Fungal Infections and Colonization after Bilateral Lung Transplant: A Six-Year Single-Center Experience
Abstract
1. Introduction
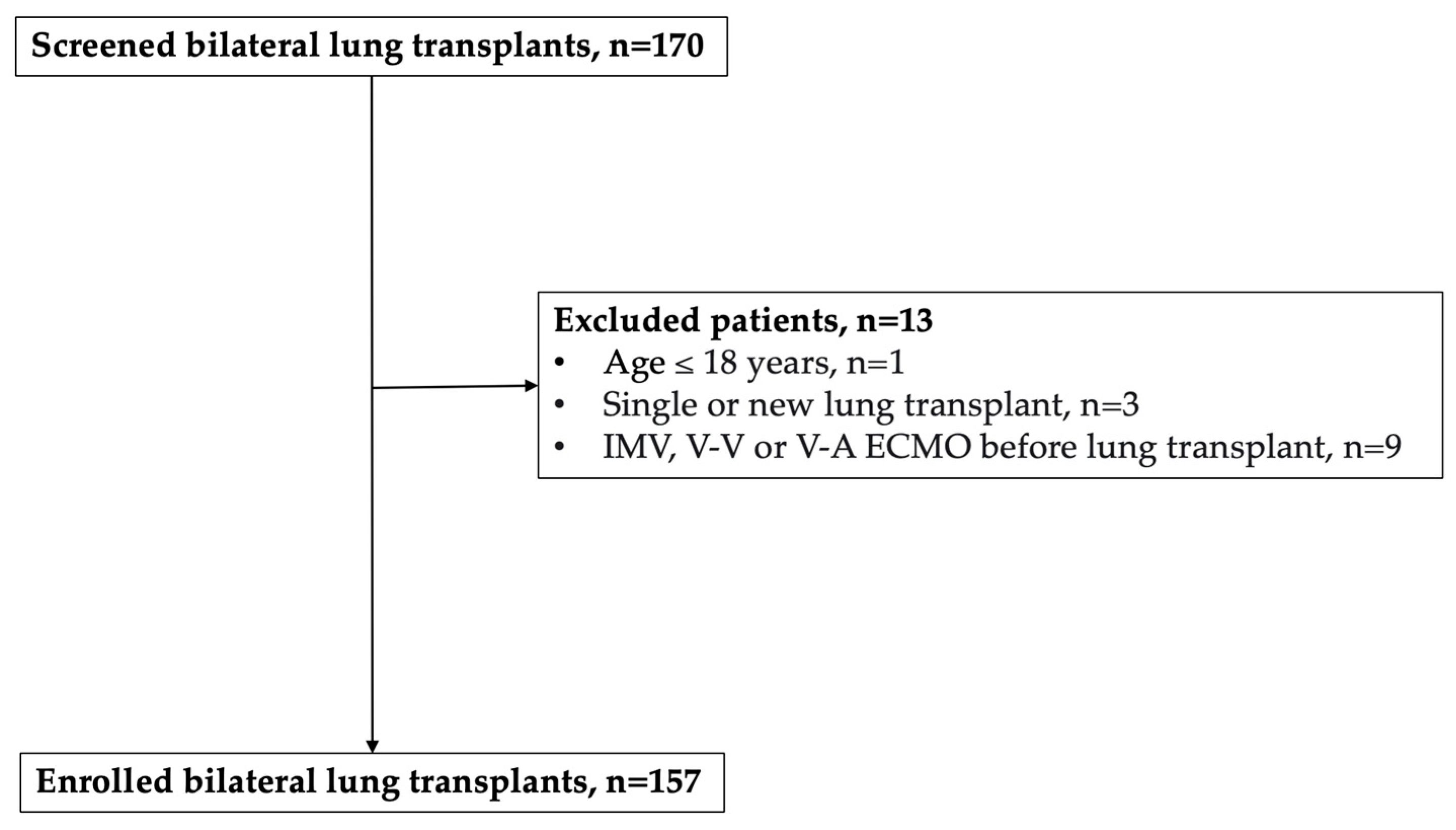
2. Materials and Methods
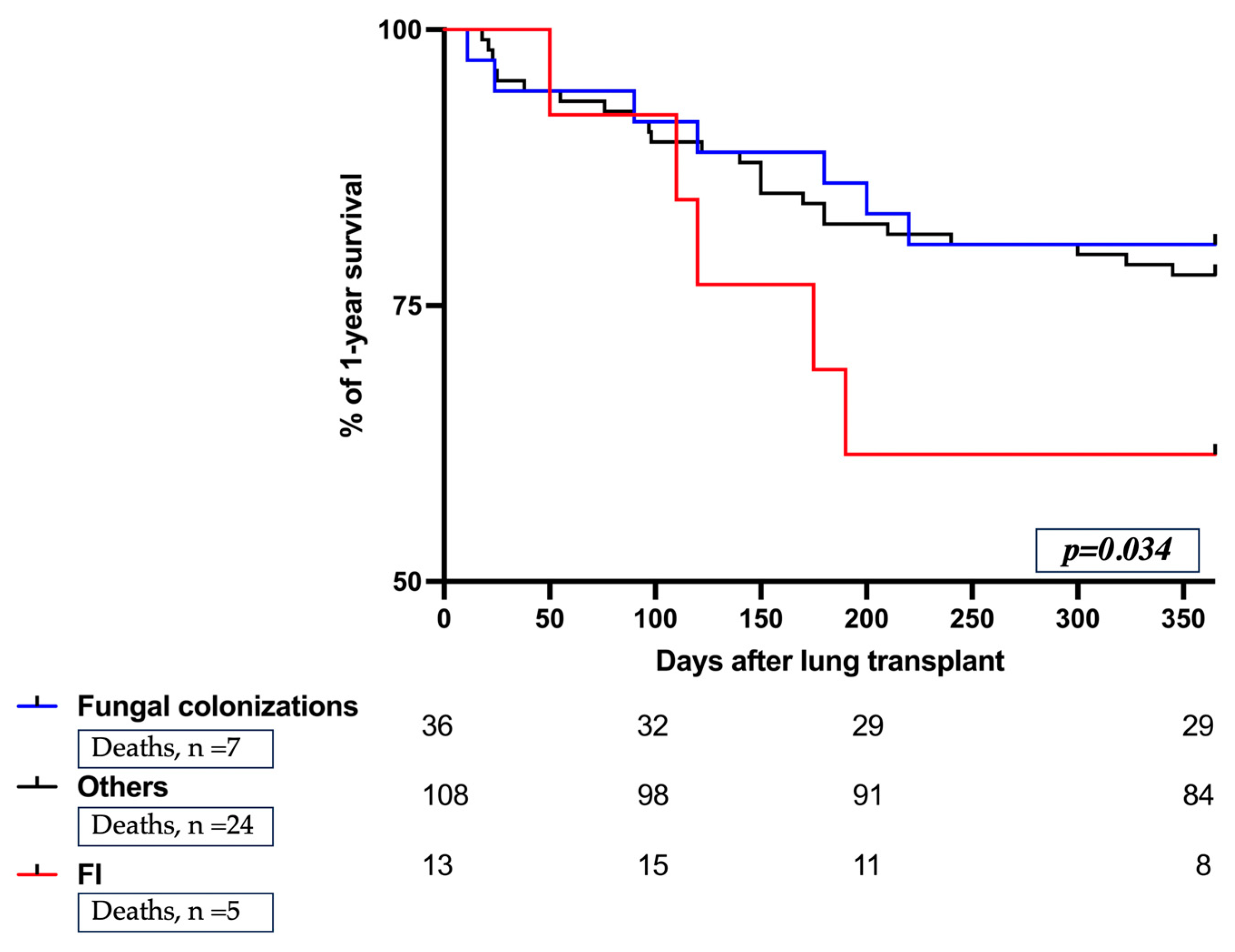
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ascioglu, S.; Rex, J.H.; de Pauw, B.; Bennett, J.E.; Bille, J.; Crokaert, F.; Denning, D.W.; Donnelly, J.P.; Edwards, J.E.; Erjavec, Z.; et al. Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: An international consensus. Clin. Infect. Dis. 2002, 34, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Ullmann, A.J.; Aguado, J.M.; Arikan-Akdagli, S.; Denning, D.W.; Groll, A.H.; Lagrou, K.; Lass-Flörl, C.; Lewis, R.E.; Munoz, P.; Verweij, P.E.; et al. Diagnosis and management of Aspergillus diseases: Executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin. Microbiol. Infect. 2018, 24 (Suppl. 1), e1–e38. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, J.P.; Chen, S.C.; Kauffman, C.A.; Steinbach, W.J.; Baddley, J.W.; Verweij, P.E.; Clancy, C.J.; Wingard, J.R.; Lockhart, S.R.; Groll, A.H.; et al. Revision and Update of the Consensus Definitions of Invasive Fungal Disease From the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin. Infect. Dis. 2020, 71, 1367–1376. [Google Scholar] [CrossRef] [PubMed]
- Gavalda, J.; Len, O.; San Juan, R.; Aguado, J.M.; Fortun, J.; Lumbreras, C.; Moreno, A.; Munoz, P.; Blanes, M.; Ramos, A.; et al. Risk factors for invasive aspergillosis in solid-organ transplant recipients: A case-control study. Clin. Infect. Dis. 2005, 41, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Pappas, P.G.; Alexander, B.D.; Andes, D.R.; Hadley, S.; Kauffman, C.A.; Freifeld, A.; Anaissie, E.J.; Brumble, L.M.; Herwaldt, L.; Ito, J.; et al. Invasive fungal infections among organ transplant recipients: Results of the Transplant-Associated Infection Surveillance Network (TRANSNET). Clin. Infect. Dis. 2010, 50, 1101–1111. [Google Scholar] [CrossRef] [PubMed]
