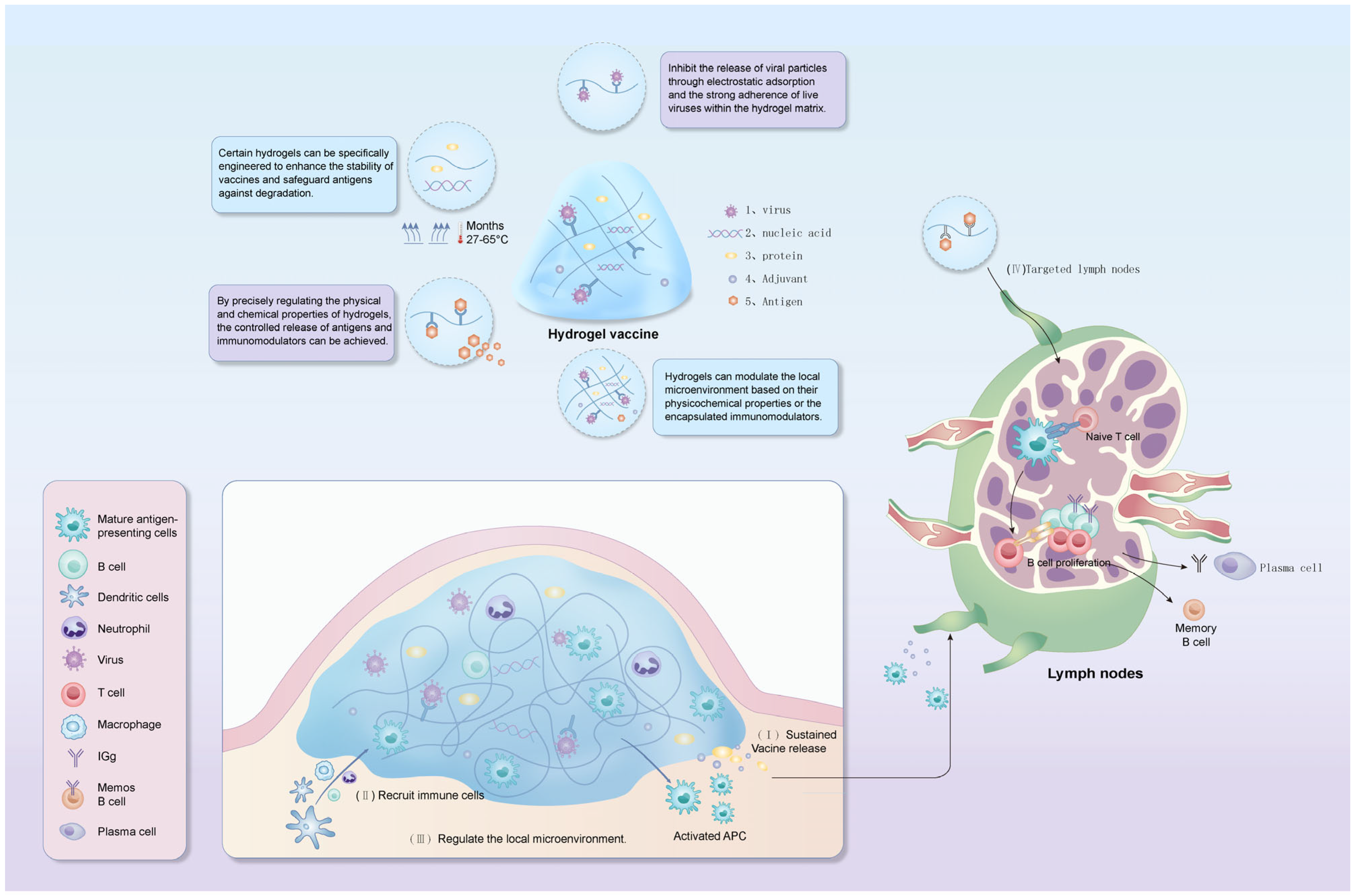
3. Strategies for Priming the Immune Response with Hydrogel-Based Vaccines
3.1. Prolonged Antigen Release
3.2. Enhancement of Phagocytosis and Antigen Presentation by Phagocytes
3.3. Regulation of the Local Inflammatory Response
3.4. Precise Release in Time and Space
4. Technological Innovations and Prospects in the Context of Veterinary Vaccines
4.1. Technological Innovation of Cold Chain Substitution
4.2. Solutions for Intensive Farming
| Hydrogel Category | Representative Materials | Advantages | Limitations | Suitable Vaccine Types | References |
|---|---|---|---|---|---|
| Coccidiosis vaccine | Eimeria spp. | Carrageenan/alginate composite hydrogel | Oral (microencapsulation) | 2.3–2.5 mm gel beads protect oocysts, enhancing stability during storage | [85] |
| Rabies vaccine | Rabies virus | Metal-phenolic network (MPN) hydrogel | Subcutaneous injection | Single-dose immunization achieves 4.3× higher neutralizing antibodies | [27,28] |
| Newcastle disease vaccine | Newcastle disease virus (NDV) | Modified starch hydrogel | Liquid formulation | Maintains viral titer stability (<0.5 log10 EID50 loss) at 37 °C | [67] |
| H7N9 avian influenza vaccine | H7N9 influenza virus | Tetrapeptide hydrogel | Intramuscular injection | Increases micro-neutralization and hemagglutination inhibition (HI) titers in mice | [52] |
| Porcine epidemic diarrhea (PED) | PED virus | Alginate-chitosan hydrogel | Oral administration | Induces sustained mucosal IgA/IgG responses in mice (200%↑ vs. free antigen) | [80] |
| PRRSV vaccine | Porcine reproductive and respiratory syndrome virus | Thermosensitive hydrogel | Intranasal spray | Forms “mucosal mask” to prolong antigen retention in nasal epithelium | [77] |
| Canine rabies vaccine | Rabies virus | Thermo-responsive chitosan hydrogel | Subcutaneous injection | Generates 327.40 IU/mL neutralizing antibodies (200×↑ vs. liquid vaccine) | [87] |
| Feline coronavirus vaccine | Feline coronavirus | mRNA-LNP hydrogel composite | Under investigation | Demonstrates rapid antigen expression capability | [86] |
| Universal vaccine platform | Multi-pathogen | Reversible PEG-based hydrogel | Injectable depot | Stabilizes biologics at 65 °C via dynamic boronate crosslinking | [65] |
| DNA hydrogel vaccine | Toxin antigens | CpG-embedded DNA hydrogel | Subcutaneous injection | Enhances humoral/cellular immunity through TLR9 activation | [69] |
4.3. Upgrade to Companion Animal Vaccines
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Verma, S.; Malik, Y.S.; Singh, G.; Dhar, P.; Singla, A.K. Core Competencies of a Veterinary Graduate; Springer Nature: Singapore, 2024; ISBN 978-981-97-0432-3. [Google Scholar]
- Sander, V.A.; Sánchez López, E.F.; Mendoza Morales, L.; Ramos Duarte, V.A.; Corigliano, M.G.; Clemente, M. Use of Veterinary Vaccines for Livestock as a Strategy to Control Foodborne Parasitic Diseases. Front. Cell. Infect. Microbiol. 2020, 10, 288. [Google Scholar] [CrossRef] [PubMed]
- Monath, T.P. Vaccines against Diseases Transmitted from Animals to Humans: A One Health Paradigm. Vaccine 2013, 31, 5321–5338. [Google Scholar] [CrossRef]
- Dumpa, N.; Goel, K.; Guo, Y.; McFall, H.; Pillai, A.R.; Shukla, A.; Repka, M.A.; Murthy, S.N. Stability of Vaccines. AAPS PharmSciTech 2019, 20, 42. [Google Scholar] [CrossRef]
- Clénet, D. Accurate Prediction of Vaccine Stability under Real Storage Conditions and during Temperature Excursions. Eur. J. Pharm. Biopharm. 2018, 125, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Gershwin, L.J. Adverse Reactions to Vaccination. Vet. Clin. N. Am. Small Anim. Pract. 2018, 48, 279–290. [Google Scholar] [CrossRef]
