A Dedicated Mycosis Flask Increases the Likelihood of Identifying Candidemia Sepsis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Extraction
2.3. Blood Culture Processing
2.4. Definitions
2.5. Statistical Methods
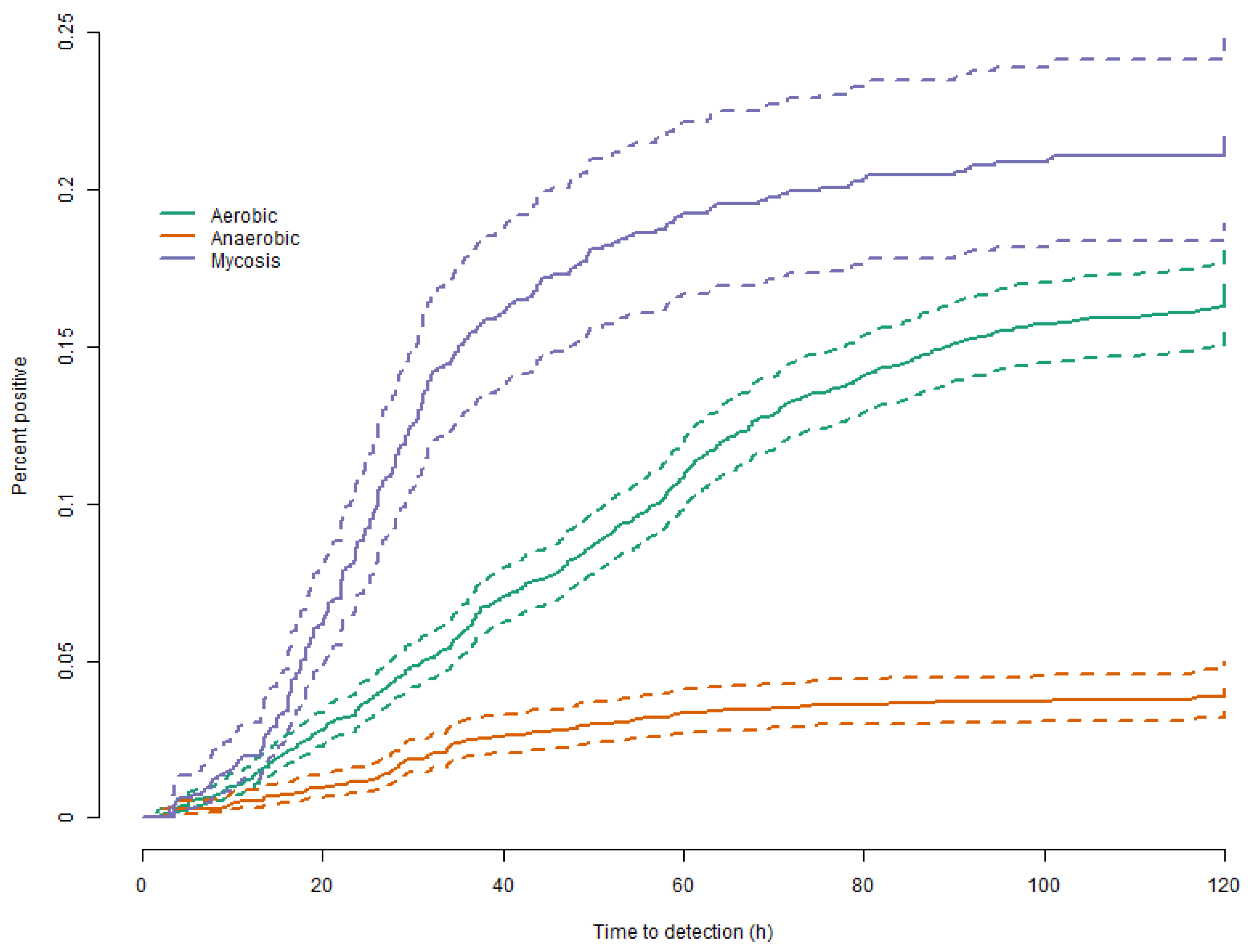
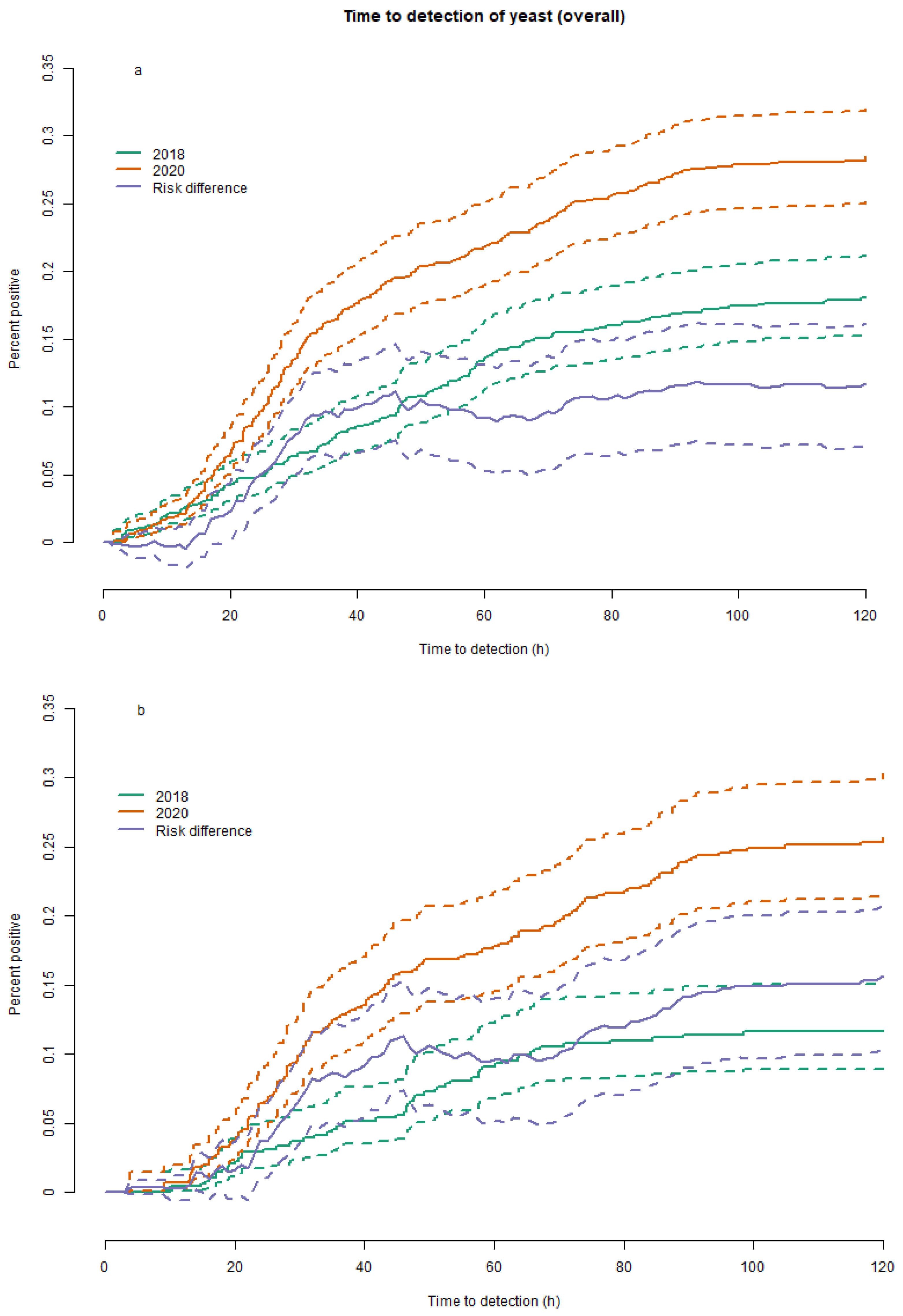
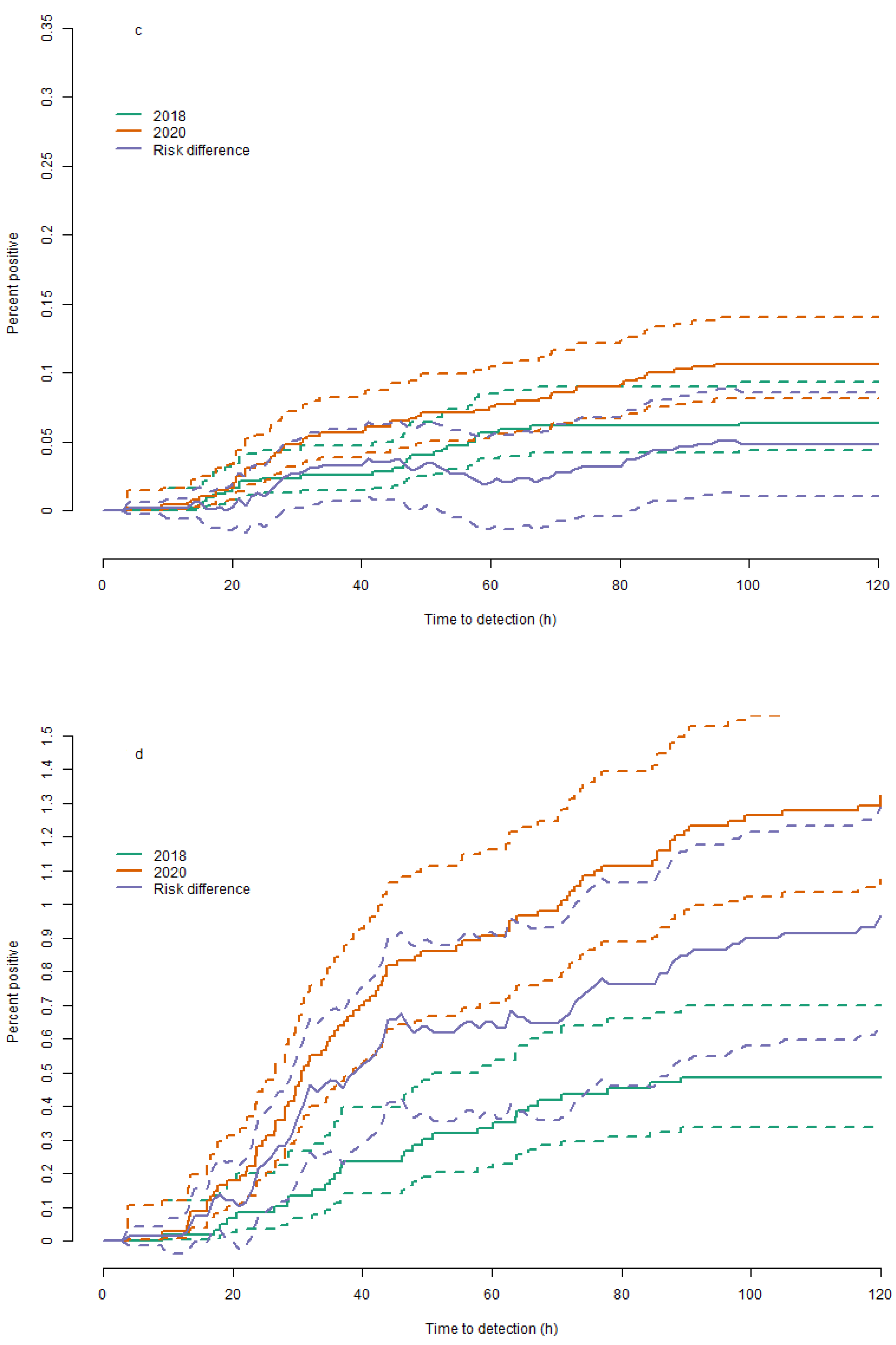
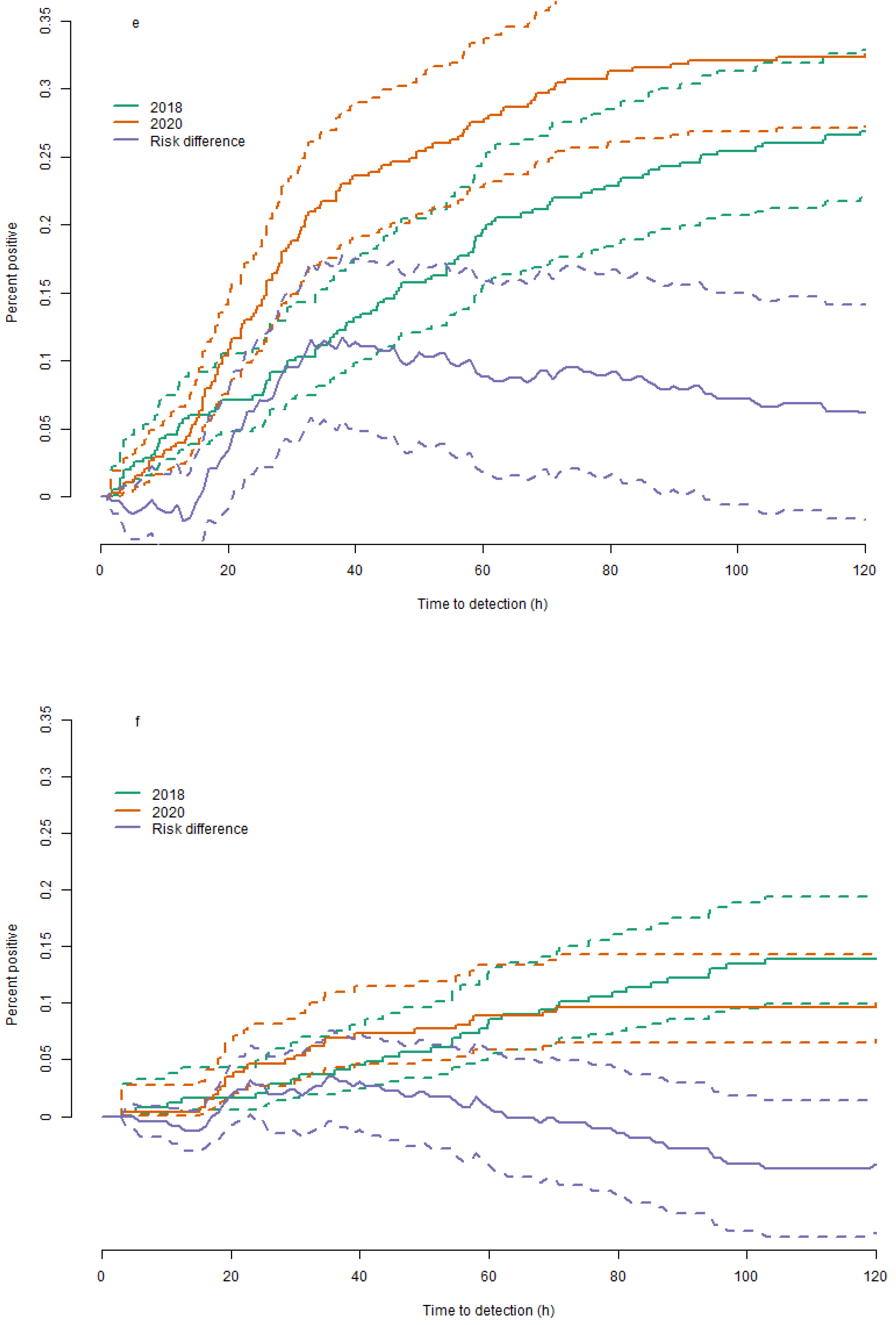
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pappas, P.G.; Lionakis, M.S.; Arendrup, M.C.; Ostrosky-Zeichner, L.; Kullberg, B.J. Invasive candidiasis. Nat. Rev. Dis. Prim. 2018, 4, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Barantsevich, N.; Barantsevich, E. Diagnosis and Treatment of Invasive Candidiasis. Antibiotics 2022, 11, 718. [Google Scholar] [CrossRef] [PubMed]
- Andes, D.R.; Safdar, N.; Baddley, J.W.; Playford, G.; Reboli, A.C.; Rex, J.H.; Sobel, J.D.; Pappas, P.G.; Kullberg, B.J. Impact of treatment strategy on outcomes in patients with candidemia and other forms of invasive candidiasis: A patient-level quantitative review of randomized trials. Clin. Infect. Dis. 2012, 54, 1110–1122. [Google Scholar] [CrossRef] [PubMed]
- Arendrup, M.C.; Sulim, S.; Holm, A.; Nielsen, L.; Nielsen, S.D.; Knudsen, J.D.; Drenck, N.E.; Christensen, J.J.; Johansen, H.K. Diagnostic issues, clinical characteristics, and outcomes for patients with fungemia. J. Clin. Microbiol. 2011, 49, 3300–3308. [Google Scholar] [CrossRef] [PubMed]
- Gokbolat, E.; Oz, Y.; Metintas, S. Evaluation of three different bottles in BACTEC 9240 automated blood culture system and direct identification of Candida species to shorten the turnaround time of blood culture. J. Med. Microbiol. 2017, 66, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Köck, R.; Eibing, L.C.; Boschin, M.G.; Ellger, B.; Horn, D.; Idelevich, E.A.; Becker, K. Evaluation of Bactec mycosis IC/F and plus aerobic/f blood culture bottles for detection of Candida in the presence of antifungal agents. J. Clin. Microbiol. 2013, 51, 3683–3687. [Google Scholar] [CrossRef] [PubMed]
