Fungi Sensitization in Spain: Importance of the Alternaria alternata Species and Its Major Allergen Alt a 1 in the Allergenicity
Abstract
:1. Introduction
2. Materials and Methods
3. Results
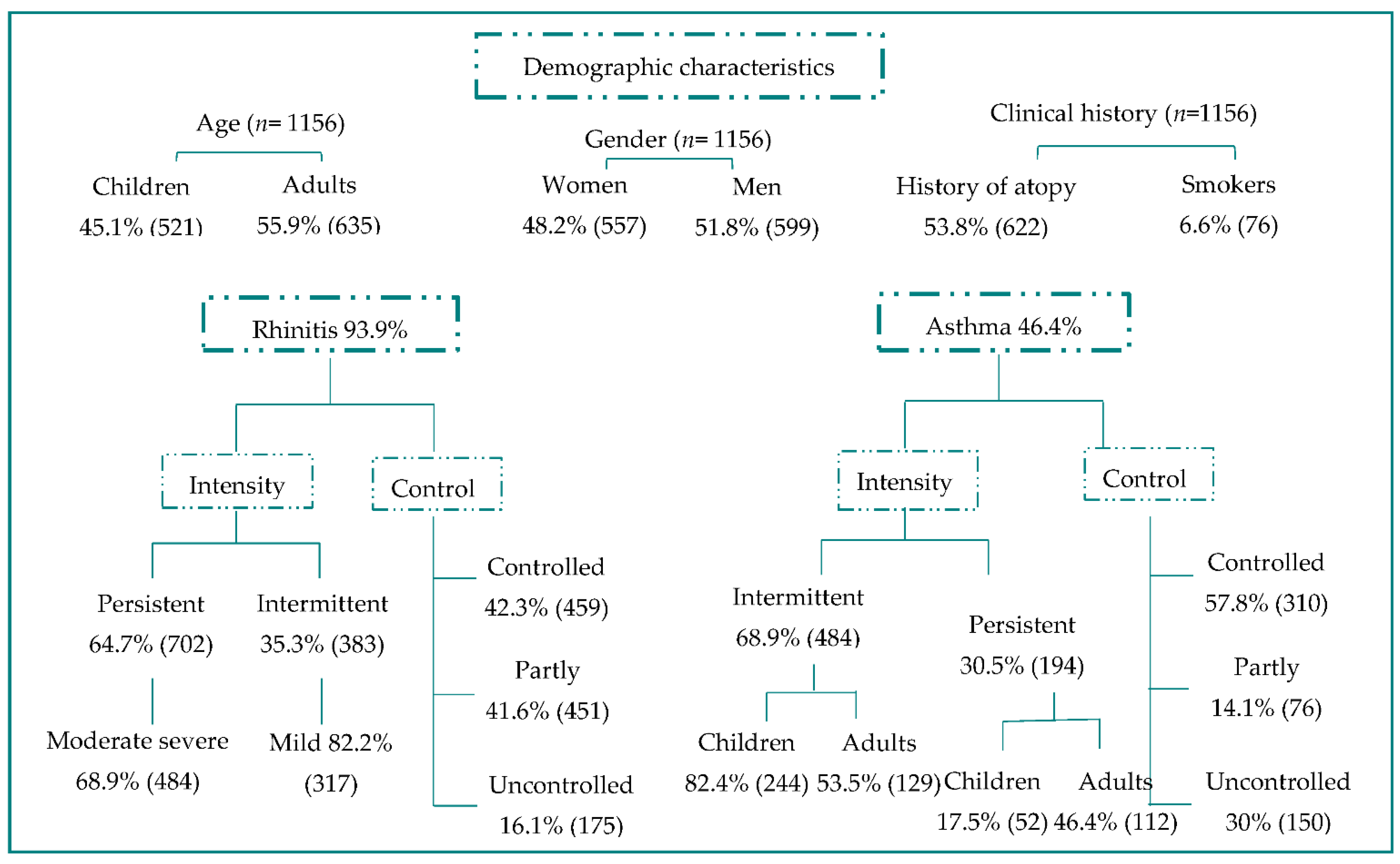
3.1. Recruitment
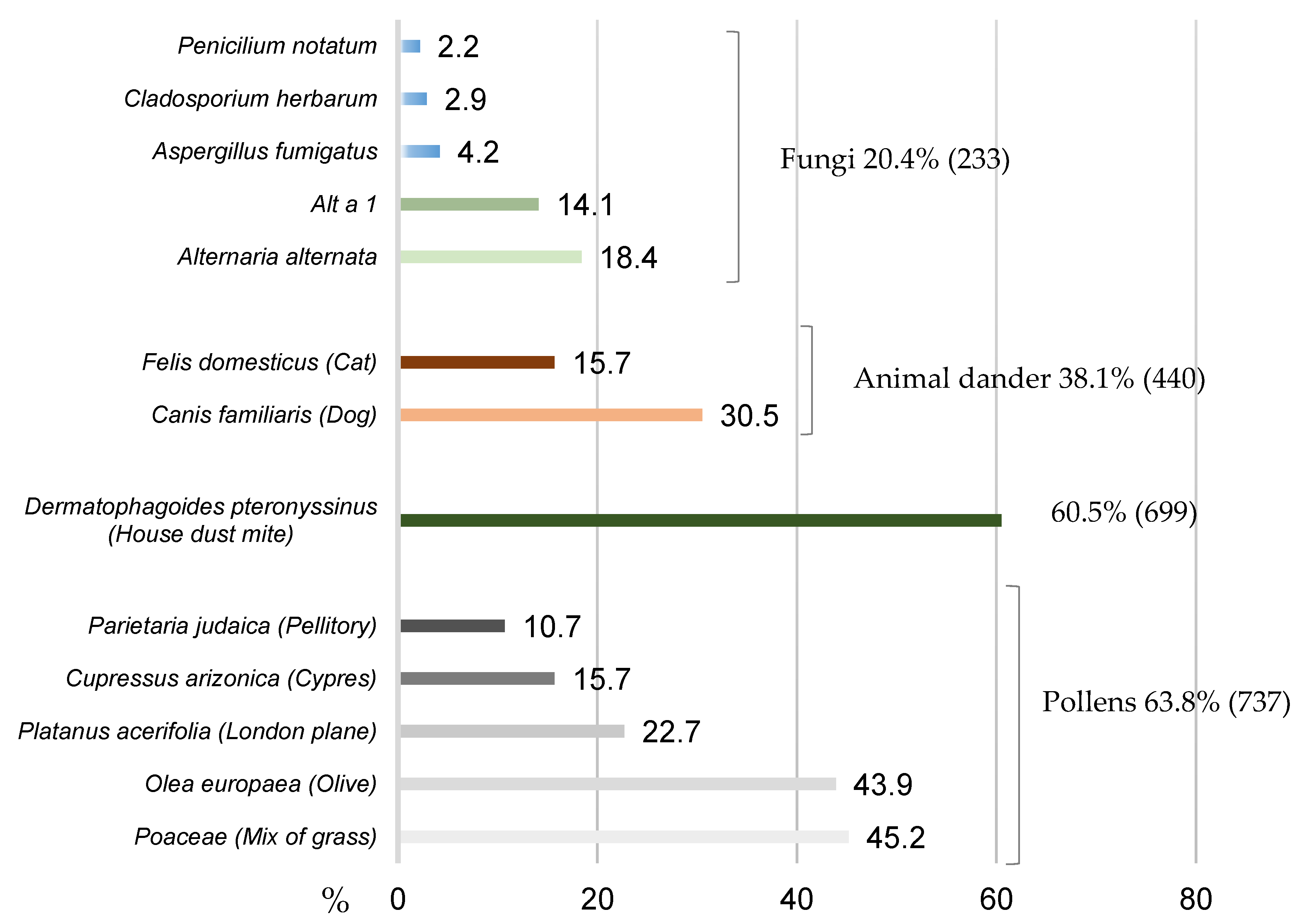
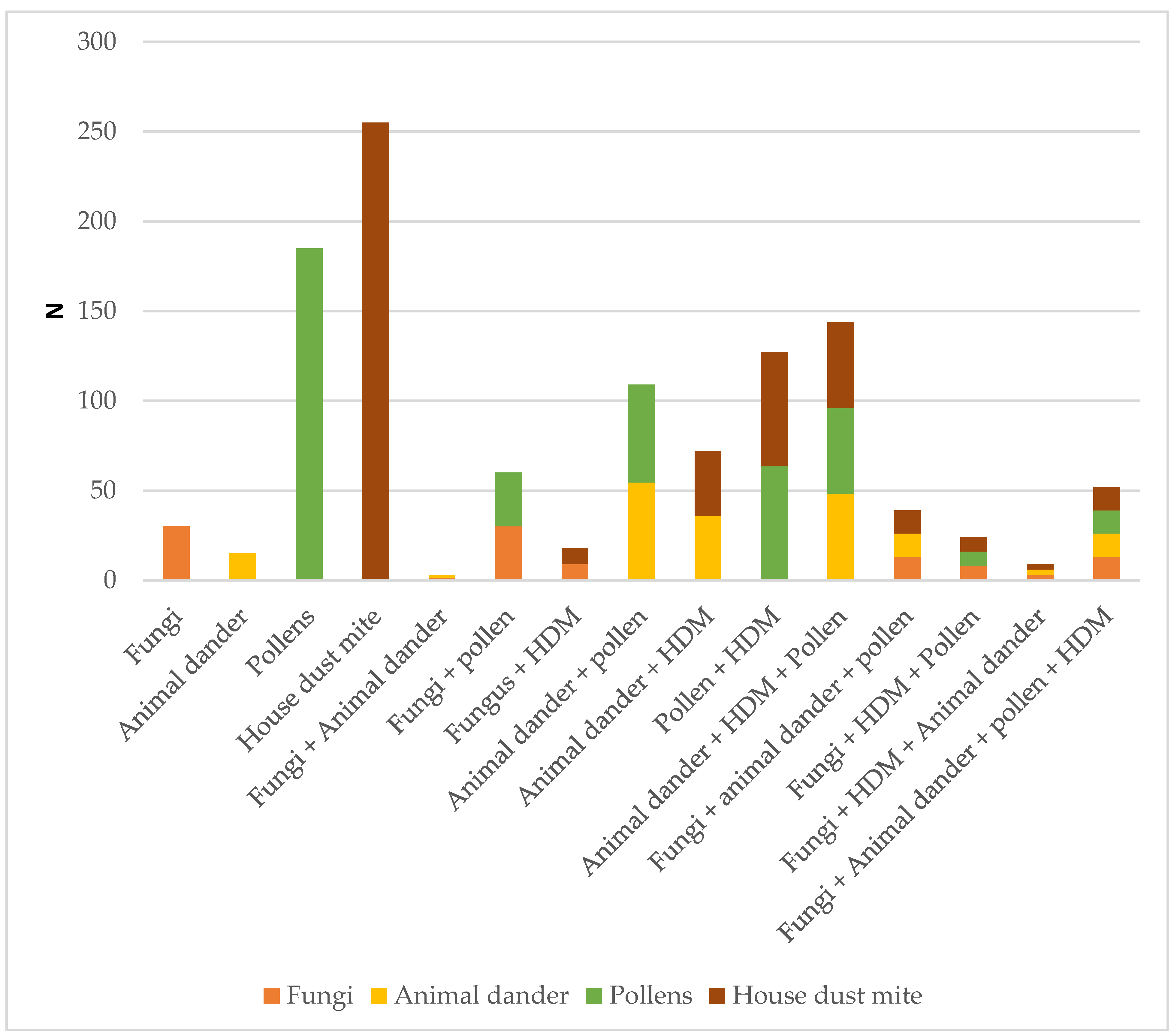
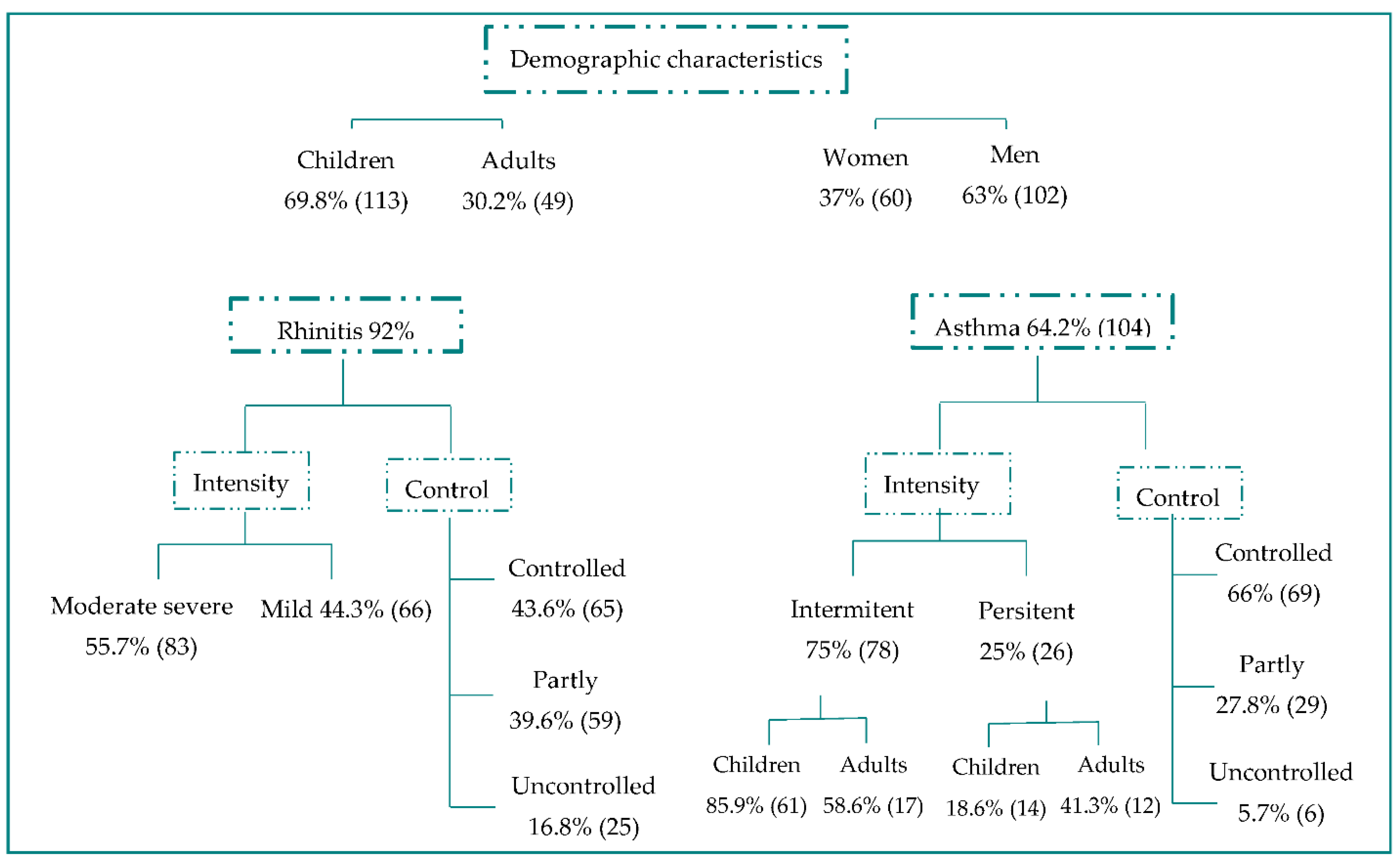
3.2. Primary Objective
3.3. Secondary Objectives
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Mold Questionnaire Part 1
| Sensitization | Alternaria alternata/Alt a 1 | |
| Part 1 | N | % |
| 161 | 100.0 |
| 76 | 47.2 |
| 85 | 52.8 |
| 162 | 100.0 |
| 76 | 46.9 |
| 86 | 53.1 |
| 160 | 100.0 |
| 52 | 32.5 |
| 108 | 67.5 |
| 160 | 100.0 |
| 71 | 44.4 |
| 89 | 55.6 |
| 161 | 100.0 |
| 50 | 31.1 |
| 111 | 68.9 |
| 161 | 100.0 |
| 81 | 50.3 |
| 80 | 49.7 |
| 161 | 100.0 |
| 97 | 60.2 |
| 64 | 39.8 |
Appendix B. Mold Questionnaire Part 2
| Sensitization | Alternaria alternata/Alt a 1 | |
| Part 2 | N | % |
| 162 | 100.0 |
| 37 | 22.8 |
| 125 | 77.2 |
| 162 | 100.0 |
| 9 | 5.6 |
| 4 | 2.5 |
| 4 | 2.5 |
| 37 | 22.8 |
| 108 | 66.7 |
| 162 | 100.0 |
| 42 | 25.9 |
| 120 | 74.1 |
| 162 | 100.0 |
| 55 | 34.0 |
| 107 | 66.0 |
| 162 | 100.0 |
| 7 | 4.3 |
| 154 | 95.7 |
References
- Hawksworth, D.L. The fungal dimension of biodiversity: Magnitude, significance and conservation. Micol. Res. 2006, 95, 641–645. [Google Scholar] [CrossRef]
