Twenty-Year Course of Antifungal Resistance in Candida albicans in Türkiye: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
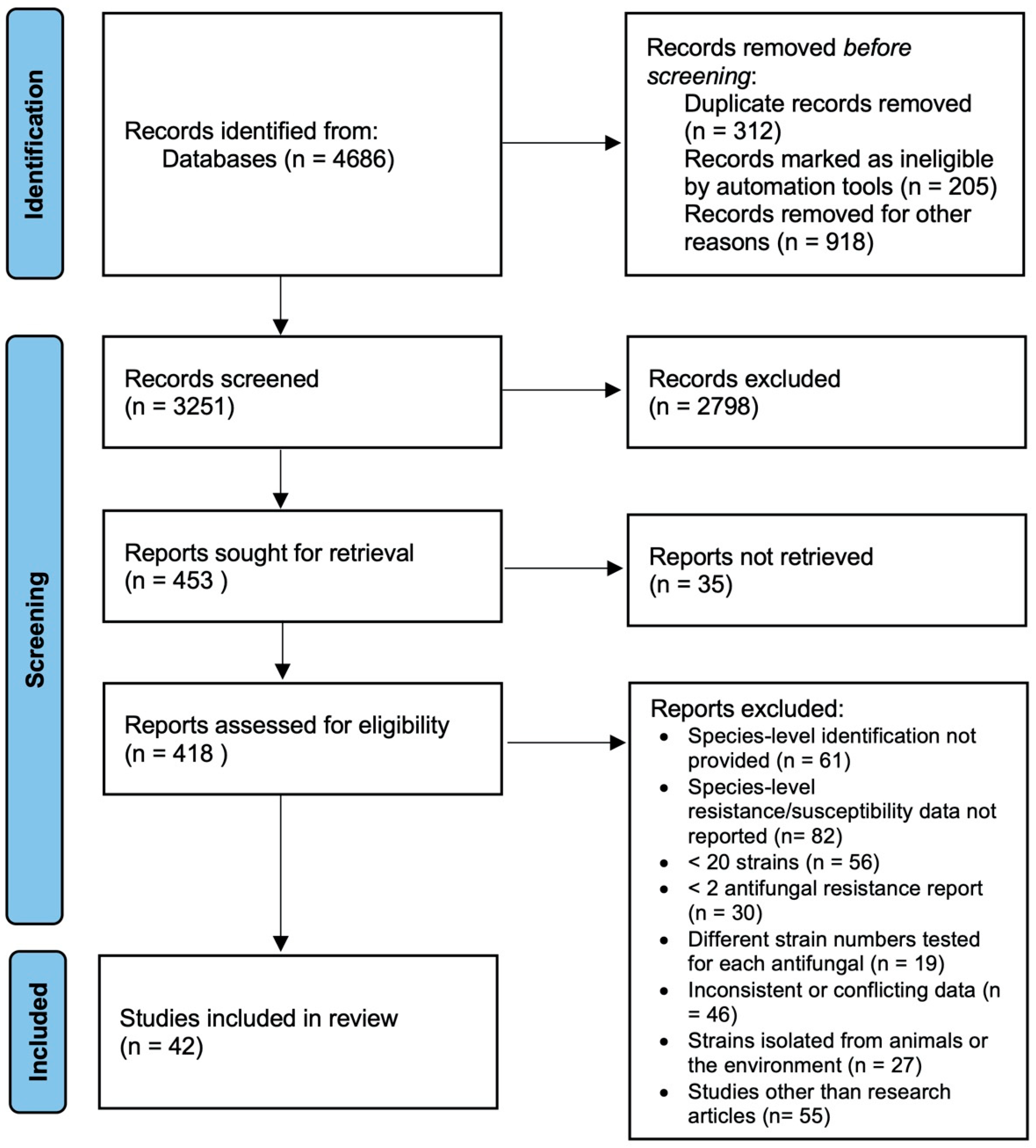
2. Material and Methods
2.1. Protocol
2.2. Literature Search
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Quality Control of Data
2.6. Data Analysis
3. Results
3.1. Characteristics of the Studies
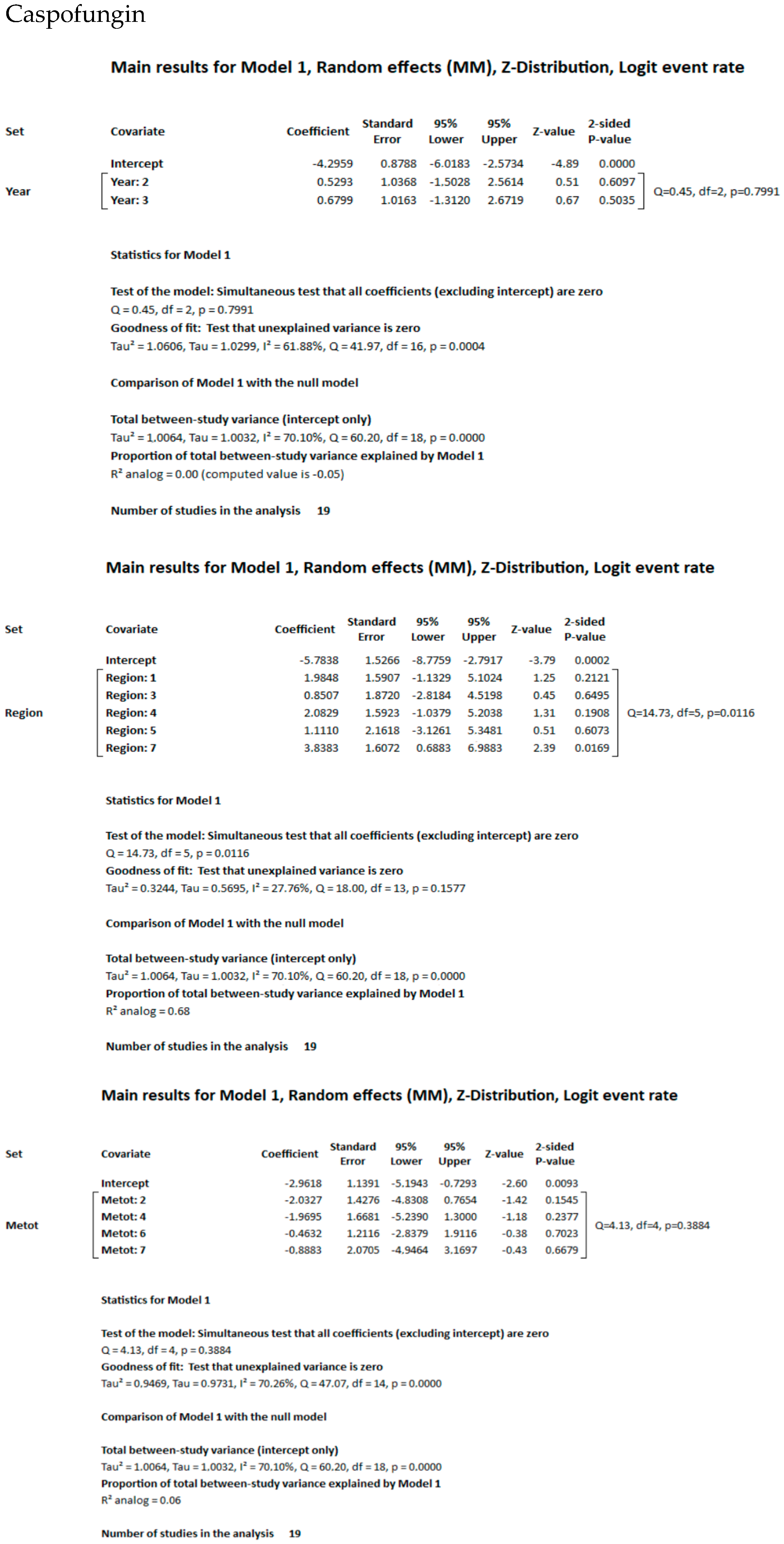
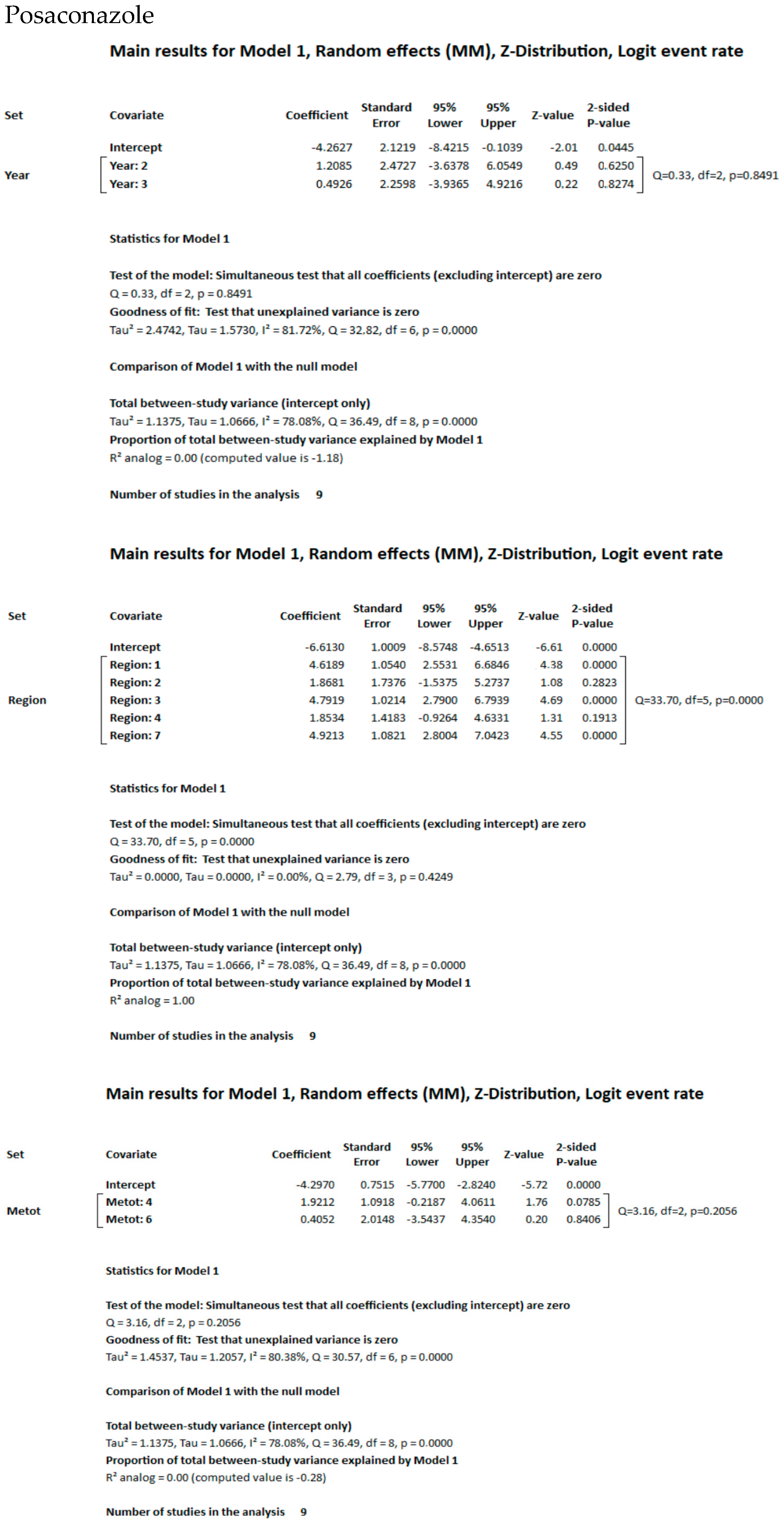
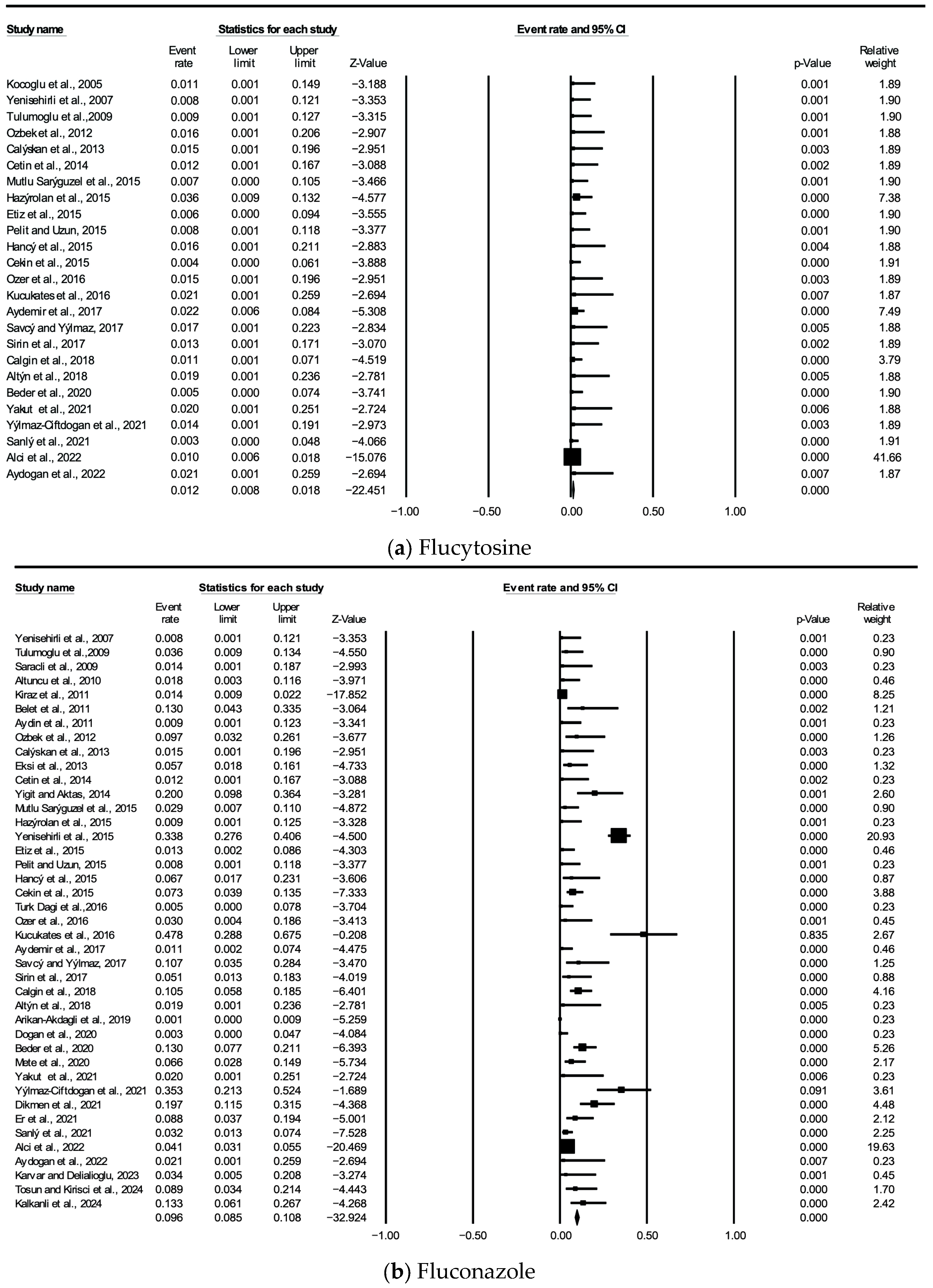
3.2. Meta-Analysis and Meta-Regression Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A


References
- Nobile, C.J.; Johnson, A.D. Candida albicans biofilms and human disease. Annu. Rev. Microbiol. 2015, 69, 71–92. [Google Scholar] [CrossRef]
- Nishimoto, A.T.; Sharma, C.; Rogers, P.D. Molecular and genetic basis of azole antifungal resistance in the opportunistic pathogenic fungus Candida albicans. J. Antimicrob. Chemother. 2020, 75, 257–270. [Google Scholar] [CrossRef]
- Daneshnia, F.; de Almeida Júnior, J.N.; Ilkit, M.; Lombardi, L.; Perry, A.M.; Gao, M.; Nobile, C.J.; Egger, M.; Perlin, D.S.; Zhai, B.; et al. Worldwide emergence of fluconazole-resistant Candida parapsilosis: Current framework and future research roadmap. Lancet Microbe 2023, 4, e470–e480. [Google Scholar] [CrossRef]
- Vaezi, A.; Fakhim, H.; Khodavaisy, S.; Alizadeh, A.; Nazeri, M. Epidemiological and mycological characteristics of candidemia in Iran: A systematic review and meta-analysis. J. Mycol. Med. 2017, 27, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Badran, E.F.; Al Baramki, J.H.; Al Shamyleh, A.; Shehabi, A.; Khuri-Bulos, N. Epidemiology and clinical outcome of candidaemia among Jordanian newborns over a 10-year period. Scand. J. Infect. Dis. 2008, 40, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Kermani, F.; Taghizadeh-Armaki, M.; Hosseini, S.A.; Amirrajab, N.; Javidnia, J.; Fami Zaghrami, M.; Shokohi, T. Antifungal resistance of clinical Candida albicans isolates in Iran: A systematic review and meta-analysis. Iran. J. Public Health 2023, 52, 290–305. [Google Scholar] [CrossRef] [PubMed]
- Brown, G.D.; Denning, D.W.; Gow, N.A.; Levitz, S.M.; Netea, M.G.; White, T.C. Hidden killers: Human fungal infections. Sci. Transl. Med. 2012, 4, 165rv13. [Google Scholar] [CrossRef]
- Denning, D.W. Global incidence and mortality of severe fungal disease. Lancet Infect. Dis. 2024, 24, e428–e438. [Google Scholar] [CrossRef]
- Kilbaş, İ.; Çiftçi, İ.H. A comprehensive meta-analysis of antifungal resistance in Candida albicans in Turkey. Int. J. Clin. Med. Res. 2017, 4, 44–50. [Google Scholar]
- Pfaller, M.A.; Diekema, D.J.; Turnidge, J.D.; Castanheira, M.; Jones, R.N. Twenty years of the SENTRY antifungal surveillance program: Results for Candida species from 1997–2016. Open Forum Infect. Dis. 2019, 6 (Suppl. 1), S79–S94. [Google Scholar] [CrossRef]