- Doligalski, C.T.; Benedict, K.; Cleveland, A.A.; Park, B.; Derado, G.; Pappas, P.G.; Baddley, J.W.; Zaas, D.W.; Harris, M.T.; Alexander, B.D. Epidemiology of invasive mold infections in lung transplant recipients. Am. J. Transplant. 2014, 14, 1328–1333. [Google Scholar] [CrossRef]
- Vazquez, R.; Vazquez-Guillamet, M.C.; Suarez, J.; Mooney, J.; Montoya, J.G.; Dhillon, G.S. Invasive mold infections in lung and heart-lung transplant recipients: Stanford University experience. Transpl. Infect. Dis. 2015, 17, 259–266. [Google Scholar] [CrossRef]
- Villalobos, A.P.; Husain, S. Infection prophylaxis and management of fungal infection in lung transplant. Ann. Transl. Med. 2020, 8, 414. [Google Scholar] [CrossRef]
- Kennedy, C.C.; Pennington, K.M.; Beam, E. Fungal infection in lung transplant. Semin. Respir. Crit. Care Med. 2021, 42, 471–482. [Google Scholar]
- Baek, Y.-J.; Cho, Y.-S.; Kim, M.-H.; Hyun, J.-H.; Sohn, Y.-J.; Kim, S.-Y.; Jeong, S.-J.; Park, M.-S.; Lee, J.-G.; Paik, H.-C. The prediction and Prognosis of Fungal Infection in Lung Transplant Recipients—A retrospective cohort study in South Korea. J. Fungi 2021, 7, 639. [Google Scholar] [CrossRef]
- Hosseini-Moghaddam, S.M.; Ouédraogo, A.; Naylor, K.L.; Bota, S.E.; Husain, S.; Nash, D.M.; Paterson, J.M. Incidence and outcomes of invasive fungal infection among solid organ trans-plant recipients: A population-based cohort study. Transpl. Infect. Dis. 2020, 22, e13250. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.; Musk, M.; Lavender, M.; Wrobel, J.; Yaw, M.; Lawrence, S.; Chirayath, S.; Boan, P. Epidemiology of invasive fungal infections in lung transplant recipients in Western Australia. Transpl. Infect. Dis. 2019, 21, e13085. [Google Scholar] [CrossRef] [PubMed]
- Pennington, K.M.; Aversa, M.; Martinu, T.; Johnson, B.; Husain, S. Fungal infection and colonization in lung transplant recipients with chronic lung allograft dysfunction. Transpl. Inf. Dis. 2022, 24, e13986. [Google Scholar] [CrossRef] [PubMed]