- Amadori, M.; Zanotti, C. Immunoprophylaxis in Intensive Farming Systems: The Way Forward. Vet. Immunol. Immunopathol. 2016, 181, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Rana, M.M.; Demirkaya, C.; De La Hoz Siegler, H. Beyond Needles: Immunomodulatory Hydrogel-Guided Vaccine Delivery Systems. Gels 2024, 11, 7. [Google Scholar] [CrossRef]
- Bustamante-Torres, M.; Romero-Fierro, D.; Arcentales-Vera, B.; Palomino, K.; Magaña, H.; Bucio, E. Hydrogels Classification According to the Physical or Chemical Interactions and as Stimuli-Sensitive Materials. Gels 2021, 7, 182. [Google Scholar] [CrossRef]
- Kohar, R.; Ghosh, M.; Sawale, J.A.; Singh, A.; Rangra, N.K.; Bhatia, R. Insights into Translational and Biomedical Applications of Hydrogels as Versatile Drug Delivery Systems. AAPS PharmSciTech 2024, 25, 17. [Google Scholar] [CrossRef]
- Wu, Y.; Wei, W.; Zhou, M.; Wang, Y.; Wu, J.; Ma, G.; Su, Z. Thermal-Sensitive Hydrogel as Adjuvant-Free Vaccine Delivery System for H5N1 Intranasal Immunization. Biomaterials 2012, 33, 2351–2360. [Google Scholar] [CrossRef]
- Wei, J.; Xue, W.; Yu, X.; Qiu, X.; Liu, Z. pH Sensitive Phosphorylated Chitosan Hydrogel as Vaccine Delivery System for Intramuscular Immunization. J. Biomater. Appl. 2017, 31, 1358–1369. [Google Scholar] [CrossRef]
- Yuan, N.; Shao, K.; Huang, S.; Chen, C. Chitosan, Alginate, Hyaluronic Acid and Other Novel Multifunctional Hydrogel Dressings for Wound Healing: A Review. Int. J. Biol. Macromol. 2023, 240, 124321. [Google Scholar] [CrossRef] [PubMed]
- Phutane, P.; Telange, D.; Agrawal, S.; Gunde, M.; Kotkar, K.; Pethe, A. Biofunctionalization and Applications of Polymeric Nanofibers in Tissue Engineering and Regenerative Medicine. Polymers 2023, 15, 1202. [Google Scholar] [CrossRef] [PubMed]
- Kłosiński, K.K.; Wach, R.A.; Girek-Bąk, M.K.; Rokita, B.; Kołat, D.; Kałuzińska-Kołat, Ż.; Kłosińska, B.; Duda, Ł.; Pasieka, Z.W. Biocompatibility and Mechanical Properties of Carboxymethyl Chitosan Hydrogels. Polymers 2022, 15, 144. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Ren, C.; Shang, Y.; Yang, C.; Guo, Q.; Chu, L.; Liu, J. Co-Assembled Supramolecular Nanofibers with Tunable Surface Properties for Efficient Vaccine Delivery. Front. Chem. 2020, 8, 500. [Google Scholar] [CrossRef] [PubMed]
- Bordbar-Khiabani, A.; Gasik, M. Smart Hydrogels for Advanced Drug Delivery Systems. Int. J. Mol. Sci. 2022, 23, 3665. [Google Scholar] [CrossRef]
- Lai, Y.; Wang, S.; Shen, X.; Qi, R.; Liu, T.; Du, F.; YuHe, Y.; Miao, B.; Zhai, J.; Zhang, Y.; et al. An Injectable Chitosan Hydrochloride-Sodium Alginate Hydrogel Adjuvant Capable of Eliciting Potent Humoral and Cellular Immunity. ACS Appl. Mater. Interfaces 2025, 17, 14444–14459. [Google Scholar] [CrossRef]
- Verheul, R.J.; Slütter, B.; Bal, S.M.; Bouwstra, J.A.; Jiskoot, W.; Hennink, W.E. Covalently Stabilized Trimethyl Chitosan-Hyaluronic Acid Nanoparticles for Nasal and Intradermal Vaccination. J. Control. Release 2011, 156, 46–52. [Google Scholar] [CrossRef]
- Ruan, X.; Hu, J.; Lu, L.; Wang, Y.; Tang, C.; Liu, F.; Gao, X.; Zhang, L.; Wu, H.; Huang, X.; et al. Poloxamer 407/188 Binary Thermosensitive Gel as a Moxidectin Delivery System: In Vitro Release and In Vivo Evaluation. Molecules 2022, 27, 3063. [Google Scholar] [CrossRef]
- Yin, Y.; Li, X.; Ma, H.; Zhang, J.; Yu, D.; Zhao, R.; Yu, S.; Nie, G.; Wang, H. In Situ Transforming RNA Nanovaccines from Polyethylenimine Functionalized Graphene Oxide Hydrogel for Durable Cancer Immunotherapy. Nano Lett. 2021, 21, 2224–2231. [Google Scholar] [CrossRef]
- Merino, S.; Martín, C.; Kostarelos, K.; Prato, M.; Vázquez, E. Nanocomposite Hydrogels: 3D Polymer–Nanoparticle Synergies for On-Demand Drug Delivery. ACS Nano 2015, 9, 4686–4697. [Google Scholar] [CrossRef]
