Hydrogels for Cardio and Vascular Tissue Repair and Regeneration
Abstract
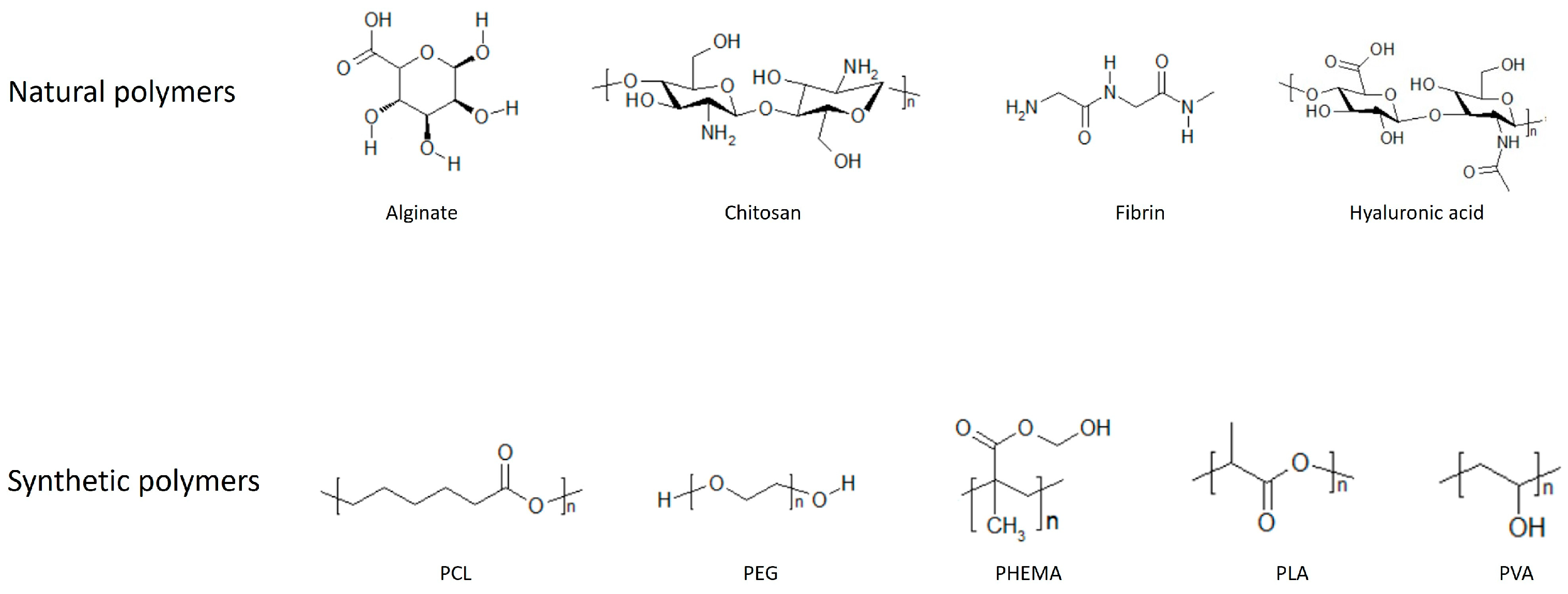
1. Introduction
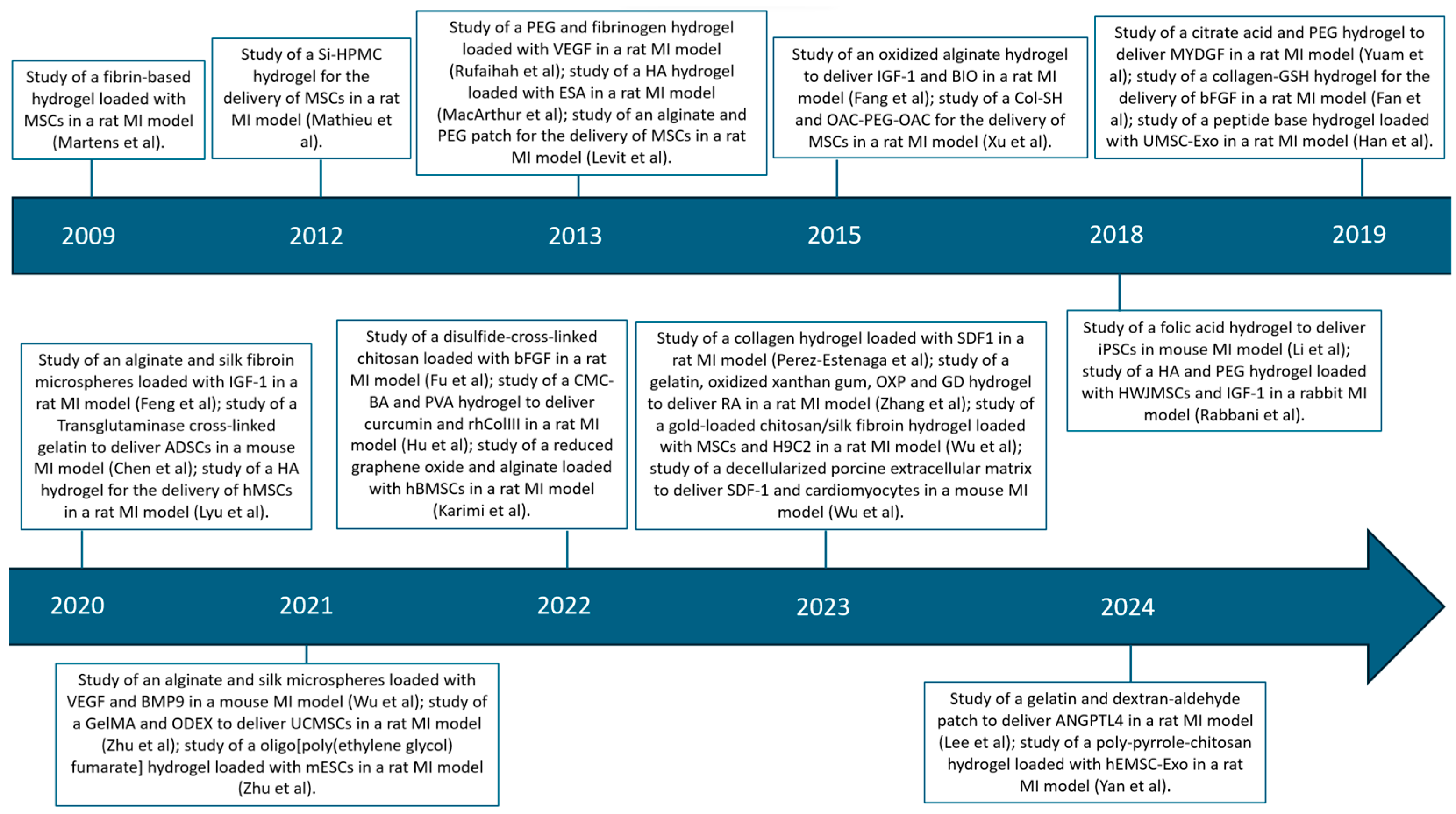
2. Cardiac Repair and Regeneration
2.1. Ventricular Wall Thickening
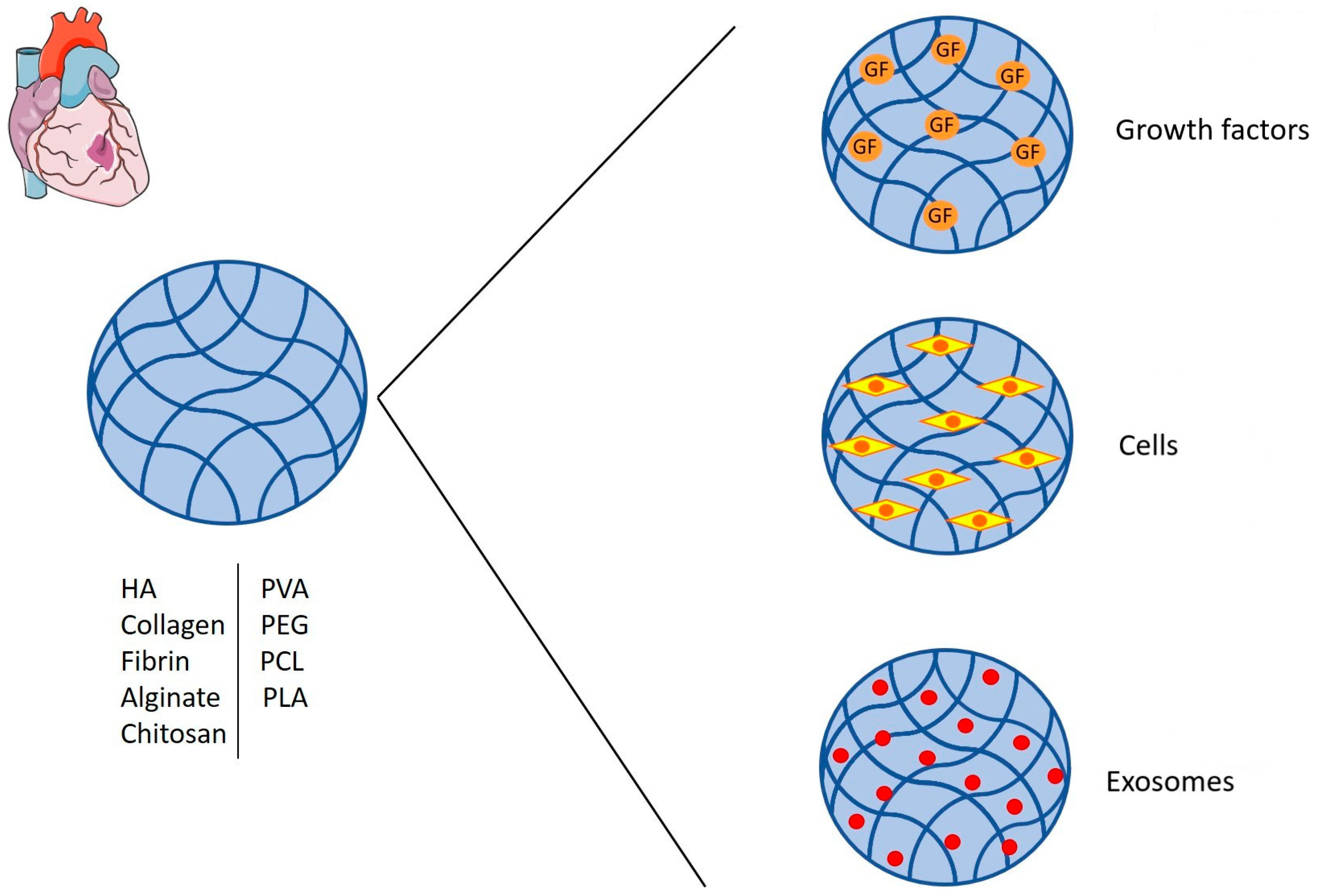
2.2. Growth Factors and Cells Delivery
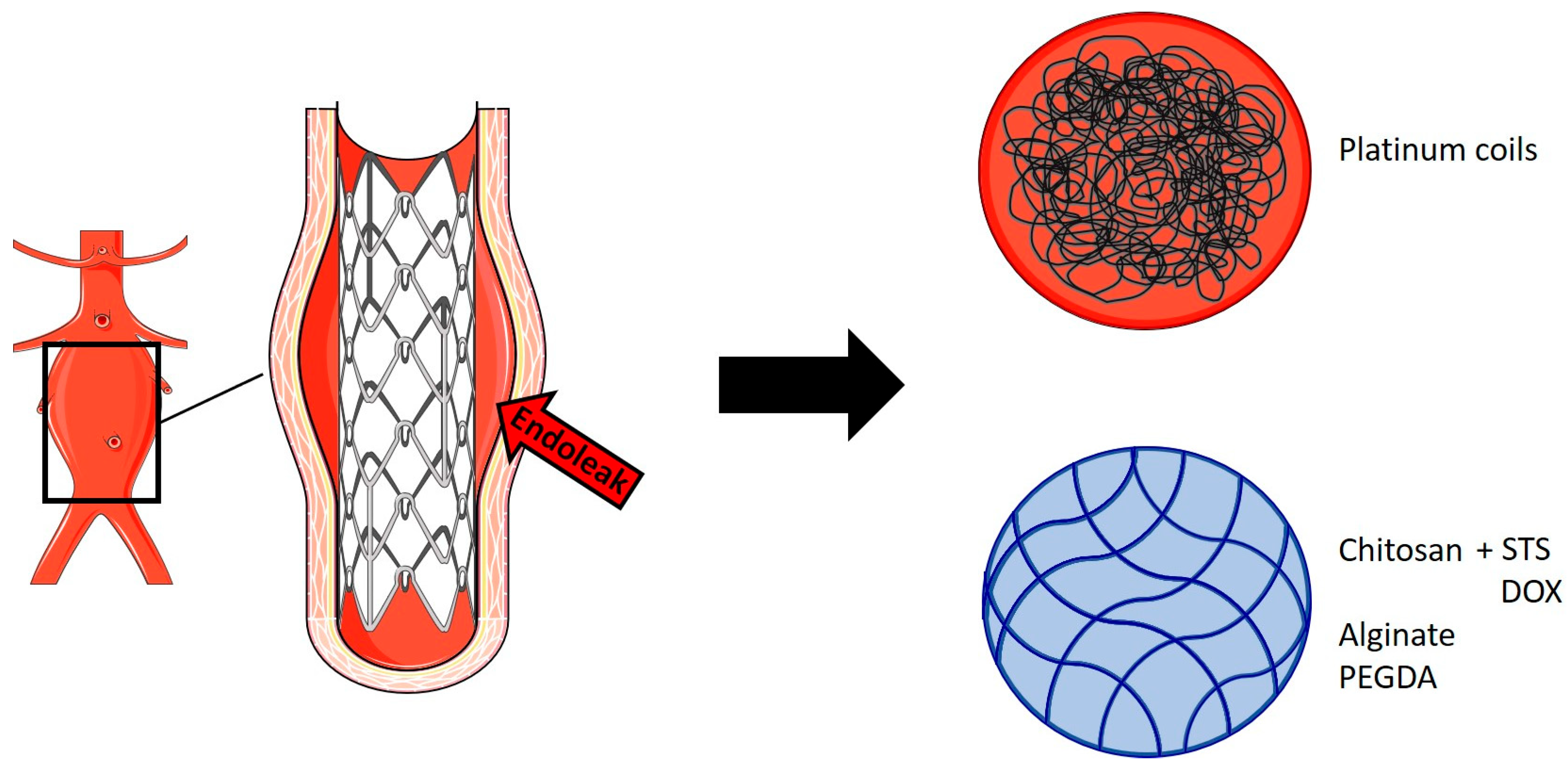
3. Arterial Repair
3.1. Hydrogel-Coated Coils in Intracranial Aneurysms
3.2. Abdominal Aortic Aneurysm (AAA)
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
References
- Peppas, N.A.; Hilt, J.Z.; Khademhosseini, A.; Langer, R. Hydrogels in Biology and Medicine: From Molecular Principles to Bionanotechnology. Adv. Mater. 2006, 18, 1345–1360. [Google Scholar] [CrossRef]
- Hoffman, A.S. Hydrogels for biomedical applications. Adv. Drug Deliv. Rev. 2012, 64, 18–23. [Google Scholar] [CrossRef]
- Caló, E.; Khutoryanskiy, V.V. Biomedical applications of hydrogels: A review of patents and commercial products. Eur. Polym. J. 2015, 65, 252–267. [Google Scholar] [CrossRef]
- Chirani, N.; Yahia, L.H.; Gritsch, L.; Motta, F.; Chirani, S.; Farè, S. History and Applications of Hydrogels. J. Biomed. Sci. 2015, 4, 13–23. [Google Scholar]
- Chai, Q.; Jiao, Y.; Yu, X. Hydrogels for Biomedical Applications: Their Characteristics and the Mechanisms behind Them. Gels 2017, 3, 6. [Google Scholar] [CrossRef]
- Li, Q.; Ning, Z.; Ren, J.; Liao, W. Structural Design and Physicochemical Foundations of Hydrogels for Biomedical Applications. Curr. Med. Chem. 2018, 25, 963–981. [Google Scholar] [CrossRef]
- Aswathy, S.H.; Narendrakumar, U.; Manjubala, I. Commercial hydrogels for biomedical applications. Heliyon 2020, 6, e03719. [Google Scholar] [CrossRef]
- Li, X.; Wu, X. The microspheres/hydrogels scaffolds based on the proteins, nucleic acids, or polysaccharides composite as carriers for tissue repair: A review. Int. J. Biol. Macromol. 2023, 253, 126611. [Google Scholar] [CrossRef] [PubMed]
- Catoira, M.C.; Fusaro, L.; Di Francesco, D.; Ramella, M.; Boccafoschi, F. Overview of natural hydrogels for regenerative medicine applications. J. Mater. Sci. Mater. Med. 2019, 30, 115. [Google Scholar] [CrossRef] [PubMed]
- Burdick, J.A.; Prestwich, G.D. Hyaluronic acid hydrogels for biomedical applications. Adv. Mater. 2011, 23, H41–H56. [Google Scholar] [CrossRef] [PubMed]
- Yuan, N.; Shao, K.; Huang, S.; Chen, C. Chitosan, alginate, hyaluronic acid and other novel multifunctional hydrogel dressings for wound healing: A review. Int. J. Biol. Macromol. 2023, 240, 124321. [Google Scholar] [CrossRef]
- Van Vlierberghe, S.; Dubruel, P.; Schacht, E. Biopolymer-Based Hydrogels as Scaffolds for Tissue Engineering Applications: A Review. Biomacromolecules 2011, 12, 1387–1408. [Google Scholar] [CrossRef] [PubMed]
- Wichterle, O.; Lím, D. Hydrophilic Gels for Biological Use. Nature 1960, 185, 117–118. [Google Scholar] [CrossRef]
- Kim, T.H.; An, D.B.; Oh, S.H.; Kang, M.K.; Song, H.H.; Lee, J.H. Creating stiffness gradient polyvinyl alcohol hydrogel using a simple gradual freezing–thawing method to investigate stem cell differentiation behaviors. Biomaterials 2015, 40, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Kenawy, E.R.; Kamoun, E.A.; Mohy Eldin, M.S.; El-Meligy, M.A. Physically crosslinked poly(vinyl alcohol)-hydroxyethyl starch blend hydrogel membranes: Synthesis and characterization for biomedical applications. Arab. J. Chem. 2014, 7, 372–380. [Google Scholar] [CrossRef]