- Twaroch, T.E.; Curin, M.; Valenta, R.; Swoboda, I. Mold allergens in respiratory allergy: From structure to therapy. Allergy Asthma Immunol. Res. 2015, 7, 205–220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mari, A.; Scheneider, P.; Wally, V.; Breitenbach, M.; Simon-Nobbe, B. Sensitization to fungi: Epidemiology, comparative skin test and IgE reactivity of fungal extracts. Clin. Exp. Allergy 2003, 33, 1429–1438. [Google Scholar] [CrossRef]
- Bousquet, P.J.; Hooper, R.; Kogevinas, M.; Jarvis, D.; Burney, P. Number of allergens to be tested to asses allergenic sensitization in epidemiologicstudies: Results of the European Community Respiratory Health Survey I. Clin. Exp. Allergy 2007, 37, 780–787. [Google Scholar] [CrossRef]
- Heinzeding, L.I.; Burbaeh, G.J.; Edenharter, G. GA2LEN skin test study: GA2LEN harmonization of skin prick testing: Novel sensitization patterns for inhalant allergens in Europe. Allergy 2009, 64, 1498–1506. [Google Scholar] [CrossRef]
- Arbes, S.J., Jr.; Gergen, P.J.; Elliott, L.; Zeldin, D.C. Prevalences of positive skin test responses to 10 common allergens in the US population: Results from the third National Health and Nutrition Examination Survey. J. Allergy Clin. Immunol. 2005, 116, 377–383. [Google Scholar] [CrossRef]