- Peron, I.H.; Reichert-Lima, F.; Busso-Lopes, A.F.; Nagasako, C.K.; Lyra, L.; Moretti, M.L.; Schreiber, A.Z. Resistance surveillance in Candida albicans: A five-year antifungal susceptibility evaluation in a Brazilian university hospital. PLoS ONE 2016, 11, e0158126. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Moola, S.; Lisy, K.; Riitano, D.; Tufanaru, C. Systematic reviews of prevalence and incidence. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, SA, Australia, 2020; Chapter 5; pp. 117–217. [Google Scholar]
- Koçoğlu, E.; Bayram, A.; Balcı, İ. Klinik örneklerden izole edilen kandida türleri ve antifungal duyarlılıkları. Van. Tıp Derg. 2005, 12, 195–200. [Google Scholar]
- Yenisehirli, G.; Bulut, N.; Yenisehirli, A.; Bulut, Y. In vitro susceptibilities of Candida albicans isolates to antifungal agents in Tokat, Turkey. Jundishapur J. Microbiol. 2015, 8, e28057. [Google Scholar] [CrossRef]
- Yenisehirli, G.; Bulut, Y.; Gunday, E. Yoğun bakım ünitesinde yatan hastaların kan kültürlerinden izole edilen Candida albicans suşlarında antifungallere duyarlılık. ANKEM Derg. 2007, 21, 146–149. [Google Scholar]
- Tulumoğlu, Ş.; Kariptaş, E.; Erdem, B. Identification and antifungal susceptibility of Candida isolates from various clinical specimens in Doctor Behçet Uz Hospital. Anatol. J. Clin. Investig. 2009, 3, 170–173. [Google Scholar]
- Saracli, M.A.; Gumral, R.; Gul, H.C.; Gonlum, A.; Yildiran, S.T. Species distribution and in vitro susceptibility of Candida bloodstream isolates to six new and current antifungal agents in a Turkish tertiary care military hospital, recovered through 2001 and 2006. Mil. Med. 2009, 174, 860–865. [Google Scholar] [CrossRef]
- Altuncu, E.; Bilgen, H.; Cerikçioğlu, N.; Ilki, A.; Ulger, N.; Bakır, M.; Akman, I.; Ozek, E. Neonatal Candida infections and the antifungal susceptibilities of the related Candida species. Mikrobiyol. Bul. 2010, 44, 593–603. [Google Scholar]
- Kiraz, N.; Oz, Y. Species distribution and in vitro antifungal susceptibility of clinical Candida isolates from a university hospital in Turkey over a 5-year period. Med. Mycol. 2011, 49, 126–131. [Google Scholar] [CrossRef]
- Belet, N.; Çiftçi, E.; Aysev, D.; Güriz, H.; Uysal, Z.; Taçyıldız, N.; Atasay, B.; Doğu, F.; Kendirli, T.; Kuloğlu, Z.; et al. Invasive Candida infections in children: The clinical characteristics and species distribution and antifungal susceptibility of Candida spp. Turk. J. Pediatr. 2011, 53, 489–498. [Google Scholar]
- Aydin, F.; Bayramoglu, G.; Guler, N.C.; Kaklikkaya, N.; Tosun, I. Bloodstream yeast infections in a university hospital in Northeast Turkey: A 4-year survey. Med. Mycol. 2011, 49, 316–319. [Google Scholar] [CrossRef]
- Özbek, E.; Tekay, F.; Çolak Pirinççioğlu, H. Antifungal resistance of Candida isolates obtained from various specimens of intensive care unit patients. Dicle Med. J. 2012, 39, 207–212. [Google Scholar] [CrossRef]
