Abstract
We report a case of spondylodiscitis caused by Aspergillus nidulans (SCAN). A. nidulans is a saprophytic fungus and emerging pathogen responsible for a variety of infections, although it is rarely implicated in osteoarticular infections. The patient was a 59-year-old immunocompromised patient with a history of lymphoma and splenectomy. Following diagnosis, the patient was promptly and effectively treated with voriconazole. A literature review underlines the distinctive features of the few case reports of SCAN, as well as the original features of the present case report.
1. Introduction
Aspergillus nidulans is a filamentous saprophytic fungus in the phylum Ascomycota. In immunocompromised patients, it can lead to sinusitis and pulmonary infections. A. nidulans can be distinguished from other Aspergillus species by its dark green colonies, which appear brown on the reverse side, its short, brown conidiophores, and its biseriate heads [1].
Osteoarticular infections caused by the Aspergillus spp. are rare and mainly affect immunocompromised patients [2,3]. The most commonly reported species in this context is A. fumigatus (55%), followed by A. flavus (12%) and then A. nidulans (7%) [3]. We describe a case of spondylodiscitis caused by A. nidulans (SCAN) in an immunocompromised patient with a history of lymphoma and splenectomy.
2. Case Report
On 26 September 2018, a 59-year-old man was seen in consultation in our Infectious Disease Department for the follow-up of a left pneumococcal empyema and endocarditis caused by Streptococcus pneumoniae in June 2018, for which the patient was treated with amoxicillin for 6 weeks. His medical history included hypothyroidism, viral pericarditis in 1998, bacteremia due to Streptococcus gallolyticus in 2016, ulcerative esophagitis, and non-Hodgkin lymphoma (NHL). During the consultation, he reported suffering from lower back pain for 2 weeks. The lumbar pain was associated with paresthesia of the lower left limb. Magnetic Resonance Imaging (MRI) was performed a week later and showed edema associated with erosion of the L1–L2 vertebral endplates (Figure 1), suggestive of an intravertebral disc herniation or infectious spondylodiscitis. Secondary MRI was performed 10 days later and showed persistence of the previous images.
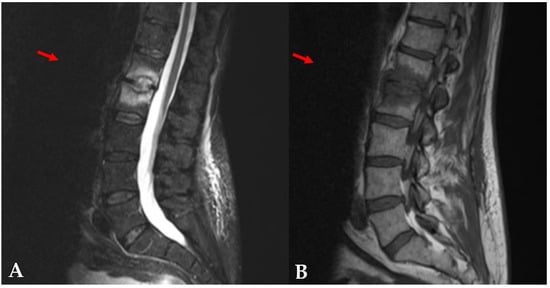
Figure 1.
Magnetic Resonance Imaging of the patient. The sagittal STIR image (A) showed bright high-signal intensity of L1–L2 disc, which was well enhanced on the sagittal T1-weighted image (B).
The patient was hospitalized in the Infectious Disease Department on October 25 to perform disc biopsies, respecting the 2-month therapeutic window following his antibiotic treatment. His laboratory results included a blood leukocyte count of 8.9 × 109/L, with 74% neutrophils, and a C-reactive protein level of 7.7 mg/L. Two disc biopsies were performed and sent to the microbiology and pathology laboratories for analysis. Five days of culture at 35 °C on bacterial culture media (Columbia Selective Agar with Sheep Blood and Chocolate agar with Vitox, Thermo Scientific®, France) and on Sabouraud plates (Sabouraud agar with gentamicin and chloramphenicol, Thermo Scientific®) yielded green colonies in pure culture. A direct examination with methylene blue was performed and showed short conidiophores prolonged with small vesicles. The Aspergillus heads were biseriate, in flared columns, and the microconidia were echinulate. As there were no Hulle cells or cleistothecia, the Aspergillus spp. was identified, and the culture was sent to the Mycology Department at the Regional University Hospital. The culture strain was analyzed via conventional PCR targeting the internal transcribed spacer (ITS) region, using the primers ITS1 (5′-TCCGATAGGTGAACCTGCGG-3′) and ITS4 (5′-TCCTCCGCTTATTGATATGC-3′), followed by sequencing of the 375 bp amplification products. Taq polymerase (Taq Hot Diamond, Eurogentec) and TaqMan polymerase were employed for the amplification of the target fragment (<500 bp) and for sequencing, respectively. BLAST analysis (Version 2.8.1) revealed a 99.2% nucleotide sequence identity with the sequence UOA/HCPF 9011 from the A. nidulans strain MITS 265 ISHAM-ITS. In parallel, we performed a galactomannan antigenemia assay (PlateliaTM Aspergillus Ag; Biorad®), which was positive at 0.83 (controlled at 1.1), and a (1-3)-β-D-glucan assay (Fungitell®), which was negative (48 pg/mL). Histopathologic examination of the biopsies revealed no evidence of fungal invasion or fungal elements.