- Shoukat, H.; Buksh, K.; Noreen, S.; Pervaiz, F.; Maqbool, I. Hydrogels as Potential Drug-Delivery Systems: Network Design and Applications. Ther. Deliv. 2021, 12, 375–396. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, Y.; Fu, Y.; Wang, N.; Liu, Q.; Zhao, S.; Yang, H.Y.; Liu, C. Fabrication of Temperature and pH Dual-Sensitive Semi-Interpenetrating Network Hydrogel with Enhanced Adhesion and Antibacterial Properties. Polymer 2025, 326, 128343. [Google Scholar] [CrossRef]
- Zubris, K.A.V.; Colson, Y.L.; Grinstaff, M.W. Hydrogels as Intracellular Depots for Drug Delivery. Mol. Pharm. 2012, 9, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S.; Nair, A.B.; Shah, J.; Sreeharsha, N.; Gupta, S.; Shinu, P. Emerging Role of Hydrogels in Drug Delivery Systems, Tissue Engineering and Wound Management. Pharmaceutics 2021, 13, 357. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Xi, Z.; Fan, C.; Mei, Y.; Zhao, J.; Jiang, Y.; Zhao, M.; Xu, L. Hydrogels for Nucleic Acid Drugs Delivery. Adv. Healthc. Mater. 2024, 13, 2401895. [Google Scholar] [CrossRef]
- He, P.; Dai, L.; Wei, J.; Zhu, X.; Li, J.; Chen, Z.; Ni, Y. Nanocellulose-Based Hydrogels as Versatile Drug Delivery Vehicles: A Review. Int. J. Biol. Macromol. 2022, 222, 830–843. [Google Scholar] [CrossRef]
- Hao, H.; Wu, S.; Lin, J.; Zheng, Z.; Zhou, Y.; Zhang, Y.; Guo, Q.; Tian, F.; Zhao, M.; Chen, Y.; et al. Immunization against Zika by Entrapping Live Virus in a Subcutaneous Self-Adjuvanting Hydrogel. Nat. Biomed. Eng. 2023, 7, 928–942. [Google Scholar] [CrossRef]
- Song, H.; Su, Q.; Nie, Y.; Zhang, C.; Huang, P.; Shi, S.; Liu, Q.; Wang, W. Supramolecular Assembly of a Trivalent Peptide Hydrogel Vaccine for Cancer Immunotherapy. Acta Biomater. 2023, 158, 535–546. [Google Scholar] [CrossRef]
- Bayon, J.L.; Shih, C.; Craig, S.L.; Steinmetz, N.F. A Simple Swell-and-Click Method for the Covalent Attachment of Virus-like Particles to Polymer Hydrogels. Mater. Today Chem. 2024, 38, 102100. [Google Scholar] [CrossRef]
- Deng, J.; Wang, Z.; Wu, L.; Song, Z.; Bahlol, H.S.; Li, X.; Zhao, L.; Han, H. Metal–Phenolic Network Hydrogel Vaccine Platform for Enhanced Humoral Immunity against Lethal Rabies Virus. ACS Nano 2025, 19, 9042–9052. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.; Duong, V.T.; Shalash, A.O.; Skwarczynski, M.; Toth, I. Chemical Conjugation Strategies for the Development of Protein-Based Subunit Nanovaccines. Vaccines 2021, 9, 563. [Google Scholar] [CrossRef] [PubMed]
- Biondi, M.; Borzacchiello, A.; Mayol, L.; Ambrosio, L. Nanoparticle-Integrated Hydrogels as Multifunctional Composite Materials for Biomedical Applications. Gels 2015, 1, 162–178. [Google Scholar] [CrossRef]
- He, W.; Wang, Y.; Li, X.; Ji, Y.; Yuan, J.; Yang, W.; Yan, S.; Yan, J. Sealing the Pandora’s Vase of Pancreatic Fistula through Entrapping the Digestive Enzymes within a Dextrorotary (D)-Peptide Hydrogel. Nat. Commun. 2024, 15, 7235. [Google Scholar] [CrossRef]
- Sepe, F.; Valentino, A.; Marcolongo, L.; Petillo, O.; Conte, R.; Margarucci, S.; Peluso, G.; Calarco, A. Marine-Derived Polysaccharide Hydrogels as Delivery Platforms for Natural Bioactive Compounds. Int. J. Mol. Sci. 2025, 26, 764. [Google Scholar] [CrossRef]
- Liu, Y.; Yin, Y.; Wang, L.; Zhang, W.; Chen, X.; Yang, X.; Xu, J.; Ma, G. Surface Hydrophobicity of Microparticles Modulates Adjuvanticity. J. Mater. Chem. B 2013, 1, 3888. [Google Scholar] [CrossRef]
- Wu, C.; Zhang, H.; Guo, Y.; Sun, X.; Hu, Z.; Teng, L.; Zeng, Z. Porous Hydrogels for Immunomodulatory Applications. Int. J. Mol. Sci. 2024, 25, 5152. [Google Scholar] [CrossRef] [PubMed]
- Fenton, O.S.; Tibbitt, M.W.; Appel, E.A.; Jhunjhunwala, S.; Webber, M.J.; Langer, R. Injectable Polymer–Nanoparticle Hydrogels for Local Immune Cell Recruitment. Biomacromolecules 2019, 20, 4430–4436. [Google Scholar] [CrossRef]
