Therapy and Management of Pneumocystis jirovecii Infection
Abstract
:1. Introduction
2. Diagnosis
3. Primary Prophylaxis
3.1. HIV-Positive Population
3.2. Solid Organ Transplant Recipients
3.3. Haematology Patients
3.4. Other Populations
4. Therapy
4.1. HIV-Positive Population
4.2. Solid Organ Transplant Recipients
4.3. Haematology Patients
5. Secondary Prophylaxis
6. Side-Effects and Interactions
7. Resistance
8. Outbreaks
9. Paediatrics
10. Concluding Remarks
Author Contributions
Conflicts of Interest
References
- Maini, R.; Henderson, K.L.; Sheridan, E.A.; Lamagni, T.; Nichols, G.; Delpech, V.; Phin, N. Increasing Pneumocystis pneumonia, England, UK, 2000–2010. Emerg. Infect. Dis. 2013, 19, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Patterson, L.; Coyle, P.; Curran, T.; Verlander, N.Q.; Johnston, J. Changing epidemiology of Pneumocystis pneumonia, Northern Ireland, UK and implications for prevention, 1 July 2011–31 July 2012. J. Med. Microbiol 2017, 66, 1650–1655. [Google Scholar] [CrossRef] [PubMed]
- Pegorie, M.; Denning, D.W.; Welfare, W. Estimating the burden of Invasive and Serious Fungal Disease in the United Kingdom. J. Infect. 2017, 74, 60–71. [Google Scholar] [CrossRef] [PubMed]
- Buchacz, K.; Lau, B.; Jing, Y.; Bosch, R.; Abraham, A.G.; Gill, M.J.; Silverberg, M.J.; Goedert, J.J.; Sterling, T.R.; Althoff, K.N.; et al. Incidence of AIDS-Defining Opportunistic Infections in a Multicohort Analysis of HIV-infected Persons in the United States and Canada, 2000–2010. J. Infect. Dis. 2016, 214, 862–872. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, K.M.; Ahn, K.W.; Chen, M.; Aljurf, M.D.; Agwu, A.L.; Chen, A.R.; Walsh, T.J.; Szabolcs, P.; Boeckh, M.J.; Auletta, J.J.; et al. The incidence, mortality and timing of Pneumocystis jiroveci pneumonia after hematopoietic cell transplantation: A CIBMTR analysis. Bone Marrow Transplant. 2016, 51, 573–580. [Google Scholar] [CrossRef] [PubMed]
- Avino, L.J.; Naylor, S.M.; Roecker, A.M. Pneumocystis jirovecii pneumonia in the non-HIV infected population. Ann. Pharmacother. 2016, 50, 673–679. [Google Scholar] [CrossRef] [PubMed]
- Iriat, X.; Challan Belval, T.; Fillaux, J.; Esposito, L.; Lavergne, R.A.; Cardeau-Desangles, I.; Roques, O.; Del Bello, A.; Cointault, O.; Lavayssière, L.; et al. Risk factors of Pneumocystis Pneumonia in Solid Organ recipients in the era of the common use of post transplantation prophylaxis. Am. J. Transplant. 2015, 15, 190–199. [Google Scholar]
- Kermani, T.; Ytterberg, S.; Warrington, K. Pneumocystis jiroveci pneumonia in giant cell arteritis: A case series. Arthritis Care Res. 2011, 63, 761–765. [Google Scholar] [CrossRef] [PubMed]
- Weng, C.; Liu, M.; Weng, M.; Lee, N.; Wang, M.; Lin, W.; Ou, C.; Lai, W.; Hsu, S.; Chao, S.; et al. Pneumocystis jirovecii Pneumonia in Systemic Lupus Erythematosus from Southern Taiwan. J. Clin. Rheumatol. 2013, 19, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Ichai, P.; Azoulay, D.; Feray, C.; Saliba, F.; Antoun, F.; Roche, B.; Bismuth, H.; Samuel, D. Pneumocystis carinii and cytomegalovirus pneumonia after corticosteroid therapy in acute severe alcoholic hepatitis: 2 case reports. Gastroenterol. Clin. Biol. 2002, 26, 532–534. [Google Scholar] [PubMed]
- Velayos, F.; Sandborn, W. Pneumocystis carinii Pneumonia During Maintenance Anti-Tumor Necrosis Factor-α Therapy with Infliximab for Crohn’s Disease. Inflamm. Bowel Dis. 2004, 10, 657–660. [Google Scholar] [CrossRef] [PubMed]
- Podlipnik, S.; de la Mora, L.; Alsina, M.; Mascaró, J. Pneumocystis jirovecii pneumonia in a patient with pustular psoriasis with an IL-36RN deficiency treated with infliximab: Case report and review of the literature. Australas. J. Dermatol. 2016, 58, e44–e47. [Google Scholar] [CrossRef] [PubMed]
- Mukasa, Y.; Ichiyasu, H.; Akaike, K.; Okamoto, S.; Komohara, Y.; Kohrogi, H. Autopsy case of pulmonary zygomycosis and Pneumocystis pneumonia in a patient with interstitial pneumonia treated by corticosteroid therapy. Nihon Kokyuki Gakkai Zasshi 2010, 48, 847–854. [Google Scholar] [PubMed]
- Heiming, R.; Beuschausen, T.; Liebner, T.; Seidenberg, J.; Roesler, J. Life threatening Pneumocystis carinii pneumonia in a 4-month-old boy with hyper-IgM syndrome. Monatsschr Kinderheilkd 1993, 141, 860–863. [Google Scholar] [PubMed]
- Plakke, M.; Jalota, L.; Lloyd, B. Pneumocystis pneumonia in a non-HIV patient on chronic corticosteroid therapy: A question of prophylaxis. Case Rep. 2013. [Google Scholar] [CrossRef] [PubMed]
- Aymonier, M.; Abed, S.; Boyé, T.; Barazzutti, H.; Fournier, B.; Morand, J. Dermatomyosite associée aux anticorps anti-MDA5 et pneumocystose pulmonaire: Deux cas d’évolution fatale. Ann. Dermatol. Venereol. 2017, 144, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Van Halem, K.; Vrolijk, L.; Pereira, A.M.; de Boer, M.G.J. Characteristics and Mortality of Pneumocystis Pneumonia in patients with Cushing’s syndrome: A Plea for timely initiation of chemoprophylaxis. Open Forum Infect. Dis. 2017. [Google Scholar] [CrossRef] [PubMed]
- Kaur, N.; Mahl, T. Pneumocystis jiroveci (carinii) Pneumonia After Infliximab Therapy: A Review of 84 Cases. Dig. Dis. Sci. 2007, 52, 1481–1484. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.F.; Le Noury, J.; Corbett, E.L.; Felton, J.M.; De Cock, K.M. Pneumocystis carinii infection: Current treatment and prevention. J. Antimicrob. Chemother. 1996, 37, 33–53. [Google Scholar] [CrossRef] [PubMed]
- Maschmeyer, G.; Helweg-Larsen, J.; Pagano, L.; Robin, C.; Cordonnier, C.; Schellongowski, P. 6th European Conference on Infections in Leukemia (ECIL-6), a joint venture of The European Group for Blood and Marrow Transplantation (EBMT), The European Organization for Research and Treatment of Cancer (EORTC), the International Immunocompromised Host Society (ICHS) and The European LeukemiaNet (ELN). ECIL guidelines for treatment of Pneumocystis jirovecii pneumonia in non-HIV-infected haematology patients. J. Antimicrob. Chemother. 2016, 71, 2405–2413. [Google Scholar] [PubMed]
- White, P.L.; Backx, M.; Barnes, R.A. Diagnosis and management of Pneumocystis jirovecii infection. Expert Rev. Anti. Infect. Ther 2017, 15, 435–447. [Google Scholar] [CrossRef] [PubMed]