Based on the clinical signs, imaging investigations, culture examination, and positive antigenic tests, a diagnosis of SCAN was made. An antifungal susceptibility test (AFST) was performed using the E-test (bioMerieux®) to determine the minimum inhibitory concentration (MIC), interpreted according to the breakpoints set by the European Committee on Antimicrobial Susceptibility Testing (EUCAST). The strain was susceptible to itraconazole and isavuconazole (Table 1).

Table 1.
Antifungal susceptibility test results on the A. nidulans strain.
There were no established breakpoints for voriconazole, posaconazole, caspofungin, or amphotericin B in 2018. Conventionally , in the absence of an interpretative threshold, a low MIC value is considered susceptible. The patient received 6 mg/kg of voriconazole every 12 h on day 1 followed by 4 mg/kg (350 mg) twice daily. Monitoring performed on day 5 of treatment found that the plasma voriconazole concentration was too high at 10.35 mg/L (trough levels between 1 and 5 mg/L), so the dose was reduced to 200 mg twice daily. The plasma concentrations of voriconazole were monitored on the 12th and 20th days, with the levels measured at 5.69 and 2.98 mg/L, respectively. Spine immobilization was prescribed, but no surgery was required. As recommended by the National Reference Center of Mycology, the patient received antifungal treatment with voriconazole for 6 months, with clinical improvement observed after 3 months (from January) and radiologic regression a month later. The center advised discontinuing the therapy based on clinical and imaging findings.
The galactomannan serum antigen was measured twice in November and at every follow-up consultation (in January, February, and April). It remained positive for 3 months until January. To understand the route of infection, fibroscopy and bronchoalveolar lavage were performed, revealing an inflammatory aspect of the bronchi. The culture examination from the fibro-aspiration found a colony of A. fumigatus and the development of Candida albicans. Additionally, sinus, cerebral, and pulmonary computer tomography (CT) scans were performed, but no microbiological documentation was found. Hepatic MRI found a lesion suggestive of a fungal abscess, but it was not explored further, as it was not accessible by ultrasound. A positron emission tomography (PET) scan performed in March found no abnormality. Thus, SCAN was considered successfully managed. Nevertheless, the patient died from comorbidities 4 years later, in October 2022.
3. Discussion
In the case we present here, the patient suffered from lower back pain associated with an inflammatory syndrome. MRI revealed vertebral lesions and microbiology results confirmed A. nidulans on two disc biopsies. These elements confirmed a diagnosis of SCAN. Diagnosis was further supported by galactomannan antigen testing, which was >0.8 in November and remained positive (>0.5) for 3 months after the initiation of antifungal therapy.
A limitation in the strain identification level should be noted. The molecular target (ITS) confirmed the nidulans complex. For species-level confirmation, markers like β-tubulin or calmodulin should be used [2].
It is important to remember that spondylodiscitis, or vertebral osteomyelitis, is an infection of the intervertebral disc, with a possible extension to adjacent vertebrae. Immunocompromised patients presenting inflammatory spinal pain associated with positive imaging should be investigated for infectious spondylodiscitis [4]. Aspergillus spondylodiscitis is diagnosed on a positive culture of bone tissue obtained via disc biopsy [5].
A review of the literature including the key words “spondylodiscitis” or “vertebral osteomyelitis”, “case report”, and “Aspergillus nidulans” was performed in January 2024 and found two published cases. In 2013, a case report and literature review by Jiang et al. [6] covering the period 1965 to 2012 found three cases of SCAN. In 2014, Gamaletsou et al. [7] analyzed 180 well-described cases of Aspergillus osteomyelitis over a period from 1947 to 2013 and also found three cases due to A. nidulans. Seven years later, Pernat et al. [8] found 112 cases of vertebral aspergillosis, with 2 being due to A. nidulans. The same year, Koutserimpas et al. [9] reviewed 118 cases of spondylodiscitis caused by Aspergillus spp. (SCAS) between 1936 and 2021, finding 7 due to A. nidulans. We summarize the findings of the 13 published case reports of SCAN in Table 2 [6,10,11,12,13,14,15,16,17,18,19]. Whatever the exact number of cases, SCAS is rare, especially cases due to A. nidulans.