- D’amato, G.; Chatzigeorgiou, G.; Corsico, R.; Gioulekas, D.; Jäger, L.; Jäger, S.; Kontou-Fili, K.; Kouridakis, S.; Liccardi, G.; Meriggi, A.; et al. Evaluation of the prevalence of skin prick test positivity to Alternaria and Cladosporium in patients with suspected respiratory allergy. A European multicenter study promoted by the Subcommittee on Aerobiology and Environmental aspects of inhalant allergens of the European Academy of Allergology and Clinical Immunology. Allergy 1997, 52, 711–716. [Google Scholar]
- Deards, M.J.; Montagne, A.E. Purification and characterization of a major allergen of Alternaria alternata. Mol. Immunol. 1991, 28, 408–415. [Google Scholar] [CrossRef]
- Chruszcz, M.; Chapman, M.D.; Osinski, T.; Solberg, R.; Demas, M.; Porebski, P.; Majorek, K.A.; Pomés, A.; Minor, W. Alternaria alternata allergen Alt a 1: A unique β-barrel protein dimer found exclusively in fungi. J. Allergy Clin. Immunol. 2012, 130, 241–247. [Google Scholar] [CrossRef] [Green Version]
- Twaroch, T.E.; Arcalís, E.; Sterflinger, K.; Stöger, E.; Swoboda, I.; Valenta, R. Predominant localization of the major Alternaria alternata allergen Alt a 1 in the cell wall of airborne spores. J. Allergy Clin. Immunol. 2012, 129, 1148–1149. [Google Scholar] [CrossRef]
- Gutiérrez-Rodríguez, A.; Postigo, I.; Guisantes, J.A.; Suñén, E.; Martínez, J. Identification of allergen homologous to Alt a 1 from Stemphylium botryosum and Ulocladium botrytis. Med. Mycol. 2011, 49, 892–896. [Google Scholar]
