The Impacts of Aspergillosis on Outcome, Burden and Risks for Mortality in Influenza Patients with Critical Illness
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Definition
2.3. Statistical Analysis
3. Results
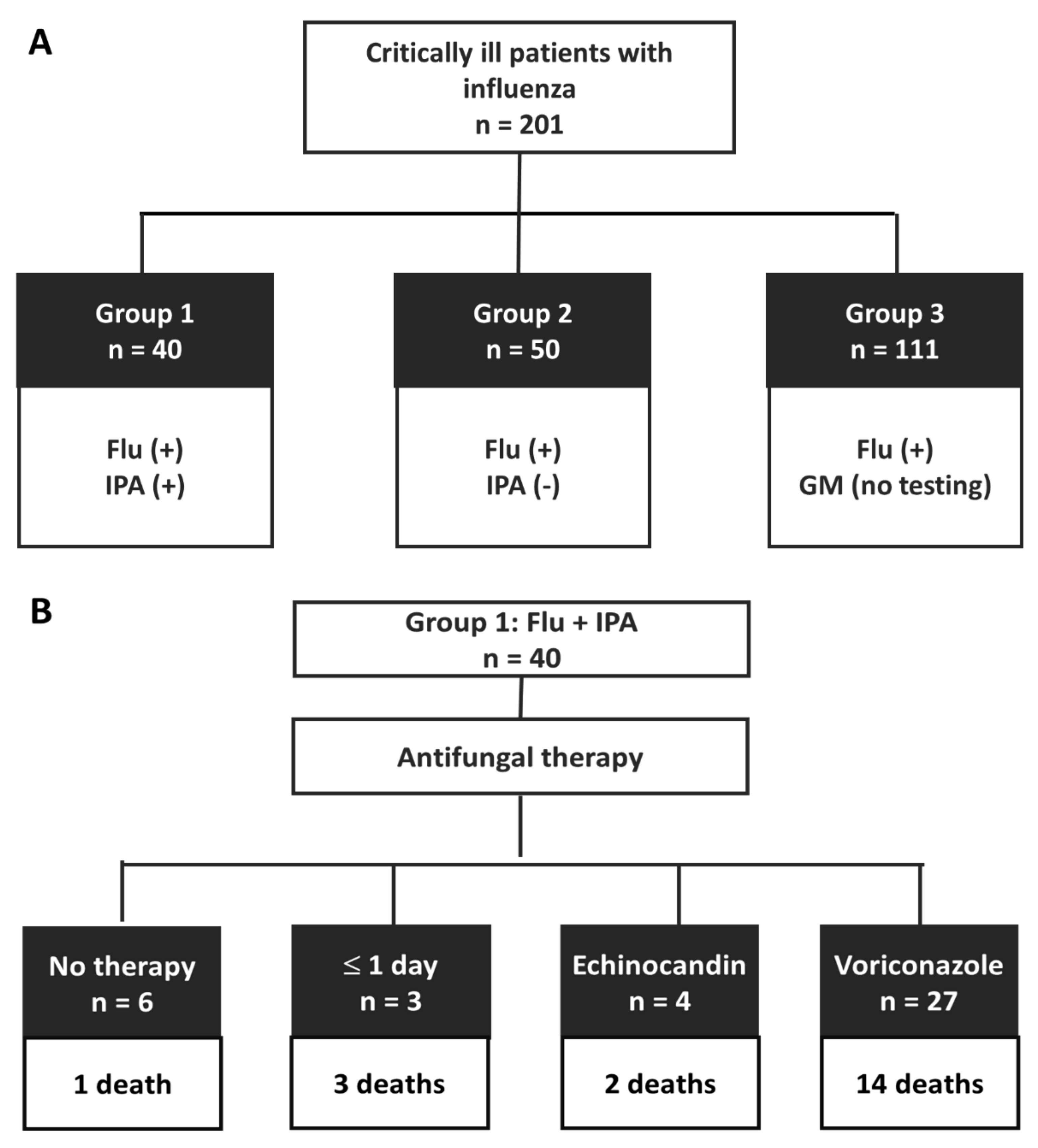
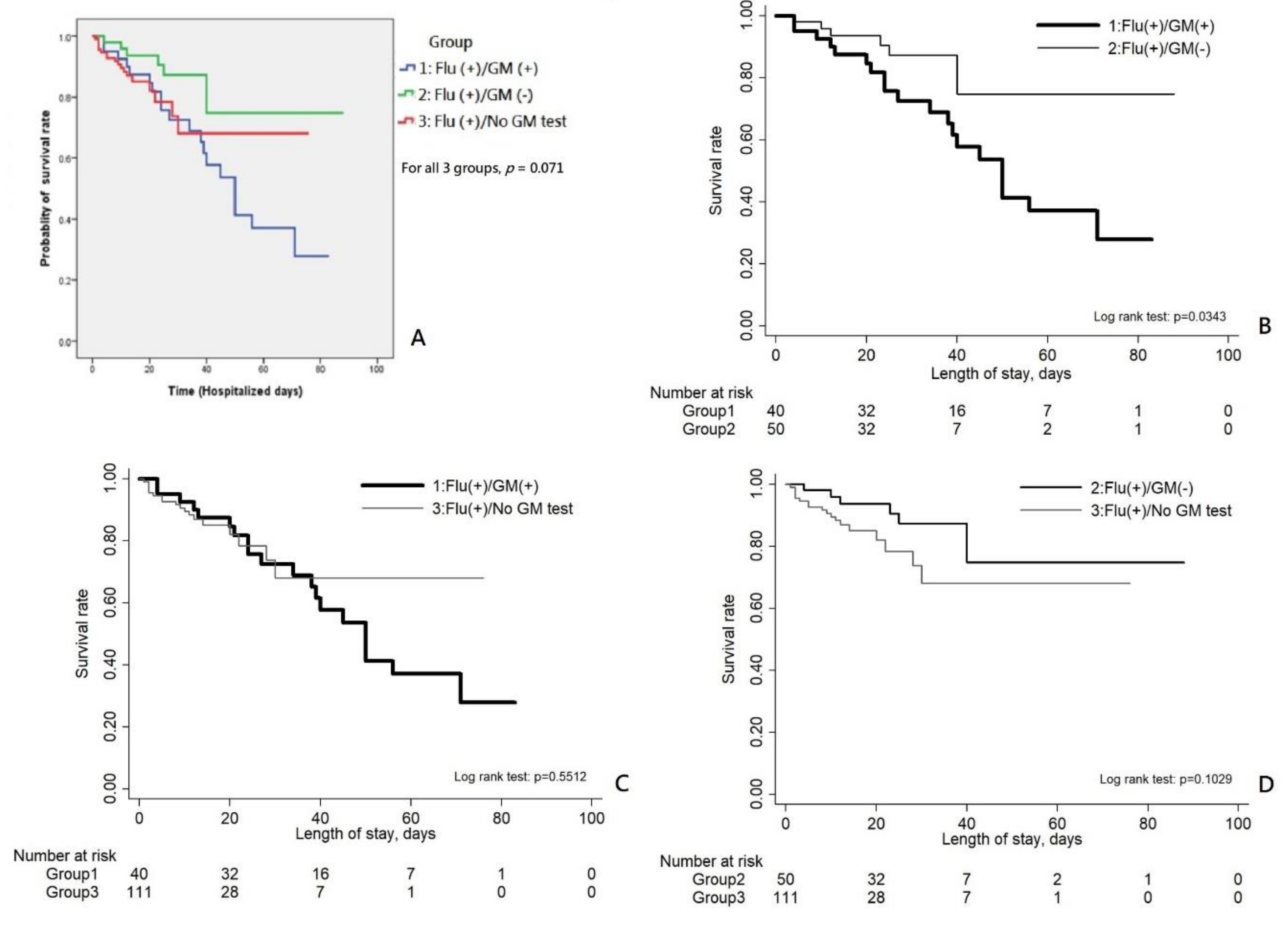
3.1. Study Subjects
3.2. Clinical Characteristics of Patients with Severe Influenza
3.3. Clinical Characteristics of Patients with Coinfection of IPA and Influenza
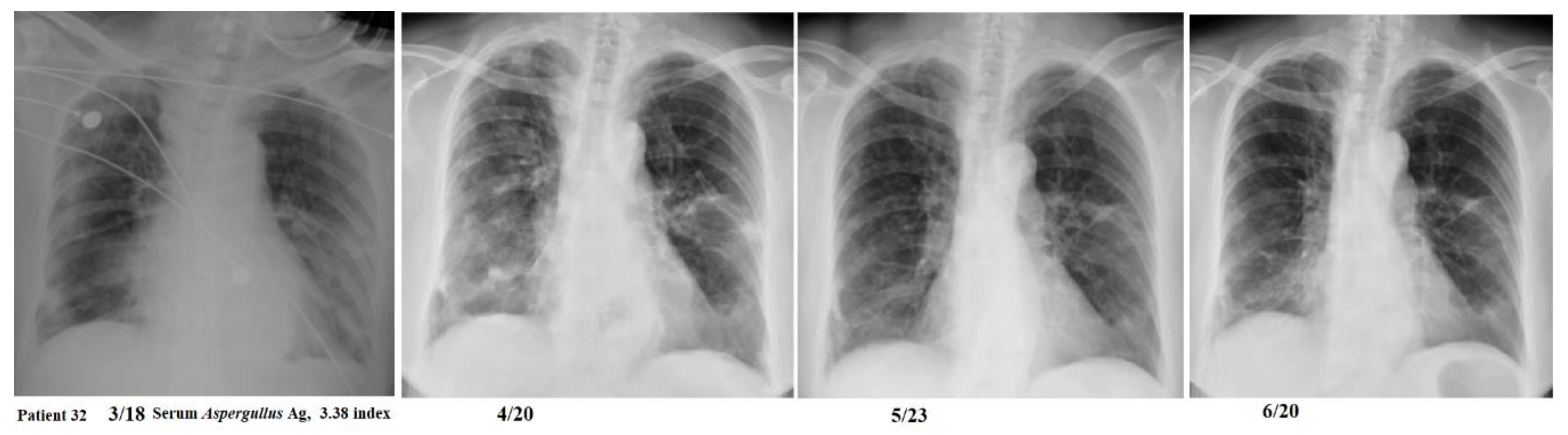
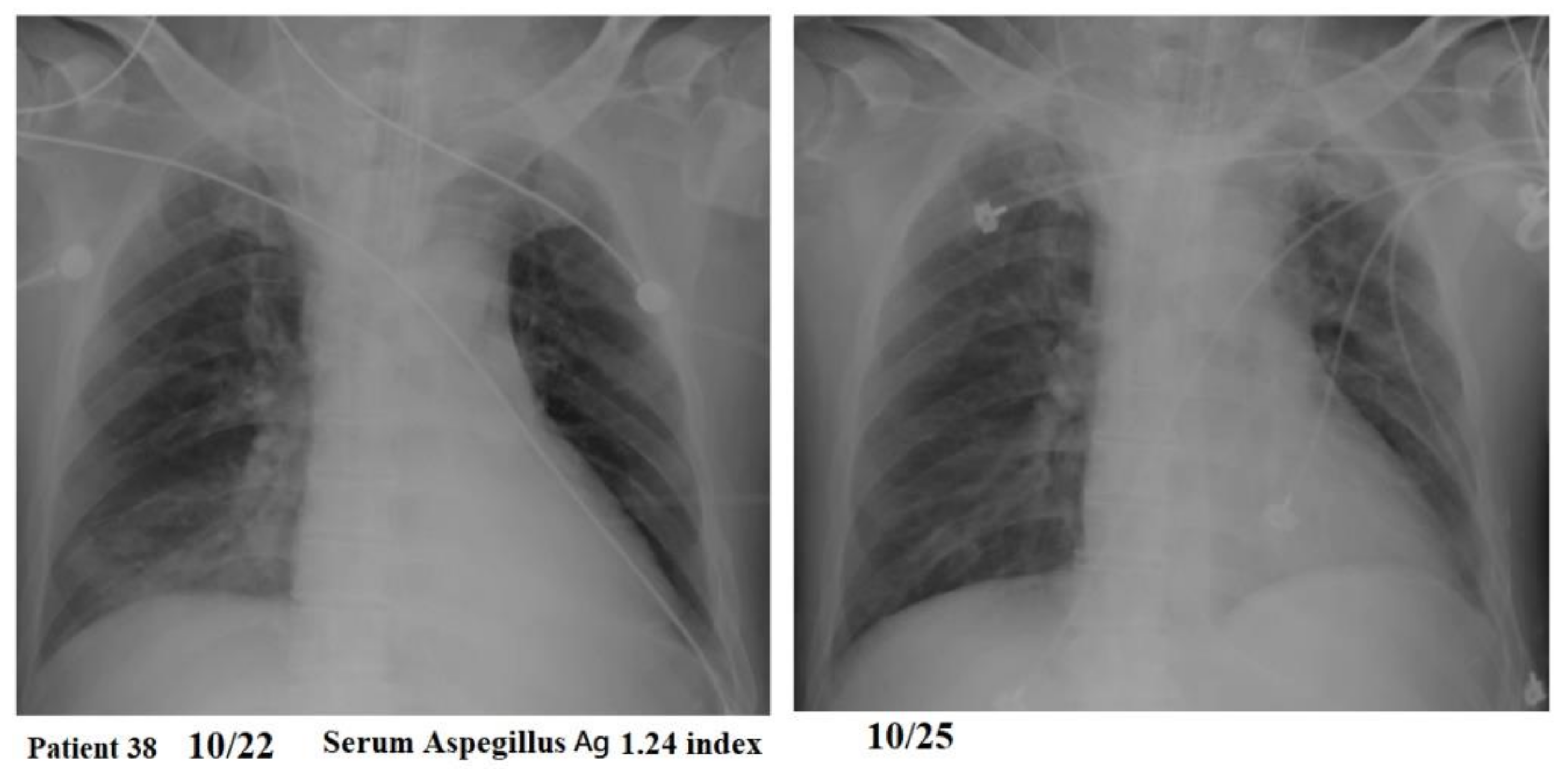
3.4. Outcome of IPA-Coinfected Influenza Patients Receiving Antifungal Therapy
3.5. Risk Factors for Mortality of Group 1 Patients (Flu with IPA)
3.6. Risk Factors for Mortality of Group 1 and Group 2 Patients (Severe Flu with and without IPA)
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Blanchard, E.; Gabriel, F.; Jeanne-Leroyer, C.; Servant, V.; Dumas, P.Y. Invasive pulmonary aspergillosis. Rev. Mal. Respir. 2018, 35, 171–187. [Google Scholar] [CrossRef]
- Gregg, K.S.; Kauffman, C.A. Invasive aspergillosis: Epidemiology, clinical aspects, and treatment. Semin. Respir. Crit. Care Med. 2015, 36, 662–672. [Google Scholar] [CrossRef]
- Thompson, G.R., 3rd; Patterson, T.F. Pulmonary aspergillosis: Recent advances. Semin. Respir. Crit. Care Med. 2011, 32, 673–681. [Google Scholar] [CrossRef]
- Tudesq, J.J.; Peyrony, O.; Lemiale, V.; Azoulay, E. Invasive pulmonary aspergillosis in nonimmunocompromised hosts. Semin. Respir. Crit. Care Med. 2019, 40, 540–547. [Google Scholar] [CrossRef]
- Bassetti, M.; Righi, E.; De Pascale, G.; De Gaudio, R.; Giarratano, A.; Mazzei, T.; Morace, G.; Petrosillo, N.; Stefani, S.; Antonelli, M. How to manage aspergillosis in non-neutropenic intensive care unit patients. Crit. Care 2014, 18, 458. [Google Scholar] [CrossRef] [Green Version]
- Dimopoulos, G.; Frantzeskaki, F.; Poulakou, G.; Armaganidis, A. Invasive aspergillosis in the intensive care unit. Ann. N. Y. Acad. Sci. 2012, 1272, 31–39. [Google Scholar] [CrossRef]
- Huang, L.; Zhang, N.; Huang, X.; Xiong, S.; Feng, Y.; Zhang, Y.; Li, M.; Zhan, Q. Invasive pulmonary aspergillosis in patients with influenza infection: A retrospective study and review of the literature. Clin. Respir. J. 2019, 13, 202–211. [Google Scholar] [CrossRef]