- Zheng, S.; Ng, T.Y.; Li, H.; Tan, A.L.; Tan, T.T.; Tan, B.H. A dedicated fungal culture medium is useful in the diagnosis of fungemia: A retrospective cross-sectional study. PLoS ONE 2016, 11, e0164668. [Google Scholar] [CrossRef] [PubMed]
- Datcu, R.; Boel, J.; Jensen, I.M.; Arpi, M. Comparison of BACTECTM blood culture media for the detection of fungemia. Eur. J. Clin. Microbiol. Infect. Dis. 2017, 36, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M.H.; Letscher-Bru, V.; Jaulhac, B.; Waller, J.; Candolfi, E. Comparison of Mycosis IC/F and Plus Aerobic/F Media for Diagnosis of Fungemia by the Bactec 9240 System. J. Clin. Microbiol. 2004, 42, 773–777. [Google Scholar] [CrossRef] [PubMed]
- Menchinelli, G.; Liotti, F.M.; Fiori, B.; De Angelis, G.; D’Inzeo, T.; Giordano, L.; Posteraro, B.; Sabbatucci, M.; Sanguinetti, M.; Spanu, T. In vitro evaluation of BACT/ALERT®VIRTUO®, BACT/ALERT 3D®, and BACTECTM FX automated blood culture systems for detection of microbial pathogens using simulated human blood samples. Front. Microbiol. 2019, 10, 221. [Google Scholar] [CrossRef] [PubMed]
- Mueller-Premru, M.; Jeverica, S.; Papst, L.; Nagy, E. Performance of two blood culture systems to detect anaerobic bacteria. Is there any difference? Anaerobe 2017, 45, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Butler-Laporte, G.; Yansouni, C.P.; Paquette, K.; Lawandi, A.; Stabler, S.N.; Akhter, M.; Davidson, A.C.; Gavric, M.; Jinah, R.; Saeed, Z.; et al. Real-world time to positivity of 2 widely used commercial blood culture systems in patients with severe manifestations of sepsis: An analysis of the FABLED study. Open Forum Infect. Dis. 2020, 7, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Nawrot, U.; Kowalska-Krochmal, B.; Sulik-Tyszka, B.; Kozak, M.; Świętek, K.; Pajączkowska, M.; Piątkowska, E.; Rosiak, D.; Swoboda-Kopeć, E. Evaluation of blood culture media for the detection of fungi. Eur. J. Clin. Microbiol. Infect. Dis. 2015, 34, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Almuhayawi, M.; Altun, O.; Abdulmajeed, A.D.; Ullberg, M.; Özenci, V. The performance of the four anaerobic blood culture bottles BacT/ALERT-FN,-FN Plus, bactec-plus and-lytic in detection of anaerobic bacteria and identification by direct MALDI-TOF MS. PLoS ONE 2015, 10, e0142398. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.M.; Binnicker, M.J.; Campbell, S.; Carroll, K.C.; Chapin, K.C.; Gilligan, P.H.; Gonzalez, M.D.; Jerris, R.C.; Kehl, S.C.; Patel, R.; et al. A Guide to Utilization of the Microbiology Laboratory for Diagnosis of Infectious Diseases: 2018 Update by the Infectious Diseases Society of America and the American Society for Microbiology. Clin. Infect. Dis. 2018, 67, e1–e94. [Google Scholar] [CrossRef] [PubMed]
- Nemer, S.; Imtiaz, T.; Varikkara, M.; Collier, A.; Bal, A.M. Management of candidaemia with reference to the European confederation of medical mycology quality indicators. Infect. Dis. 2019, 51, 527–533. [Google Scholar] [CrossRef] [PubMed]
| 2018 | 2018 | 2018 | 2020 | 2020 | 2020 | |
|---|---|---|---|---|---|---|
| BACTEC™ | BacTAlert™ | Total | BACTEC™ | BACTEC™ in the Hospital’s Formerly Using BacTAlert™ *, # | Total | |
| Blood culture flasks * | 155,450; 233 (0.15%) | 192,272; 120 (0.06%) | 347,722; 353 (0.1%) | 162,245; 274 (0.17%) | 227,165; 301 (0.13%) | 389,410; 575 (0.15%) |
| Unique patients | 22,346 | 30,808 | 52,215 | 22,383 | 33,371 | 54,862 |
| Flask type * | ||||||
| Mycosis flask | 2409; 7 (0.29%) | 0; 0 (-) | 2409; 7 (0.29%) | 38,659; 101 (0.26%) | 56,765; 104 (0.18%) | 95,424; 205 (0.21%) |
| Aerobic flask | 76,511; 196 (0.26%) | 96,027; 91 (0.09%) | 172,538; 287 (0.17%) | 80,450; 151 (0.19%) | 113,457; 170 (0.15%) | 193,907; 321 (0.17%) |
| Anaerobic flask | 76,530; 30 (0.04%) | 96,245; 29 (0.03%) | 172,775; 59 (0.03%) | 43,136; 22 (0.05%) | 56,943; 27 (0.05%) | 100,079; 49 (0.05%) |
| Department of Clinical Microbiology * | ||||||