- Moreno, A.; Pineda, F.; Alcover, J.; Rodríguez, D.; Palacios, R.; Martínez-Naves, E. Orthologous allergens and diagnostic utility of major allergen Alt a 1. Allergy Asthma Immunol. Res. 2016, 8, 428–435. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simon-Nobbe, B.; Probst, G.; Kajava, A.V.; Oberkofler, H.; Susani, M.; Crameri, R.; Ferreira, F.; Ebner, C.; Breitenbach, M. IgE-binding epitopes of enolases, a class of highly conserved fungal allergens. J. Allergy Clin. Immunol. 2000, 106, 887–895. [Google Scholar] [CrossRef]
- Gabriel, M.F.; Postigo, I.; Gutierrez-Rodriguez, A.; Sunen, E.; Guisantes, J.; Tomaz, C.T.; Martinez, J. Characterization of Alternaria alternata manganese-dependent superoxide dismutase, a cross-reactive allergen homologue to Asp f 6. Immunology 2015, 220, 851–858. [Google Scholar]
- Gabriel, M.F.; Postigo, I.; Tomaz, C.T.; Martínez, J. Markers of exposure, phylogeny and risk of fungi-induced respiratory allergy. Environ. Int. 2016, 89–90, 71–80. [Google Scholar] [CrossRef]
- Kim, H.-K.; Lund, S.; Baum, R.; Rosenthal, P.; Khorram, N.; Doherty, T.A. Innate Type 2 Response to Alternaria Extract Enhances Ryegrass-Induced Lung Inflammation. Int. Arch. Allergy Immunol. 2014, 163, 92–105. [Google Scholar] [CrossRef] [Green Version]