- Vanderbeke, L.; Spriet, I.; Breynaert, C.; Rijnders, B.J.A.; Verweij, P.E.; Wauters, J. Invasive pulmonary aspergillosis complicating severe influenza: Epidemiology, diagnosis and treatment. Curr. Opin. Infect. Dis. 2018, 31, 471–480. [Google Scholar] [CrossRef]
- Ku, Y.H.; Chan, K.S.; Yang, C.C.; Tan, C.K.; Chuang, Y.C.; Yu, W.L. Higher mortality of severe influenza patients with probable aspergillosis than those with and without other coinfections. J. Formos. Med. Assoc. 2017, 116, 660–670. [Google Scholar] [CrossRef]
- Verweij, P.E.; Rijnders, B.J.A.; Brüggemann, R.J.M.; Azoulay, E.; Bassetti, M.; Blot, S.; Calandra, T.; Clancy, C.J.; Cornely, O.A.; Chiller, T.; et al. Review of influenza-associated pulmonary aspergillosis in ICU patients and proposal for a case definition: An expert opinion. Intensive Care Med. 2020, 46, 1524–1535. [Google Scholar] [CrossRef]
- Coste, A.; Frérou, A.; Raute, A.; Couturaud, F.; Morin, J.; Egreteau, P.Y.; Blanc, F.X.; Reignier, J.; Tadié, J.M.; Tran, A.; et al. The extend of aspergillosis in critically ill patients with severe influenza pneumonia: A multicenter cohort study. Crit. Care Med. 2021, 49, 934–942. [Google Scholar] [CrossRef]
- Schauwvlieghe, A.; Rijnders, B.J.A.; Philips, N.; Verwijs, R.; Vanderbeke, L.; Van Tienen, C.; Lagrou, K.; Verweij, P.E.; Van de Veerdonk, F.L.; Gommers, D.; et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: A retrospective cohort study. Lancet Respir. Med. 2018, 6, 782–792. [Google Scholar] [CrossRef]
- Nyga, R.; Maizel, J.; Nseir, S.; Chouaki, T.; Milic, I.; Roger, P.A.; van Grunderbeeck, N.; Lemyze, M.; Totet, A.; Castelain, S.; et al. Invasive tracheobronchial aspergillosis in critically ill patients with severe influenza. A clinical trial. Am. J. Respir. Crit. Care Med. 2020, 202, 708–716. [Google Scholar] [CrossRef]
- Wauters, J.; Baar, I.; Meersseman, P.; Meersseman, W.; Dams, K.; De Paep, R.; Lagrou, K.; Wilmer, A.; Jorens, P.; Hermans, G. Invasive pulmonary aspergillosis is a frequent complication of critically ill H1N1 patients: A retrospective study. Intensive Care Med. 2012, 38, 1761–1768. [Google Scholar] [CrossRef]
- Guervilly, C.; Roch, A.; Ranque, S.; Forel, J.M.; Hraiech, S.; Xeridat, F.; Adda, M.; Papazian, L. A strategy based on galactomannan antigen detection and PCR for invasive pulmonary aspergillosis following influenza A (H1N1) pneumonia. J. Infect. 2012, 65, 470–473. [Google Scholar] [CrossRef]