- Çalışkan, E.; Dede, A.; Biten Güven, G. Distribution and antifungal susceptibilities of Candida species detected in blood cultures. ANKEM Derg. 2013, 27, 25–30. [Google Scholar] [CrossRef]
- Eksi, F.; Gayyurhan, E.D.; Balci, I. In Vitro Susceptibility of Candida Species to Four Antifungal Agents Assessed by the Reference Broth Microdilution Method. Sci. J. 2013, 2013, 236903. [Google Scholar] [CrossRef] [PubMed]
- Çetin, F.; Mumcuoğlu, İ.; Aksoy, A.; Gürkan, Y.; Aksu, N. Kan kültürlerinden izole edilen mikroorganizmalar ve antimikrobiyal duyarlılıkları. Turk. Hij. Den. Biyol. Derg. 2014, 71, 67–74. [Google Scholar]
- Yiğit, N.; Aktaş, E. Activities of amphotericin B, fluconazole and voriconazole against Candida bloodstream isolates determined by broth microdilution and disk diffusion methods. Turk. Hij. Den. Biyol. Derg. 2014, 71, 131–140. [Google Scholar] [CrossRef]
- Mutlu Sarıgüzel, F.; Koç, A.N.; Karagöz, S. Distribution and antifungal susceptibilities with VITEK 2 system of yeast isolated from blood cultures. Harran Üniversitesi Tıp Fakültesi Derg. 2015, 12, 261–268. [Google Scholar]
- Hazırolan, G.; Yıldıran, D.; Baran, I.; Mumcuoğlu, İ.; Aksu, N. Yatan hasta örneklerinden izole edilen Candida izolatlarının tür dağılımlarının ve antifungal duyarlılık profillerinin değerlendirilmesi. Turk. Hij. Den. Biyol. Derg. 2015, 72, 17–26. [Google Scholar] [CrossRef]
- Etiz, P.; Kibar, F.; Ekenoğlu, Y.; Yaman, A. Kan kültürlerinden izole edilen Candida türlerinin dağılımının ve antifungal duyarlılıklarının retrospektif olarak değerlendirilmesi. ANKEM Derg. 2015, 29, 105–113. [Google Scholar]
- Pelit, S.; Uzun, M. Yoğun bakım ünitelerinde yatan hastalara ait çeşitli klinik örneklerden izole edilen Candida suşlarında tür dağılımının ve antifungal duyarlılıkların araştırılması. Yoğun Bakım Derg. 2016, 7, 49–52. [Google Scholar] [CrossRef]
- Hancı, S.Y.; Derici, Y.K.; Şirin, M.C.; Şamlıoğlu, P.; Bayram, A.; Ağuş, N.; Yılmaz, N. Üçüncü basamak bir hastanede, geriatrik olgularda izole edilen Candida türlerinin tiplendirilmesi ve kanda üreyen mayalarda antifungal duyarlılık. Dicle Tıp Derg. 2015, 42, 438–444. [Google Scholar]
- Çekin, Y.; Pekintürk, N.; Cekin, A.H. Evaluation of species distribution and antifungal resistance of Candida isolates from hospitalized patients. J. Clin. Anal. Med. 2015, 6, 8–11. [Google Scholar] [CrossRef]
- Türk Dagi, H.T.; Findik, D.; Senkeles, C.; Arslan, U. Identification and antifungal susceptibility of Candida species isolated from bloodstream infections in Konya, Turkey. Ann. Clin. Microbiol. Antimicrob. 2016, 15, 36. [Google Scholar] [CrossRef] [PubMed]
- Özer, T.; Durmaz, S.; Yula, E. Antifungal susceptibilities of Candida species isolated from urine culture. J. Infect. Chemother. 2016, 22, 629–632. [Google Scholar] [CrossRef]