- Muppalaneni, S.; Omidian, H. Polyvinyl Alcohol in Medicine and Pharmacy: A Perspective. J. Dev. Drugs 2013, 2, 112. [Google Scholar] [CrossRef]
- Peppas, N.A.; Keys, K.B.; Torres-Lugo, M.; Lowman, A.M. Poly(ethylene glycol)-containing hydrogels in drug delivery. J. Control. Release 1999, 62, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.C.; Anseth, K.S. PEG Hydrogels for the Controlled Release of Biomolecules in Regenerative Medicine. Pharm. Res. 2008, 26, 631–643. [Google Scholar] [CrossRef]
- Deng, H.; Dong, A.; Song, J.; Chen, X. Injectable thermosensitive hydrogel systems based on functional PEG/PCL block polymer for local drug delivery. J. Control. Release 2019, 297, 60–70. [Google Scholar] [CrossRef]
- Zhang, K.; Tang, X.; Zhang, J.; Lu, W.; Lin, X.; Zhang, Y.; Tian, B.; Yang, H.; He, H. PEG–PLGA copolymers: Their structure and structure-influenced drug delivery applications. J. Control. Release 2014, 183, 77–86. [Google Scholar] [CrossRef]
- Maeda, T. Structures and Applications of Thermoresponsive Hydrogels and Nanocomposite-Hydrogels Based on Copolymers with Poly (Ethylene Glycol) and Poly (Lactide-Co-Glycolide) Blocks. Bioengineering 2019, 6, 107. [Google Scholar] [CrossRef]
- Zhao, S.P.; Ma, D.; Zhang, L.M. New Semi-Interpenetrating Network Hydrogels: Synthesis, Characterization and Properties. Macromol. Biosci. 2006, 6, 445–451. [Google Scholar] [CrossRef]
- Dhingra, S.; Weisel, R.D.; Li, R.K. Synthesis of aliphatic polyester hydrogel for cardiac tissue engineering. Methods Mol. Biol. 2014, 1181, 51–59. [Google Scholar] [PubMed]
- Lecomte, P.; Detrembleur, C.; Lou, X.; Mazza, M.; Halleux, O.; Jérôme, R. Novel functionalization routes of poly(ε-caprolactone). Macromol. Symp. 2000, 157, 47–60. [Google Scholar] [CrossRef]
- Siddiqui, N.; Asawa, S.; Birru, B.; Baadhe, R.; Rao, S. PCL-Based Composite Scaffold Matrices for Tissue Engineering Applications. Mol. Biotechnol. 2018, 60, 506–532. [Google Scholar] [CrossRef] [PubMed]
- Sinha, V.R.; Bansal, K.; Kaushik, R.; Kumria, R.; Trehan, A. Poly-ϵ-caprolactone microspheres and nanospheres: An overview. Int. J. Pharm. 2004, 278, 1–23. [Google Scholar] [CrossRef]
- Dash, T.K.; Konkimalla, V.B. Poly-є-caprolactone based formulations for drug delivery and tissue engineering: A review. J. Control. Release 2012, 158, 15–33. [Google Scholar] [CrossRef]
- Singhvi, M.S.; Zinjarde, S.S.; Gokhale, D.V. Polylactic acid: Synthesis and biomedical applications. J. App Microbiol. 2019, 127, 1612–1626. [Google Scholar] [CrossRef]
- Lisboa, E.S.; Serafim, C.; Santana, W.; dos Santos, V.L.S.; de Albuquerque-Junior, R.L.C.; Chaud, M.V.; Cardoso, J.C.; Jain, S.; Severino, P.; Souto, E.B. Nanomaterials-combined methacrylated gelatin hydrogels (GelMA) for cardiac tissue constructs. J. Control. Release 2024, 365, 617–639. [Google Scholar] [CrossRef]
- Lu, L.; Liu, M.; Sun, R.; Zheng, Y.; Zhang, P. Myocardial Infarction: Symptoms and Treatments. Cell Biochem. Biophys. 2015, 72, 865–867. [Google Scholar] [CrossRef] [PubMed]
- Masci, P.G.; Bogaert, J. Post myocardial infarction of the left ventricle: The course ahead seen by cardiac MRI. Cardiovasc. Diagn. Ther. 2012, 2, 113–127. [Google Scholar]
- Pazos-López, P.; Peteiro-Vázquez, J.; Carcía-Campos, A.; García-Bueno, L.; Abugattás-de-Torres, J.P.; Castro-Beiras, A. The causes, consequences, and treatment of left or right heart failure. Vasc. Health Risk Manag. 2011, 237, 237–254. [Google Scholar]