- Shi, Z.; Gao, Z.; Zhuang, X.; Si, X.; Huang, Z.; Di, Y.; Ma, S.; Guo, Z.; Li, C.; Jin, N.; et al. Dynamic Covalent Hydrogel as a Single-Dose Vaccine Adjuvant for Sustained Antigen Release and Significantly Elevated Humoral Immunity. Adv. Healthc. Mater. 2024, 13, 2400886. [Google Scholar] [CrossRef]
- Kim, E.-H.; Wahl, K.; Guelfi, E.; Lee, D. Engineering the Physical Characteristics of Biomaterials for Innate Immune-Mediated Cancer Immunotherapy. J. Control. Release 2025, 378, 814–830. [Google Scholar] [CrossRef]
- Palgen, J.-L.; Tchitchek, N.; Elhmouzi-Younes, J.; Delandre, S.; Namet, I.; Rosenbaum, P.; Dereuddre-Bosquet, N.; Martinon, F.; Cosma, A.; Lévy, Y.; et al. Prime and Boost Vaccination Elicit a Distinct Innate Myeloid Cell Immune Response. Sci. Rep. 2018, 8, 3087. [Google Scholar] [CrossRef]
- Watson, B.; Viner, K. How the Immune Response to Vaccines Is Created, Maintained and Measured: Addressing Patient Questions About Vaccination. Prim. Care Clin. Off. Pract. 2011, 38, 581–593. [Google Scholar] [CrossRef] [PubMed]
- Tanner, R.; Villarreal-Ramos, B.; Vordermeier, H.M.; McShane, H. The Humoral Immune Response to BCG Vaccination. Front. Immunol. 2019, 10, 1317. [Google Scholar] [CrossRef] [PubMed]
- Linares-Fernández, S.; Lacroix, C.; Exposito, J.-Y.; Verrier, B. Tailoring mRNA Vaccine to Balance Innate/Adaptive Immune Response. Trends Mol. Med. 2020, 26, 311–323. [Google Scholar] [CrossRef]
- Salvador, A.; Igartua, M.; Hernández, R.M.; Pedraz, J.L. Combination of Immune Stimulating Adjuvants with Poly(Lactide-Co-Glycolide) Microspheres Enhances the Immune Response of Vaccines. Vaccine 2012, 30, 589–596. [Google Scholar] [CrossRef]
- Hallengärd, D.; Applequist, S.E.; Nyström, S.; Maltais, A.-K.; Marovich, M.; Moss, B.; Earl, P.; Nihlmark, K.; Wahren, B.; Bråve, A. Immunization with Multiple Vaccine Modalities Induce Strong HIV-Specific Cellular and Humoral Immune Responses. Viral Immunol. 2012, 25, 423–432. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y.; Ho, M.; Hu, Y.; Shi, Y. Vaccine Adjuvants: Current Status, Research and Development, Licensing, and Future Opportunities. J. Mater. Chem. B 2024, 12, 4118–4137. [Google Scholar] [CrossRef]
- Charerntantanakul, W. Adjuvants for Swine Vaccines: Mechanisms of Actions and Adjuvant Effects. Vaccine 2020, 38, 6659–6681. [Google Scholar] [CrossRef]
- Shao, Y.; Sun, Z.-Y.; Wang, Y.; Zhang, B.-D.; Liu, D.; Li, Y.-M. Designable Immune Therapeutical Vaccine System Based on DNA Supramolecular Hydrogels. ACS Appl. Mater. Interfaces 2018, 10, 9310–9314. [Google Scholar] [CrossRef]
- Noh, K.H.; Park, Y.M.; Kim, H.S.; Kang, T.H.; Song, K.-H.; Lee, Y.-H.; Byeon, Y.; Jeon, H.N.; Jung, I.D.; Shin, B.C.; et al. GM-CSF-Loaded Chitosan Hydrogel as an Immunoadjuvant Enhances Antigen-Specific Immune Responses with Reduced Toxicity. BMC Immunol. 2014, 15, 48. [Google Scholar] [CrossRef]
- Pérez-Luna, V.H.; González-Reynoso, O. Encapsulation of Biological Agents in Hydrogels for Therapeutic Applications. Gels 2018, 4, 61. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Liang, J.; Dong, X.; Wang, C.; Kong, D.; Lv, F. Injectable Hydrogels Coencapsulating Granulocyte-Macrophage Colony-Stimulating Factor and Ovalbumin Nanoparticles to Enhance Antigen Uptake Efficiency. ACS Appl. Mater. Interfaces 2018, 10, 20315–20325. [Google Scholar] [CrossRef] [PubMed]
- Miura, R.; Sawada, S.; Mukai, S.; Sasaki, Y.; Akiyoshi, K. Antigen Delivery to Antigen-Presenting Cells for Adaptive Immune Response by Self-Assembled Anionic Polysaccharide Nanogel Vaccines. Biomacromolecules 2020, 21, 621–629. [Google Scholar] [CrossRef]