- Crum-Cianflone, N.F. Invasive aspergillosis associated with severe influenza infections. Open Forum Infect. Dis. 2016, 3, ofw171. [Google Scholar] [CrossRef] [Green Version]
- Zhou, W.; Li, H.; Zhang, Y.; Huang, M.; He, Q.; Li, P.; Zhang, F.; Shi, Y.; Su, X. Diagnostic value of galactomannan antigen test in serum and bronchoalveolar lavage fluid samples from patients with nonneutropenic invasive pulmonary aspergillosis. J. Clin. Microbiol. 2017, 55, 2153–2161. [Google Scholar]
- Donnelly, J.P.; Chen, S.C.; Kauffman, C.A.; Steinbach, W.J.; Baddley, J.W.; Verweij, P.E.; Clancy, C.J.; Wingard, J.R.; Lockhart, S.R.; Groll, A.H.; et al. Revision and update of the consensus definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin. Infect. Dis. 2020, 71, 1367–1376. [Google Scholar] [CrossRef] [Green Version]
- Blot, S.I.; Taccone, F.S.; van den Abeele, A.M.; Bulpa, P.; Meersseman, W.; Brusselaers, N.; Dimopoulos, G.; Paiva, J.A.; Misset, B.; Rello, J.; et al. A clinical algorithm to diagnose invasive pulmonary aspergillosis in critically ill patients. Am. J. Respir. Crit. Care Med. 2012, 186, 56–64. [Google Scholar]
- Martin-Loeches, I.; Schultz, M.J.; Vincent, J.L.; Alvarez-Lerma, F.; Bos, L.D.; Solé-Violán, J.; Torres, A.; Rodriguez, A. Increased incidence of co-infection in critically ill patients with influenza. Intensive Care Med. 2017, 43, 48–58. [Google Scholar] [CrossRef]
- Liu, J.W.; Ku, Y.H.; Chao, C.M.; Ou, H.F.; Ho, C.H.; Chan, K.S.; Yu, W.L. Epidemiological correlation of pulmonary aspergillus infections with ambient pollutions and influenza A (H1N1) in southern Taiwan. J. Fungi 2021, 7, 227. [Google Scholar] [CrossRef]
- Van de Veerdonk, F.L.; Kolwijck, E.; Lestrade, P.P.; Hodiamont, C.J.; Rijnders, B.J.; van Paassen, J.; Haas, P.J.; Oliveira Dos Santos, C.; Kampinga, G.A.; Bergmans, D.C.; et al. Influenza-associated aspergillosis in critically ill patients. Am. J. Respir. Crit. Care Med. 2017, 196, 524–527. [Google Scholar]
- Corcione, S.; Lupia, T.; Raviolo, S.; Montrucchio, G.; Trentalange, A.; Curtoni, A.; Cavallo, R.; de Rosa, F.G. Putative invasive pulmonary aspergillosis within medical wards and intensive care units: A 4-year retrospective, observational, single-centre study. Intern. Emerg. Med. 2021, 16, 1619–1627. [Google Scholar] [CrossRef]
- Kuo, C.W.; Wang, S.Y.; Tsai, H.P.; Su, P.L.; Cia, C.T.; Lai, C.H.; Chen, C.W.; Shieh, C.C.; Lin, S.H. Invasive pulmonary aspergillosis is associated with cytomegalovirus viremia in critically ill patients—A retrospective cohort study. J. Microbiol. Immunol. Infect. 2021. [Google Scholar] [CrossRef]