- Peña, B.; Laughter, M.; Jett, S.; Rowland, T.J.; Taylor, M.R.G.; Mestroni, L.; Park, D. Injectable Hydrogels for Cardiac Tissue Engineering. Macromol. Biosci. 2018, 18, 1800079. [Google Scholar] [CrossRef]
- Maruyama, K.; Imanaka-Yoshida, K. The Pathogenesis of Cardiac Fibrosis: A Review of Recent Progress. Int. J. Mol. Sci. 2022, 23, 2617. [Google Scholar] [CrossRef]
- Guo, Q.Y.; Yang, J.Q.; Feng, X.X.; Zhou, Y.J. Regeneration of the heart: From molecular mechanisms to clinical therapeutics. Mil. Med. Res. 2023, 10, 18. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, O.; Bhardwaj, R.D.; Bernard, S.; Zdunek, S.; Barnabé-Heider, F.; Walsh, S.; Zupicich, J.; Alkass, K.; Buchholz, B.A.; Druid, H.; et al. Evidence for cardiomyocyte renewal in humans. Science 2009, 324, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Sutton, M.G.S.J.; Sharpe, N. Left Ventricular Remodeling After Myocardial Infarction. Circulation 2000, 101, 2981–2988. [Google Scholar] [CrossRef] [PubMed]
- Cokkinos, D.V.; Belogianneas, C. Left Ventricular Remodelling: A Problem in Search of Solutions. Eur. Cardiol. Rev. 2016, 11, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, A.S.; Ambrosy, A.P.; Velazquez, E.J. Adverse Remodeling and Reverse Remodeling After Myocardial Infarction. Curr. Cardiol. Rep. 2017, 19, 71. [Google Scholar] [CrossRef]
- Zhu, Y.; Matsumura, Y.; Wagner, W.R. Ventricular wall biomaterial injection therapy after myocardial infarction: Advances in material design, mechanistic insight and early clinical experiences. Biomaterials 2017, 129, 37–53. [Google Scholar] [CrossRef] [PubMed]
- Truskey, G.A. Advancing cardiovascular tissue engineering. F1000Research 2016, 5, 1045. [Google Scholar] [CrossRef]
- Chiu, L.L.; Radisic, M. Cardiac tissue engineering. Curr. Opin. Chem. Eng. 2013, 2, 41–52. [Google Scholar] [CrossRef]
- Hoeben, A.; Landuyt, B.; Highley, M.S.; Wildiers, H.; Van Oosterom, A.T.; De Bruijn, E.A. Vascular endothelial growth factor and angiogenesis. Pharmacol. Rev. 2004, 54, 549–580. [Google Scholar] [CrossRef]
- Rufaihah, A.J.; Vaibavi, S.R.; Plotkin, M.; Shen, J.; Nithya, V.; Wang, J.; Seliktar, D.; Kofidis, T. Enhanced infarct stabilization and neovascularization mediated by VEGF-loaded PEGylated fibrinogen hydrogel in a rodent myocardial infarction model. Biomaterials 2013, 34, 8195–8202. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Jiang, X.; Li, X.; Hu, M.; Wan, W.; Wen, Y.; He, Y.; Zheng, X. Intramyocardial delivery of VEGF165 via a novel biodegradable hydrogel induces angiogenesis and improves cardiac function after rat myocardial infarction. Heart Vessel. 2015, 31, 963–975. [Google Scholar] [CrossRef] [PubMed]
- Morine, K.J.; Qiao, X.; York, S.; Natov, P.S.; Paruchuri, V.; Zhang, Y.; Aronovitz, M.J.; Karas, R.H.; Kapur, N.K. Bone Morphogenetic Protein 9 Reduces Cardiac Fibrosis and Improves Cardiac Function in Heart Failure. Circulation 2018, 138, 513–526. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Chang, T.; Chen, W.; Wang, X.; Li, J.; Chen, Y.; Yu, Y.; Shen, Z.; Yu, Q.; Zhang, Y. Release of VEGF and BMP9 from injectable alginate based composite hydrogel for treatment of myocardial infarction. Bioact. Mater. 2021, 6, 520–528. [Google Scholar] [CrossRef] [PubMed]
- MacArthur, J.W.; Trubelja, A.; Shudo, Y.; Hsiao, P.; Fairman, A.S.; Yang, E.; Hiesinger, W.; Sarver, J.J.; Atluri, P.; Woo, Y.J. Mathematically engineered stromal cell–derived factor-1α stem cell cytokine analog enhances mechanical properties of infarcted myocardium. J. Thorac. Cardiovasc. Surg. 2013, 145, 278–284. [Google Scholar] [CrossRef]