- Iriart, X.; Bouar, M.L.; Kamar, N.; Berry, A. Pneumocystis Pneumonia in Solid-Organ Transplant Recipients. J. Fungi 2015, 1, 293–331. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Su, L.; Jiang, S.J.; Qu, H. Risk factors for mortality from Pneumocystis carinii pneumonia (PCP) in non-HIV patients: A meta-analysis. Oncotarget 2017, 8, 59729–59739. [Google Scholar] [CrossRef] [PubMed]
- Hagiya, H.; Kuroe, Y.; Nojima, H.; Sugiyama, J.; Naito, H.; Hagioka, S.; Morimoto, N.; Miyake, T.; Kokumai, Y.; Murase, T. Co-infection with invasive pulmonary aspergillosis and Pneumocystis jirovecii pneumonia after corticosteroid therapy. J. Infect. Chemother. 2013, 19, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Markantonatou, A.; Ioakimidou, A.; Arvaniti, K.; Manou, E.; Papadopoulos, V.; Kiriklidou, P.; Samaras, K.; Kioumi, A.; Vyzantiadis, T. Pulmonary co-infections by Pneumocystis jirovecii and Aspergillus fumigatus in non-HIV patients: A report of two cases and literature review. Mycoses 2017, 60, 626–633. [Google Scholar] [CrossRef] [PubMed]
- Ikawa, H.; Hayashi, Y.; Ohbayashi, C.; Tankawa, H.; Itoh, H. Autopsy case of alcoholic hepatitis and cirrhosis treated with corticosteroids and affected by Pneumocystis carinii and cytomegalovirus pneumonia. Pathol. Int 2001, 51, 629–632. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.; Lee, T.; Bae, Y.; Park, S.; Park, H.; Kim, S.; Cho, Y.; Moon, H.; Lee, S. Severe Pneumonia Caused by Combined Infection with Pneumocystis jiroveci, Parainfluenza Virus Type 3, Cytomegalovirus, and Aspergillus fumigatus in a Patient with Stevens-Johnson Syndrome/toxic Epidermal Necrolysis. Acta Derm. Venereol. 2010, 90, 625–629. [Google Scholar] [CrossRef] [PubMed]
- Dunphy, L.; Singh, N.; Keating, E. Multiple myeloma presenting with bilateral ankle pain (microangiopathy) and complicated by streptococcal meningitis and Pneumocystis carinii pneumonia. BMJ Case Rep. 2017. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.; Fe, A.; Desai, A.; Ilowite, J.; Cunha, B.; Mathew, J. A Case of Pneumonia Caused by Pneumocystis jirovecii and Cryptococcus Neoformans in a Patient with HTLV-1 Associated Adult T-Cell Leukemia/Lymphoma: Occam’s Razor Blunted. Conn. Med. 2016, 80, 81–83. [Google Scholar] [PubMed]
- Bava, A.; Romero, M.; Prieto, R.; Troncoso, A. A case report of pulmonary coinfection of Strongyloides stercoralis and Pneumocystis jiroveci. Asian Pac. J. Trop. Biomed. 2011, 1, 334–336. [Google Scholar] [CrossRef]
- Burke, J.; Soubani, A. Influenza and Pneumocystis jirovecii pneumonia in an allogeneic hematopoietic stem cell transplantation recipient: Coinfection or superinfection? Transpl. Infect. Dis. 2017, 20. [Google Scholar] [CrossRef] [PubMed]
- Musallam, N.; Bamberger, E.; Srugo, I.; Dabbah, H.; Glikman, D.; Zonis, Z.; Kessel, A.; Genizi, J. Legionella pneumophila and Pneumocystis jirovecii Coinfection in an Infant Treated with Adrenocorticotropic Hormone for Infantile Spasm. J. Child Neurol 2013, 29, 240–242. [Google Scholar] [CrossRef] [PubMed]
- Khawcharoenporn, T.; Apisarnthanarak, A.; Sakonlaya, D.; Mundy, L.; Bailey, T. Dual Infection with Mycobacterium tuberculosis and Pneumocystis jiroveci Lymphadenitis in a Patient with HIV Infection: Case Report and Review of the Literature. AIDS Patient Care STDS 2006, 20, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Alvaro-Meca, A.; Palomares-Sancho, I.; Diaz, A.; Resino, R.; De Miguel, G.; Resino, S. Pneumocystis pneumonia in HIV-positive patients in Spain: Epidemiology and environmental risk factors. J. Int. AIDS Soc. 2015, 18, 19906. [Google Scholar] [CrossRef] [PubMed]
- Sing, A.; Schmoldt, S.; Laubender, R.P.; Heesemann, J.; Sing, D.; Wildner, M. Seasonal variation of Pneumocystis jirovecii infection: Analysis of underlying climatic factors. Clin. Microbiol. Infect. 2009, 15, 957–960. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.F.; Evans, H.E.; Copas, A.J.; Huggett, J.F.; Edwards, S.G.; Walzer, P.D. Seasonal variation in mortality of Pneumocystis jirovecii pneumonia in HIV-infected patients. Int. J. STD AIDS 2010, 21, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Fei, M.W.; Kim, E.J.; Sant, C.A.; Jarlsberg, G.L.; Davis, J.L.; Swartzman, A.; Huang, L. Prediciting mortality from HIV-associated Pneumocystis pneumonia at illness presentation: An observational cohort study. Thorax 2009, 64, 1070–1076. [Google Scholar] [CrossRef] [PubMed]
- Weng, L.; Huang, X.; Chen, L.; Feng, L.Q.; Jiang, W.; Hu, X.Y.; Peng, J.M.; Wang, C.Y.; Zhan, Q.Y.; Du, B. Prognostic factors for severe Pneumocystis jiroveci pneumonia of non-HIV patients in intensive care unit: A bicentric retrospective study. BMC Infect. Dis. 2016, 16, 528. [Google Scholar] [CrossRef] [PubMed]
- Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents. Available online: http://aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf (accessed on 11 September 2018).
- Cordonnier, C.; Cesaro, S.; Maschmeyer, G.; Einsele, H.; Donnelly, J.P.; Alanio, A.; Hauser, PM.; Lagrou, K.; Melchers, W.J.; Helweg-Larsen, J.; et al. Fifth European Conference on Infections in Leukemia (ECIL-5), a joint venture of The European Group for Blood and Marrow Transplantation (EBMT), The European Organization for Research and Treatment of Cancer (EORTC), the Immunocompromised Host Society (ICHS) and The European LeukemiaNet (ELN). Pneumocystis jirovecii pneumonia: Still a concern in patients with haematological malignancies and stem cell transplant recipients. J. Antimicrob. Chemother. 2016, 71, 2379–2385. [Google Scholar]
- Alanio, A.; Hauser, P.M.; Lagrou, K.; Melchers, W.J.; Helweg-Larsen, J.; Matos, O.; Cesaro, S.; Maschmeyer, G.; Einsele, H.; Donnelly, J.P.; et al. 5th European Conference on Infections in Leukemia (ECIL-5), a joint venture of The European Group for Blood and Marrow Transplantation (EBMT), The European Organization for Research and Treatment of Cancer (EORTC), the Immunocompromised Host Society (ICHS) and The European LeukemiaNet (ELN). ECIL guidelines for the diagnosis of Pneumocystis jirovecii pneumonia in patients with haematological malignancies and stem cell transplant recipients. J. Antimicrob. Chemother. 2016, 71, 2386–2396. [Google Scholar] [PubMed]
- Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-Exposed and HIV-Infected Children. Available online: https://aidsetc.org/disclaimer (accessed on 11 October 2016).