- Kapadia, C.H.; Tian, S.; Perry, J.L.; Sailer, D.; Christopher Luft, J.; DeSimone, J.M. Extending Antigen Release from Particulate Vaccines Results in Enhanced Antitumor Immune Response. J. Control. Release 2018, 269, 393–404. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Ji, H.; Peng, L.; Gao, X.; Jiang, S. Development of PLGA-PEG-PLGA Hydrogel Delivery System for Enhanced Immunoreaction and Efficacy of Newcastle Disease Virus DNA Vaccine. Molecules 2020, 25, 2505. [Google Scholar] [CrossRef]
- Li, H.; Liang, X.; Sun, W.; Zhuang, B.; Cao, Y.; Zhang, J.; Shen, J.; Wang, Y.; Yu, L. Immunological Evaluation of a Recombinant Vaccine Delivered with an Analogous Hyaluronic Acid Chitosan Nanoparticle-Hydrogel against Toxoplasma Gondii in Mice. Microb. Pathog. 2023, 179, 106092. [Google Scholar] [CrossRef]
- Nkanga, C.I.; Ortega-Rivera, O.A.; Shin, M.D.; Moreno-Gonzalez, M.A.; Steinmetz, N.F. Injectable Slow-Release Hydrogel Formulation of a Plant Virus-Based COVID-19 Vaccine Candidate. Biomacromolecules 2022, 23, 1812–1825. [Google Scholar] [CrossRef]
- Xia, J.; Liu, Z.-Y.; Han, Z.-Y.; Yuan, Y.; Shao, Y.; Feng, X.-Q.; Weitz, D.A. Regulation of Cell Attachment, Spreading, and Migration by Hydrogel Substrates with Independently Tunable Mesh Size. Acta Biomater. 2022, 141, 178–189. [Google Scholar] [CrossRef]
- Korupalli, C.; Pan, W.-Y.; Yeh, C.-Y.; Chen, P.-M.; Mi, F.-L.; Tsai, H.-W.; Chang, Y.; Wei, H.-J.; Sung, H.-W. Single-Injecting, Bioinspired Nanocomposite Hydrogel That Can Recruit Host Immune Cells in Situ to Elicit Potent and Long-Lasting Humoral Immune Responses. Biomaterials 2019, 216, 119268. [Google Scholar] [CrossRef]
- Iliev, D.B.; Skjæveland, I.; Jørgensen, J.B. CpG Oligonucleotides Bind TLR9 and RRM-Containing Proteins in Atlantic Salmon (Salmo salar). BMC Immunol. 2013, 14, 12. [Google Scholar] [CrossRef]
- Dammermann, W.; Dornbrack, J.; Bröker, K.; Bentzien, F.; Lüth, S. CpG Oligonucleotides Increase HBV-Specific Cytokine Responses in Whole Blood and Enhance Cytokine Release Assay Sensitivity. J. Virol. Methods 2017, 248, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Tang, S.; Wang, Z.; Ma, X.; Zhang, L.; Zhang, F.; Xiao, L.; Zhao, S.; Li, Q.; Wang, Y.; et al. Immune Enhancement by the Tetra-Peptide Hydrogel as a Promising Adjuvant for an H7N9 Vaccine against Highly Pathogenic H7N9 Virus. Vaccines 2022, 10, 130. [Google Scholar] [CrossRef] [PubMed]
- Shi, T.; Lu, H.; Zhu, J.; Zhou, X.; He, C.; Li, F.; Yang, G. Naturally Derived Dual Dynamic Crosslinked Multifunctional Hydrogel for Diabetic Wound Healing. Compos. Part B Eng. 2023, 257, 110687. [Google Scholar] [CrossRef]
- Abaricia, J.O.; Shah, A.H.; Ruzga, M.N.; Olivares-Navarrete, R. Surface Characteristics on Commercial Dental Implants Differentially Activate Macrophages in Vitro and in Vivo. Clin. Oral Implant. Res. 2021, 32, 487–497. [Google Scholar] [CrossRef]
- Yuan, W.; Huang, C.; Deng, W.; Lai, J.; Chen, J.; Jie, J.; Wu, Y.; You, T.; Wu, L.-P. Hyaluronic Acid Methacryloyl/Chitosan Methacryloyl/3-Methacrylamidophenylboronic Acid Multifunctional Hydrogel Loading Exosome for Diabetic Wound Healing. Int. J. Biol. Macromol. 2024, 280, 135562. [Google Scholar] [CrossRef]
- Liu, J.; Zeng, H.; Xiao, P.; Yang, A.; Situ, X.; Wang, Y.; Zhang, X.; Li, W.; Pan, W.; Wang, Y. Sustained Release of Magnesium Ions Mediated by a Dynamic Mechanical Hydrogel to Enhance BMSC Proliferation and Differentiation. ACS Omega 2020, 5, 24477–24486. [Google Scholar] [CrossRef]
- Zhang, K.; Lin, S.; Feng, Q.; Dong, C.; Yang, Y.; Li, G.; Bian, L. Nanocomposite Hydrogels Stabilized by Self-Assembled Multivalent Bisphosphonate-Magnesium Nanoparticles Mediate Sustained Release of Magnesium Ion and Promote in-Situ Bone Regeneration. Acta Biomater. 2017, 64, 389–400. [Google Scholar] [CrossRef] [PubMed]
- Oshiumi, H. Circulating Extracellular Vesicles Carry Immune Regulatory miRNAs and Regulate Vaccine Efficacy and Local Inflammatory Response After Vaccination. Front. Immunol. 2021, 12, 685344. [Google Scholar] [CrossRef]