| Hvidovre | 0; 0 (-) | 125,515; 115 (0.09%) | 125,515; 115 (0.09%) | 0; 0 (-) | 151,053; 212 (0.14%) | 151,053; 212 (0.14%) |
| Herlev | 108,671; 76 (0.07%) | 66,757; 5 (0.01%) | 175,428; 81 (0.05%) | 113,688; 71 (0.06%) | 76,112; 89 (0.12%) | 189,800; 160 (0.08%) |
| Rigshospitalet | 46,779; 157 (0.34%) | 0; 0 (-) | 46,779; 157 (0.34%) | 48,557; 203 (0.42%) | 0; 0 (-) | 48,557; 203 (0.42%) |
| Department * | ||||||
| Low risk | 102,452; 61 (0.06%) | 167,998; 58 (0.03%) | 270,450; 119 (0.04%) | 107,084; 43 (0.04%) | 194,647; 109 (0.06%) | 301,731; 152 (0.05%) |
| High risk | 52,998; 172 (0.32%) | 24,274; 62 (0.26%) | 77,272; 234 (0.3%) | 55,161; 231 (0.42%) | 32,518; 192 (0.59%) | 87,679; 423 (0.48%) |
| Hematology | 11,704; 6 (0.05%) | 16; 0 (0%) | 11,720; 6 (0.05%) | 10,312; 21 (0.2%) | 16; 0 (0%) | 10,328; 21 (0.2%) |
| Oncology | 9288; 11 (0.12%) | 1105; 0 (0%) | 10,393; 11 (0.11%) | 9501; 5 (0.05%) | 875; 0 (0%) | 10,376; 5 (0.05%) |
| Gastric surgery | 4319; 17 (0.39%) | 10,086; 14 (0.14%) | 14,405; 31 (0.22%) | 5206; 49 (0.94%) | 11,841; 45 (0.38%) | 17,047; 94 (0.55%) |
| Gastroenterology | 6626; 34 (0.51%) | 3148; 8 (0.25%) | 9774; 42 (0.43%) | 5976; 32 (0.54%) | 3492; 35 (1%) | 9468; 67 (0.71%) |
| Urology | 4180; 16 (0.38%) | 0; 0 (-) | 4180; 16 (0.38%) | 3775; 25 (0.66%) | 4; 0 (0%) | 3779; 25 (0.66%) |
| Nephrology | 8573; 9 (0.1%) | 2055; 0 (0%) | 10,628; 9 (0.08%) | 7575; 15 (0.2%) | 1908; 5 (0.26%) | 9483; 20 (0.21%) |
| Intensive care unit * | 8308; 79 (0.95%) | 7864; 40 (0.51%) | 16,172; 119 (0.74%) | 12,816; 84 (0.66%) | 14,382; 107 (0.74%) | 27,198; 191 (0.7%) |
| Microscopy negative * | 707; 9 (1.27%) | 1243; 11 (0.88%) | 1950; 20 (1.03%) | 545; 7 (1.28%) | 1234; 32 (2.59%) | 1779; 39 (2.19%) |
| Candidemia–which species | ||||||
| Candida albicans | 82 (35%) | 46 (38%) | 128 (36%) | 126 (46%) | 112 (37%) | 238 (41%) |
| Candida glabrata | 82 (35%) | 63 (52%) | 145 (41%) | 90 (33%) | 138 (46%) | 228 (40%) |
| Candida krusei | 8 (3.4%) | 0 (0%) | 8 (2.3%) | 4 (1.5%) | 0 (0%) | 4 (0.7%) |