- MacArthur, J.W.; Purcell, B.P.; Shudo, Y.; Cohen, J.E.; Fairman, A.; Trubelja, A.; Patel, J.; Hsiao, P.; Yang, E.; Lloyd, K.; et al. Sustained Release of Engineered Stromal Cell-Derived Factor 1-α From Injectable Hydrogels Effectively Recruits Endothelial Progenitor Cells and Preserves Ventricular Function After Myocardial Infarction. Circulation 2013, 128, S79–S86. [Google Scholar] [CrossRef] [PubMed]
- Perez-Estenaga, I.; Chevalier, M.T.; Peña, E.; Abizanda, G.; Alsharabasy, A.M.; Larequi, E.; Cilla, M.; Perez, M.M.; Gurtubay, J.; Garcia-Yebenes Castro, M.; et al. A Multimodal Scaffold for SDF1 Delivery Improves Cardiac Function in a Rat Subacute Myocardial Infarct Model. ACS Appl. Mater. Interfaces 2023, 15, 50638–50651. [Google Scholar] [CrossRef]
- Puche, J.E.; Castilla-Cortázar, I. Human conditions of insulin-like growth factor-I (IGF-I) deficiency. J. Transl. Med. 2012, 10, 224. [Google Scholar] [CrossRef] [PubMed]
- Ungvari, Z.; Csiszar, A. The Emerging Role of IGF-1 Deficiency in Cardiovascular Aging: Recent Advances. J. Gerontol. A 2012, 67A, 599–610. [Google Scholar] [CrossRef]
- Vinciguerra, M.; Santini, M.P.; Claycomb, W.C.; Ladurner, A.G.; Rosenthal, N. Local IGF-1 isoform protects cardiomyocytes from hypertrophic and oxidative stresses via SirT1 activity. Aging 2009, 2, 43–62. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Wu, Y.; Chen, W.; Li, J.; Wang, X.; Chen, Y.; Yu, Y.; Shen, Z.; Zhang, Y. Sustained release of bioactive IGF-1 from a silk fibroin microsphere-based injectable alginate hydrogel for the treatment of myocardial infarction. J. Mater. Chem. B 2020, 8, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Tseng, A.S.; Engel, F.B.; Keating, M.T. The GSK-3 Inhibitor BIO Promotes Proliferation in Mammalian Cardiomyocytes. Chem. Biol. 2006, 13, 957–963. [Google Scholar] [CrossRef] [PubMed]
- Fang, R.; Qiao, S.; Liu, Y.; Chen, X.; Song, B.; Meng, Q.; Hou, X.; Tian, W. Sustained co-delivery of BIO and IGF-1 by a novel hybrid hydrogel system to stimulate endogenous cardiac repair in myocardial infarcted rat hearts. Int. J. Nanomed. 2015, 10, 4691–4703. [Google Scholar] [CrossRef] [PubMed]
- Cully, M. MYDGF promotes heart repair after myocardial infarction. Nat. Rev. Drug Discov. 2015, 14, 164–165. [Google Scholar] [CrossRef]
- Yuan, Z.; Tsou, Y.H.; Zhang, X.Q.; Huang, S.; Yang, Y.; Gao, M.; Ho, W.; Zhao, Q.; Ye, X.; Xu, X. Injectable Citrate-Based Hydrogel as an Angiogenic Biomaterial Improves Cardiac Repair after Myocardial Infarction. ACS Appl. Mater. Interfaces 2019, 11, 38429–38439. [Google Scholar] [CrossRef]
- Klagsbrun, M. The fibroblast growth factor family: Structural and biological properties. Prog. Growth Factor Res. 1989, 1, 207–235. [Google Scholar] [CrossRef]
- Fan, C.; Shi, J.; Zhuang, Y.; Zhang, L.; Huang, L.; Yang, W.; Chen, B.; Chen, Y.; Xiao, Z.; Shen, H.; et al. Myocardial–Infarction–Responsive Smart Hydrogels Targeting Matrix Metalloproteinase for On–Demand Growth Factor Delivery. Adv. Mater. 2019, 31, 1902900. [Google Scholar] [CrossRef]
- Fan, Z.; Xu, Z.; Niu, H.; Sui, Y.; Li, H.; Ma, J.; Guan, J. Spatiotemporal delivery of basic fibroblast growth factor to directly and simultaneously attenuate cardiac fibrosis and promote cardiac tissue vascularization following myocardial infarction. J. Control. Release 2019, 311–312, 233–244. [Google Scholar] [CrossRef]