| Variables | Group 1 (n = 40) | Group 2 (n = 50) | Group 3 (n = 111) | p Value |
|---|---|---|---|---|
| Hospital (CMMC), no. (%) | 31 (77.5) | 37 (74) | 53 (47.7) * | <0.001 |
| Female, no. (%) | 16 (40) | 20 (40) | 43 (38.7) | 0.984 |
| Age (mean ± SD) | 60 ± 14 * | 66 ± 13 | 70 ± 14 | <0.001 |
| BMI (mean ± SD) | 24.5 ± 4.8 | 25 ± 4.7 | 23.9 ± 6.1 | 0.496 |
| Underlying diseases, no. (%) | ||||
| Diabetes mellitus | 19 (47.5) | 20 (40) | 42 (37.8) | 0.565 |
| Chronic obstructive pulmonary disease | 2 (5) | 3 (6) | 17 (15.3) | 0.087 |
| Solid cancer | 9 (22.5) * | 2 (4) | 10 (9) | 0.013 |
| ESRD with maintenance dialysis | 3 (7.5) | 6 (12) | 11 (9.9) | 0.815 F |
| Liver cirrhosis | 3 (7.5) | 5 (10) | 4 (3.6) | 0.233 F |
| Hematological malignance | 1 (2.5) | 0 | 2 (1.8) | 0.771 F |
| Solid organ transplant recipient | 2 (5) | 1 (2) | 0 (0) | 0.051 F |
| HIV infection | 0 | 0 | 0 | - |
| Autoimmune disease | 0 | 0 | 0 | - |
| Charlson comorbidity index (mean ± SD) | 4.4 ± 2.5 | 5.2 ± 2.7 | 5.2 ± 2.2 | 0.161 |
| Steroid (prednisolone or equivalent), no. (%) | ||||
| Long-term use, >0.3 mg/kg/day, >3weeks | 0 | 0 | 0 | |
| Within 3 weeks, >5 mg/day, >7 days | 1 (2.5) | 2 (4) | 1 (0.9) | 0.308 F |
| In ICU, >5 mg/day, >5 days | 31 (77.5) * | 22 (44) | 48 (43.2) | 0.001 |
| Daily dose (mg) | 30.6 ± 13.3 | 27 ± 17.2 | 25.1 ± 19 | 0.230 |
| Total dose (mg) | 629.5 ± 507.3 | 424.4 ± 430.5 | 170.7 ± 199.1 * | <0.001 W |
| Duration (day) | 19.9 ± 15.8 | 14.7 ± 16 | 5.5 ± 6.8 * | <0.001 W |
| Temperature (°C) on admission (mean ± SD) | 37 ± 0.7 | 37.1 ± 0.8 | 37 ± 0.7 | 0.746 |
| Fever (≥38 °C) on admission, no. (%) | 3 (7.5) | 6 (12) | 13 (11.7) | 0.826 |
| Severity status, no. (%) | ||||
| APACHE II score (mean ± SD) | 21.1 ± 10.4 | 18.0 ± 8.5 | 18.1 ± 8.2 | 0.236 W |
| SOFA score (mean ± SD) | 7.7 ± 4.4 * | 6.7 ± 4.2 a | 5.5 ± 5 a | 0.030 |
| Ventilator use | 25 (62.5) | 33 (66) | 41 (36.9) * | 0.001 |
| On ECMO | 1 (2.5) | 0 | 1 (0.9) | 0.420 F |
| Complications, no. (%) | ||||
| Septic shock | 39 (97.5) | 48 (96) | 106 (95.5) | 1.000 |
| Bloodstream infection | 7 (17.5) | 4 (8) | 8 (7.2) | 0.158 |
| Acute kidney injury (Creatinine > 2 mg/dL) | 15 (37.5) | 10 (23.3) | 32 (30.8) | 0.369 |