- Kucukates, E.; Gultekin, N.N.; Alisan, Z.; Hondur, N.; Ozturk, R. Identification of Candida species and susceptibility testing with Sensititre YeastOne microdilution panel to 9 antifungal agents. Saudi Med. J. 2016, 37, 750–757. [Google Scholar] [CrossRef]
- Aydemir, Ö.; Demiray, T.; Köroğlu, M.; Aydemir, Y.; Altındiş, M. Emergence of non-albicans Candida species: Evaluation of Candida species and antifungal susceptibilities according to years. Biomed. Res. 2017, 28, 1–6. [Google Scholar]
- Savcı, Ü.; Yılmaz, N. Çeşitli örneklerden izole edilen Candidaların tür dağılımı ve antifungal direnç oranları. Turk. J. Clin. Lab. 2017, 8, 85–90. [Google Scholar] [CrossRef][Green Version]
- Şirin, M.C.; Ağuş, N.; Yılmaz, N.; Bayram, A.; Yılmaz-Hancı, S.; Şamlıoğlu, P.; Karaca-Derici, Y.; Doğan, G. Yoğun bakım ünitelerinde yatan hastaların kan kültürlerinden izole edilen mikroorganizmalar ve antibiyotik duyarlılıkları. Turk. Hij. Den. Biyol. Derg. 2017, 74, 269–278. [Google Scholar] [CrossRef]
- Calgin, M.K.; Cetinkol, Y. Distribution and antifungal susceptibility patterns of Candida species at a university hospital in Northern Turkey. J. Infect. Dev. Ctries. 2018, 12, 97–101. [Google Scholar] [CrossRef]
- Altın, N.; Cesur, S.; Yapar Toros, G.; Koldaş, K.; Solgun, G.; Şencan, İ. Yoğun bakım ünitesinde yatan hastaların klinik örneklerinden izole edilen Candida türlerinin dağılımı ve antifungal duyarlılıkları. Ortadoğu Tıp Derg. 2018, 10, 130–134. [Google Scholar]
- Arikan-Akdagli, S.; Gülmez, D.; Doğan, Ö.; Çerikçioğlu, N.; Doluca Dereli, M.; Birinci, A.; Yıldıran, Ş.T.; Ener, B.; Öz, Y.; Metin, D.Y.; et al. First multicentre report of in vitro resistance rates in Candidaemia isolates in Turkey. J. Glob. Antimicrob. Resist. 2019, 18, 230–234. [Google Scholar] [CrossRef]
- Doğan, Ö.; Yeşilkaya, A.; Menekşe, Ş.; Güler, Ö.; Karakoç, Ç.; Çınar, G.; Kapmaz, M.; Aydın, M.; Keske, Ş.; Şahin, S.; et al. Effect of initial antifungal therapy on mortality among patients with bloodstream infections with different Candida species and resistance to antifungal agents: A multicentre observational study by the Turkish Fungal Infections Study Group. Int. J. Antimicrob. Agents 2020, 56, 105992. [Google Scholar] [CrossRef]
- Beder, D.; Esenkaya Taşbent, F.; Doğan, M. Kan kültürlerinde tespit edilen Candida izolatlarının dağılımı ve antifungal duyarlılıkları. ANKEM Derg. 2020, 34, 77–85. [Google Scholar]
- Mete, B.; Zerdali, E.Y.; Aygun, G.; Saltoglu, N.; Balkan, I.I.; Karaali, R.; Kaya, S.Y.; Karaismailoğlu, B.; Kaya, A.; Urkmez, S.; et al. Change in species distribution and antifungal susceptibility of candidemias in an intensive care unit of a university hospital (10-year experience). Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 325–333. [Google Scholar] [CrossRef]