- Fu, B.; Wang, X.; Chen, Z.; Jiang, N.; Guo, Z.; Zhang, Y.; Zhang, S.; Liua, X.; Liu, L. Improved myocardial performance in infarcted rat heart by injection of disulfide-cross-linked chitosan hydrogels loaded with basic fibroblast growth factor. J. Mater. Chem. B 2022, 10, 656–665. [Google Scholar] [CrossRef]
- Zhang, L.; Bei, Z.; Li, T.; Qian, Z. An injectable conductive hydrogel with dual responsive release of rosmarinic acid improves cardiac function and promotes repair after myocardial infarction. Bioact. Mater. 2023, 29, 132–150. [Google Scholar] [CrossRef]
- Lee, M.; Kim, Y.S.; Park, J.; Choe, G.; Lee, S.; Kang, B.G.; Jun, J.H.; Shin, Y.; Kim, M.; Ahn, Y.; et al. A paintable and adhesive hydrogel cardiac patch with sustained release of ANGPTL4 for infarcted heart repair. Bioact. Mater. 2024, 31, 395–407. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.; Liu, W.; Long, L.; Wang, Z.; Zhang, W.; He, S.; Lu, L.; Fan, H.; Yang, L.; Wang, Y. Regeneration of infarcted hearts by myocardial infarction-responsive injectable hydrogels with combined anti-apoptosis, anti-inflammatory and pro-angiogenesis properties. Biomaterials 2022, 290, 121849. [Google Scholar] [CrossRef] [PubMed]
- Kolios, G.; Moodley, Y. Introduction to Stem Cells and Regenerative Medicine. Respiration 2013, 85, 3–10. [Google Scholar] [CrossRef]
- Martens, T.P.; Godier, A.F.G.; Parks, J.J.; Wan, L.Q.; Koeckert, M.S.; Eng, G.M.; Hudson, B.I.; Sherman, W.; Vunjak-Novakovic, G. Percutaneous Cell Delivery into the Heart Using Hydrogels Polymerizing in Situ. Cell Transpl. 2009, 18, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Levit, R.D.; Landázuri, N.; Phelps, E.A.; Brown, M.E.; García, A.J.; Davis, M.E.; Joseph, G.; Long, R.; Safley, S.A.; Suever, J.D.; et al. Cellular Encapsulation Enhances Cardiac Repair. J. Am. Heart Assoc. 2013, 2, e000367. [Google Scholar] [CrossRef]
- Mathieu, E.; Lamirault, G.; Toquet, C.; Lhommet, P.; Rederstorff, E.; Sourice, S.; Biteau, K.; Hulin, P.; Forest, V.; Weiss, P.; et al. Intramyocardial Delivery of Mesenchymal Stem Cell-Seeded Hydrogel Preserves Cardiac Function and Attenuates Ventricular Remodeling after Myocardial Infarction. PLoS ONE 2012, 7, e51991. [Google Scholar] [CrossRef]
- Xu, G.; Wang, X.; Deng, C.; Teng, X.; Suuronen, E.J.; Shen, Z.; Zhong, Z. Injectable biodegradable hybrid hydrogels based on thiolated collagen and oligo(acryloyl carbonate)–poly(ethylene glycol)–oligo(acryloyl carbonate) copolymer for functional cardiac regeneration. Acta Biomater. 2015, 15, 55–64. [Google Scholar] [CrossRef]
- Wu, Z.; Li, W.; Cheng, S.; Liu, J.; Wang, S. Novel fabrication of bioengineered injectable chitosan hydrogel loaded with conductive nanoparticles to improve therapeutic potential of mesenchymal stem cells in functional recovery after ischemic myocardial infarction. Nanomedicine 2023, 47, 102616. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Manhas, A.; Gupta, S.; Dikshit, M.; Jagavelu, K.; Verma, R.S. Fabrication, characterization and in vivo assessment of cardiogel loaded chitosan patch for myocardial regeneration. Int. J. Biol. Macromol. 2022, 222, 3045–3056. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Li, C.; Li, C.; Chen, J.; Li, Y.; Xie, H.; Lin, C.; Fan, M.; Guo, Y.; Gao, E.; et al. Tailorable Hydrogel Improves Retention and Cardioprotection of Intramyocardial Transplanted Mesenchymal Stem Cells for the Treatment of Acute Myocardial Infarction in Mice. J. Am. Heart Assoc. 2020, 9, e013784. [Google Scholar] [CrossRef] [PubMed]