- Husain, S.; Paterson, D.L.; Studer, S.; Pilewski, J.; Crespo, M.; Zaldonis, D.; Shutt, K.; Pakstis, D.L.; Zeevi, A.; Johnson, B.; et al. Voriconazole prophylaxis in lung transplant recipients. Am. J. Transplant. 2006, 6, 3008–3016. [Google Scholar] [CrossRef]
- Luong, M.L.; Chaparro, C.; Stephenson, A.; Rotstein, C.; Singer, L.G.; Waters, V.; Azad, S.; Keshavjee, S.; Tullis, E.; Husain, S. Pretransplant Aspergillus colonization of cystic fibrosis patients and the incidence of post-lung transplant invasive aspergillosis. Transplantation 2014, 97, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, C.A.; Hamandi, B.; Fegbeutel, C.; Silveira, F.; Verschuuren, E.; Ussetti, P.; Chin-Hong, P.; Sole, A.; Holmes-Liew, C.; Billaud, E.; et al. Clinical Risk Factors for Invasive Aspergillosis in Lung Transplant Recipients: Results of an International Cohort Study. J. Heart Lung Transplant. 2018, 36, S24. [Google Scholar] [CrossRef]
- Pilarczyk, K.; Haake, N.; Heckmann, J.; Carstens, H.; Haneya, A.; Cremer, J.; Jakob, H.; Pizanis, N.; Kamler, M. Is universal antifungal prophylaxis mandatory in adults after lung transplantation? A review and meta-analysis of observational studies. Clin. Transplant. 2016, 30, 1522–1531. [Google Scholar] [CrossRef] [PubMed]
- Patterson, T.F.; Thompson, G.R., 3rd; Denning, D.W.; Fishman, J.A.; Hadley, S.; Herbrecht, R.; Kontoyiannis, D.P.; Marr, K.A.; Morrison, V.A.; Nguyen, H.M.; et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 63, e1–e60. [Google Scholar] [CrossRef]
- Pennington, K.M.; Yost, K.J.; Escalante, P.; Razonable, R.R.; Kennedy, C.C. Antifungal prophylaxis in lung transplant: A survey of United States’ transplant centers. Clin. Transplant. 2019, 33, e13630. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13 (Suppl. 1), S31–S34. [Google Scholar] [CrossRef]