Table 2.
The listing of 13 case reports of spondylodiscitis caused by A. nidulans, with findings precisely published, and our case.
The most recent published case report with A. nidulans described infection in an immunocompetent patient [18]. More generally, osteomyelitis caused by the Aspergillus spp. affects immunocompromised patients [3,6,7,9,20]. The main risk factors are corticosteroid use, primary immunodeficiencies, mainly chronic granulomatous disease (CGD), neutropenia, transplantation, hematological malignancy, solid tumors, HIV infection, and diabetes mellitus [3,20]. More specifically, A. nidulans, an extremely rare mold in patients with cancer, is isolated much more frequently in CGD patients and, indeed, with the same frequency as that of A. fumigatus [20]. On analyzing the thirteen published cases of SCAN, ten (77%) patients were immunocompromised, and nine of these (69%) were due to CGD. The male sex and young age of the majority of patients with SCAN are linked to CGD. Three patients were identified as immunocompetent, although the first case was probably unknown CGD. Our case is the first SCAN to be declared in an immunocompromised patient by a pathology other than CGD.
The most recent review of SCAS [9] reports that the lumbar spine is frequently affected (37.3%), as described in the present case report. However, this is not true for the 13 case reports of SCAN (Table 2) where the thoracic vertebra was the main localization for 12 (86%) and extensive in 5 (36%).
The definite diagnosis of SCAS remains delicate. Since 1994, most cases are suggested by lesions detected on MRI and diagnosed through cultures (73.7%), followed by histopathology, but rarely by the galactomannan antigen (2 cases = 1.8%) [9]. Moreover, antifungal susceptibilities are generally not provided [8,9]. In our case, the diagnosis was suspected on MRI images, and the involvement of the Aspergillus spp. was confirmed by cultures on two biopsies. The A. nidulans complex was identified through molecular biology, along with persistently positive galactomannan, and susceptibility tests were performed.
Although most of the authors do not describe the gateway [3,6,7,8,21], SCAS could be explained by three pathogenic mechanisms: direct invasion by contiguous pulmonary foci, hematogenous diffusion, and iatrogenic or traumatic inoculation [9,22]. In our case, fibroscopy and bronchoalveolar lavage did not provide contributive findings. Additionally, sinus, cerebral, and pulmonary CT scans revealed no abnormalities. Once again, the route of infection remained unidentified.
In 2023, an extensive systematic review analyzed 1072 patients with fungal osteomyelitis by Aspergillus (26.5%), followed by Candida (20.7%) and Mucor (16.8%) [23]. Full recovery was observed in 72.8%. These authors reported that Aspergillus infection was strongly associated with mortality, and vertebral involvement further reduced the chances of survival. Surprisingly, the three reviews focusing specifically on SCAS found quite similar percentages of positive outcomes: 71%, 71.2%, and 78.8% [3,8,9]. The mortality rate of SCAN appears to be high, with potential differences between A. nidulans osteomyelitis and spondylodiscitis, despite the small cohort sizes. Indeed, in 2004, A. nidulans osteomyelitis was associated with a 50% mortality (7/14 cases) compared to A. fumigatus osteomyelitis (0/10 cases) in CGD patients [24]. Ten years later, our review confirms these data with six (46%) patients who died (Table 2). Dotis et al. [24] specified that a successful outcome was achieved by prompt antifungal treatment combined with surgery and immunotherapy. In our case, SCAN was successfully resolved, more than likely because of prompt treatment on symptom onset, a non-extensive vertebra lesion, and weakening with the use of voriconazole.
Surgery to treat SCAS does not appear to be of added value to antifungal therapy for some authors [3,9,20], while it does for others [7,18]. More precisely, surgery was performed in 11 (85%) of the SCAN cases we reported (Table 2), probably due to the severity of the cases, but also due to non-compliant discontinuation of voriconazole after hospital discharge in one case. Surgical debridement was not necessary for the case we report here.
