Loop-Mediated Isothermal Amplification (LAMP): Potential Point-of-Care Testing for Vulvovaginal Candidiasis
Abstract
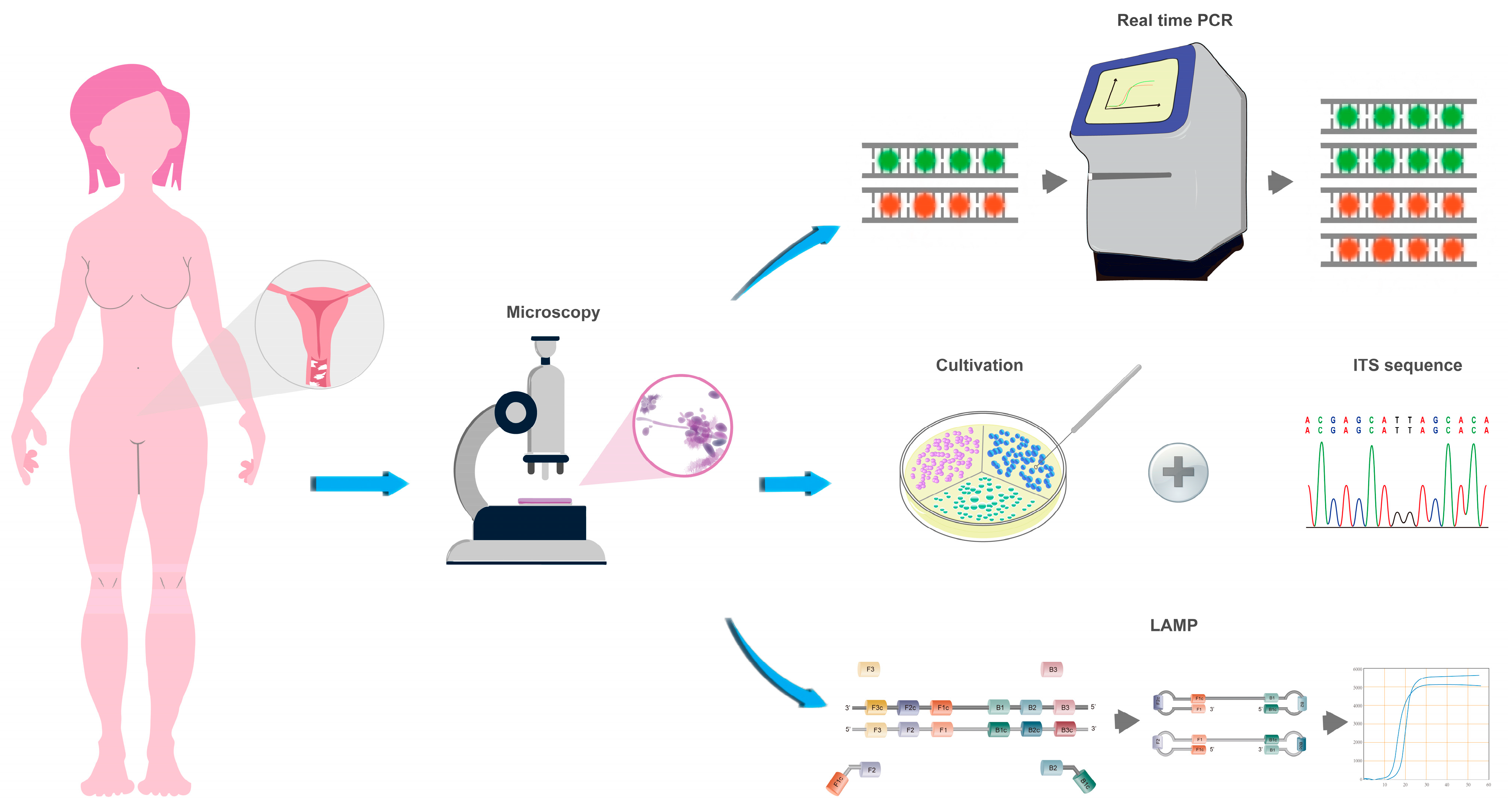
:1. Introduction
2. Materials and Methods
2.1. Study Design and Enrolment
2.2. Sample Collection and Processing
2.3. Cultivation and Internal Transcribed Spacer (ITS) Sequencing
2.4. Microscopy
2.5. Real-Time PCR
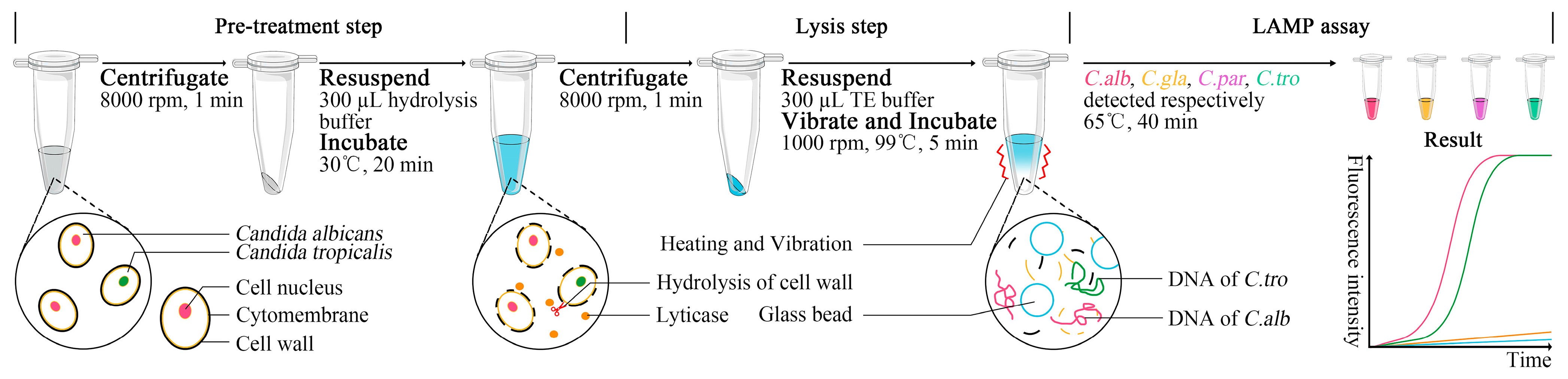
2.6. LAMP Assay
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Achkar, J.M.; Fries, B.C. Candida Infections of the Genitourinary Tract. Clin. Microbiol. Rev. 2010, 23, 253–273. [Google Scholar] [CrossRef]
- Gonçalves, B.; Ferreira, C.; Alves, C.T.; Henriques, M.; Azeredo, J.; Silva, S. Vulvovaginal Candidiasis: Epidemiology, Microbiology and Risk Factors. Crit. Rev. Microbiol. 2016, 42, 905–927. [Google Scholar] [CrossRef]
- Workowski, K.A.; Bachmann, L.H.; Chan, P.A.; Johnston, C.M.; Muzny, C.A.; Park, I.; Reno, H.; Zenilman, J.M.; Bolan, G.A. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm. Rep. 2021, 70, 1–187. [Google Scholar] [CrossRef] [PubMed]
- Blostein, F.; Levin-Sparenberg, E.; Wagner, J.; Foxman, B. Recurrent Vulvovaginal Candidiasis. Ann. Epidemiol. 2017, 27, 575–582.e3. [Google Scholar] [CrossRef]
- Khaksar Baniasadi, A.; Ayatollahi Mosavi, S.A.; Sharifi, I.; Bamorovat, M.; Salari, S.; Ahmadi, A.; Amanizadeh, A.; Agha Kuchak Afshari, S. Vulvovaginal Candidiasis in Iranian Women: Molecular Identification and Antifungal Susceptibility Pattern. J. Obstet. Gynaecol. 2022, 48, 3292–3303. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Zhu, Y.; Fan, S.; Liu, X.; Liang, Y.; Shan, Y. Molecular Identification and Antifungal Susceptibility Profile of Yeast from Vulvovaginal Candidiasis. BMC Infect. Dis. 2020, 20, 287. [Google Scholar] [CrossRef]
- Favrot, C. Polymerase Chain Reaction: Advantages and Drawbacks. In Proceedings of the 3. Congresso Latinoamericano de Dermatologia Veterinaria, Buenos Aires, Argentina, 26–27 November 2015. [Google Scholar] [CrossRef]
- Álvarez, C.; Prestløkken, E.; Nielsen, N.I.; Volden, H.; Klemetsdal, G.; Weisbjerg, M.R. Precision and Additivity of Organic Matter Digestibility Obtained via in Vitro Multi-Enzymatic Method. J. Dairy Sci. 2020, 103, 4880–4891. [Google Scholar] [CrossRef] [PubMed]