- Maertens, J.; Cesaro, S.; Maschmeyer, G.; Einsele, H.; Donnelly, J.P.; Alanio, A.; Hauser, P.M.; Lagrou, K.; Melchers, W.J.; Helweg-Larsen, J.; et al. 5th European Conference on Infections in Leukaemia (ECIL-5), a joint venture of the European Group for Blood and Marrow Transplantation (EBMT), the European Organisation for Research and Treatment of Cancer (EORTC), the Immunocompromised Host Society (ICHS) and the European LeukemiaNet (ELN). ECIL guidelines for preventing Pneumocystis jirovecii pneumonia in patients with haematological malignancies and stem cell transplant recipients. J. Antimicrob. Chemother. 2016, 71, 2397–2404. [Google Scholar] [PubMed]
- Martin, S.I.; Fishman, J.A.; The AST Infectious Diseases Community of Practice. Pneumocystis pneumonia in Solid organ transplantation. Am. J. Translant. 2013, 13, 272–279. [Google Scholar]
- Mu, X.-D.; Jia, P.; Gao, Li.; Su, L.; Zhang, C.; Wang, R.-G.; Wang, G.-F. Relationship between radiological stages and prognoses of Pneumocystis pneumonia in Non-AIDS immunocompromised patients. J. Chin. Med. 2016, 129, 2020–2025. [Google Scholar] [CrossRef] [PubMed]
- Vogel, M.N.; Brodoefel, H.; Hierl, T.; Beck, R.; Bethge, W.A.; Claussen, C.D.; Horger, M.S. Differences and similarities of cytomegalovirus and Pneumocystis pneumonia in HIV-negative immunocompromised patients thin section CT morphology in the early phase of the disease. Br. J. Radiol. 2007, 80, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Salzer, H.J.F.; Schäfer, G.; Hoenigl, M.; Günther, G.; Hoffmann, C.; Kalsdorf, B.; Alanio, A.; Lange, C. Clinical, Diagnostic, and Treatment Disparities between HIV-Infected and Non-HIV-Infected Immunocompromised Patients with Pneumocystis jirovecii Pneumonia. Respiration 2018, 96, 52–65. [Google Scholar] [CrossRef] [PubMed]
- Vogel, M.N.; Weissgerber, P.; Goeppert, B.; Hetzel, J.; Vatlach, M.; Claussen, C.; Horger, M. Accuracy of serum LDH elevation for the diagnosis of Pneumocystis jiroveci pneumonia. Swiss Med Wkly 2011, 141, w13184. [Google Scholar] [CrossRef] [PubMed]
- Nyamande, K.; Lalloo, U.G. Serum procalcitonin distinguishes CAP due to bacteria, Mycobacterium tuberculosis and PJP. Int. J. Tuberc. Lund Dis. 2006, 10, 510–515. [Google Scholar]
- Schildgen, V.; Mai, S.; Khalfaoui, S.; Lüsebrink, J.; Pieper, M.; Tillmann, R.L.; Brockmann, M.; Schildgen, O. Pneumocystis jiroveci can be productively cultured in differentiated CuFi-8 airway cells. Mbio 2014, 5, E01186-14. [Google Scholar] [CrossRef] [PubMed]
- Cruciani, M.; Marcati, P.; Malena, M.; Bosco, O.; Serpelloni, G.; Mengoli, C. Meta-analysis of diagnostic procedures for Pneumocystis carnii pneumonia in HIV-1-infected patients. Eur. Respir. J. 2002, 20, 982–989. [Google Scholar] [CrossRef]
- Summah, H.; Zhu, Y.-G.; Falagas, M.E.; Vouloumanou, E.K.; Qu, J.-M. Use of real-time polymerase chain reaction for the diagnosis of Pneumocystis pneumonia in immuncompromised patients: A meta-analysis. J. Chin. Med. 2013, 126, 1965–1973. [Google Scholar]
- Fan, L.-C.; Lu, H.-W.; Cheng, K.-B.; Li, H.-P.; Xu, J.-F. Evaluation of PCR in bronchoalveolar lavage fluid for diagnosis of Pneumocystis jirovecii pneumonia: A bivariate meta-analysis and systematic review. PLoS ONE 2013, 8, E73099. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Ling, G.; Qiang, C.; Ming, Q.; Wu, C.; Wang, K.; Ying, Z. PCR Diagnosis of Pneumocystis pneumonia: A bivariate meta-analysis. J. Clin. Microbiol. 2011, 49, 4361–4363. [Google Scholar] [CrossRef] [PubMed]
- Sasso, M.; Chastang-Dumas, E.; Bastide, S.; Alonso, S.; Lechiche, C.; Bourgeois, N.; Lachaud, L. Performances of four real-time PCR assays for the diagnosis of Pneumocystis jirovecii Pneumonia. J. Clin. Microbiol. 2016, 54, 625–630. [Google Scholar] [CrossRef] [PubMed]
- Karageorgopoulos, D.E.; Qu, J.M.; Korbila, I.P.; Zhu, Y.G.; Vasileiou, V.A.; Falagas, M.E. Accuracy of β-d-glucan for the diagnosis of Pneumocystis jirovecii pneumonia: A meta-analysis. Clin. Microbiol. Infect. 2013, 19, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Onishi, A.; Sugiyama, D.; Kogata, Y.; Saegusa, J.; Sugimoto, T.; Kawano, S.; Morinobu, A.; Nishimura, K.; Kumagai, S. Diagnostic Accuracy of Serum 1,3-β-d-Glucan for Pneumocystis jiroveci Pneumonia, Invasive Candidiasis, and Invasive Aspergillosis: Systematic Review and Meta-Analysis. J. Clin. Microbiol. 2012, 50, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Li, W.J.; Guo, Y.L.; Liu, T.J.; Wang, K.; Kong, J.L. Diagnosis of Pneumocystis pneumonia using serum (1-3)-β-d-Glucan:a bivariate meta-analysis and systematic review. Thorac. Dis. 2015, 7, 2214–2225. [Google Scholar]
- Damiani, C.; Le Gal, S.; Da Costa, C.; Virmaux, M.; Nevez, G.; Totet, A. Combined quantification of pulmonary Pneumocystis jirovecii DNA and serum (1-3)-β-d-glucan for differential diagnosis of Pneumocystis pneumonia and Pneumocystis colonisation. J. Clin. Microbiol. 2013, 51, 3380–3388. [Google Scholar] [CrossRef] [PubMed]
- Rose, S.R.; Vallabhajosyula, S.; Velez, M.G.; Fedorko, D.P.; VanRaden, M.J.; Gea-Banacloche, J.C.; Lionakis, M.S. The utility of bronchoalveolar lavage β-d-glucan testing for the diagnosis of invasive fungal infections. J. Infect. 2014, 69, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Salerno, D.; Mushatt, D.; Myers, L.; Zhuang, Y.; de la Rua, N.; Calderon, E.J.; Welsh, D.A. Serum and BAL β-d-glucan for the diagnosis of Pneumocystis pneumonia in HIV positive patients. Respir. Med. 2014, 108, 1688–1695. [Google Scholar] [CrossRef] [PubMed]
- White, P.L.; Wingard, J.R.; Bretagne, S.; Löffler, J.; Patterson, T.F.; Slavin, M.A.; Barnes, R.A.; Pappas, P.G.; Donnelly, J. Aspergillus Polymerase Chain Reaction: Systematic Review of Evidence for Clinical Use in Comparison with Antigen Testing. Clin. Infect. Dis. 2015, 61, 1293–1303. [Google Scholar] [PubMed]