There is currently a lack of firm treatment recommendations for Aspergillus spondylodiscitis [25,26]. In the 2014 review by Gabrielli et al. [3], the most commonly used drug was amphotericin B, followed by itraconazole and voriconazole. In the first 2021 review, Koutserimpas et al. [9] report that voriconazole is used as the first antifungal agent (62%) after 2003. However, this contrasts with the second review published in 2021 by Perna et al. [8], which reports that medical treatments consisted mainly of a combination of two or more drugs (50 patients = 45%, 2 with voriconazole), with only 12 patients (10.8%) receiving voriconazole alone. Focusing on the thirteen cases of SCAN, nine (69%) and seven (54%) patients received amphotericin B or voriconazole alone or in combination, respectively (Table 2). The choice of the antifungal obviously depends on the year of the observation. In our case, voriconazole was selected as the drug of choice for invasive aspergillosis [20,27]. With reference to the data found in the literature, the duration of antifungal treatment seems to be at least 6 months. We consulted the National Reference Center of Mycology for advice in our case, who recommended 6 months of voriconazole and to check MRI and clinical values before stopping treatment. Notably, the recent 2023 systematic review of reported cases of fungal osteomyelitis found an association between longer treatment duration and increased survival, whereas shorter treatment was linked to higher mortality [23].
Some authors underline the importance of identifying the species [27] notably involved in SCAS [9]. The same authors emphasized the critical importance of performing antifungal susceptibility testing, as an increased rate of azole resistance was reported recently in the Netherlands and the United Kingdom [9]. Susceptibility tests are essential not only to treat the patient but also to monitor resistance to the antifungal. An example was described in the case report and review published in 2013 [6]. The patient underwent decompressive surgery before receiving voriconazole. Nevertheless, she did not continue voriconazole treatment after discharge and relapsed 16 months later. After the second drug susceptibility results, she continued with voriconazole treatment for a further 6 months with a successful outcome.
In 2016, the Infectious Diseases Society of America recommended that for the diagnosis and management of aspergillosis, serial monitoring of serum galactomannan could be used in appropriate patient subpopulations (hematologic malignancy, after hematopoietic stem cell transplantation) who have an elevated galactomannan level at baseline to monitor disease progression and therapeutic response and to predict the outcome [26]. Focusing specifically on SCAS, the role of serum galactomannan remains a topic of debate Ref. [8] and is rarely used as a diagnostic tool [8,9,23]. In our case, the galactomannan assay remained positive for 3 months. It appears, therefore, to be an interesting marker for suspected spondylodiscitis of fungal origin and constitutes another diagnostic element.
In our case, the (1-3)-β-D-glucan assay was not contributory in advancing the diagnosis of SCAN. This result supports the limited role of this marker in invasive aspergillosis [27].
This case represents the comprehensive management of a SCAN case, detailing the clinical signs, imaging findings, fungal isolation and identification, antifungal susceptibility, and galactomannan antigen dynamics. Based on our current knowledge, it is the first reported case of SCAN in an immunocompromised patient with a malignancy other than CGD to achieve a successful therapeutic outcome without surgical debridement.
Author Contributions
All authors contributed to the data collection. The first draft of the manuscript was written by S.N. and E.M. All authors commented on previous versions of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The Clinical Research Ethics Commission (CERCl) of Valenciennes Hospital met to examine the project entitled “Spondylodiscitis caused by Aspergillus nidulans, a case report of a rare cause of osteomyelitis” and gave a favorable opinion (Ref CHV-2023-013) after examining its conformity with the rules governing clinical research (Date: 20 December 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data used in this study are available upon reasonable request.
Conflicts of Interest
The authors declare no competing interests.