| Acute jaundice (Total bilirubin > 2 mg/dL) | 4 (16.7) | 2 (6.9) | 3 (5.9) | 0.339 F |
| Platelet count <100,000/μL | 7 (17.9) | 6 (12) | 17 (15.3) | 0.731 |
| Blood PCR for Cytomegalovirus DNA | 7 (17.5) * | 4 (8) a | 1 (0.9) a | 0.006 |
| Chest X-ray finding | ||||
| Normal | None | None | None | - |
| Peribronchial infiltrations | 2 (5) | 2 (4) | 14 (45.9) | 0.129 |
| Bilateral lung patch infiltrates | 7 (17.5) | 12 (24) | 51 (45.9) * | <0.001 |
| Multiple patches with necrotizing processes | 10 (25) | 17 (34) | 29 (26.1) | 0.531 |
| Diffuse ground-glass appearance | 6 (15) | 9 (18) | 9 (8.1) | 0.161 |
| Extensive consolidation on one lung | 1 (2.5) | 2 (4) | 7 (6.3) | 0.596 |
| Extensive consolidation on bilateral lungs | 11 (27.5) * | 6 (12) a | 1 (0.9) a | <0.001 |
| Diffuse air-space infiltration pattern | 3 (7.5) | 2 (4) | 0 (0) | - |
| ARDS, no. (%) | 33 (82.5) * | 32 (66.7) | 58 (63) | 0.003 |
| Mild | 5 (12.5) | 11 (22.9) | 25 (27.2) | 0.382 |
| Moderate | 16 (40) | 12 (25) | 26 (28.3) | 0.111 |
| Severe | 12 (30) * | 9 (18.8) | 7 (7.6) | <0.001 |
| PaO2/FiO2 ratio (mean ± SD) | 210 ± 185 * | 259 ± 231 | 310 ± 217 | 0.034 |
| Bacterial coinfections (within 2 days), no. (%) | 18 (45) | 20 (41.7) | 37 (38.1) | 0.746 |
| Influenza assay | ||||
| RIDT (negative result) | 14 (35) * | 11 (22) | 18 (16.2) | 0.045 |
| Influenza A (H1N1) | 15 (37.5) | 19 (38) | 26 (23.4) | 0.087 |
| Influenza A (H3N2) | 3 (7.5) * | 19 (38) a | 71 (64) a | <0.001 |
| Influenza A (negative for H1N1 and H3N2) | 15 (37.5) * | 7 (14) | 6 (5.4) | <0.001 |
| Influenza B | 7 (17.5) | 5 (10) | 8 (7.2) | 0.176 |
| Inflammatory markers | ||||
| White blood cell count/μL (mean ± SD) × 1000 | 11.1 ± 6.2 | 10.7 ± 5.1 | 10.9 ± 7.1 | 0.944 |
| Lymphopenia (<1000/μL), no. (%) | 33 (82.5) * | 33 (66) | 67 (64.4) | 0.040 |
| C-reactive protein (mean ± SD) | 135.3 ± 129 | 105.6 ± 80.8 | 42 ± 54 | 0.051 |
| Procalcitonin (mean ± SD) | 22.8 ± 45.5 | 25 ± 51.4 | 18.5 ± 37.1 | 0.788 |
| Platelet count/μL (mean ± SD) × 1000 | 175.4 ± 79.5 | 182.5 ± 74.5 | 172.4 ± 82.5 | 0.759 |
| Antiviral therapy | ||||
| Oseltamivir, no. (%) | 37 (92.5) | 45 (90) | 99 (89.2) | 0.903 |
| Peramivir, no. (%) | 6 (15) | 7 (14) | 22 (19.8) | 0.602 |
| Antifungal therapy | ||||
| Voriconazole, no. (%) | 27 (67.5) * | 1 (2) | 1 (0.9) | <0.001 |
| Caspofungin, no. (%) | 8 (20) | 0 (0) | 0 (0) | - |
| Liposomal amphotericin B, no. (%) | 3 (7.5) | 0 (0) | 0 (0) | - |