- Lyu, Y.; Xie, J.; Liu, Y.; Xiao, M.; Li, Y.; Yang, J.; Yang, J.; Liu, W. Injectable Hyaluronic Acid Hydrogel Loaded with Functionalized Human Mesenchymal Stem Cell Aggregates for Repairing Infarcted Myocardium. ACS Biomater. Sci. Eng. 2020, 6, 6926–6937. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Yu, C.; Liu, N.; Zhao, M.; Chen, Z.; Liu, J.; Li, G.; Huang, H.; Guo, H.; Sun, T.; et al. Injectable conductive gelatin methacrylate / oxidized dextran hydrogel encapsulating umbilical cord mesenchymal stem cells for myocardial infarction treatment. Bioact. Mater. 2021, 13, 119–134. [Google Scholar] [CrossRef]
- Karimi Hajishoreh, N.; Baheiraei, N.; Naderi, N.; Salehnia, M.; Razavi, M. Left Ventricular Geometry and Angiogenesis Improvement in Rat Chronic Ischemic Cardiomyopathy following Injection of Encapsulated Mesenchymal Stem Cells. Cell J. 2022, 24, 741–747. [Google Scholar] [PubMed]
- Hong, X.; Luo, A.C.; Doulamis, I.; Oh, N.; Im, G.B.; Lin, C.Y.; del Nido, P.J.; Lin, R.Z.; Melero-Martin, J.M. Photopolymerizable Hydrogel for Enhanced Intramyocardial Vascular Progenitor Cell Delivery and Post-Myocardial Infarction Healing. Adv. Healthc. Mater. 2023, 12, 2301581. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liu, Z.; Li, D.; Guo, X.; Kasper, F.K.; Duan, C.; Zhou, J.; Mikos, A.G.; Wang, C. Injectable biodegradable hydrogels for embryonic stem cell transplantation: Improved cardiac remodeling and function of myocardial infarction. J. Cell Mol. Med. 2012, 16, 1310–1320. [Google Scholar] [CrossRef]
- Tan, Y.; Wang, L.; Chen, G.; Liu, W.; Li, Z.; Wang, Y.; Wang, L.; Li, W.; Wu, J.; Hao, J. Hyaluronate supports hESC-cardiomyocyte cell therapy for cardiac regeneration after acute myocardial infarction. Cell Prolif. 2020, 53, e12942. [Google Scholar] [CrossRef]
- Wang, X.; Chun, Y.W.; Zhong, L.; Chiusa, M.; Balikov, D.A.; Frist, A.Y.; Lim, C.C.; Maltais, S.; Bellan, L.; Hong, C.C.; et al. A temperature-sensitive, self-adhesive hydrogel to deliver iPSC-derived cardiomyocytes for heart repair. Int. J. Cardiol. 2015, 190, 177–180. [Google Scholar] [CrossRef]
- Li, H.; Gao, J.; Shang, Y.; Hua, Y.; Ye, M.; Yang, Z.; Ou, C.; Chen, M. Folic Acid Derived Hydrogel Enhances the Survival and Promotes Therapeutic Efficacy of iPS Cells for Acute Myocardial Infarction. ACS Appl. Mater. Interfaces 2018, 10, 24459–24468. [Google Scholar] [CrossRef]
- Pezhouman, A.; Nguyen, N.B.; Kay, M.; Kanjilal, B.; Noshadi, I.; Ardehali, R. Cardiac regeneration—Past advancements, current challenges, and future directions. J. Mol. Cell Cardiol. 2023, 182, 75–85. [Google Scholar] [CrossRef]
- Barile, L.; Moccetti, T.; Marbán, E.; Vassalli, G. Roles of exosomes in cardioprotection. Eur. Heart J. 2016, 38, 1372–1379. [Google Scholar] [CrossRef]
- Han, C.; Zhou, J.; Liang, C.; Liu, B.; Pan, X.; Zhang, Y.; Wang, Y.; Yan, B.; Xie, W.; Liu, F.; et al. Human umbilical cord mesenchymal stem cell derived exosomes encapsulated in functional peptide hydrogels promote cardiac repair. Biomater. Sci. 2019, 7, 2920–2933. [Google Scholar] [CrossRef]
- Yan, C.; Wang, X.; Wang, Q.; Li, H.; Song, H.; Zhou, J.; Peng, Z.; Yin, W.; Fan, X.; Yang, K.; et al. A Novel Conductive Polypyrrole-Chitosan Hydrogel Containing Human Endometrial Mesenchymal Stem Cell-Derived Exosomes Facilitated Sustained Release for Cardiac Repair. Adv. Healthc. Mater. 2024, 2304207. [Google Scholar] [CrossRef]