- Di Nardo, M.; Tikkanen, J.; Husain, S.; Singer, L.G.; Cypel, M.; Ferguson, N.D.; Keshavjee, S.; Del Sorbo, L. Postoperative Management of Lung Transplant Recipients in the Intensive Care Unit. Anesthesiology 2022, 136, 482–499. [Google Scholar] [CrossRef] [PubMed]
- Marczin, N.; de Waal, E.E.C.; Hopkins, P.M.A.; Mulligan, M.S.; Simon, A.; Shaw, A.D.; Van Raemdonck, D.; Neyrinck, A.; Gries, C.J.; Algotsson, L.; et al. International consensus recommendations for anesthetic and intensive care management of lung transplantation. An EACTAIC, SCA, ISHLT, ESOT, ESTS, and AST approved document. J. Heart Lung Transplant. 2021, 40, 1327–1348. [Google Scholar] [CrossRef] [PubMed]
- Aslam, S.; Rotstein, C. Candida infections in solid organ transplantation: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. AST Infect. Dis. Community Pract. Clin. Transplant. 2019, 33, e13623. [Google Scholar] [CrossRef] [PubMed]
- Boscolo, A.; Sella, N.; Pettenuzzo, T.; De Cassai, A.; Crociani, S.; Schiavolin, C.; Simoni, C.; Geraldini, F.; Lorenzoni, G.; Faccioli, E.; et al. Multidrug-Resistant and Extended-Spectrum β-Lactamase Gram-Negative Bacteria in Bilateral Lung Transplant Recipients: Incidence, Risk Factors, and In-Hospital Mortality. Chest 2022, 162, 1255–1264. [Google Scholar] [CrossRef] [PubMed]
- Congedi, S.; NAvalesi, P.; Boscolo, A. Multidrug-resistant organisms in lung transplant: A narrative review. Curr. Opin. Organ Transplant. 2023, 28, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Boscolo, A.; Dell’Amore, A.; Pettenuzzo, T.; Sella, N.; De Cassai, A.; Pistollato, E.; Cacco, N.; Manzan, A.; De Carolis, A.; Geraldini, F.; et al. The Impact of New Treatments on Short- and MID-Term Outcomes in Bilateral Lung Transplant: A Propensity Score Study. J. Clin. Med. 2022, 11, 5859. [Google Scholar] [CrossRef] [PubMed]