- Spinillo, A.; Capuzzo, E.; Gulminetti, R.; Marone, P.; Colonna, L.; Piazzi, G. Prevalence of and Risk Factors for Fungal Vaginitis Caused by Non-Albicans Species. Am. J. Obstet. Gynecol. 1997, 176, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Marchaim, D.; Lemanek, L.; Bheemreddy, S.; Kaye, K.S.; Sobel, J.D. Fluconazole-Resistant Candida Albicans Vulvovaginitis. Obstet. Gynecol. 2012, 120, 1407–1414. [Google Scholar] [CrossRef]
- Notomi, T.; Okayama, H.; Masubuchi, H.; Yonekawa, T.; Watanabe, K.; Amino, N.; Hase, T. Loop-Mediated Isothermal Amplification of DNA. Nucleic Acids Res. 2000, 28, E63. [Google Scholar] [CrossRef]
- Parida, M.; Sannarangaiah, S.; Dash, P.K.; Rao, P.V.L.; Morita, K. Loop Mediated Isothermal Amplification (LAMP): A New Generation of Innovative Gene Amplification Technique; Perspectives in Clinical Diagnosis of Infectious Diseases. Rev. Med. Virol. 2008, 18, 407–421. [Google Scholar] [CrossRef]
- Bentaleb, E.M.; Abid, M.; El Messaoudi, M.D.; Lakssir, B.; Ressami, E.M.; Amzazi, S.; Sefrioui, H.; Ait Benhassou, H. Development and Evaluation of an In-House Single Step Loop-Mediated Isothermal Amplification (SS-LAMP) Assay for the Detection of Mycobacterium Tuberculosis Complex in Sputum Samples from Moroccan Patients. BMC Infect. Dis. 2016, 16, 517. [Google Scholar] [CrossRef] [PubMed]
- Yari, F.; Abiri, R.; Aryan, E.; Ahmadi Jouybari, T.; Navabi, J.; Alvandi, A. Loop-Mediated Isothermal Amplification as a Fast Noninvasive Method of Helicobacter Pylori Diagnosis. J. Clin. Lab. Anal. 2016, 30, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Kim, E.J.; Kilgore, P.E.; Takahashi, H.; Ohnishi, M.; Tomono, J.; Miyamoto, S.; Omagari, D.; Kim, D.W.; Seki, M. A Novel Loop-Mediated Isothermal Amplification Assay for Serogroup Identification of Neisseria Meningitidis in Cerebrospinal Fluid. Front. Microbiol. 2015, 6, 1548. [Google Scholar] [CrossRef] [PubMed]
- Kitajima, H.; Tamura, Y.; Yoshida, H.; Kinoshita, H.; Katsuta, H.; Matsui, C.; Matsushita, A.; Arai, T.; Hashimoto, S.; Iuchi, A.; et al. Clinical COVID-19 Diagnostic Methods: Comparison of Reverse Transcription Loop-Mediated Isothermal Amplification (RT-LAMP) and Quantitative RT-PCR (qRT-PCR). J. Clin. Virol. 2021, 139, 104813. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.; Li, M.; Mao, Z.; Deng, A.; Lv, W.; Huang, L.; Zhong, H.; Yang, H.; Zhang, L.; Liao, Q.; et al. An Integrated and Multi-Target Nucleic Acid Isothermal Analysis System for Rapid Diagnosis of Vulvovaginal Candidiasis. Biosensors 2023, 13, 559. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, K.; Mage, P.L.; Csordas, A.T.; Eisenstein, M.; Soh, H.T. Simultaneous Elimination of Carryover Contamination and Detection of DNA with Uracil-DNA-Glycosylase-Supplemented Loop-Mediated Isothermal Amplification (UDG-LAMP). Chem. Commun. 2014, 50, 3747–3749. [Google Scholar] [CrossRef]
- Kennedy, M.A.; Sobel, J.D. Vulvovaginal Candidiasis Caused by Non-Albicans Candida Species: New Insights. Curr. Infect. Dis. Rep. 2010, 12, 465–470. [Google Scholar] [CrossRef]
- Sasani, E.; Rafat, Z.; Ashrafi, K.; Salimi, Y.; Zandi, M.; Soltani, S.; Hashemi, F.; Hashemi, S.J. Vulvovaginal Candidiasis in Iran: A Systematic Review and Meta-Analysis on the Epidemiology, Clinical Manifestations, Demographic Characteristics, Risk Factors, Etiologic Agents and Laboratory Diagnosis. Microb. Pathog. 2021, 154, 104802. [Google Scholar] [CrossRef]
- Denning, D.W.; Kneale, M.; Sobel, J.D.; Rautemaa-Richardson, R. Global Burden of Recurrent Vulvovaginal Candidiasis: A Systematic Review. Lancet Infect. Dis. 2018, 18, e339–e347. [Google Scholar] [CrossRef]
- Donders, G.; Sziller, I.O.; Paavonen, J.; Hay, P.; de Seta, F.; Bohbot, J.M.; Kotarski, J.; Vives, J.A.; Szabo, B.; Cepuliené, R.; et al. Management of Recurrent Vulvovaginal Candidosis: Narrative Review of the Literature and European Expert Panel Opinion. Front. Cell. Infect. Microbiol. 2022, 12, 934353. [Google Scholar] [CrossRef] [PubMed]
- Sobel, J.D.; Faro, S.; Force, R.W.; Foxman, B.; Ledger, W.J.; Nyirjesy, P.R.; Reed, B.D.; Summers, P.R. Vulvovaginal Candidiasis: Epidemiologic, Diagnostic, and Therapeutic Considerations. Am. J. Obstet. Gynecol. 1998, 178, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.; Zhang, Y.; Zhang, T.; Xue, Y.; Xu, H.; An, R. Risk Factors of Vulvovaginal Candidiasis among Women of Reproductive Age in Xi’an: A Cross-Sectional Study. Biomed. Res. Int. 2018, 2018, 9703754. [Google Scholar] [CrossRef] [PubMed]
- Jaeger, M.; Carvalho, A.; Cunha, C.; Plantinga, T.S.; van de Veerdonk, F.; Puccetti, M.; Galosi, C.; Joosten, L.A.B.; Dupont, B.; Kullberg, B.J.; et al. Association of a Variable Number Tandem Repeat in the NLRP3 Gene in Women with Susceptibility to RVVC. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 797–801. [Google Scholar] [CrossRef]