- Yakut, N.; Kepenekli, E.; Ergenc, Z.; Baran, E.; Cerikcioglu, N. Antifungal susceptibility, species distribution and risk factors associated with mortality of invasive candidiasis in children in Turkey: A six-year retrospective, single-centre study. J. Mycol. Med. 2021, 31, 101082. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz-Ciftdoğan, D.; Kara-Aksay, A.; Erbaş, G.; Sarkış, Ü.B.; Karadağ-Oncel, E.; Anıl, A.B.; Baran, M.; Er, H.; Yılmaz, N. Epidemiology of candidemia in children over 7 years in a medical center in Turkey. Microbiol. Spectr. 2021, 9, e0045321. [Google Scholar] [CrossRef] [PubMed]
- Dikmen, N.; Duran, N.; Ay, E.; Cimen, F.; Tek, E. Genotyping, drug resistance and virulence factors of Candida species isolated from patients using long-term inhaled steroids. Int. J. Clin. Pract. 2021, 75, e14820. [Google Scholar] [CrossRef] [PubMed]
- Er, H.; Özkalay Yılmaz, N.; Karaca Derici, Y.; Hancı, S.; Saba Çopur, Ş. Kandidemi etkenlerinin tür dağılımı ve duyarlılıkları: Hastanemizde ampirik antifungal tedavi politikası değiştirilmeli mi? Turk. Mikrobiyol. Cemiy. Derg. 2021, 51, 150–155. [Google Scholar] [CrossRef]
- Şanlı, K.; Mart Kömürcü, S.Z.; Şahin, A.S. Kan kültürlerinde üretilen yoğun bakım ünitesi hastalarında Candida epidemiyolojisi ve antifungal direnç değişiminin incelenmesi, 2015–2019. Dicle Med. J. 2021, 48, 796–805. [Google Scholar] [CrossRef]
- Alçi, G.; Keçeli, S.A.; Sarıtaş, B.M. Distribution of Candida species isolated from different clinical specimens and their antifungal susceptibility profile: A 5 year retrospective analysis. KOU Sağlık Bil. Derg. 2022, 8, 92–98. [Google Scholar] [CrossRef]
- Aydoğan, S.; Samadzade, R.; Maçin, S.; Türk Dağı, H.; Fındık, D. Pandemi döneminde kan kültürlerinden izole edilen Candida türlerinin dağılımı ve antifungal duyarlılıklarının değerlendirilmesi. Mantar Derg. 2022, 13, 105–110. [Google Scholar]
- Karvar, Ş.; Delialioğlu, N. Kan kültüründen izole edilen Candida türlerinin dağılımı ve antifungal duyarlılığının araştırılması. FLORA 2023, 28, 331–340. [Google Scholar] [CrossRef]
- Tosun, M.İ.; Kirişci, Ö. Kan kültürlerinde tespit edilen Candida izolatlarının dağılımı ve antifungal duyarlılıklarının ticari bir sıvı mikrodilüsyon testi ile belirlenmesi. ANKEM Derg. 2024, 38, 53–61. [Google Scholar] [CrossRef]
- Kalkanlı, N.; Atmaca, S.; Özcan, N. Antifungal susceptibilities of Candida species isolated to clinical samples. Hamidiye Med. J. 2024, 5, 148–156. [Google Scholar] [CrossRef]
- Süzük, S.; Kaşkatepe, B.; Avcıküçük, H.; Aksaray, S.; Başustaoğlu, A. CLSI’dan EUCAST’e Geçişte Üriner Sistem Enfeksiyonu Etkeni Escherichia coli İzolatlarının Antibiyotik Duyarlılıklarının Karşılaştırılması. Mikrobiyol. Bul. 2015, 49, 494–501. [Google Scholar] [CrossRef]
- EUCAST. Breakpoint Tables for Interpretation of MICs for Antifungal Agents, Version 9.0, 2019. European Committee on Antimicrobial Susceptibility Testing. Available online: https://www.eucast.org/newsiandr (accessed on 13 June 2025).