| Anidulafungin, no. (%) | 3 (7.5) | 0 (0) | 0 | - |
| Clinical outcome | ||||
| ICU stay >21 days, no. (%) | 20 (50) * | 7 (14) | 8 (7.2) | <0.001 |
| Hospitalization day (mean ± SD) | 37 ± 21.4 * | 26.7 ± 16.1 | 16.1 ± 12.6 | <0.001 W |
| Overall death, no. (%) | 20 (50) * | 6 (12) | 18 (16.2) | <0.001 |
| Disease economic burden (NTD) | ||||
| Hospital cost (mean ± SD) | 339,133 ± 245,959 * | 112,391 ± 81,738 | 64,620 ± 99,841 | <0.001 W |
| Drug fee (mean ± SD) | 256,782 ± 199,789 * | 59,285 ± 57,589 | 28,793 ± 64,565 | <0.001 W |
| Laboratory fee (mean ± SD) | 82,350 ± 103,220 a | 53,105 ± 36,953 | 35,826 ± 60,280 a | 0.010 W |
| Patient | Age. Sex | Ventilator Use | ARDS | P/F Ratio | Day of IPA Dx Post Influenza (d) | Total Dose (mg) | Outcome | Hospital Stay (d) | Serum GM Index | BAL GM Index |
|---|---|---|---|---|---|---|---|---|---|---|
| No therapy | ||||||||||
| Patient 7 | 38 F | nil | moderate | 165.6 | 23 | 0 | survived | 68 | 0.60 | NA |
| Patient 10 | 57 M | nil | moderate | 155.6 | 9 | 0 | survived | 39 | 0.50 | NA |
| Patient 17 | 58 F | nil | moderate | 124 | 6 | 0 | survived | 17 | 0.78 | NA |
| Patient 20 | 61 F | yes | moderate | 162 | 10 | 0 | died | 20 | 0.65 | NA |
| Patient 32 | 64 F | nil | moderate | 141.6 | 2 | 0 | survived | 20 | 3.38 | NA |
| Patient 38 | 48 M | yes | nil | 694 | 1 | 0 | survived | 9 | 1.24 | 0.19 |
| Inadequate therapy | ||||||||||
| Patient 3 | 45 F | yes | moderate | 184 | 7 | C 70 | died | 4 | 0.56 | NA |
| Patient 25 | 59 M | yes | severe | 86.13 | 64 | V 900 | died | 71 | 1.93 | NA |
| Patient 30 | 59 M | nil | mild | 259.7 | 2 | V 300 | died | 4 | 3.35 | NA |
| Alternative therapy | ||||||||||
| Patient 27 | 56 F | nil | mild | 214.3 | 33 | A 500 | died | 50 | 1.99 | NA |
| Patient 33 | 60 M | yes | moderate | 172.67 | 1 | M 1000 | survived | 31 | 0.69 | NA |
| Patient 36 | 60 M | yes | nil | 382.67 | 14 | C 670 | died | 39 | 13.63 | NA |
| Patient 40 | 36 F | yes | nil | 504 | 6 | A 3600 | survived | 25 | 0.14 | 8.19 |
| Variables | Group1 (n = 40) | Survival (n = 20) | Death (n = 20) | p Value |
|---|---|---|---|---|
| Female, no. (%) | 16 (40) | 9 (56.3) | 7 (43.7) | 0.748 |
| Age (mean ± SD) | 60 ± 14 | 55.9 ± 13.6 | 64.5 ± 13.3 | 0.050 |
| BMI (mean ± SD) | 24.5 ± 4.8 | 25.0 ± 5.2 | 24.1 ± 4.3 | 0.560 |
| Underlying diseases, no. (%) | ||||
| Diabetes mellitus | 19 (47.5) | 7 (36.8) | 12 (63.2) | 0.205 |