- Alvarez, B.; Arcos, J.; Fernandez-Guerrero, M.L. Pulmonary infectious diseases in patients with primary immunodeficiency and those treated with biologic immunomodulating agents. Curr. Opin. Pulm. Med. 2011, 17, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Baddley, J.W.; Winthrop, K.L.; Chen, L.; Liu, L.; Grijalva, C.G.; Delzell, E.; Beukelman, T.; Patkar, N.M.; Xie, F.; Saag, K.G.; et al. Non-viral opportunistic infections in new users of tumour necrosis factor inhibitor therapy: Results of the SAfety Assessment of Biologic ThERapy (SABER) Study. Ann Rheum. Dis. 2014, 73, 1942–1948. [Google Scholar] [CrossRef] [PubMed]
- Park, J.W.; Curtis, J.R.; Moon, J.; Song, Y.W.; Kim, S.; Lee, E.B. Prophylactic effect of trimethoprim-sulfamethoxazole for Pneumocystis pneumonia in patients with rheumatic diseases exposed to prolonged high-dose glucocorticoids. Ann. Rheum. Dis 2018, 77, 644–649. [Google Scholar] [CrossRef] [PubMed]
- Green, H.; Paul, M.; Vidal, L.; Leibovici, L. Prophylaxis of Pneumocystis pneumonia in immunocompromised non-HIV-infected patients: Systematic review and meta-analysis of randomized controlled trials. Mayo Clin. Proc. 2007, 82, 1052–1059. [Google Scholar] [CrossRef] [PubMed]
- The Opportunistic Infections Project Team of the Collaboration of Observational HIV Epidemiological Research in Europe (COHERE). Is It Safe to Discontinue Primary Pneumocystis jiroveci Pneumonia Prophylaxis in Patients with Virologically Suppressed HIV Infection and a CD4 Cell Count <200 Cells/mL? Clin. Infect. Dis. 2010, 51, 611–619. [Google Scholar]
- Fishman, J.A. Prevention of infection caused by Pneumocystis carinii in transplant recipients. Clin. Infect. Dis. 2001, 33, 1397–1405. [Google Scholar] [CrossRef] [PubMed]
- Kasiske, B.L.; Zeier, M.G.; Chapman, J.R.; Craig, J.C.; Ekberg, H.; Garvey, C.A.; Green, M.D.; Jha, V.; Josephson, M.A.; Kiberd, B.A.; et al. KDIGO clinical practice guideline for the care kidney transplant recipients: A summary. Kidney Int. 2010, 77, 299–311. [Google Scholar] [CrossRef] [PubMed]
- Goto, N.; Takahashi-Nakazato, A.; Futamura, K.; Okada, M.; Yamamoto, T.; Tsujita, M.; Hiramitsu, T.; Narumi, S.; Tsuchiya, K.; Gatanaga, H.; et al. Lifelong Prophylaxis with Trimethoprim-Sulfamethoxazole for Prevention of Outbreak of Pneumocystis jirovecii Pneumonia in Kidney Transplant Recipients. Transplant. Direct. 2017, 3, E151. [Google Scholar] [CrossRef] [PubMed]
- Faure, E.; Lionet, A.; Kipnis, E.; Noel, C.; Hazzan, M. Risk factors for Pneumocystis pneumonia after the first 6 months following renal transplantation. Transplant. Infect. Dis. 2017, 19. [Google Scholar] [CrossRef] [PubMed]
- Stern, A.; Green, H.; Paul, M.; Vidal, L.; Leibovici, L. Prophylaxis for Pneumocystis pneumonia (PCP) in non-HIV immunocompromised patients. Cochrane Database Syst. Rev. 2014, 1. [Google Scholar] [CrossRef]
- Evans, R.A.; Clifford, T.M.; Tang, S.; Au, T.; Fugit, A.M. Efficacy of once-weekly dapsone dosing for Pneumocystis jirovecii pneumonia prophylaxis post transplantation. Transpl. Infect. Dis. 2015, 17, 816–821. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.; Barton, T.D.; Goral, S.; Doyle, A.M.; Bloom, R.D.; Chojnowski, D.; Korenda, K.; Blumberg, E.A. Complications related to dapsone use for Pneumocystis jirovecii pneumonia prophylaxis in solid organ transplant recipients. Am. J. Transplant. 2005, 5, 2791–2795. [Google Scholar] [CrossRef] [PubMed]
- Walker, D.J.; Wakefield, A.E.; Dohn, M.N.; Miller, R.F.; Baughman, R.P.; Hossler, P.A.; Bartlett, M.S.; Smith, J.W.; Kazanjian, P.; Meshnick, S.R. Sequence polymorphisms in the Pneumocystis carinii cytochrome b gene and their association with atovaquone prophylaxis failure. J. Infect. Dis. 1998, 178, 1767–1775. [Google Scholar] [CrossRef] [PubMed]
- Kazanjian, P.; Armstrong, W.; Hossler, P.A.; Lee, C.H.; Huang, L.; Beard, C.B.; Carter, J.; Crane, L.; Duchin, J.; Burman, W.; et al. Pneumocystis carinii cytochrome b mutations are associated with atovaquone exposure in patients with AIDS. J. Infect. Dis. 2001, 183, 819–822. [Google Scholar] [CrossRef] [PubMed]
- Argy, N.; Le Gal, S.; Coppée, R.; Song, Z.; Vindrios, W.; Massias, L.; Kao, W.C.; Hunte, C.; Yazdanpanah, Y.; Lucet, J.C.; et al. Pneumocystis Cytochrome b Mutants Associated With Atovaquone Prophylaxis Failure as the Cause of Pneumocystis Infection Outbreak Among Heart Transplant Recipients. Clin. Infect. Dis. 2018, 67, 913–919. [Google Scholar] [CrossRef] [PubMed]
- Vasconcelles, M.J.; Bernardo, M.V.; King, C.; Weller, E.A.; Antin, J.H. Aerosolized pentamidine as Pneumocystis prophylaxis after bone marrow transplantation is inferior to other regimens and is associated with decreased survival and an increased risk of other infections. Biol. Blood Marrow Transplant. 2000, 6, 35–43. [Google Scholar] [CrossRef]
- Souza, J.P.; Boeckh, M.; Gooley, T.A.; Flowers, M.E.D.; Crawford, S.W. High rates of Pneumocystis carinii pneumonia in allogeneic blood and marrow transplant recipients receivingdapsone prophylaxis. Clin. Infect. Dis. 1999, 29, 1467–1471. [Google Scholar] [CrossRef] [PubMed]
- Colby, C.; McAfee, S.; Sackstein, R.; Finkelstein, D.; Fishman, J.; Spitzer, T. A prospective randomized trial comparing the toxicity and safety of atovaquone with SXTas Pneumocystis carinii pneumonia prophylaxis following autologous peripheral blood stem cell transplantation. Bone Marrow Transplant. 1999, 24, 897–902. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, R.M.; Peacock, J.E., Jr. Pneumocystis Pneumonia and the Rheumatologist: Which Patients are at Risk and How Can PCP Be Prevented? Curr. Rheumatol. Rep. 2017, 19, 35. [Google Scholar] [CrossRef] [PubMed]
- Katsuyama, T.; Saito, K.; Kubo, S.; Nawata, M.; Tanaka, Y. Prophylaxis for Pneumocystis pneumonia in patients with rheumatoid arthritis treated with biologics, based on risk factors found in a retrospective study. Arthritis Res. Ther. 2014, 16, R43. [Google Scholar] [CrossRef] [PubMed]
- Baulier, G.; Issa, N.; Gabriel, F.; Accoceberry, I.; Camou, F.; Duffau, P. Guidelines for prophylaxis of Pneumocystis pneumonia cannot rely solely on CD4-cell count in autoimmune and inflammatory diseases. Clin. Exp. Rheumatol. 2018, 36, 490–493. [Google Scholar] [PubMed]