- Cantani, A.; Clachi, V. Epidemiology of Alternaria alternata allergy: A prospective study in 6840 Italian asthmatic children. Eur. Rev. Med. Pharmacol. Sci. 2004, 8, 289–294. [Google Scholar] [PubMed]
- Burbach, G.J.; Heinzerling, L.M.; Edenharter, G.; Bachert, C.; Bindslev-Jensen, C.; Bonini, S.; Bousquet, J.; Bousquet-Rouanet, L.; Bousquet, P.J.; Bresciani, M.; et al. GA2LEN skin test study II: Clinical relevance of inhalant allergen sensitizations in Europe. Allergy 2009, 64, 1507–1515. [Google Scholar] [CrossRef] [PubMed]
- Zureik, M.; Neukirch, C.; Leynaert, B.; Liard, R.; Bousquet, J.; Neukirch, F. European Community Respuratory Health Survey. Sensitization to airborne molds and severity of asthma: Cross sectional study from European Community Respiratory Health Survey. BMJ 2002, 125, 411–414. [Google Scholar] [CrossRef] [Green Version]
- Black, P.N.; Udy, A.A.; Brodie, S.M. Sensitivity to fungal allergens is a risk factor for life-threatening asthma. Allergy 2000, 55, 501–504. [Google Scholar] [CrossRef] [PubMed]
- Pose, G.; Patriarca, A.; Kyanko, V.; Pardo, A.; Pinto, V.F. Effect of water activity and temperature on growth of Alternaria alternata on a syntetic tomato medium. Int. J. Food Microbiol. 2009, 135, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Pose, G.; Patriarca, A.; Kyanko, V.; Pardo, A.; Pinto, V.F. Water activity and temperature effects on mycotoxin production by Alternaria alternata on a syntetic tomato médium. Int. J. Food Microbiol. 2010, 142, 348–353. [Google Scholar] [CrossRef] [PubMed]