- ElFeky, D.S.; Gohar, N.M.; El-Seidi, E.A.; Ezzat, M.M.; AboElew, S.H. Species Identification and Antifungal Susceptibility Pattern of Candida Isolates in Cases of Vulvovaginal Candidiasis. Alex. J. Med. 2016, 52, 269–277. [Google Scholar]
- Zeng, J.; Zong, L.; Mao, T.; Huang, Y.; Xu, Z. Distribution of Candida Albican Genotype and Candida Species Is Associated with the Severity of Vulvovagianl Candidiasis. Nan Fang Yi Ke Da Xue Xue Bao 2011, 31, 1649–1653. [Google Scholar]
- Ozcan, K.; Ilkit, M.; Ates, A.; Turac-Bicer, A.; Demirhindi, H. Performance of Chromogenic Candida Agar and CHROMagar Candida in Recovery and Presumptive Identification of Monofungal and Polyfungal Vaginal Isolates. Med. Mycol. 2010, 48, 29–34. [Google Scholar] [CrossRef]
- Foxman, B.; Muraglia, R.; Dietz, J.-P.; Sobel, J.D.; Wagner, J. Prevalence of Recurrent Vulvovaginal Candidiasis in 5 European Countries and the United States: Results from an Internet Panel Survey. J. Low. Genit. Tract Dis. 2013, 17, 340–345. [Google Scholar] [CrossRef]
- Landers, D.V.; Wiesenfeld, H.C.; Heine, R.P.; Krohn, M.A.; Hillier, S.L. Predictive Value of the Clinical Diagnosis of Lower Genital Tract Infection in Women. Am. J. Obstet. Gynecol. 2004, 190, 1004–1010. [Google Scholar] [CrossRef]
- Anderson, M.R.; Klink, K.; Cohrssen, A. Evaluation of Vaginal Complaints. JAMA 2004, 291, 1368–1379. [Google Scholar] [CrossRef]
- Shirvani, F.; Fattahi, M. Molecular Identification of Candida Species Isolated from Candiduria and Its Risk Factors in Neonates and Children. Curr. Med. Mycol. 2021, 7, 9–12. [Google Scholar] [CrossRef]
- Alam, M.Z.; Alam, Q.; Jiman-Fatani, A.; Kamal, M.A.; Abuzenadah, A.M.; Chaudhary, A.G.; Akram, M.; Haque, A. Candida Identification: A Journey from Conventional to Molecular Methods in Medical Mycology. World J. Microbiol. Biotechnol. 2014, 30, 1437–1451. [Google Scholar] [CrossRef]
- Pulcrano, G.; Iula, D.V.; Vollaro, A.; Tucci, A.; Cerullo, M.; Esposito, M.; Rossano, F.; Catania, M.R. Rapid and Reliable MALDI-TOF Mass Spectrometry Identification of Candida Non-Albicans Isolates from Bloodstream Infections. J. Microbiol. Methods 2013, 94, 262–266. [Google Scholar] [CrossRef]
- Magalhães, J.; Correia, M.J.; Silva, R.M.; Esteves, A.C.; Alves, A.; Duarte, A.S. Molecular Techniques and Target Selection for the Identification of Candida Spp. in Oral Samples. Appl. Sci. 2022, 12, 9204. [Google Scholar] [CrossRef]