References
- De Hoog, G.S.; Guarro, J.; Gené, J.; Ahmed, S.; Al-Hatmi, A.M.S.; Figueras, M.J.; Vitale, R.G. Atlas of Clinical Fungi, 3rd ed.; Westerdijk Institute: Utrecht, The Netherlands; Universitat Rovira i Virgili: Reus, Spain, 2019. [Google Scholar]
- Seyedmousavi, S.; Lionakis, M.S.; Parta, M.; Peterson, S.W.; Kwon-Chung, K.J. Emerging Aspergillus Species Almost Exclusively Associated With Primary Immunodeficiencies. Open Forum Infect. Dis. 2018, 5, ofy213. [Google Scholar] [CrossRef] [PubMed]
- Gabrielli, E.; Fothergill, A.W.; Brescini, L.; Sutton, D.A.; Marchionni, E.; Orsetti, E.; Staffolani, S.; Castelli, P.; Gesuita, R.; Barchiesi, F. Osteomyelitis caused by Aspergillus species: A review of 310 reported cases. Clin. Microbiol. Infect. 2014, 20, 559–565. [Google Scholar] [CrossRef]
- Berbari, E.F.; Kanj, S.S.; Kowalski, T.J.; Darouiche, R.O.; Widmer, A.F.; Schmitt, S.K.; Hendershot, E.F.; Holtom, P.D.; Huddleston, P.M.; Petermann, G.W.; et al. 2015 Infectious Diseases Society of America (IDSA) Clinical Practice Guidelines for the Diagnosis and Treatment of Native Vertebral Osteomyelitis in Adults. Clin. Infect. Dis. 2015, 61, e26–e46. [Google Scholar] [CrossRef] [PubMed]
- Dotis, J.; Panagopoulou, P.; Filioti, J.; Winn, R.; Toptsis, C.; Panteliadis, C.; Roilides, E. Femoral Osteomyelitis Due to Aspergillus nidulans in a Patient with Chronic Granulomatous Disease. Infection 2003, 31, 121–124. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; Wang, Y.; Jiang, Y.; Xu, Y.; Meng, B. Vertebral osteomyelitis and epidural abscess due to Aspergillus nidulans resulting in spinal cord compression: Case report and literature review. J. Int. Med. Res. 2013, 41, 502–510. [Google Scholar] [CrossRef]
- Gamaletsou, M.N.; Rammaert, B.; Bueno, M.A.; Moriyama, B.; Sipsas, N.V.; Kontoyiannis, D.P.; Roilides, E.; Zeller, V.; Prinapori, R.; Taj-Aldeen, S.J.; et al. Aspergillus osteomyelitis: Epidemiology, clinical manifestations, management, and outcome. J. Infect. 2014, 68, 478–493. [Google Scholar] [CrossRef]
- Perna, A.; Ricciardi, L.; Fantoni, M.; Taccari, F.; Torelli, R.; Santagada, D.A.; Fumo, C.; Tamburrelli, F.C.; Proietti, L. Spontaneous Vertebral Aspergillosis, the State of Art: A Systematic Literature Review. Neurospine 2021, 18, 23–33. [Google Scholar] [CrossRef]
- Koutserimpas, C.; Chamakioti, I.; Naoum, S.; Raptis, K.; Alpantaki, K.; Kofteridis, D.P.; Samonis, G. Spondylodiscitis Caused by Aspergillus Species. Diagnostics 2021, 11, 1899. [Google Scholar] [CrossRef]
- Redmond, A.; Carre, I.J.; Biggart, J.D.; Mackenzie, D.W. Aspergillosis (Aspergillus nidulans) involving bone. J. Pathol. Bacteriol. 1965, 89, 391–395. [Google Scholar] [CrossRef]
- Altman, A.R. Thoracic wall invasion secondary to pulmonary aspergillosis: A complication of chronic granulomatous disease of childhood. AJR Am. J. Roentgenol. 1977, 129, 140–142. [Google Scholar] [CrossRef]
- White, C.J.; Kwon-Chung, K.J.; Gallin, J.I. Chronic granulomatous disease of childhood. An unusual case of infection with Aspergillus nidulans var. echinulatus. Am. J. Clin. Pathol. 1988, 90, 312–316. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Shin, J.H.; Suh, S.P.; Ryang, D.W.; Park, C.S.; Kim, C.; Kook, H.; Kim, J. Aspergillus nidulans infection in a patient with chronic granulomatous disease. J. Korean Med. Sci. 1997, 12, 244–248. [Google Scholar] [CrossRef]