- Weber, R.W. Alternaria alternata. Ann. Allergy Asthma Immunol. 2001, 87, A-4. [Google Scholar]
- Bush, R.K.; Prochman, J.J. Case study: Alternaria induced asthma. J. Allergy Clin. Immunol. 2004, 113, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Ishibashi, M.; Tonori, H.; Miki, T.; Miyajima, E.; Kudo, Y.; Tsunoda, M.; Sakabe, K.; Aizawa, Y. Classification of patients complaining of skin house syndrome and/or multiple chemical sensitivity. Tohoku J. Exp. Med. 2007, 211, 223–233. [Google Scholar] [CrossRef] [Green Version]
- Rapiejko, P.; Lipiec, A.; Wojdas, A.; Jurkiewicz, D. Treshold pollen concentration necessary to evoke allergic symptoms. Int. Rev. Allergol. Clin. 2004, 10, 91–94. [Google Scholar]
- Javier Martín Vide y Jorge Olcina. Climas y Tiempos de España; Alianza Editorial: Madrid, Spain, 2001; p. 258. [Google Scholar]
- Brożek, J.L.; Bousquet, J.; Agache, I.; Agarwal, A.; Bachert, C.; Bosnic-Anticevich, S.; Brignardello-Petersen, R.; Canonica, G.W.; Casale, T.; Chavannes, N.H.; et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines—2016 revision. J. Allergy Clin. Immunol. 2017, 140, 950–958. [Google Scholar] [CrossRef] [Green Version]
- GEMA 5.0 Guía Española Para el Manejo del Asma. Available online: www.gemasma.com (accessed on 2 August 2021).