| Solid cancer | 9 (22.5) | 3 (33.3) | 6 (66.6) | 0.451 F |
| ESRD with maintenance dialysis | 3 (7.5) | 2 (66.7) | 1 (33.3) | 1.000 F |
| Liver cirrhosis | 3 (7.5) | 0 (0) | 3 (100) | 0.231 F |
| Charlson comorbidity index (mean ± SD) | 4.4 ± 2.5 | 3.4 ± 2.4 | 5.4 ± 2.3 | 0.010 |
| Steroid (prednisolone or equivalent), no. (%) | ||||
| Daily dose (mg) | 30.6 ± 13.3 | 29.2 ± 16.9 | 32.0 ± 8.5 | 0.510 |
| Total dose (mg) | 629.5 ± 507.3 | 544.4 ± 511.5 | 714.5 ± 501.3 | 0.295 |
| Duration (day) | 19.9 ± 15.8 | 16.9 ± 15.4 | 23.0 ± 16.1 | 0.228 |
| Inflammatory markers | ||||
| Lymphopenia (<1000/μL), no. (%) | 33 (82.5) | 17 (51.5) | 16 (48.5) | 1.000 F |
| C-reactive protein (mean ± SD) | 135.3 ± 129 | 168.3 ± 165.5 | 105.8 ± 78.0 | 0.149 |
| Procalcitonin (mean ± SD) | 22.8 ± 45.5 | 21.6 ± 49.8 | 23.9 ± 42.5 | 0.886 |
| Platelet count/μL (mean ± SD) × 1000 | 175.4 ± 79.5 | 185.3 ± 61.5 | 166.0 ± 94.1 | 0.451 |
| Severity status, no. (%) | ||||
| APACHE II score (mean ± SD) | 21.1 ± 10.4 | 15. 8± 8.4 | 26.4 ± 9.6 | 0.001 |
| SOFA score (mean ± SD) | 7.7 ± 4.4 | 6.9 ± 4.1 | 8.6 ± 4.6 | 0.216 |
| Ventilator use | 25 (62.5) | 12 (48) | 13 (52) | 1.000 |
| Septic shock | 39 (97.5) | 20 (51.3) | 19 (48.7) | 1.000 F |
| ARDS, no. (%) | 33 (82.5) | 16 (48.5) | 17 (51.5) | 1.000 F |
| Severe ARDS, no. (%) | 12 (30) | 3 (25) | 9 (75) | 0.038 |
| PaO2/FiO2 ratio (mean ± SD) | 210 ± 185 | 233.3 ± 156.2 | 197.2 ± 212.4 | 0.661 |
| Bacterial coinfections (within 2 days), no. (%) | 18 (45) | 7 (38.9) | 11 (61.1) | 0.341 |
| Blood PCR for Cytomegalovirus DNA | 7 (17.5) | 3 (42.9) | 4 (57.1) | 1.000 F |
| Influenza assay | 0.588 | |||
| Influenza A (H1N1) | 15 (37.5) | 8 (53.3) | 7 (46.7) | |
| Influenza A (H3N2) | 3 (7.5) | 1 (33.3) | 2 (66.7) | |
| Influenza A (negative for H1N1 and H3N2) | 15 (37.5) | 9 (60) | 6 (40) | |
| Influenza B | 7 (17.5) | 2 (28.6) | 5 (71.4) | |
| Diagnosis criteria for aspergillosis | ||||
| BAL galactomannan level (index) | 2.4 ± 3.4 | 1.6 ± 3.2 | 4.9 ± 3.6 | 0.262 |
| Serum galactomannan level (index) | 1.5 ± 2.3 | 1.1 ± 1.3 | 2.0 ± 3.2 | 0.272 |
| Antiviral therapy | ||||
| Oseltamivir, no. (%) | 37 (92.5) | 18 (48.6) | 19 (51.4) | 1.000 F |
| Peramivir, no. (%) | 6 (15) | 4 (66.7) | 2 (33.3) | 0.661 F |
| Antifungal therapy | ||||
| Voriconazole, no. (%) | 27 (67.5) | 11 (42.3) | 15 (57.7) | 0.320 |