- Segal, B.H.; DeCarlo, E.S.; Kwon-Chung, K.J.; Malech, H.L.; Gallin, J.I.; Holland, S.M. Aspergillus nidulans infection in chronic granulomatous disease. Medicine 1998, 77, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Notheis, G.; Tarani, L.; Costantino, F.; Jansson, A.; Rosenecker, J.; Friederici, D.; Belohradsky, B.H.; Reinhardt, D.; Seger, R.; Schweinitz, D.V.; et al. Posaconazole for treatment of refractory invasive fungal disease. Mycoses 2006, 49 (Suppl. 1), 37–41. [Google Scholar] [CrossRef]
- Dellepiane, R.M.; Tortorano, A.M.; Liotto, N.; Laicini, E.; Di Landro, G.; Carnelli, V.; Pietrogrande, M.C. Invasive Aspergillus nidulans infection in a patient with chronic granulomatous disease. Mycoses 2008, 51, 458–460. [Google Scholar] [CrossRef] [PubMed]
- Bukhari, E.; Alrabiaah, A. First case of extensive spinal cord infection with Aspergillus nidulans in a child with chronic granulomatous disease. J. Infect. Dev. Ctries. 2009, 3, 321–323. [Google Scholar] [CrossRef][Green Version]
- Lyons, M.K.; Neal, M.T.; Patel, N.P.; Vikram, H.R. Progressive Back Pain due to Aspergillus nidulans Vertebral Osteomyelitis in an Immunocompetent Patient: Surgical and Antifungal Management. Case Rep. Orthop. 2019, 2019, 4268468. [Google Scholar] [CrossRef]
- Tavakoli, M.; Hedayati, M.T.; Mirhendi, H.; Nouripour-Sisakht, S.; Hedayati, N.; Saghafi, F.; Mamishi, S. The first rare and fatal case of invasive aspergillosis of spinal cord due to Aspergillus nidulans in an Iranian child with chronic granulomatosis disease: Review of literature. Curr. Med. Mycol. 2020, 6, 55–60. [Google Scholar] [CrossRef]
- Papachristou, S.G.; Iosifidis, E.; Sipsas, N.V.; Gamaletsou, M.N.; Walsh, T.J.; Roilides, E. Management of osteoarticular fungal infections in the setting of immunodeficiency. Expert Rev. Anti Infect. Ther. 2020, 18, 461–474. [Google Scholar] [CrossRef]
- Comacle, P.; Le Govic, Y.; Hoche-Delchet, C.; Sandrini, J.; Aguilar, C.; Bouyer, B.; Blanchi, S.; Penn, P. Spondylodiscitis Due to Aspergillus terreus in an Immunocompetent Host: Case Report and Literature Review. Mycopathologia 2016, 181, 575–581. [Google Scholar] [CrossRef]
- Studemeister, A.; Stevens, D.A. Aspergillus vertebral osteomyelitis in immunocompetent hosts: Role of triazole antifungal therapy. Clin. Infect. Dis. 2011, 52, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Asperges, E.; Albi, G.; Truffelli, F.; Salvaderi, A.; Puci, F.; Sangani, A.; Zuccaro, V.; Scotti, V.; Orsolini, P.; Brunetti, E.; et al. Fungal Osteomyelitis: A Systematic Review of Reported Cases. Microorganisms 2023, 11, 1828. [Google Scholar] [CrossRef] [PubMed]
- Dotis, J.; Roilides, E. Osteomyelitis due to Aspergillus spp. in patients with chronic granulomatous disease: Comparison of Aspergillus nidulans and Aspergillus fumigatus. Int. J. Infect. Dis. 2004, 8, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Tissot, F.; Agrawal, S.; Pagano, L.; Petrikkos, G.; Groll, A.H.; Skiada, A.; Lass-Flörl, C.; Calandra, T.; Viscoli, C.; Herbrecht, R. ECIL-6 guidelines for the treatment of invasive candidiasis, aspergillosis and mucormycosis in leukemia and hematopoietic stem cell transplant patients. Haematologica 2017, 102, 433–444. [Google Scholar] [CrossRef]
- Patterson, T.F.; Thompson, G.R.; Denning, D.W.; Fishman, J.A.; Hadley, S.; Herbrecht, R.; Kontoyiannis, D.P.; Marr, K.A.; Morrison, V.A.; Nguyen, M.H.; et al. Practice Guidelines for the Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 63, e1–e60. [Google Scholar] [CrossRef]
- Ullmann, A.J.; Aguado, J.M.; Arikan-Akdagli, S.; Denning, D.W.; Groll, A.H.; Lagrou, K.; Lass-Flörl, C.; Lewis, R.E.; Munoz, P.; Verweij, P.E.; et al. Diagnosis and management of Aspergillus diseases: Executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin. Microbiol. Infect. 2018, 24 (Suppl. 1), e1–e38. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).