| Candida parapsilosis | 14 (6%) | 4 (3.3%) | 18 (5.1%) | 28 (10%) | 14 (4.7%) | 42 (7.3%) |
| Candida tropicalis | 11 (4.7%) | 6 (5%) | 17 (4.8%) | 17 (6.2%) | 13 (4.3%) | 30 (5.2%) |
| Candida dubliniensis | 18 (7.7%) | 1 (0.83%) | 19 (5.4%) | 5 (1.8%) | 10 (3.3%) | 15 (2.6%) |
| Candida kefyr | 13 (5.6%) | 0 (0%) | 13 (3.7%) | 1 (0.36%) | 7 (2.3%) | 8 (1.4%) |
| Candida guilliermondii | 0 (0%) | 0 (0%) | 0 (0%) | 8 (2.9%) | 6 (2%) | 14 (2.4%) |
| Cryptococcus neoformans | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (0.66%) | 2 (0.35%) |
| Other fungi | 11 (4.7%) | 0 (0%) | 11 (3.1%) | 0 (0%) | 1 (0.33%) | 1 (0.17%) |
| Bacteraemia | 6291 (4%) | 7468 (3.9%) | 13,759 (4%) | 5508 (3.4%) | 10,551 (4.6%) | 16,059 (4.1%) |
| Combined bacteraemia and fungaemia | 5 (0.003%) | 15 (0.008%) | 20 (0.006%) | 1 (0.001%) | 11 (0.005%) | 12 (0.003%) |
| 2018 | 2020 | |||||
|---|---|---|---|---|---|---|
| BACTEC™ | BacTAlert™ | Total | BACTEC™ | BACTEC™ in the Hospital’s Formerly Using BacTAlert™ * | Total | |
| Blood culture sets | 34,977; 81 (0.23%) | 48,182; 44 (0.09%) | 83,159; 125 (0.15%) | 37,724; 105 (0.28%) | 54,533; 108 (0.2%) | 92,257; 213 (0.23%) |
| Unique patients | 20,996 | 30,155 | 50,251 | 21,825 | 33,304 | 54,244 |
| Department of clinical microbiology | ||||||
| Hvidovre | 0; 0 (-) | 31,883; 43 (0.13%) | 31,883; 43 (0.13%) | 0; 0 (-) | 36,147; 71 (0.2%) | 36,147; 71 (0.2%) |
| Herlev | 26,142; 37 (0.14%) | 16,299; 1 (0.01%) | 42,441; 38 (0.09%) | 27,590; 31 (0.11%) | 18,386; 37 (0.2%) | 45,976; 68 (0.15%) |
| Rigshospitalet | 8835; 44 (0.5%) | 0; 0 (-) | 8835; 44 (0.5%) | 10,134; 74 (0.73%) | 0; 0 (-) | 10,134; 74 (0.73%) |
| Number of flasks in blood culture set | ||||||
| 3 | 790; 2 (0.25%) | 1470; 1 (0.07%) | 2260; 3 (0.13%) | 1361; 18 (1.32%) | 611; 0 (0%) | 1972; 18 (0.91%) |
| 4 | 30,742; 62 (0.2%) | 44,730; 35 (0.08%) | 75,472; 97 (0.13%) | 33,617; 60 (0.18%) | 51,070; 70 (0.14%) | 84,687; 130 (0.15%) |