- Zhong, S.; Xin, Z.; Hou, Y.; Li, Y.; Huang, H.-W.; Sun, T.; Shi, Q.; Wang, H. Double-Modal Locomotion of a Hydrogel Ultra-Soft Magnetic Miniature Robot with Switchable Forms. Cyborg Bionic Syst. 2024, 5, 0077. [Google Scholar] [CrossRef]
- Camci-Unal, G.; Aubin, H.; Ahari, A.F.; Bae, H.; Nichol, J.W.; Khademhosseini, A. Surface-Modified Hyaluronic Acid Hydrogels to Capture Endothelial Progenitor Cells. Soft Matter 2010, 6, 5120. [Google Scholar] [CrossRef]
- Hammer, J.A.; Ruta, A.; Therien, A.M.; West, J.L. Cell-Compatible, Site-Specific Covalent Modification of Hydrogel Scaffolds Enables User-Defined Control over Cell–Material Interactions. Biomacromolecules 2019, 20, 2486–2493. [Google Scholar] [CrossRef] [PubMed]
- Tacken, P.J.; Zeelenberg, I.S.; Cruz, L.J.; Van Hout-Kuijer, M.A.; Van De Glind, G.; Fokkink, R.G.; Lambeck, A.J.A.; Figdor, C.G. Targeted Delivery of TLR Ligands to Human and Mouse Dendritic Cells Strongly Enhances Adjuvanticity. Blood 2011, 118, 6836–6844. [Google Scholar] [CrossRef] [PubMed]
- Marco-Dufort, B.; Janczy, J.R.; Hu, T.; Lütolf, M.; Gatti, F.; Wolf, M.; Woods, A.; Tetter, S.; Sridhar, B.V.; Tibbitt, M.W. Thermal Stabilization of Diverse Biologics Using Reversible Hydrogels. Sci. Adv. 2022, 8, eabo0502. [Google Scholar] [CrossRef]
- Sim, H.J.; Thambi, T.; Lee, D.S. Heparin-Based Temperature-Sensitive Injectable Hydrogels for Protein Delivery. J. Mater. Chem. B 2015, 3, 8892–8901. [Google Scholar] [CrossRef]
- Guktur, R.E.; Nep, E.I.; Asala, O.; Olorunfemi, P.O.; Ngwuluka, N.C.; Ochekpe, N.A.; Sagay, A.S. Carboxymethylated and Acetylated Xerogel Derivatives of Plectranthus Esculentus Starch Protect Newcastle Disease Vaccines against Cold Chain Failure. Vaccine 2021, 39, 4871–4884. [Google Scholar] [CrossRef]
- Guo, Y.; Ryan, U.; Feng, Y.; Xiao, L. Association of Common Zoonotic Pathogens with Concentrated Animal Feeding Operations. Front. Microbiol. 2022, 12, 810142. [Google Scholar] [CrossRef] [PubMed]
- Modaresifar, K.; Hadjizadeh, A.; Niknejad, H. Design and Fabrication of GelMA/Chitosan Nanoparticles Composite Hydrogel for Angiogenic Growth Factor Delivery. Artif. Cells Nanomed. Biotechnol. 2017, 46, 1799–1808. [Google Scholar] [CrossRef]
- Bobbala, S.; Gibson, B.; Gamble, A.B.; McDowell, A.; Hook, S. Poloxamer 407-chitosan Grafted Thermoresponsive Hydrogels Achieve Synchronous and Sustained Release of Antigen and Adjuvant from Single-shot Vaccines. Immunol. Cell Biol. 2018, 96, 656–665. [Google Scholar] [CrossRef]
- Chandna, S.; Povolotsky, T.L.; Nie, C.; Schwartz, S.; Wedepohl, S.; Quaas, E.; Ludwig, K.; Boyakova, Y.; Bhatia, S.; Meyer, K.; et al. Lignin-Based Mucus-Mimicking Antiviral Hydrogels with Enzyme Stability and Tunable Porosity. ACS Appl. Mater. Interfaces 2025, 17, 8962–8975. [Google Scholar] [CrossRef]
- Bej, R.; Stevens, C.A.; Nie, C.; Ludwig, K.; Degen, G.D.; Kerkhoff, Y.; Pigaleva, M.; Adler, J.M.; Bustos, N.A.; Page, T.M.; et al. Mucus-Inspired Self-Healing Hydrogels: A Protective Barrier for Cells against Viral Infection. Adv. Mater. 2024, 36, 2401745. [Google Scholar] [CrossRef]
- Nakahashi-Ouchida, R.; Yuki, Y.; Kiyono, H. Cationic Pullulan Nanogel as a Safe and Effective Nasal Vaccine Delivery System for Respiratory Infectious Diseases. Human. Vaccines Immunother. 2018, 14, 2189–2193. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Tang, H.; Duan, Y.; Zhang, Q.; Shan, W.; Wang, X.; Ren, L. Oral Biomimetic Virus Vaccine Hydrogel for Robust Abscopal Antitumour Efficacy. J. Colloid Interface Sci. 2024, 674, 92–107. [Google Scholar] [CrossRef] [PubMed]