- Alexander, B.D.; Pfaller, M.A. Contemporary Tools for the Diagnosis and Management of Invasive Mycoses. Clin. Infect. Dis. 2006, 43, S15–S27. [Google Scholar] [CrossRef]
- Reef, S.E.; Lasker, B.A.; Butcher, D.S.; McNeil, M.M.; Pruitt, R.; Keyserling, H.; Jarvis, W.R. Nonperinatal Nosocomial Transmission of Candida Albicans in a Neonatal Intensive Care Unit: Prospective Study. J. Clin. Microbiol. 1998, 36, 1255–1259. [Google Scholar] [CrossRef]
- del Pilar Vercher, M.; García Martínez, J.M.; Cantón, E.; Pemán, J.; Gómez García, M.M.; Gómez, E.V.; del Castillo Agudo, L. Differentiation of Candida Parapsilosis, C. Orthopsilosis, and C. Metapsilosis by Specific PCR Amplification of the RPS0 Intron. Int. J. Med. Microbiol. 2011, 301, 531–535. [Google Scholar] [CrossRef] [PubMed]
- Odds, F.C. Molecular Phylogenetics and Epidemiology of Candida Albicans. Future Microbiol. 2010, 5, 67–79. [Google Scholar] [CrossRef] [PubMed]
- Price, C.P. Point of Care Testing. BMJ 2001, 322, 1285–1288. [Google Scholar] [CrossRef] [PubMed]
- Nichols, J.H. Utilizing Point-of-Care Testing to Optimize Patient Care. EJIFCC 2021, 32, 140–144. [Google Scholar] [PubMed]
- Mori, Y.; Kitao, M.; Tomita, N.; Notomi, T. Real-Time Turbidimetry of LAMP Reaction for Quantifying Template DNA. J. Biochem. Biophys. Methods 2004, 59, 145–157. [Google Scholar] [CrossRef] [PubMed]
- Biswas, G.; Sakai, M. Loop-Mediated Isothermal Amplification (LAMP) Assays for Detection and Identification of Aquaculture Pathogens: Current State and Perspectives. Appl. Microbiol. Biotechnol. 2014, 98, 2881–2895. [Google Scholar] [CrossRef]
- Parida, M.M. Rapid and Real-Time Detection Technologies for Emerging Viruses of Biomedical Importance. J. Biosci. 2008, 33, 617–628. [Google Scholar] [CrossRef] [PubMed]
- Dean, D.; Swaminathan, S.; Kama, M.; Goemans, S.; Faktaufon, D.; Alnabelseya, N.; Spelke, D.; Kahrizi, K.; Black, M.; Mitra, D. Development and Evaluation of a Point-of-Care Test in a Low-Resource Setting with High Rates of Chlamydia Trachomatis Urogenital Infections in Fiji. J. Clin. Microbiol. 2021, 59, e0018221. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Xiao, F.; Fu, J.; Huang, X.; Jia, N.; Xu, Z.; Wang, Y.; Cui, X. Loop-Mediated Isothermal Amplification Coupled With Nanoparticle-Based Lateral Biosensor for Rapid, Sensitive, and Specific Detection of Bordetella Pertussis. Front. Bioeng. Biotechnol. 2021, 9, 797957. [Google Scholar] [CrossRef] [PubMed]