| 5 | 1624; 4 (0.25%) | 34; 1 (2.94%) | 1658; 5 (0.3%) | 377; 3 (0.8%) | 401; 3 (0.75%) | 778; 6 (0.77%) |
| 6 | 429; 6 (1.4%) | 411; 0 (0%) | 840; 6 (0.71%) | 317; 2 (0.63%) | 148; 2 (1.35%) | 465; 4 (0.86%) |
| 7 | 87; 0 (0%) | 41; 0 (0%) | 128; 0 (0%) | 167; 1 (0.6%) | 128; 4 (3.12%) | 295; 5 (1.69%) |
| 8 | 1052; 6 (0.57%) | 1360; 7 (0.51%) | 2412; 13 (0.54%) | 1676; 20 (1.19%) | 1873; 27 (1.44%) | 3549; 47 (1.32%) |
| >8 | 1305; 7 (0.54%) | 1496; 7 (0.47%) | 2801; 14 (0.5%) | 1885; 21 (1.11%) | 2175; 29 (1.33%) | 4060; 50 (1.23%) |
| Departments | ||||||
| Low risk | 24,547; 30 (0.12%) | 42,212; 20 (0.05%) | 66,759; 50 (0.07%) | 25,964; 22 (0.08%) | 47,804; 38 (0.08%) | 73,768; 60 (0.08%) |
| High risk | 10,430; 51 (0.49%) | 5970; 24 (0.4%) | 16,400; 75 (0.46%) | 11,760; 83 (0.71%) | 6729; 70 (1.04%) | 18,489; 153 (0.83%) |
| Hematology | 1697; 2 (0.12%) | 4; 0 (0%) | 1701; 2 (0.12%) | 1783; 10 (0.56%) | 4; 0 (0%) | 1787; 10 (0.56%) |
| Oncology | 2200; 5 (0.23%) | 270; 0 (0%) | 2470; 5 (0.2%) | 2235; 1 (0.04%) | 209; 0 (0%) | 2444; 1 (0.04%) |
| Gastric surgery | 925; 8 (0.86%) | 2692; 3 (0.11%) | 3617; 11 (0.3%) | 1166; 13 (1.11%) | 2878; 16 (0.56%) | 4044; 29 (0.72%) |
| Gastroenterology | 1420; 14 (0.99%) | 820; 4 (0.49%) | 2240; 18 (0.8%) | 1305; 7 (0.54%) | 821; 9 (1.1%) | 2126; 16 (0.75%) |
| Urology | 1000; 7 (0.7%) | 0; 0 (-) | 1000; 7 (0.7%) | 920; 11 (1.2%) | 1; 0 (0%) | 921; 11 (1.19%) |
| Nephrology | 1967; 4 (0.4%) | 506; 0 (-) | 2473; 4 (0.4%) | 1717; 7 (0.76%) | 464; 3 (300%) | 2181; 10 (1.09%) |
| Intensive care unit | 1221; 11 (0.9%) | 1678; 17 (1.01%) | 2899; 28 (0.97%) | 2634; 34 (1.29%) | 2352; 42 (1.79%) | 4986; 76 (1.52%) |
| Bacteremia | 3396 (9.7%) | 3101 (6.4%) | 6497 (7.8%) | 3797 (10%) | 5517 (10%) | 9314 (10%) |
| Combined bacteraemia and fungaemia | 13 (0.04%) | 12 (0.03%) | 25 (0.03%) | 18 (0.05%) | 32 (0.06%) | 50 (0.05%) |
| Overall Comparison | ||||||
|---|---|---|---|---|---|---|
| 2018 | 2020 | |||||