- Fu, W.; Guo, M.; Zhou, X.; Wang, Z.; Sun, J.; An, Y.; Guan, T.; Hu, M.; Li, J.; Chen, Z.; et al. Injectable Hydrogel Mucosal Vaccine Elicits Protective Immunity against Respiratory Viruses. ACS Nano 2024, 18, 11200–11216. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, M.C.; Parker, C.; Klopp, S.; O’Brien, C.; Miska, K.; Fetterer, R. Gel-Bead Delivery of Eimeria Oocysts Protects Chickens Against Coccidiosis. Avian Dis. 2012, 56, 306–309. [Google Scholar] [CrossRef]
- Li, X.; Wu, Z.; He, Y.; Ye, B.-C.; Wang, J. Preparation and Characterization of Monodisperse Microcapsules with Alginate and Bentonite via External Gelation Technique Encapsulating Pseudomonas putida Rs-198. J. Biomater. Sci. Polym. Ed. 2017, 28, 1556–1571. [Google Scholar] [CrossRef]
- Opriessnig, T.; Giménez-Lirola, L.G.; Halbur, P.G. Polymicrobial Respiratory Disease in Pigs. Anim. Health. Res. Rev. 2011, 12, 133–148. [Google Scholar] [CrossRef]
- Tsai, C.J.Y.; Loh, J.M.S.; Fujihashi, K.; Kiyono, H. Mucosal Vaccination: Onward and Upward. Expert Rev. Vaccines 2023, 22, 885–899. [Google Scholar] [CrossRef]
- Wen, Z.; Xu, Z.; Zhou, Q.; Li, W.; Wu, Y.; Du, Y.; Chen, L.; Zhang, Y.; Xue, C.; Cao, Y. Oral Administration of Coated PEDV-Loaded Microspheres Elicited PEDV-Specific Immunity in Weaned Piglets. Vaccine 2018, 36, 6803–6809. [Google Scholar] [CrossRef]
- Zhang, J.; Cui, L.; Zhang, Y.; Pan, H.; Yuan, H.; Zhou, S.; Chen, H.; Song, Y. Oral Administration of PEDV-Dissolved Alg-CS Gel Induces High and Sustained Mucosal Immunity in Mice. J. Gen. Virol. 2024, 105, 001979. [Google Scholar] [CrossRef]
- Yu, X.; Wen, T.; Cao, P.; Shan, L.; Li, L. Alginate-Chitosan Coated Layered Double Hydroxide Nanocomposites for Enhanced Oral Vaccine Delivery. J. Colloid Interface Sci. 2019, 556, 258–265. [Google Scholar] [CrossRef]
- Bedford, J.G.; Caminschi, I.; Wakim, L.M. Intranasal Delivery of a Chitosan-Hydrogel Vaccine Generates Nasal Tissue Resident Memory CD8+ T Cells That Are Protective against Influenza Virus Infection. Vaccines 2020, 8, 572. [Google Scholar] [CrossRef]
- Frydas, I.S.; Nauwynck, H.J. Replication Characteristics of Eight Virulent and Two Attenuated Genotype 1 and 2 Porcine Reproductive and Respiratory Syndrome Virus (PRRSV) Strains in Nasal Mucosa Explants. Vet. Microbiol. 2016, 182, 156–162. [Google Scholar] [CrossRef]
- Zeng, L. Mucosal Adjuvants: Opportunities and Challenges. Hum. Vaccines Immunother. 2016, 12, 2456–2458. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zeng, M.; Shan, H.; Tong, C. Microneedle Patches as Drug and Vaccine Delivery Platform. Curr. Med. Chem. 2017, 24, 2413–2422. [Google Scholar] [CrossRef]
- Pastor, Y.; Ting, I.; Martínez, A.L.; Irache, J.M.; Gamazo, C. Intranasal Delivery System of Bacterial Antigen Using Thermosensitive Hydrogels Based on a Pluronic-Gantrez Conjugate. Int. J. Pharm. 2020, 579, 119154. [Google Scholar] [CrossRef] [PubMed]
- Aida, V.; Pliasas, V.C.; Neasham, P.J.; North, J.F.; McWhorter, K.L.; Glover, S.R.; Kyriakis, C.S. Novel Vaccine Technologies in Veterinary Medicine: A Herald to Human Medicine Vaccines. Front. Vet. Sci. 2021, 8, 654289. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Yang, Y.; Kling, C.; Seigler, L.; Gallardo-Romero, N.F.; Martin, B.E.; Smith, T.G.; Olson, V.A. Inactivated Rabies Virus-Vectored Immunocontraceptive Vaccine in a Thermo-Responsive Hydrogel Induces High and Persistent Antibodies against Rabies, but Insufficient Antibodies against Gonadotropin-Releasing Hormone for Contraception. Vaccines 2019, 7, 73. [Google Scholar] [CrossRef]
- Perez Cuevas, M.B.; Kodani, M.; Choi, Y.; Joyce, J.; O’Connor, S.M.; Kamili, S.; Prausnitz, M.R. Hepatitis B Vaccination Using a Dissolvable Microneedle Patch Is Immunogenic in Mice and Rhesus Macaques. Bioeng. Transl. Med. 2018, 3, 186–196. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, F.; Zeng, Y.; Lin, L.; Yu, H.; Zhang, S.; Yang, W. Hydrogel Systems for Spatiotemporal Controlled Delivery of Immunomodulators: Engineering the Tumor Immune Microenvironment for Enhanced Cancer Immunotherapy. Front. Cell Dev. Biol. 2024, 12, 1514595. [Google Scholar] [CrossRef]