- Lehman, J.S.; Gonzalez Santiago, T.M.; Wetter, D.A.; Kalaaji, A.N.; Limper, A.H. Weighing the risks and benefits of Pneumocystis pneumonia prophylaxis in iatrogenically immunosuppressed dermatology patients. Int. J. Dermatol. 2017, 56, e5–e6. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, S.J.; Sadarangani, M.; Jacobson, K. Pneumocystis jirovecii Pneumonia in pediatric inflammatory bowel disease: A Case report and literature review. Front Pediatr. 2017, 5, 161. [Google Scholar] [CrossRef] [PubMed]
- Cushion, M.T.; Collins, M.S. Susceptibility of Pneumocystis to echinocandins in suspension and biofilm cultures. Antimicrob. Agents Chemother. 2011, 55, 4513–4518. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.I.; Liang, H.; Ye, L.I.; Jiang, J.; Liang, B.; Huang, J. Adjunctive corticosteroids for the treatment of Pneumocystis jiroveci pneumonia in patients with HIV: A meta-analysis. Exp. Ther. Med. 2016, 11, 683–687. [Google Scholar] [CrossRef] [PubMed]
- Zolopa, A.; Andersen, J.; Powderly, W.; Sanchez, A.; Sanne, I.; Suckow, C.; Hogg, E.; Komarow, L. Early antiretroviral therapy reduces AIDS progression/death in individuals with acute opportunistic infections: A multicenter randomized strategy trial. PLoS ONE 2009, 4, e5575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kosaka, M.; Ushiki, A.; Ikuyama, Y.; Hirai, K.; Matsuo, A.; Hachiya, T.; Hanaoka, M. A Four-Center Retrospective Study of the Efficacy and Toxicity of Low-Dose Trimethoprim-Sulfamethoxazole for the Treatment of Pneumocystis Pneumonia in Patients without HIV Infection. Antimicrob. Agents Chemother. 2017, 61. [Google Scholar] [CrossRef] [PubMed]
- Bollee, G.; Sarfati, C.; Thiery, G.; Bergeron, A.; de Miranda, S.; Menotti, J.; de Castro, N.; Tazi, A.; Schlemmer, B.; Azoulay, E. Clinical picture of Pneumocystis jiroveci pneumonia in cancer patients. Chest 2007, 132, 1305–1310. [Google Scholar] [CrossRef] [PubMed]
- Lemiale, V.; Debrumetz, A.; Delannoy, A.; Alberti, C.; Azoulay, E. Adjunctive steroid in HIV-negative patients with severe Pneumocystis pneumonia. Respir. Res. 2013, 14, 87. [Google Scholar] [CrossRef] [PubMed]
- Injean, P.; Eells, S.J.; Wu, H.; McElroy, I.; Gregson, A.L.; McKinnell, J.A. A Systematic Review and Meta-Analysis of the Data Behind Current Recommendations for Corticosteroids in Non-HIV-Related PCP: Knowing When You Are on Shaky Foundations. Transplant. Direct. 2017, 3, E137. [Google Scholar] [CrossRef] [PubMed]
- Wieruszewski, P.M.; Barreto, J.N.; Frazee, E.; Daniels, C.E.; Tosh, P.K.; Dierkhising, R.A.; Mara, K.C.; Limper, AH. Early Corticosteroids for Pneumocystis Pneumonia in Adults Without HIV Are Not Associated with Better Outcome. Chest 2018, 154, 636–644. [Google Scholar] [CrossRef] [PubMed]
- Torres, H.A.; Chemaly, R.F.; Storey, R.; Aguilera, E.A.; Nogueras, G.M.; Safdar, A.; Rolston, K.V.; Raad, I.I.; Kontoyiannis, D.P. Influence of type of cancer and hematopoietic stem cell transplantation on clinical presentation of Pneumocystis jiroveci pneumonia in cancer patients. Eur. J. Clin. Microbiol. Infect. Dis. 2006, 25, 382–388. [Google Scholar] [CrossRef] [PubMed]
- Roger, P.M.; Vandenbos, F.; Pugliese, P.; De Salvador, F.; Durant, J.; Le Fichoux, Y.; Dellamonica, P. Persistence of Pneumocystis carinii after effective treatment of P. carinii pneumonia is not related to relapse or survival among patients infected with human immunodeficiency virus infection. Clin. Infect. Dis. 1998, 26, 509–510. [Google Scholar] [PubMed]
- Monnet, X.; Vidal-Petiot, E.; Osman, D.; Hamzaoui, O.; Durrbach, A.; Goujard, C.; Miceli, C.; Bourée, P.; Richard, C. Critical care management and outcome of severe Pneumocystis pneumonia in patients with and without HIV infection. Crit. Care 2008, 12, R28. [Google Scholar] [CrossRef] [PubMed]
- Soares, M.; Salluh, J.I.; Azoulay, E. Noninvasive ventilation in patients with malignancies and hypoxemic acute respiratory failure: A still pending question. J. Crit. Care 2010, 25, 37–38. [Google Scholar] [CrossRef] [PubMed]
- Hardy, W.D.; Feinberg, J.; Finkelstein, D.M.; Power, M.E.; He, W.; Kaczka, C.; Frame, P.T.; Holmes, M.; Waskin, H.; Fass, R.J. A controlled trial of trimethoprim-sulfamethoxazole or aerosolized pentamidine for secondary prophylaxis of Pneumocystis carinii pneumonia in patients with the acquired immunodeficiency syndrome. AIDS Clinical Trials Group Protocol 021. N. Engl. J. Med. 1992, 327, 1842–1848. [Google Scholar] [CrossRef] [PubMed]
- Schneider, M.M.; Hoepelman, A.I.; Eeftinck Schattenkerk, J.K.; Nielen, T.L.; van der Graaf, Y.; Frissen, J.P.; van der Ende, I.M.; Kolsters, A.F.; Borleffs, J.C. A controlled trial of aerosolized pentamidine or trimethoprim-sulfamethoxazole as primary prophylaxis against Pneumocystis carinii pneumonia in patients with human immunodeficiency virus infection. The Dutch AIDS Treatment Group. N. Engl. J. Med 1992, 327, 1836–1841. [Google Scholar] [CrossRef] [PubMed]
- Robin, C.; Lê, M.P.; Melica, G.; Massias, L.; Redjoul, R.; Khoudour, N.; Leclerc, M.; Beckerich, F.; Maury, S.; Hulin, A.; et al. Plasma concentrations of atovaquone given to immunocompromised patients to prevent Pneumocystis jirovecii. J. Antimicrob. Chemother. 2017, 72, 2602–2606. [Google Scholar] [CrossRef] [PubMed]
- Calderón, M.M.; Penzak, S.R.; Pau, A.K.; Kumar, P.; McManus, M.; Alfaro, R.M.; Kovacs, J.A. Efavirenz but Not Atazanavir/Ritonavir Significantly Reduces Atovaquone Concentrations in HIV-Infected Subjects. Clin. Infect. Dis. 2016, 62, 1036–1042. [Google Scholar]
- Suárez, I.; Roderus, L.; van Gumpel, E.; Jung, N.; Lehmann, C.; Fätkenheuer, G.; Hartmann, P.; Plum, G.; Rybniker, J. Low prevalence of DHFR and DHPS mutations in Pneumocystis jirovecii strains obtained from a German cohort. Infection 2017, 45, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Cho, Y.; Sung, Y.; Chung, D.; Jeong, S.; Park, J.; Lee, S. A Case of Pneumonia Caused by Pneumocystis jirovecii Resistant to Trimethoprim-Sulfamethoxazole. Korean J. Parasitol. 2015, 53, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Nahimana, A.; Rabodonirina, M.; Helweg-Larsen, J.; Meneau, I.; Francioli, P.; Bille, J.; Hauser, P. Sulfa Resistance and Dihydropteroate Synthase Mutants in Recurrent Pneumocystis carinii Pneumonia. Emerg. Infect. Dis. 2003, 9, 864–867. [Google Scholar] [CrossRef] [PubMed]