- Vega, J.M.; Badia, X.; Badiola, C.; López-Viña, A.; Olaguíbel, J.M.; Picado, C.; Sastre, J.; Dal-Ré, R. Validation of the Spanish version of the asthma control test (ACT). J. Asthma 2007, 44, 867–872. [Google Scholar] [CrossRef]
- Pérez-Yarza, E.G.; Castro-Rodriguez, J.A.; Villa Asensi, J.R.; Garde Garde, J.; Hidalgo Bermejo, F.J.; on behalf of the VESCASI Group. Validación de la versión en español de la prueba de control del asma infantil (ACT) para su uso en España [Validation of a Spanish version of the Childhood Asthma Control Test (Sc-ACT) for use in Spain]. An. Pediatr. 2015, 83, 94–103. (In Spanish) [Google Scholar] [CrossRef] [PubMed]
- Spanish Society of Allergology and Clinical Immunology. Allergológica 2015. In Spanish Society of Allergology and Clinical Immunology. Available online: https://www.seaic.org/inicio/noticias-general/alergologica-2015.html (accessed on 2 August 2021).
- Warm, K.; Hedman, L.; Lindberg, A.; Lötvall, J.; Lundbäck, B.; Rönmark, E. Allergic sensitization isa ge-dependently associated with rhinitis, but les so with asthma. J. Allergy Clin. Immunol. 2015, 136, 1559–1565. [Google Scholar] [CrossRef] [PubMed]
- Crameri, R.; Zeller, S.; Glaser, A.G.; Vilhelmsson, M.; Rhyner, C. Cross-reactivity among fungal allergens: A clinically relevant phenomenon? Mycoses 2009, 52, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Chew, G.L.; Horner, W.E.; Kennedy, K.; Grimes, C.; Barnes, C.S.; Phipatanakul, W.; Larenas-Linnemann, D.; Miller, J.D.; Portnoy, J.; Levetin, E.; et al. Environmental Allergens Workgroup. Procedures to Assist Health Care Providers to Determine When Home Assessments for Potential Molds Exposure Are Warranted. J. Allergy Clin. Immunol. Pract. 2016, 4, 417–422.e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karvonen, A.M.; Hyvarinen, A.; Korppi, M.; Haverinen-Shaughnessy, U.; Renz, H.; Pfefferle, P.I.; Remes, S.; Genuneit, J.; Pekkanen, J. Moisture damage and asthma: A birth cohort study. Pediatrics 2015, 135, e598–e606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larenas-Linnemann, D.; Baxi, S.; Phipatanakul, W.; Portnoy, J.M.; Barnes, C.; Grimes, C.; Horner, W.E.; Kennedy, K.; Levetin, E.; Miller, J.D.; et al. Environmental Allergens Workgroup. Clinical Evaluation and Management of Patients with Suspected Fungus Sensitivity. J. Allergy Clin. Immunol. Pract. 2016, 4, 405–414. [Google Scholar] [CrossRef]
| Centers | Children | Adults | Total (%) |
|---|---|---|---|
| Andalusia | 126 | 269 | 395 (34.1) |
| Catalonia | 181 | 106 | 287 (24.8) |
| Extremadura | 96 | 99 | 195 (16.9) |
| Valencian Community | 98 | 50 | 148 (12.8) |
| Galicia | 18 | 82 | 100 (8.7) |