- Fallahi, S.; Babaei, M.; Rostami, A.; Mirahmadi, H.; Arab-Mazar, Z.; Sepahvand, A. Diagnosis of Candida Albicans: Conventional Diagnostic Methods Compared to the Loop-Mediated Isothermal Amplification (LAMP) Assay. Arch. Microbiol. 2020, 202, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhao, X.; Zhou, Y.; Lu, J.; Yu, H.; Li, S. Establishment and Application of Loop-Mediated Isothermal Amplification Coupled with Nanoparticle-Based Lateral Flow Biosensor (LAMP-LFB) for Visual and Rapid Diagnosis of Candida Albicans in Clinical Samples. Front. Bioeng. Biotechnol. 2022, 10, 1025083. [Google Scholar] [CrossRef]
- Budziszewska, M.; Wieczorek, P.; Obrępalska-Stęplowska, A. One-Step Reverse Transcription Loop-Mediated Isothermal Amplification (RT-LAMP) for Detection of Tomato Torrado Virus. Arch. Virol. 2016, 161, 1359–1364. [Google Scholar] [CrossRef]
- Li, X.; Zhou, Y.; Ji, H.; Xu, Z.; Zhu, L. One-Step Reverse Transcription-Loop-Mediated Isothermal Amplification Assay for Sensitive and Rapid Detection of Porcine Kobuvirus. J. Virol. Methods 2014, 207, 1–5. [Google Scholar] [CrossRef]
- Arenas, M.; Pereira, F.; Oliveira, M.; Pinto, N.; Lopes, A.M.; Gomes, V.; Carracedo, A.; Amorim, A. Forensic Genetics and Genomics: Much More than Just a Human Affair. PLoS Genet. 2017, 13, e1006960. [Google Scholar] [CrossRef]
- WHO. The Use of Loop-Mediated Isothermal Amplification (TB-LAMP) for the Diagnosis of Pulmonary Tuberculosis: Policy Guidance; WHO Guidelines Approved by the Guidelines Review Committee; World Health Organization: Geneva, Switzerland, 2016; ISBN 978-92-4-151118-6. [Google Scholar]
- Wong, Y.-P.; Othman, S.; Lau, Y.-L.; Radu, S.; Chee, H.-Y. Loop-Mediated Isothermal Amplification (LAMP): A Versatile Technique for Detection of Micro-Organisms. J. Appl. Microbiol. 2018, 124, 626–643. [Google Scholar] [CrossRef]
- da Silva, S.J.R.; Pardee, K.; Pena, L. Loop-Mediated Isothermal Amplification (LAMP) for the Diagnosis of Zika Virus: A Review. Viruses 2019, 12, 19. [Google Scholar] [CrossRef]
- Foo, P.C.; Chan, Y.Y.; Mohamed, M.; Wong, W.K.; Nurul Najian, A.B.; Lim, B.H. Development of a Thermostabilised Triplex LAMP Assay with Dry-Reagent Four Target Lateral Flow Dipstick for Detection of Entamoeba histolytica and Non-Pathogenic Entamoeba spp. Anal. Chim. Acta 2017, 966, 71–80. [Google Scholar] [CrossRef]