- Helweg-Larsen, J.; Benfield, T.; Eugen-Olsen, J.; Lundgren, J.; Lundgren, B. Effects of mutations in Pneumocystis carinii dihydropteroate synthase gene on outcome of AIDS-associated P. carinii pneumonia. Lancet 1999, 354, 1347–1351. [Google Scholar] [CrossRef]
- Ponce, C.A.; Chabé, M.; George, C.; Cárdenas, A.; Durán, L.; Guerrero, J.; Bustamante, R.; Matos, O.; Huang, L.; Miller, R.F.; et al. High Prevalence of Pneumocystis jirovecii Dihydropteroate Synthase Gene Mutations in Patients with a First Episode of Pneumocystis Pneumonia in Santiago, Chile, and Clinical Response to Trimethoprim-Sulfamethoxazole Therapy. Antimicrob. Agents Chemother. 2017, 61. [Google Scholar] [CrossRef] [PubMed]
- Ahn, A.; Chang, J.; Sung, H.; Kim, M. A Case of Pneumonia Caused by Pneumocystis jirovecii Resistant to SXT in the Absence of Previous Drug Exposure. Lab. Med. Online 2016, 6, 250. [Google Scholar] [CrossRef]
- Long, Y.; Zhang, C.; Su, L.; Que, C. Pneumocystis jirovecii dihydropteroate synthase gene mutations in a group of HIV-negative immunocompromised patients with Pneumocystis pneumonia. Exp.Ther. Med. 2014, 8, 1825–1830. [Google Scholar] [CrossRef] [PubMed]
- Hauser, P.M.; Nahimana, A.; Taffe, P.; Weber, R.; Francioli, P.; Bille, J.; Rabodonirina, M. Interhuman transmission as a potential key parameter for geographical variation in the prevalence of Pneumocystis jirovecii dihydropteroate synthase mutations. Clin. Infect. Dis. 2010, 51, e28–e33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, L.; Beard, C.B.; Creasman, J.; Levy, D.; Duchin, J.S.; Lee, S.; Pieniazek, N.; Carter, J.L.; del Rio, C.; Rimland, D.; Navin, T.R. Sulfa or sulfone prophylaxis and geographic region predict mutations in the Pneumocystis carinii dihydropteroate synthase gene. J. Infect. Dis. 2000, 182, 1192–1198. [Google Scholar] [CrossRef] [PubMed]
- Montesinos, I.; Delforge, M.L.; Ajjaham, F.; Brancart, F.; Hites, M.; Jacobs, F.; Denis, O. Evaluation of a new commercial real-time PCR assay for diagnosis of Pneumocystis jirovecii pneumonia and identification of dihydropteroate synthase (DHPS) mutations. Diagn. Microbiol. Infect. Dis. 2017, 87, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Yiannakis, E.P.; Boswell, T.C. Systematic review of outbreaks of Pneumocystis jirovecii pneumonia: Evidence that P. jirovecii is a transmissible organism and the implications for healthcare infection control. J. Hosp. Infect. 2016, 93, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.F.; Ambrose, H.E.; Wakefield, A.E. Pneumocystis carinii f. sp. hominis DNA in immunocompetent health care workers in contact with patients with P. carinii pneumonia. J. Clin. Microbiol. 2001, 39, 3877–3882. [Google Scholar] [CrossRef] [PubMed]
- Choukri, F.; Menotti, J.; Sarfati, C.; Lucet, J.C.; Nevez, G.; Garin, Y.J.; Derouin, F.; Totet, A. Quantification and spread of Pneumocystis jirovecii in the surrounding air of patients with Pneumocystis pneumonia. Clin. Infect. Dis. 2010, 51, 259–265. [Google Scholar] [CrossRef] [PubMed]
- De Boer, M.G.; Bruijnesteijn van Coppenraet, L.E.; Gaasbeek, A.; Berger, S.P.; Gelinck, L.B.; van Houwelingen, H.C.; van den Broek, P.; Kuijper, E.J.; Kroon, F.P.; Vandenbroucke, J.P. An outbreak of Pneumocystis jiroveci pneumonia with 1 predominant genotype among renal transplant recipients: Interhuman transmission or a common environmental source? Clin. Infect. Dis. 2007, 44, 1143–1149. [Google Scholar] [CrossRef] [PubMed]
- Chapman, J.R.; Marriott, D.J.; Chen, S.C.; MacDonald, P.S. Post-transplant Pneumocystis jirovecii pneumonia—A re-emerged public health problem? Kidney Int. 2013, 84, 240–243. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, M.S.; Vermund, S.H.; Jacobs, R.; Durant, P.J.; Shaw, M.M.; Smith, J.W.; Tang, X.; Lu, J.J.; Li, B.; Jin, S.; et al. Detection of Pneumocystis carinii DNA in air samples: Likely environmental risk to susceptible persons. J. Clin. Microbiol. 1997, 35, 2511–2513. [Google Scholar] [PubMed]
- Olsson, M.; Lidman, C.; Latouche, S.; Björkman, A.; Roux, P.; Linder, E.; Wahlgren, M. Identification of Pneumocystis carinii f. sp. hominis gene sequences in filtered air in hospital environments. J. Clin. Microbiol. 1998, 36, 1737–1740. [Google Scholar] [PubMed]
- Mori, S.; Sugimoto, M. Pneumocystis jirovecii infection: An emerging threat to patients with rheumatoid arthritis. Rheumatology 2012, 51, 2120–2130. [Google Scholar] [CrossRef] [PubMed]
- Yazaki, H.; Goto, N.; Uchida, K.; Kobayashi, T.; Gatanaga, H.; Oka, S. Outbreak of Pneumocystis jiroveci pneumonia in renal transplant recipients: P. jiroveci is contagious to the susceptible host. Transplantation 2009, 88, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Helweg-Larsen, J.; Tang, X.; Jin, S.; Li, B.; Bartlett, M.S.; Lu, J.J.; Lundgren, B.; Lundgren, J.D.; Olsson, M.; et al. Update on Pneumocystis carinii f. sp. hominis typing based on nucleotide sequence variations in internal transcribed spacer regions of rRNA genes. J. Clin. Microbiol. 1998, 36, 734–741. [Google Scholar] [PubMed]
- Lu, J.J.; Lee, C.H. Pneumocystis pneumonia. J. Formos. Med. Assoc. 2008, 107, 830–842. [Google Scholar] [CrossRef]
- Alanio, A.; Gits-Muselli, M.; Mercier-Delarue, S.; Dromer, F.; Bretagne, S. Diversity of Pneumocystis jirovecii during Infection Revealed by Ultra-Deep Pyrosequencing. Front. Microbiol. 2016, 7, 733. [Google Scholar] [CrossRef] [PubMed]
- Gits-Muselli, M.; Peraldi, M.N.; de Castro, N.; Delcey, V.; Menotti, J.; Guigue, N.; Hamane, S.; Raffoux, E.; Bergeron, A.; Valade, S.; et al. New Short Tandem Repeat-Based Molecular Typing Method for Pneumocystis jirovecii Reveals Intrahospital Transmission between Patients from Different Wards. PLoS ONE 2015, 10, e0125763. [Google Scholar] [CrossRef] [PubMed]
- Mortier, E.; Pouchot, J.; Bossi, P.; Molinié, V. Maternal-fetal transmission of Pneumocystis carinii in human immunodeficiency virus infection. N. Engl. J. Med. 1995, 332, 825. [Google Scholar] [CrossRef] [PubMed]
- Schneider, M.M.; Borleffs, J.C.; Stolk, R.P.; Jaspers, C.A.; Hoepelman, A.I. Discontinuation of prophylaxis for Pneumocystis carinii pneumonia in HIV-1-infected patients treated with highly active antiretroviral therapy. Lancet 1999, 353, 201–203. [Google Scholar] [CrossRef]