- Rabbani, S.; Soleimani, M.; Sahebjam, M.; Imani, M.; Haeri, A.; Ghiaseddin, A.; Nassiri, S.M.; Majd Ardakani, J.; Tajik Rostami, M.; Jalali, A.; et al. Simultaneous Delivery of Wharton’s Jelly Mesenchymal Stem Cells and Insulin-Like Growth Factor-1 in Acute Myocardial Infarction. Iran. J. Pharm. Res. 2018, 17, 426–441. [Google Scholar] [PubMed]
- Liang, W.; Chen, J.; Li, L.; Li, M.; Wei, X.; Tan, B.; Shang, Y.; Fan, G.; Wang, W.; Liu, W. Conductive Hydrogen Sulfide-Releasing Hydrogel Encapsulating ADSCs for Myocardial Infarction Treatment. ACS Appl. Mater. Interfaces 2019, 11, 14619–14629. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.; Wang, Y.; Yang, H.; Chen, Y.; Lu, K.; Wu, Y.; Liu, C.; Zhang, H.; Meng, H.; Yu, Q.; et al. Injectable Decellularized Extracellular Matrix Hydrogel Containing Stromal Cell-Derived Factor 1 Promotes Transplanted Cardiomyocyte Engraftment and Functional Regeneration after Myocardial Infarction. ACS Appl. Mater. Interfaces 2023, 15, 2578–2589. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Lin, H.; Summers, R.; Yang, M.; Cousins, B.G.; Tsui, J. Current Treatment Strategies for Intracranial Aneurysms: An Overview. Angiology 2017, 69, 17–30. [Google Scholar] [CrossRef]
- Xue, T.; Chen, Z.; Lin, W.; Xu, J.; Shen, X.; Wang, Z. Hydrogel coils versus bare platinum coils for the endovascular treatment of intracranial aneurysms: A meta-analysis of randomized controlled trials. BMC Neurol. 2018, 18, 167. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, A.T.; Haskal, Z.J.; Hertzer, N.R.; Bakal, C.W.; Creager, M.A.; Halperin, J.L.; Hiratzka, L.F.; Murphy, W.R.C.; Olin, J.W.; Puschett, J.B.; et al. ACC/AHA 2005 Practice Guidelines for the Management of Patients With Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic). Circulation 2006, 113, e463–e654. [Google Scholar] [CrossRef]
- Ouriel, K.; Green, R.M.; Donayre, C.; Shortell, C.K.; Elliott, J.; DeWeese, J.A. An evaluation of new methods of expressing aortic aneurysm size: Relationship to rupture. J. Vasc. Surg. 1992, 15, 12–18, discussion 19–20. [Google Scholar] [CrossRef]
- Bengtsson, H.; Bergqvist, D. Ruptured abdominal aortic aneurysm: A population-based study. J. Vasc. Surg. 1993, 18, 74–80. [Google Scholar] [CrossRef]
- England, A.; McWilliams, R. Endovascular Aortic Aneurysm Repair (EVAR). Ulst. Med. J. 2013, 82, 3–10. [Google Scholar]
- Corriere, M.A.; Feurer, I.D.; Becker, S.Y.; Dattilo, J.B.; Passman, M.A.; Guzman, R.J.; Naslund, T.C. Endoleak Following Endovascular Abdominal Aortic Aneurysm Repair. Ann. Surg. 2004, 239, 800–807. [Google Scholar] [CrossRef]
- Fatimi, A.; Chabrot, P.; Berrahmoune, S.; Coutu, J.M.; Soulez, G.; Lerouge, S. A new injectable radiopaque chitosan-based sclerosing embolizing hydrogel for endovascular therapies. Acta Biomater. 2012, 8, 2712–2721. [Google Scholar] [CrossRef] [PubMed]
- Barnett, B.P.; Hughes, A.H.; Lin, S.; Arepally, A.; Gailloud, P.H. In Vitro Assessment of EmboGel and UltraGel Radiopaque Hydrogels for the Endovascular Treatment of Aneurysms. J. Vasc. Interv. Radiol. 2009, 20, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Zehtabi, F.; Ispas-Szabo, P.; Djerir, D.; Sivakumaran, L.; Annabi, B.; Soulez, G.; Mateescu, M.A.; Lerouge, S. Chitosan-doxycycline hydrogel: An MMP inhibitor/sclerosing embolizing agent as a new approach to endoleak prevention and treatment after endovascular aneurysm repair. Acta Biomater. 2017, 64, 94–105. [Google Scholar] [CrossRef] [PubMed]
| Author/Year | Hydrogel Composition | Loading Composition | Reference |
|---|---|---|---|