- Cohen, L.; Lawrence, M.; Keith, M. Research Methods in Education, 6th ed.; Routledge: London, UK, 2007. [Google Scholar]
- Lee, Y.; Puumala, E.; Robbins, N.; Cowen, L.E. Antifungal drug resistance: Molecular mechanisms in Candida albicans and beyond. Chem. Rev. 2021, 121, 3390–3411. [Google Scholar] [CrossRef]
- Brown, G.D.; Denning, D.W.; Levitz, S.M. Tackling human fungal infections. Science 2012, 336, 647. [Google Scholar] [CrossRef]
- Pappas, P.G.; Kauffman, C.A.; Andes, D.R.; Clancy, C.J.; Marr, K.A.; Ostrosky-Zeichner, L.; Reboli, A.C.; Schuster, M.G.; Vazquez, J.A.; Walsh, T.J.; et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 62, e1–e50. [Google Scholar] [CrossRef]
- World Health Organization. WHO Fungal Priority Pathogens List to Guide Research, Development and Public Health Action; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Kessler, S.Q.S.; Lang, P.M.; Dal-Pizzol, T.S.; Montagner, F. Resistance profiles to antifungal agents in Candida albicans isolated from human oral cavities: Systematic review and meta-analysis. Clin. Oral. Investig. 2022, 26, 6479–6489. [Google Scholar] [CrossRef]
- Arendrup, M.C.; Arikan-Akdagli, S.; Jørgensen, K.M.; Barac, A.; Steinmann, J.; Toscano, C.; Arsenijevic, V.A.; Sartor, A.; Lass-Flörl, C.; Hamprecht, A.; et al. European Candidaemia is characterised by notable differential epidemiology and susceptibility pattern: Results from the ECMM Candida III study. J. Infect. 2023, 87, 428–437. [Google Scholar] [CrossRef]
- Verma, R.; Pradhan, D.; Hasan, Z.; Singh, H.; Jain, A.K.; Khan, L.A. A systematic review on distribution and antifungal resistance pattern of Candida species in the Indian population. Med. Mycol. 2021, 59, 1145–1165. [Google Scholar] [CrossRef]
- Mushi, M.F.; Bader, O.; Taverne-Ghadwal, L.; Bii, C.; Groß, U.; Mshana, S.E. Oral candidiasis among African human immunodeficiency virus-infected individuals: Ten years of systematic review and meta-analysis from sub-Saharan Africa. J. Oral. Microbiol. 2017, 9, 1317579. [Google Scholar] [CrossRef]
- Castanheira, M.; Deshpande, L.M.; Davis, A.P.; Rhomberg, P.R.; Pfaller, M.A. Monitoring antifungal resistance in a global collection of invasive yeasts and molds: Application of CLSI epidemiological cutoff values and whole-genome sequencing analysis for detection of azole resistance in Candida albicans. Antimicrob. Agents Chemother. 2017, 61, e00906–e00917. [Google Scholar] [CrossRef] [PubMed]
- Bustamante, B.; Martins, M.A.; Bonfietti, L.X.; Szeszs, M.W.; Jacobs, J.; Garcia, C.; Melhem, M.S.C. Species distribution and antifungal susceptibility profile of Candida isolates from bloodstream infections in Lima, Peru. J. Med. Microbiol. 2014, 63, 855–860. [Google Scholar] [CrossRef] [PubMed]
- Doi, A.M.; Pignatari, A.C.; Edmond, M.B.; Marra, A.R.; Camargo, L.F.; Siqueira, R.A.; da Mota, V.P.; Colombo, A.L. Epidemiology and microbiologic characterization of nosocomial candidemia from a Brazilian national surveillance program. PLoS ONE 2016, 11, e0146909. [Google Scholar] [CrossRef] [PubMed]
- Cuenca-Estrella, M.; Gomez-Lopez, A.; Cuesta, I.; Zaragoza, O.; Mellado, E.; Rodriguez-Tudela, J.L.; Antifungal Subcommittee of European Committee on Antimicrobial Susceptibility Testing. Frequency of voriconazole resistance in vitro among Spanish clinical isolates of Candida spp. according to breakpoints established by the Antifungal Subcommittee of the European Committee on Antimicrobial Susceptibility Testing. Antimicrob. Agents Chemother. 2011, 55, 1794–1797. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Diekema, D.J.; Gibbs, D.L.; Newell, V.A.; Nagy, E.; Dobiasova, S.; Rinaldi, M.; Barton, R.; Veselov, A.; Global Antifungal Surveillance Group. Candida krusei, a multidrug-resistant opportunistic fungal pathogen: Geographic and temporal trends from the ARTEMIS DISK Antifungal Surveillance Program, 2001 to 2005. J. Clin. Microbiol. 2008, 46, 515–521. [Google Scholar] [CrossRef]