| Basque Country | 2 | 29 | 31 (2.7) |
| Total | 521 | 635 | 1156 (100) |
| Centers | Patients Included N | Positive SPT to Any Fungi N (%) | Positive IgE to A. alternata and Alt a 1 N (%) | Positive SPT to A. alternata and Alt a 1 | |
|---|---|---|---|---|---|
| Children N (%) | Adults N (%) | ||||
| Andalusia | 395 | 78 (19.7) | 55 (13.9) | 20 (5.1) | 28 (7.1%) |
| Catalonia | 287 | 81 (28.2) | 51 (17.8) | 34 (11.8) | 22 (7.7%) |
| Extremadura | 195 | 53 (27.2) | 41 (21.0) | 30 (15.4) | 12 (6.2%) |
| Valencian Community | 148 | 15 (10.1) | 12 (8.1) | 8 (5.4) | 2 (1.4%) |
| Galicia | 100 | 1 (1.0) | 1 (1.0) | 1 (1.0) | 0 (0%) |
| Basque Country | 31 | 5 (16.1) | 2 (6.5) | 0 (0) | 2 (6.5%) |
| Total | 1156 | 233 (20.2) | 162 (14.0) | 93 (8.0) | 64 (5.5%) |
| Bioclimatic Areas | Patients Included N | Positive SPT to Any Fungi N (%) | Positive IgE to A. alternata or Alt a 1 N (%) |
|---|---|---|---|
| Mediterranean | 592 | 124 (20.9) | 71 (12.0) |
| Semidesert | 201 | 27 (13.4) | 14 (7.0) |
| Continental | 232 | 76 (32.8) | 59 (25.4) |
| Oceanic | 131 | 6 (4.6) | 3 (2.3) |
| Total | 1156 | 233 (20.2) | 147 (12.7) |
| Fungus | Sensitized (n = 233) | With Allergic Rhinitis (n = 214)/% |
|---|---|---|
| Alternaria alternata and Alt a 1 | 162 | 149/92% |
| Cladosporium herbarum | 31 | 31/100% |
| Aspergillus fumigatus | 45 | 43/95.5% |
| Penicilium notatum | 24 | 23/95.8% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López Couso, V.P.; Tortajada-Girbés, M.; Rodriguez Gil, D.; Martínez Quesada, J.; Palacios Pelaez, R. Fungi Sensitization in Spain: Importance of the Alternaria alternata Species and Its Major Allergen Alt a 1 in the Allergenicity. J. Fungi 2021, 7, 631. https://doi.org/10.3390/jof7080631
López Couso VP, Tortajada-Girbés M, Rodriguez Gil D, Martínez Quesada J, Palacios Pelaez R. Fungi Sensitization in Spain: Importance of the Alternaria alternata Species and Its Major Allergen Alt a 1 in the Allergenicity. Journal of Fungi. 2021; 7(8):631. https://doi.org/10.3390/jof7080631
Chicago/Turabian StyleLópez Couso, Verónica P., Miguel Tortajada-Girbés, David Rodriguez Gil, Jorge Martínez Quesada, and Ricardo Palacios Pelaez. 2021. "Fungi Sensitization in Spain: Importance of the Alternaria alternata Species and Its Major Allergen Alt a 1 in the Allergenicity" Journal of Fungi 7, no. 8: 631. https://doi.org/10.3390/jof7080631
APA StyleLópez Couso, V. P., Tortajada-Girbés, M., Rodriguez Gil, D., Martínez Quesada, J., & Palacios Pelaez, R. (2021). Fungi Sensitization in Spain: Importance of the Alternaria alternata Species and Its Major Allergen Alt a 1 in the Allergenicity. Journal of Fungi, 7(8), 631. https://doi.org/10.3390/jof7080631