- Ling, C.; Qian, S.; Wang, Q.; Zeng, J.; Jia, X.; Liu, J.; Li, Z. Pneumocystis pneumonia in non-HIV children: A 10-year retrospective study. J. Clin. Respir. 2018, 12, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Chen, Z.; Huang da, W.; Kutty, G.; Ishihara, M.; Wang, H.; Abouelleil, A.; Bishop, L.; Davey, E.; Deng, R.; et al. Genome analysis of three Pneumocystis species reveals adaptation mechanisms to life exclusively in mammalian hosts. Nat. Commun. 2016, 22, 10740. [Google Scholar] [CrossRef] [PubMed]
| Underlying Disease | Number of Cases/ Medical History | Treatment | Outcome | Reference |
|---|---|---|---|---|
| Severe alcoholic hepatitis | 2 | Not available | Both died | [10] |
| Giant cell arteritis | 7 F = 5 M = 2 | All on prednisone at diagnosis of PcP No PcP prophylaxis All received trimethoprim/sulfamethoxazole for PcP | 5 recovered 2 died | [8] |
| Crohn’s disease. | 1 M, 19 y Post-marketing surveillance through June 2001, ntified 10 cases of PcP during infliximab treatment, 3 of which died | For Crohn’s disease— Azathioprine and infliximab For PcP— Steroids and trimethoprim-sulfamethoxazole | Follow up 2 weeks later confirmed clinical response to therapy. | [11] |
| Pustular psoriasis with an IL-36RN deficiency. | 1 M, 54 y PCP developed after infliximab | For pustular psoriasis— Cyclosporin which was unresponsive then Infliximab For PcP IV trimethoprim/ sulfamethoxazole | Mutation found in the IL36RN gene compatible with IL-36RN deficiency anakinra started and psoriasis improved | [12] |
| Diabetes mellitus with pneumoconiosis and interstitial pneumonia | 1 M, 75 y Carcinoma of the buccal mucosa | Corticosteroids for interstitial pneumonia Trimethoprim/sulfamethoxazole and voriconazole for PcP and Aspergillus fumigatus | Died | [13] |
| Systemic lupus erythematosus. | 5 cases Study of 858 hospitalized lupus patients. ID from lung biopsy in 2 and BAL in 3 | Prednisolone and concomitant biologics or immunosuppressants | 3 died | [9] |
| Hyper-IgM syndrome | 1 M, 4 months | IgM syndrome diagnosis made after PcP was detected. trimethoprim/sulfamethoxazole for PcP | Recovered | [14] |
| Membranoproliferative glomerulonephritis | 1 M, 50 y | Corticosteroids for underlying condition For PcP Trimethoprim/sulfamethoxazole | Recovered | [15] |
| Dermatomyositis associated with anti-MDA-5 autoanti bodies | 2 M, 56 y Initially had interstitial lung disease without infection M, 52 y | Both treated with corticosteroids for underlying condition. Both had specific treatment for PcP M, 52 y also received cyclophosphamide bolus | Both died | [16] |
| Cushing’s Syndrome | 15 13 developed PcP after initiation of cortisol blocking therapy. | Cushing’s syndrome—Cortisol blocking therapy PcP therapy—Not stated | 11 of the 15 patients died | [17] |
| Pneumocystis jiroveci pneumonia after infliximab therapy: a review of 84 cases. | 84 Cases | 23 of the 84 patients died | [18] |
| Clinical factor | Disease Classification | ||
|---|---|---|---|
| Mild | Moderate | Severe | |
| Dysnoea | On exertion | On minimal exertion/possibly at rest | At rest |
| Resting arterial tension | PaO2 of > 11.0 kPa | PaO2 8.1–11.0 kPa | PaO2 < 8.0 kPa |
| Oxygen saturation | SaO2 > 96% | SaO2 of 91–96% | SaO2 < 91% |
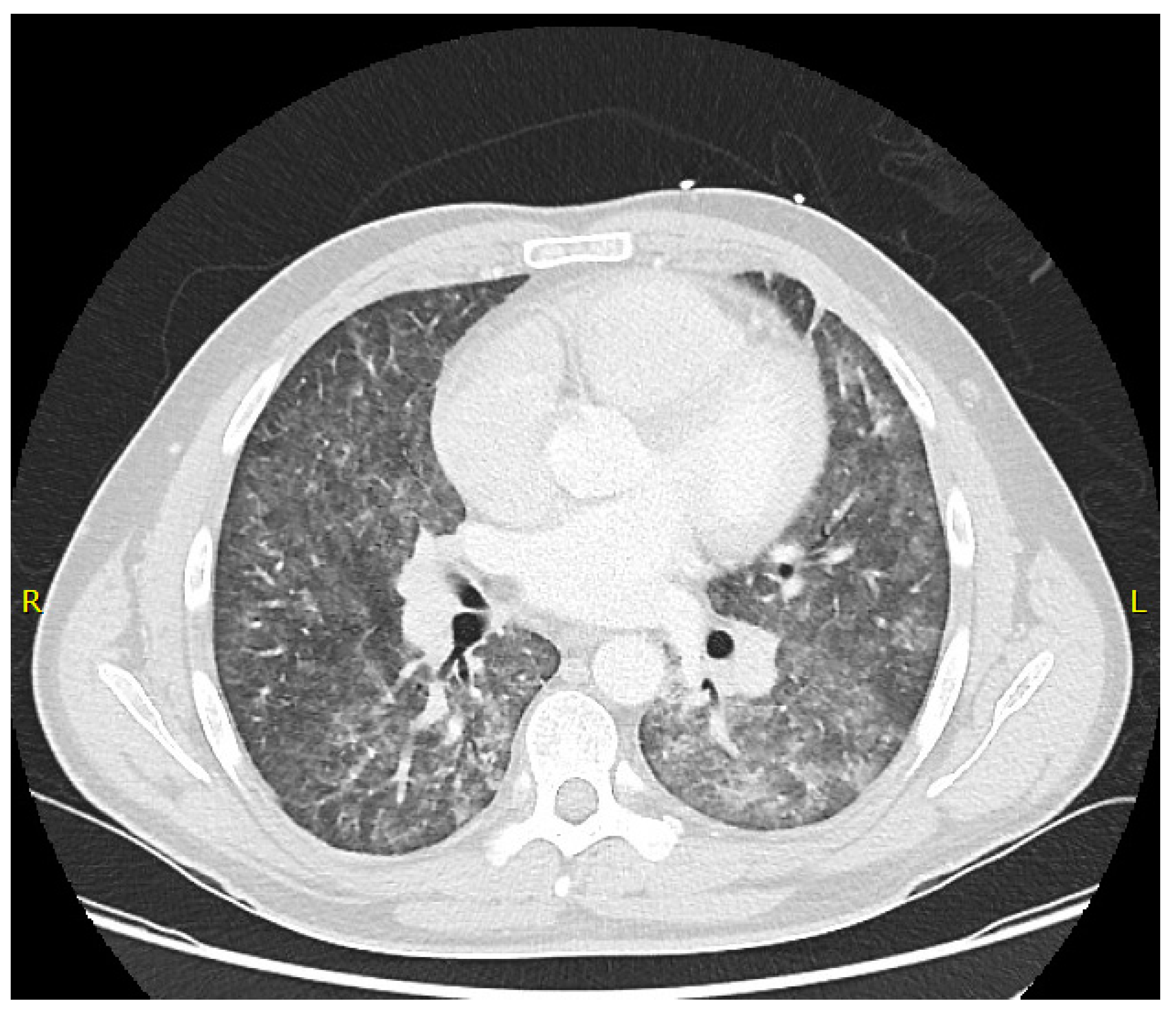
| Radiology | Normal/Minimal changes on CXR | Diffuse interstitial changes on CXR | Extensive interstitial changes with potential diffuse alveolar shadowing on CXR |
| Other | Possibly Fever | Tachypnoea at rest, fever, cough | |
| Underlying Disease | Coinfection | Number of Cases/Medical History | Treatment | Outcome | Reference |
|---|---|---|---|---|---|
| COPD and chronic hepatitis C | PcP and Aspergillosis | 1 M, 95 y, treated for lung injury caused by Chlamydophila pnemonia | Ceftriaxone and Methylprednisolone Then alternating prednisolone and methylprednisolone Then meropenem and azithromycin. Then sulfamethoxazole/ trimethoprim for PcP Then levofloxacin, minocycline, liposomal amphotericin B along with PcP treatment | Died of multiple organ failure | [24] |
| Crescentic IgA nephropathy and Non-Hodgkin lymphoma | PcP and Aspergillosis | 2 M, 29 y with crescentic IgA nephropathy on immunosuppressive drugs F, 72 y with non-Hodgkin lymphoma on chemotherapy | Both— Intravenous trimethroprim/sulphamethoxazole combined with voriconazole Prophylaxis M—Moxifloxacin and Ganciclovir F—Moxifloxacin and Valaciclovir | M—Recovered F—Died | [25] |
| Alcoholic hepatitis and cirrhosis | PcP and cytomegalovirus | 1 M, 40 y | Initially broad spectrum antibiotics then prednisolone. Amphotericin B syrup dissolved in water gargled for oral and esophageal candidiasis No treatment for PCP, found during autopsy | Died of circulatory insufficiency | [26] |
| Allopurinol-induced Stevens-Johnson syndrome and toxic epidermal necrolysis | PcP, parainfluenza virus type 3, CMV and Aspergillus fumigatus. | 1 F, 63 y Presented with mucocutaneous macular skin rash with bulla. 3 months prior had an acute myocardial infarction. 1-month prior essential thrombocytosis 30 years previous had, surgery for intestinal TB and was a hepatitis C carrier. | High-dose systemic corticosteroids and intravenous immunoglobulin for Stevens-Johnson syndrome / toxic epidermal necrolysis 100 mg/day aspirin 1 mg/day anagrelide 200 mg/day allopurinol Anti-TB treatment 30 years ago. For co-infections Trimethroprim/sulphamethoxazole, voriconazole, ganciclovir and oral ribavirin. | Recovered | [27] |
| Probable plasma cell myeloma | Streptococcal meningitis and PcP | 1 F, 64 y | Intravenous acyclovir, ceftriaxone and fluconazole for the meningitis Trimethroprim-sulfamethoxazole for PcP | Unclear | [28] |
| HTLV-1 Associated Adult T-cell leukemia/lymphoma | PcP and Cryptococcus neoformans | 1 | Trimethroprim-sulfamethoxazole, corticosteroids and fluconazole | Recovered | [29] |
| HIV | PcP and Strongyloides stercoralis | 1 M, 43 y | Trimethroprim-sulfamethoxazole, ivermectin and amphotericin B | Died | [30] |