| Fungal blood infections | Blood culture sets | Fungal blood infections | Blood culture sets | Absolute difference (95% CI), pr. 1.000 blood culture sets | Numbers needed to treat (95% CI) | |
| Overall estimates | 150 | 83,159 | 263 | 92,257 | 1.2 (0.72; 1.6) | 853 (617; 1382) |
| Stratified analyses | ||||||
| High-risk departments | 89 | 164 | 186 | 18,489 | 5.2 (3.4; 7.1) | 191 (142; 293) |
| Gastric surgery | 13 | 3617 | 39 | 4044 | 6.8 (3.2; 10) | 147 (97; 311) |
| Gastroenterology | 21 | 224 | 18 | 2126 | −0.93 (−6.5; 4.6) | - |
| Hematology | 2 | 1701 | 10 | 1787 | 4.8 (0.98; 8.6) | 209 (116; 1024) |
| Intensive care unit | 36 | 2899 | 94 | 4986 | 7.4 (1.9; 13) | 136 (78; 532) |
| Nephrology | 4 | 2473 | 10 | 2181 | 3.2 (−0.03; 6.4) | 311 (155; Inf) |
| Oncology | 5 | 247 | 2 | 2444 | −1.2 (−3.3; 0.87) | - |
| Urology | 8 | 1 | 13 | 921 | 7.4 (−2; 17) | 136 (60; Inf) |
| Low-risk departments | 61 | 66,759 | 77 | 73,768 | 0.16 (−0.17; 0.48) | 6367 (2067; Inf) |
| BACTEC™ | ||||||
| 2018 | 2020 | |||||
| Fungal blood infections | Blood culture sets | Fungal blood infections | Blood culture sets | Absolute difference (95% CI), pr. 1.000 blood culture sets | Numbers needed to treat (95% CI) | |
| Overall estimates | 94 | 34,977 | 123 | 37,724 | 0.62 (−0.17; 1.4) | 1609 (709; Inf) |
| Stratified analyses | ||||||
| High-risk departments | 60 | 1043 | 97 | 1176 | 2.7 (0.56; 4.9) | 364 (203; 1780) |
| Gastric surgery | 9 | 925 | 16 | 1166 | 4.2 (−5; 13) | 238 (75; Inf) |
| Gastroenterology | 16 | 142 | 9 | 1305 | −4.9 (−12; 2.2) | - |
| Hematology | 2 | 1697 | 10 | 1783 | 4.8 (0.98; 8.6) | 208 (116; 1020) |
| Intensive care unit | 16 | 1221 | 40 | 2634 | 2 (−5.9; 9.8) | 503 (102; Inf) |
| Nephrology | 4 | 1967 | 7 | 1717 | 2.1 (−1.5; 5.7) | 468 (174; Inf) |
| Oncology | 5 | 22 | 2 | 2235 | −1.4 (−3.8; 0.92) | - |
| Urology | 8 | 1 | 13 | 920 | −9.3 (−15; −3.8) | - |
| Low-risk departments | 34 | 24,547 | 26 | 25,964 | −0.42 (−1; 0.19) | - |
| Hospitals that used BacTAlert™ in 2018. This changed to BACTEC™ in 2020 | ||||||
| 2018 | 2020 | |||||