- Tanner, N.A.; Evans, T.C. Loop-Mediated Isothermal Amplification for Detection of Nucleic Acids. Curr. Protoc. Mol. Biol. 2014, 105, 15.14.1–15.14.14. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.J.; Park, B.H.; Jung, J.H.; Choi, G.; Lee, D.C.; Kim, D.H.; Seo, T.S. Centrifugal Loop-Mediated Isothermal Amplification Microdevice for Rapid, Multiplex and Colorimetric Foodborne Pathogen Detection. Biosens. Bioelectron. 2016, 75, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Jia, B.; Li, X.; Liu, W.; Lu, C.; Lu, X.; Ma, L.; Li, Y.-Y.; Wei, C. GLAPD: Whole Genome Based LAMP Primer Design for a Set of Target Genomes. Front. Microbiol. 2019, 10, 2860. [Google Scholar] [CrossRef] [PubMed]
- Waterfield, T.; Fairley, D.; Blackwood, B.; McKenna, J.; Shields, M.D. A Systematic Review of the Diagnostic Accuracy of Loop-Mediated-Isothermal AMPlification (LAMP) in the Diagnosis of Invasive Meningococcal Disease in Children. BMC Pediatr. 2019, 19, 49. [Google Scholar] [CrossRef]
| Methods | Cultivation | Sensitivity (95% CI) | Specificity (95% CI) | Positive Predictive Value (95% CI) | Negative Predictive Value (95% CI) | Kappa Value | |
|---|---|---|---|---|---|---|---|
| Positive | Negative | ||||||
| Microscopy | 92.05% (83.77–96.47%) | 99.12% (94.50–99.95%) | 98.78% (92.45–99.94%) | 94.17% (94.50–99.95%) | 0.919 | ||
| Positive | 81 | 1 | |||||
| Negative | 7 | 113 | |||||
| LAMP | 90.91% (82.38–95.71%) | 100% (95.93–100%) | 100% (94.29–100%) | 93.44% (87.08–96.92%) | 0.919 | ||
| Positive | 80 | 0 | |||||
| Negative | 8 | 114 | |||||
| Methods | Culture Plus ITS | Sensitivity (95% CI) | Specificity (95% CI) | Positive Predictive Value (95% CI) | Negative Predictive Value (95% CI) | Kappa Value | |
|---|---|---|---|---|---|---|---|
| Positive | Negative | ||||||
| Real-time PCR | 92.54% (82.74–97.22%) | 90.37% (83.78–94.57%) | 82.67% (71.82–90.09%) | 96.06% (90.59–98.54%) | 0.805 | ||
| Positive | 62 | 13 | |||||
| Negative | 5 | 122 | |||||
| LAMP | 94.03% (84.65–98.07%) | 100% (96.55–100%) | 100% (92.84–100%) | 97.1% (92.34–99.07%) | 0.955 | ||
| Positive | 63 | 0 | |||||
| Negative | 4 | 135 | |||||
| CHROMagar | 95.52% (86.62–98.84%) | 99.26% (95.32–99.96%) | 98.46% (90.60–99.92%) | 97.81% (93.24–99.43%) | 0.955 | ||
| Positive | 64 | 1 | |||||
| Negative | 3 | 134 | |||||