- Umeki, Y.; Saito, M.; Kusamori, K.; Tsujimura, M.; Nishimura, M.; Takahashi, Y.; Takakura, Y.; Nishikawa, M. Combined Encapsulation of a Tumor Antigen and Immune Cells Using a Self-Assembling Immunostimulatory DNA Hydrogel to Enhance Antigen-Specific Tumor Immunity. J. Control. Release 2018, 288, 189–198. [Google Scholar] [CrossRef]
- Guan, T.; Chen, Z.; Wang, X.; Gao, S.; Lu, X.; Li, Y.; Wang, Z.; Zhang, S.; Guo, Y.; Guo, M.; et al. Harnessing Mn2+ Ions and Antitumor Peptides: A Robust Hydrogel for Enhanced Tumor Immunotherapy. J. Am. Chem. Soc. 2025, 147, 6523–6535. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Geng, Y.; Yue, B.; Lo, P.-C.; Huang, J.; Jin, H. Injectable Hydrogel as a Unique Platform for Antitumor Therapy Targeting Immunosuppressive Tumor Microenvironment. Front. Immunol. 2022, 12, 832942. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Tang, W.; Wang, X.; Zhao, X.; Chen, C.; Zhu, Z. Applications of Hydrogels with Special Physical Properties in Biomedicine. Polymers 2019, 11, 1420. [Google Scholar] [CrossRef] [PubMed]
- Meany, E.L.; Klich, J.H.; Jons, C.K.; Mao, T.; Chaudhary, N.; Utz, A.; Baillet, J.; Song, Y.E.; Saouaf, O.M.; Ou, B.S.; et al. Generation of an Inflammatory Niche in a Hydrogel Depot through Recruitment of Key Immune Cells Improves Efficacy of mRNA Vaccines. Sci. Adv. 2025, 11, eadr2631. [Google Scholar] [CrossRef]
- Sexton, A.; Whitney, P.G.; Chong, S.-F.; Zelikin, A.N.; Johnston, A.P.R.; De Rose, R.; Brooks, A.G.; Caruso, F.; Kent, S.J. A Protective Vaccine Delivery System for In Vivo T Cell Stimulation Using Nanoengineered Polymer Hydrogel Capsules. ACS Nano 2009, 3, 3391–3400. [Google Scholar] [CrossRef]
| Hydrogel Category | Representative Materials | Advantages | Limitations | Suitable Vaccine Types | References |
|---|---|---|---|---|---|
| Natural hydrogels | Alginate, chitosan, hyaluronic acid | High biocompatibility, biodegradability, low toxicity | Low mechanical strength, swelling instability | Oral/mucosal vaccines (e.g., PEDV) | [13,18,19] |
| Synthetic hydrogels | PEG, Poloxamer 407/188 | High stability, controlled release, easy functionalization | Low bioactivity, potential degradation byproducts | Long-acting injectables (e.g., rabies) | [14,20] |
| Composite hydrogels | Nanoparticle-hydrogel (e.g., GO/PEI) | Targeted delivery, synergistic immune activation | Complex fabrication, safety validation needed | mRNA vaccines/cancer immunotherapy | [21,22] |
| Stimuli-responsive hydrogels | Thermosensitive chitosan, pH-sensitive phosphorylated chitosan | Spatiotemporal-controlled release, enhanced mucosal retention | Environmental sensitivity affects performance | Intranasal influenza vaccines, gut-targeted oral vaccines | [11,12] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, P.; Yang, Y.; Yu, L.; Li, G.; Zhu, D. Hydrogels in Veterinary Vaccine Development: Types, Mechanisms, and Applications. Gels 2025, 11, 468. https://doi.org/10.3390/gels11060468
Zhao P, Yang Y, Yu L, Li G, Zhu D. Hydrogels in Veterinary Vaccine Development: Types, Mechanisms, and Applications. Gels. 2025; 11(6):468. https://doi.org/10.3390/gels11060468
Chicago/Turabian StyleZhao, Peisen, Yuwei Yang, Lingxue Yu, Guoxin Li, and Dandan Zhu. 2025. "Hydrogels in Veterinary Vaccine Development: Types, Mechanisms, and Applications" Gels 11, no. 6: 468. https://doi.org/10.3390/gels11060468
APA StyleZhao, P., Yang, Y., Yu, L., Li, G., & Zhu, D. (2025). Hydrogels in Veterinary Vaccine Development: Types, Mechanisms, and Applications. Gels, 11(6), 468. https://doi.org/10.3390/gels11060468