| Fungal blood infections | Blood culture sets | Fungal blood infections | Blood culture sets | Absolute difference (95% CI), pr. 1.000 blood culture sets | Numbers needed to treat (95% CI) | |
| Overall estimates | 56 | 48,182 | 140 | 54,533 | 1.6 (1; 2.1) | 637 (478; 953) |
| Stratified analyses | ||||||
| High-risk departments | 29 | 597 | 89 | 6729 | 9.7 (6.4; 13) | 103 (78; 155) |
| Gastric surgery | 4 | 2692 | 23 | 2878 | 7.3 (3.8; 11) | 137 (92; 266) |
| Gastroenterology | 5 | 820 | 9 | 821 | 5.5 (−3.4; 14) | 183 (70; Inf) |
| Hematology | 0 | 4 | 0 | 4 | 0 (-) | - |
| Intensive care unit | 20 | 1678 | 54 | 2352 | 13 (5.5; 21) | 75 (47; 182) |
| Nephrology | 0 | 506 | 3 | 464 | 7.1 (−0.12; 14) | 140 (70; Inf) |
| Oncology | 0 | 270 | 0 | 209 | 0 (-) | - |
| Urology | NA | NA | 0 | 1 | - | - |
| Low-risk departments | 27 | 42,212 | 51 | 47,804 | 0.48 (0.1; 0.86) | 2075 (1161; 9717) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahlström, M.G.; Antsupova, V.S.; Pedersen, M.; Johansen, H.K.; Hansen, D.S.; Knudsen, I.J.D. A Dedicated Mycosis Flask Increases the Likelihood of Identifying Candidemia Sepsis. J. Fungi 2023, 9, 441. https://doi.org/10.3390/jof9040441
Ahlström MG, Antsupova VS, Pedersen M, Johansen HK, Hansen DS, Knudsen IJD. A Dedicated Mycosis Flask Increases the Likelihood of Identifying Candidemia Sepsis. Journal of Fungi. 2023; 9(4):441. https://doi.org/10.3390/jof9040441
Chicago/Turabian StyleAhlström, Magnus G., Valeria S. Antsupova, Michael Pedersen, Helle Krogh Johansen, Dennis Schrøder Hansen, and Inge Jenny Dahl Knudsen. 2023. "A Dedicated Mycosis Flask Increases the Likelihood of Identifying Candidemia Sepsis" Journal of Fungi 9, no. 4: 441. https://doi.org/10.3390/jof9040441
APA StyleAhlström, M. G., Antsupova, V. S., Pedersen, M., Johansen, H. K., Hansen, D. S., & Knudsen, I. J. D. (2023). A Dedicated Mycosis Flask Increases the Likelihood of Identifying Candidemia Sepsis. Journal of Fungi, 9(4), 441. https://doi.org/10.3390/jof9040441