| Allogeneic hematopoietic stem cell transplantation recipient | PcP and Influenza A | 1 M, 53 y Immunosuppresive therapy for treatment of GVHD | For underlying condition - daily mycophenolate mofetil, tacrolimus and prophylactic Trimethroprim-sulfamethoxazole. Treated with high-dose corticosteroids for GVHD PCP prophylaxis switched to inhaled pentamidine due to pancytopenia attributed to Trimethroprim-sulfamethoxazole. PcP treated with Trimethroprim-sulfamethoxazole. | Recovered | [31] |
| Infantile spasm | Legionella pneumophila and PcP | 1 8 month old infant | Not Stated | Died | [32] |
| HIV | Mycobacterium tuberculosis and PcP | 1 | Trimethroprim-sulfamethoxazole prophylaxis for PcP Antituberculosis medication and Trimethroprim-sulfamethoxazole | Recovered | [33] |
| Strategy | Population [Ref] | ||
|---|---|---|---|
| HIV-Positive [39] | Haematology [20,43] | Solid Organ Transplantation [44] | |
| Prophylaxis | Front line: Trimethoprim/sulfamethoxazole one single-strength (80 mg TMP/400 mg SMX) daily or one double strength tablet (160 mg TMP/800 mg SMX)/daily. Second line: Trimethoprim/sulfamethoxazole one double strength tablet (160 mg TMP/800 mg SMX) three times per week Dapsone (50 mg twice daily) Dapsone (200 mg) + pyrimethamine (75 mg) + leucovorin (25 mg) weekly Dapsone (50 mg daily) + pyrimethamine (50 mg weekly) + leucovorin (25 mg weekly) Pentamidine aerosols (300 mg per month) Atovaquone 1500 mg daily | Front line: Trimethoprim/sulfamethoxazole one single-strength (80 mg TMP/400 mg SMX)/day or double strength tablet (160 mg TMP/800 mg SMX)/day or three per week. Second line: Dapsone (50 mg twice daily) Pentamidine aerosols (300 mg per month) Atovaquone (1500 mg daily) | Front line: Trimethoprim/sulfamethoxazole one single-strength (80 mg TMP/400 mg SMX)/day or double strength tablet (160 mg TMP/800 mg SMX)/day or three per week. Second line: Dapsone (50–100 mg once a day) Atovaquone (>1000 mg daily) Third Line: Pentamidine aerosols (300 mg every 3–4 weeks) |
| Treatment | Frontline: Trimethoprim/sulfamethoxazole (15–20 mg/kg TMP; 75–100 mg/kg SMX per day) For moderate to severe disease (i.e., hypoxemia) adjunctive corticosteroids should be used Second line for severe disease: Primaquine and clindamycin (30 mg/(600 mg × 3)) per day Pentamidine IV (4 mg/kg/day) Second line for mild/moderate disease: Dapsone (100 mg daily) + trimethoprim (15 mg daily) Atovaquone (750 mg BID) | Frontline: Trimethoprim/sulfamethoxazole (15–20 mg/kg TMP; 75–100 mg/kg SMX per day) Second line: Primaquine and clindamycin (30 mg/(600 mg × 3)) per day Pentamidine IV (4 mg/kg/day) Atovaquone (750 mg/ 2–3 per day) | Frontline: Trimethoprim/sulfamethoxazole (15–20 mg/kg TMP; 75–100 mg/kg SMX per day) with TMP administered by IV every 6–8 h. For hypoxemic patients potentially in combination with 40–60 mg of prednisolone (twice daily) Second line: IV Pentamidine (Initially 4 mg/kg/day over 1–2 h) Recipients of pancreas/islet transplants should receive an alternative second line therapy. |
| Underlying Disease | Number of Cases/ Medical History | Mechanism of Resistance | Alternative Treatment | Outcome | Reference |
|---|---|---|---|---|---|
| HIV | 1 M, 50 y | Mutations at codons 55 and 57 of the, associated with resistance to Trimethoprim/sulfamethoxazole. | Clindamycin-primaquine | Recovered | [103] |
| HIV | 13 M = 11 F = 2 Each patient had 2 episodes | 3 patients had no PCP prophylaxis for both episodes only one had PcP mutations. 4 patients had no DHPS genotype mutations in their Positive PcP samples 9 patients had at least one of the mutations described below in their PcP samples M1, mutant 1 (Ala55 Pro57); M2, mutant 2 (Thr55 Ser57); M3, mutant 3 (Ala55 Ser57 double mutant). | Of the 11 patients who recovered, 9 received prophylaxis and all needed alternative therapy. | 1 with no prophylaxis died on Trimethoprim/sulfamethoxazole treatment, PcP mutations present. 1 with prophylaxis on 2nd presentation died after alternative therapy of Trimethoprim/sulfamethoxazole then pentamidine only had wild type PcP. 11 recovered. | [104] |
| HIV | 152 | 31 of the 152 had Pnuemocystis carinii DHPS mutations These mutations were more common in patients who had previous exposure to sulpha drugs | Not available | Survival of patients with mutations was significantly lowered | [105] |
| HIV and Non-HIV Immuno-suppressed | 56 46 HIV 10 Non-HIV Immuno-suppressed | Mutations in the DHPS gene | Not available | All HIV patients recovered 5 of the 10 Non-HIV patients died | [106] |
| HIV | 1 M, 50 y No previous exposure to Trimethoprim/sulfamethoxazole | DHPS gene mutations at codon 55 and 57 (Thr55Ala and Pro57Ser) | Clindamycin-primaquine | Recovered | [107] |
| Non-HIV Immunocompromised Patients | 18 | Substitution mutations: At DHPS codon 98—glutamate replaced by lysine. At DHPS codon 90—aspartate replaced by asparagine. | All patients received immunosuppressive agents but none of them received PcP prophylaxis For PcP— Trimethoprim/sulfamethoxazole Trimethoprim/sulfamethoxazole + Caspofungin Primaquine + clindamycin | Approximately 65% mortality | [108] |
| HIV | 8 | Cytochrome b substitutions in the Qo region: T121I, L123F, T100I, I120V, S125A, P239L and L248F | 5 patients received Atovaquone prophylaxis, but 3 were Atovaquone naïve | 84% overall survival: 87% of patients with mutations survived | [76] |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
White, P.L.; Price, J.S.; Backx, M. Therapy and Management of Pneumocystis jirovecii Infection. J. Fungi 2018, 4, 127. https://doi.org/10.3390/jof4040127
White PL, Price JS, Backx M. Therapy and Management of Pneumocystis jirovecii Infection. Journal of Fungi. 2018; 4(4):127. https://doi.org/10.3390/jof4040127
Chicago/Turabian StyleWhite, P. Lewis, Jessica S. Price, and Matthijs Backx. 2018. "Therapy and Management of Pneumocystis jirovecii Infection" Journal of Fungi 4, no. 4: 127. https://doi.org/10.3390/jof4040127
APA StyleWhite, P. L., Price, J. S., & Backx, M. (2018). Therapy and Management of Pneumocystis jirovecii Infection. Journal of Fungi, 4(4), 127. https://doi.org/10.3390/jof4040127