| Rufaihah et al., 2013 | PEG and fibrinogen | VEGF | [44] |
| Zhu et al., 2015 | Biodegradable dextran chains grafted with hydrophobic PCL-HEMA chains and PCL-grafted polysaccharide chains into the PNIPAAm network | VEGF165 | [45] |
| Wu et al., 2021 | Alginate and silk microspheres | VEGF and BMP9 | [47] |
| MacArthur et al., 2013 | Hyaluronic acid | ESA | [49] |
| Perez-Estenaga et al., 2023 | Collagen | SDF1 | [50] |
| Feng et al., 2020 | Alginate and silk fibroin microspheres | IGF-1 | [54] |
| Fang et al., 2015 | Oxidized alginate and gelatin nanoparticles | IGF-1 and BIO | [56] |
| Yuan et al., 2019 | Citrate acid and PEG | MYDGF | [58] |
| Fan et al., 2019 | Collagen-GSH | bFGF | [60] |
| Fan et al., 2020 | NIPAAm, HEMA, and AOLA | bFGF | [61] |
| Fu et al., 2022 | Disulfide cross-linked chitosan | bFGF | [62] |
| Zhang et al., 2023 | Gelatin, oxidized xanthan gum, OXP, and GD | RA | [63] |
| Lee et al., 2024 | Gelatin and dextran-aldehyde | ANGPTL4 | [64] |
| Hu et al., 2022 | Phenylboronic acid-grafted carboxymethyl cellulose (CMC-BA) and PVA | Curcumin and rhColIII | [65] |
| Martens et al., 2009 | Fibrin | MSCs | [67] |
| Levit et al., 2013 | Alginate and PEG | MSCs | [68] |
| Mathieu et al., 2012 | Silanized hydroxypropyl methylcellulose | MSCs | [69] |
| Xu et al., 2015 | Thiolated collagen and OAC-PEG-OAC | MSCs | [70] |
| Wu et al., 2023 | Gold-loaded chitosan/silk fibroin hydrogel | MSCs and cardiomyoblasts | [71] |
| Sharma et al., 2022 | Cardiogel and chitosan | MSCs | [72] |
| Chen et al., 2020 | Transglutaminase cross-linked gelatin | ADSCs | [73] |
| Lyu et al., 2020 | Hyaluronic acid | hMSCs | [74] |
| Zhu et al., 2021 | GelMA and ODEX | UCMSCs | [75] |
| Karimi Hajishoreh et al., 2022 | Reduced graphene oxide and alginate | hBMSCs | [76] |
| Hong et al., 2023 | GelMA | Human endothelial colon-forming cells and MSCs | [77] |
| Wang et al., 2021 | Oligo[poly(ethylene glycol) fumarate] | mESCs | [78] |
| Tan et al., 2020 | Matrigel, alginate, and hyaluronate | hESC-CMs | [79] |
| Wang et al., 2015 | PEG-PCL conjugated with a collagen-binding peptide (SYIRIADTNIT) | iPSC-CMs | [80] |
| Li et al., 2018 | Folic acid | iPSCs | [81] |
| Han et al., 2019 | Peptide based | UMSC-Exo | [84] |
| Yan et al., 2024 | Poly-pyrrole-chitosan | hEMSC-Exo | [85] |
| Rabbani et al., 2018 | Hyaluronic acid and PEG | HWJMSCs and IGF1 | [86] |
| Liang et al., 2019 | Partially oxidized alginate cross-linked with tetraaniline nanoparticles | APTC and ADSCs | [87] |
| Wu et al., 2023 | Decellularized porcine extracellular matrix | SDF-1 and cardiomyocytes | [88] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Motta, I.; Soccio, M.; Guidotti, G.; Lotti, N.; Pasquinelli, G. Hydrogels for Cardio and Vascular Tissue Repair and Regeneration. Gels 2024, 10, 196. https://doi.org/10.3390/gels10030196
Motta I, Soccio M, Guidotti G, Lotti N, Pasquinelli G. Hydrogels for Cardio and Vascular Tissue Repair and Regeneration. Gels. 2024; 10(3):196. https://doi.org/10.3390/gels10030196
Chicago/Turabian StyleMotta, Ilenia, Michelina Soccio, Giulia Guidotti, Nadia Lotti, and Gianandrea Pasquinelli. 2024. "Hydrogels for Cardio and Vascular Tissue Repair and Regeneration" Gels 10, no. 3: 196. https://doi.org/10.3390/gels10030196
APA StyleMotta, I., Soccio, M., Guidotti, G., Lotti, N., & Pasquinelli, G. (2024). Hydrogels for Cardio and Vascular Tissue Repair and Regeneration. Gels, 10(3), 196. https://doi.org/10.3390/gels10030196