| Methods | Culture Plus ITS | Sensitivity (95% CI) | Specificity (95% CI) | Positive Predictive Value (95% CI) | Negative Predictive Value (95% CI) | Kappa Value | |
|---|---|---|---|---|---|---|---|
| Positive | Negative | ||||||
| LAMP | 100% (71.66–100%) | 100% (97.51–100%) | 100% (71.66–100%) | 100% (97.51–100%) | 1 | ||
| Positive | 13 | 0 | |||||
| Negative | 0 | 189 | |||||
| CHROMagar | 76.92% (45.98–93.83%) | 98.94% (95.83–99.82%) | 83.33% (50.88–97.06%) | 98.42% (95.08–99.59%) | 0.787 | ||
| Positive | 10 | 2 | |||||
| Negative | 3 | 187 | |||||
| Methods | Culture Plus ITS | Sensitivity (95% CI) | Specificity (95% CI) | Positive Predictive Value (95% CI) | Negative Predictive Value (95% CI) | Kappa Value | |
|---|---|---|---|---|---|---|---|
| Positive | Negative | ||||||
| LAMP | 80% (29.88–98.95%) | 100% (97.62–100%) | 100% (39.58–100%) | 99.49% (96.79–99.97%) | 0.886 | ||
| Positive | 4 | 0 | |||||
| Negative | 1 | 197 | |||||
| CHROMagar | 60% (17.04–92.74%) | 99.49% (96.77–99.97%) | 75.0% (21.94–98.68%) | 98.99% (96.01–99.82%) | 0.659 | ||
| Positive | 3 | 1 | |||||
| Negative | 2 | 196 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, M.; Jin, X.; Jiang, Q.; Wei, H.; Deng, A.; Mao, Z.; Wang, Y.; Zeng, Z.; Wu, Y.; Liu, S.; et al. Loop-Mediated Isothermal Amplification (LAMP): Potential Point-of-Care Testing for Vulvovaginal Candidiasis. J. Fungi 2023, 9, 1159. https://doi.org/10.3390/jof9121159
Li M, Jin X, Jiang Q, Wei H, Deng A, Mao Z, Wang Y, Zeng Z, Wu Y, Liu S, et al. Loop-Mediated Isothermal Amplification (LAMP): Potential Point-of-Care Testing for Vulvovaginal Candidiasis. Journal of Fungi. 2023; 9(12):1159. https://doi.org/10.3390/jof9121159
Chicago/Turabian StyleLi, Meng, Xiangyu Jin, Qingyun Jiang, Hongbo Wei, Anni Deng, Zeyin Mao, Ying Wang, Zhen Zeng, Yifan Wu, Shuai Liu, and et al. 2023. "Loop-Mediated Isothermal Amplification (LAMP): Potential Point-of-Care Testing for Vulvovaginal Candidiasis" Journal of Fungi 9, no. 12: 1159. https://doi.org/10.3390/jof9121159
APA StyleLi, M., Jin, X., Jiang, Q., Wei, H., Deng, A., Mao, Z., Wang, Y., Zeng, Z., Wu, Y., Liu, S., Kim, J., Wang, X., Liu, Y., Liu, J., Lv, W., Huang, L., Liao, Q., Huang, G., & Zhang, L. (2023). Loop-Mediated Isothermal Amplification (LAMP): Potential Point-of-Care Testing for Vulvovaginal Candidiasis. Journal of Fungi, 9(12), 1159. https://doi.org/10.3390/jof9121159