- Jabeen, G.; Naz, S.A.; Rangel, D.E.N.; Jabeen, N.; Shafique, M.; Yasmeen, K. In vitro evaluation of virulence markers and antifungal resistance of clinical Candida albicans strains isolated from Karachi, Pakistan. Fungal Biol. 2023, 127, 1241–1249. [Google Scholar] [CrossRef]
- Kooshki, P.; Rezaei-Matehkolaei, A.; Mahmoudabadi, A.Z. The patterns of colonization and antifungal susceptibility of Candida isolated from preterm neonates in Khorramabad, South West of Iran. J. Mycol. Med. 2018, 28, 340–344. [Google Scholar] [CrossRef]
- Zarrinfar, H.; Kord, Z.; Fata, A. High incidence of azole resistance among Candida albicans and C. glabrata isolates in Northeastern Iran. Curr. Med. Mycol. 2021, 7, 18–21. [Google Scholar] [CrossRef]
- Carrillo-Muñoz, A.J.; Tur-Tur, C.; Hernández-Molina, J.M.; Quindós, G.; Marcos-Arias, C.; Eraso, E.; Cárdenes, D.; Ortiz-Maestro, O.; Santos, P.; Estivill, D.; et al. Antifungal activity of posaconazole against Candida spp. and non-Candida clinical yeasts isolates. Rev. Esp. Quimioter. 2010, 23, 122–125. [Google Scholar]
- Delma, F.Z.; Al-Hatmi, A.M.S.; Brüggemann, R.J.M.; Melchers, W.J.G.; de Hoog, S.; Verweij, P.E.; Buil, J.B. Molecular mechanisms of 5-fluorocytosine resistance in yeasts and filamentous fungi. J. Fungi 2021, 7, 909. [Google Scholar] [CrossRef]
- Barchiesi, F.; Arzeni, D.; Caselli, F.; Scalise, G. Primary resistance to flucytosine among clinical isolates of Candida spp. J. Antimicrob. Chemother. 2000, 45, 408–409. [Google Scholar] [CrossRef]
| Studies | Data Year | Geographical Region | Clinical Sample | Identification | Antifungal Susceptibility Detection Method | Antifungal Susceptibility Testing Guide |
|---|---|---|---|---|---|---|
| Kocoglu et al., 2005 [14] | 2004 | Marmara | Blood, urine, wound swab, sputum, stool, fasting gastric juice, drain fluid | API ID 32C | ATB Fungus | Unidentified |
| Yenisehirli et al., 2007 [16] | 2003–2007 | Black Sea | Blood | GTT, CCF-T80, API 20C AUX | BM, E-test | CLSI |
| Tulumoglu et al., 2009 [17] | 2006–2008 | Central Anatolia | Blood, urine, wound swab, catheter | API ID 20C AUX | API ATB Fungal 3 kit | Unidentified |
| Saracli et al., 2009 [18] | 2001–2006 | Central Anatolia | Blood | API ID 32C | BM | CLSI |
| Altuncu et al., 2010 [19] | - | Marmara | Blood, urine, CSF, PF, ETA, pleural fluid | API ID32C | BM | CLSI |
| Kiraz et al., 2011 [20] | 2003–2008 | Central Anatolia | Blood, urine, sputum, catheter, wound swab, stool, skin swab | CC, API 20C AUX | E-Test | CLSI |
| Belet et al., 2011 [21] | 2004–2008 | Black Sea | Blood, CSF, PF, pericardial fluid | API 20CAUX | E-Test | CLSI |
| Aydin et al., 2011 [22] | 2005–2009 | Black Sea | Blood | CHROMagar, API ID 32C | Disk diffusion, E-Test | CLSI |
| Ozbek et al., 2012 [23] | 2009–2010 | Southeastern Anatolia | Blood, urine, PF, sputum | VITEK® 2 | VITEK® 2 | Unidentified |
| Calıskan et al., 2013 [24] | 2009–2012 | Central Anatolia | Blood | VITEK® 2 | VITEK® 2 | Unidentified |
| Eksi et al., 2013 [25] | 2008–2009 | Southeastern Anatolia | Blood | API ID 32C | BM | CLSI |
| Cetin et al., 2014 [26] | 2012–2013 | Central Anatolia | Blood | VITEK® 2 | VITEK® 2 | CLSI |
| Yigit and Aktas, 2014 [27] | 2011–2013 | Eastern Anatolia | Blood | API 20 C AUX | BM | CLSI |
| Mutlu Sariguzel et al., 2015 [28] | 2012–2014 | Central Anatolia | Blood | VITEK® 2 | VITEK® 2 | CLSI |
| Hazirolan et al., 2015 [29] | 2013–2014 | Central Anatolia | Blood, urine, TA, wound swab, sputum, PF, catheter, abscess | VITEK® 2 | VITEK® 2 | CLSI |
| Yenisehirli et al., 2015 [15] | 2007–2012 | Black Sea | VCE | API 20C AUX | E-Test | CLSI |
| Etiz et al., 2015 [30] | 2013–2014 | Mediterranean | Blood | VITEK® 2 | VITEK® 2 | CLSI |
| Pelit and Uzun, 2015 [31] | 2014–2015 | Marmara | Urine, blood, TA, abscess | VITEK® 2 | VITEK® 2 | Unidentified |
| Hanci et al., 2015 [32] | 2011–2014 | Aegean | Blood, urine | API ID32C | API ATB Fungus 3 | CLSI and EUCAST |
| Cekin et al., 2015 [33] | 2010–2011 | Mediterranean | Blood, urine, sputum, abscess, catheter, CSF | VITEK® 2 | VITEK® 2 | Unidentified |
| Turk Dagi et al.,2016 [34] | 2010–2013 | Central Anatolia | VCE | GTT, CCF-T80, API ID 32C | BM | CLSI |