| Caspofungin, no. (%) | 8 (20) | 2 (25) | 6 (75) | 0.235 F |
| Variable | Crude Odds Ratio (95% CI) | p Value | Adjusted Odds Ratio (95% CI) | p Value |
|---|---|---|---|---|
| ARDS | ||||
| Non-severe | 1.00 | 1.00 | ||
| Severe | 4.636 (1.023–21.004) | 0.047 | 24.774 (1.913–320.859) | 0.014 |
| Charlson comorbidity index | 1.467 (1.064–2.023) | 0.019 | 1.569 (1.058–2.327) | 0.025 |
| APACHE II score | 1.128 (1.042–1.221) | 0.003 | 1.150 (1.038–1.275) | 0.008 |
| Variables | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p Value | Odds Ratio | 95% CI | p Value | |
| Clinical group | ||||||
| Group 1: Flu with IPA | 7.33 | 2.56–21.05 | <0.001 | 13.78 | 3.19–59.5 | <0.001 |
| Group 2: Flu without IPA | 1.00 | 1.00 | ||||
| Solid cancer | 3.54 | 0.97–12.8 | 0.055 | |||
| Charlson comorbidity index | 1.16 | 0.98–1.39 | 0.094 | 1.41 | 1.07–1.86 | 0.015 |
| APACHE II score | 1.10 | 1.04–1.17 | 0.001 | 1.10 | 1.02–1.19 | 0.010 |
| SOFA score (mean ± SD) | 1.13 | 1.01–1.26 | 0.029 | |||
| ARDS | ||||||
| Severe degree | 7.00 | 2.41–20.36 | <0.001 | 18.45 | 3.55–95.83 | 0.001 |
| Non-severe | 1.00 | 1.00 | ||||
| Bacterial coinfection | 2.91 | 1.13–7.49 | 0.027 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chao, C.-M.; Lai, C.-C.; Ou, H.-F.; Ho, C.-H.; Chan, K.-S.; Yang, C.-C.; Chen, C.-M.; Yu, W.-L. The Impacts of Aspergillosis on Outcome, Burden and Risks for Mortality in Influenza Patients with Critical Illness. J. Fungi 2021, 7, 922. https://doi.org/10.3390/jof7110922
Chao C-M, Lai C-C, Ou H-F, Ho C-H, Chan K-S, Yang C-C, Chen C-M, Yu W-L. The Impacts of Aspergillosis on Outcome, Burden and Risks for Mortality in Influenza Patients with Critical Illness. Journal of Fungi. 2021; 7(11):922. https://doi.org/10.3390/jof7110922
Chicago/Turabian StyleChao, Chien-Ming, Chih-Cheng Lai, Hsuan-Fu Ou, Chung-Han Ho, Khee-Siang Chan, Chun-Chieh Yang, Chin-Ming Chen, and Wen-Liang Yu. 2021. "The Impacts of Aspergillosis on Outcome, Burden and Risks for Mortality in Influenza Patients with Critical Illness" Journal of Fungi 7, no. 11: 922. https://doi.org/10.3390/jof7110922
APA StyleChao, C.-M., Lai, C.-C., Ou, H.-F., Ho, C.-H., Chan, K.-S., Yang, C.-C., Chen, C.-M., & Yu, W.-L. (2021). The Impacts of Aspergillosis on Outcome, Burden and Risks for Mortality in Influenza Patients with Critical Illness. Journal of Fungi, 7(11), 922. https://doi.org/10.3390/jof7110922