| Ozer et al., 2016 [35] | 2012–2013 | Mediterranean | Urine | VITEK® 2 | VITEK® 2 | CLSI |
| Kucukates et al., 2016 [36] | 2013–2014 | Marmara | Blood, urine, sputum, wound swab, ETA | CC, API ID 32C | CMP | Unidentified |
| Aydemir et al., 2017 [37] | 2011–2015 | Marmara | Blood, urine, TA, wound swab, CSF, catheter | VITEK® 2 | VITEK® 2 | CLSI |
| Savci and Yilmaz, 2017 [38] | 2014–2016 | Central Anatolia | Urine, VS, BAL, sputum, wound swab | VITEK® 2 | VITEK® 2 | CLSI |
| Sirin et al., 2017 [39] | 2012–2015 | Aegean | Blood | API ID 32C ve API ATB Fungus 3 | API ATB Fungus 3 | CLSI |
| Calgin et al., 2018 [40] | 2015–2017 | Black Sea | Blood, urine, sputum, wound swab | VITEK® 2 | VITEK® 2 | Unidentified |
| Altin et al., 2018 [41] | 2011–2012 | Central Anatolia | Urine, blood, BAL, wound swab | VITEK® 2 | VITEK® 2 | Unidentified |
| Arikan-Akdagli et al., 2019 [42] | 1997–2017 | - | Blood | GTT, API ID 32C, API 20C AUX | BM | CLSI |
| Dogan et al., 2020 [43] | 2015–2018 | - | Blood | MALDI-TOF/MS | BM | CLSI |
| Beder et al., 2020 [44] | 2014–2018 | Central Anatolia | VCE | VITEK® 2 | VITEK® 2 | CLSI |
| Mete et al., 2020 [45] | 2004–2008, 2013–2017 | Marmara | VCE | API ID32 | E-Test | EUCAST |
| Yakut et al., 2021 [46] | 2013–2019 | Marmara | VCE | API ID32 C, MALDI TOF MS | CMP | CLSI |
| Yilmaz-Ciftdogan et al., 2021 [47] | 2012–2018 | Aegean | Blood | API ID 32C | E-Test | CLSI |
| Dikmen et al., 2021 [48] | - | Mediterranean | Mouth swab | PCR | NA | CLSI and EUCAST |
| Er et al., 2021 [49] | 2017–2019 | Aegean | Blood | API ID 32C, MALDI-TOF MS | E-Test | EUCAST |
| Sanli et al., 2021 [50] | 2015–2019 | Marmara | VCE | PHOENİX M50 (BD USA | VITEK® 2 | CLSI |
| Alci et al., 2022 [51] | 2017–2021 | Marmara | Blood, urine, wound swab, catheter, VS, BAL and VCE | MALDI-TOF MS, VITEK 2 | VITEK® 2 | EUCAST |
| Aydogan et al., 2022 [52] | 2020–2022 | Central Anatolia | Blood | VITEK 2 | VITEK® 2 | EUCAST |
| Karvar and Delialioglu, 2023 [53] | 2020 | Mediterranean | Blood | VITEK 2 | BM | EUCAST |
| Tosun and Kirisci et al., 2024 [54] | 2022–2024 | Mediterranean | Blood | BD Phoenix M50 | BM | EUCAST |
| Kalkanli et al., 2024 [55] | 2019–2020 | Southeast Anatolia | Blood, urine, wound swab, VS, catheter, and VCE | MALDI-TOF MS | E-Test | EUCAST |
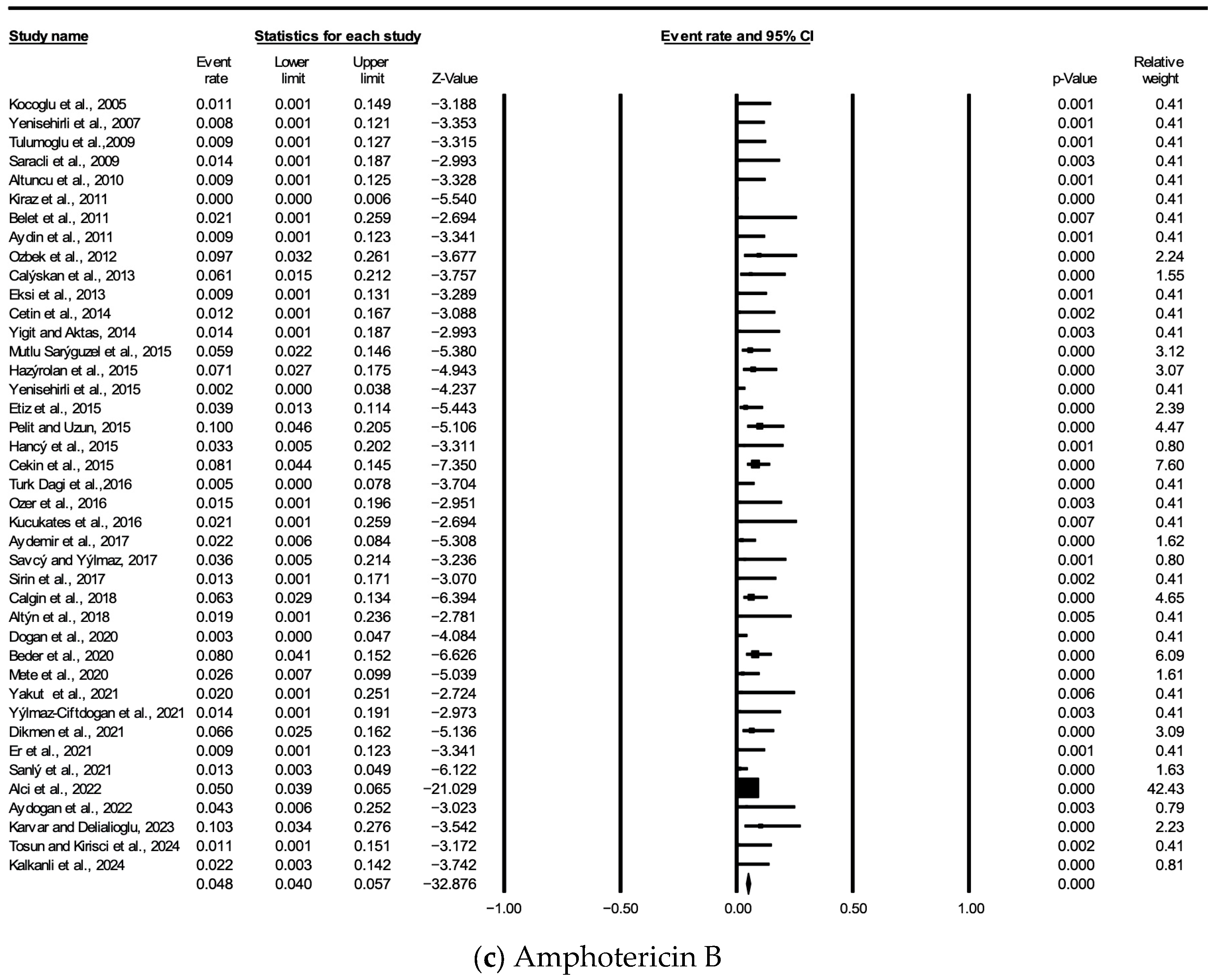
| Antifungal Agent | Number of Studies Reporting | Sample Size | Number of Resistant Isolates | Resistance Rate (%) | 95% CI |
|---|---|---|---|---|---|
| Amp B | 41 | 4718 | 117 | 2.10% | 2.04–2.92% |
| 5-FC | 25 | 2423 | 16 | 0.29% | 0.34–0.98% |
| FLC | 41 | 5523 | 248 | 4.45% | 3.94–5.04% |
| VRC | 38 | 4144 | 181 | 4.37% | 3.75–4.99% |
| ITZ | 16 | 2894 | 128 | 4.42% | 3.67–5.17% |
| CAS | 19 | 2382 | 70 | 2.94% | 2.26–3.62% |
| MFG | 12 | 2509 | 49 | 1.95% | 1.41–2.49% |
| POS | 9 | 1546 | 45 | 2.91% | 2.07–3.75% |
| ANF | 8 | 571 | 6 | 1.05% | 0.21–1.89% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kilbas, I.; Kahraman Kilbas, E.P.; Horhat, F.G.; Ciftci, I.H. Twenty-Year Course of Antifungal Resistance in Candida albicans in Türkiye: A Systematic Review and Meta-Analysis. J. Fungi 2025, 11, 603. https://doi.org/10.3390/jof11080603
Kilbas I, Kahraman Kilbas EP, Horhat FG, Ciftci IH. Twenty-Year Course of Antifungal Resistance in Candida albicans in Türkiye: A Systematic Review and Meta-Analysis. Journal of Fungi. 2025; 11(8):603. https://doi.org/10.3390/jof11080603
Chicago/Turabian StyleKilbas, Imdat, Elmas Pinar Kahraman Kilbas, Florin George Horhat, and Ihsan Hakki Ciftci. 2025. "Twenty-Year Course of Antifungal Resistance in Candida albicans in Türkiye: A Systematic Review and Meta-Analysis" Journal of Fungi 11, no. 8: 603. https://doi.org/10.3390/jof11080603
APA StyleKilbas, I., Kahraman Kilbas, E. P., Horhat, F. G., & Ciftci, I. H. (2025). Twenty-Year Course of Antifungal Resistance in Candida albicans in Türkiye: A Systematic Review and Meta-Analysis. Journal of Fungi, 11(8), 603. https://doi.org/10.3390/jof11080603