- Yong, M.Y.; Slavin, M.A.; Kontoyiannis, D.P. Invasive fungal disease and cytomegalovirus infection: Is there an association? Curr. Opin. Infect. Dis. 2018, 31, 481–489. [Google Scholar] [CrossRef]
- Avery, R.K.; Silveira, F.P.; Benedict, K.; Cleveland, A.A.; Kauffman, C.A.; Schuster, M.G.; Dubberke, E.R.; Husain, S.; Paterson, D.L.; Chiller, T.; et al. Cytomegalovirus infections in lung and hematopoietic cell transplant recipients in the Organ Transplant Infection Prevention and Detection Study: A multi-year, multicenter prospective cohort study. Transpl. Infect. Dis. 2018, 20, e12877. [Google Scholar] [CrossRef]
- Burguete, S.R.; Maselli, D.J.; Fernandez, J.F.; Levine, S.M. Lung transplant infection. Respirology 2013, 18, 22–38. [Google Scholar] [CrossRef]
- Bassetti, M.; Garnacho-Montero, J.; Calandra, T.; Kullberg, B.; Dimopoulos, G.; Azoulay, E.; Chakrabarti, A.; Kett, D.; Leon, C.; Ostrosky-Zeichner, L.; et al. Intensive care medicine research agenda on invasive fungal infection in critically ill patients. Intensive Care Med. 2017, 43, 1225–1238. [Google Scholar] [CrossRef]
- Boroujeni, Z.B.; Shamsaei, S.; Yarahmadi, M.; Getso, M.I.; Khorashad, A.S.; Haghighi, L.; Raissi, V.; Zareei, M.; Mohammadzade, A.S.; Moqarabzadeh, V.; et al. Distribution of invasive fungal infections: Molecular epidemiology, etiology, clinical conditions, diagnosis and risk factors: A 3-year experience with 490 patients under intensive care. Microb. Pathog. 2021, 152, 104616. [Google Scholar] [CrossRef] [PubMed]
- Monk, E.J.M.; Rautemaa-Richardson, R.; Felton, T.; Montalti, A.; Parkes, M.; Templeton, R.; Ashworth, A.; Garcia, M.; Barker, J.; Thomas, S. Incidence of candidemia in prolonged venovenous extracorporeal membrane oxygenation. J. Hosp. Infect. 2022, 119, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Huggins, J.P.; Pease, R.; Stanly, K.; Workman, A.; Reynolds, J.; Alexander, B.D. Safety of Inhaled Amphotericin B Lipid Complex as Antifungal Prophylaxis in Lung Transplant Recipients. Antimicrob. Agents Chemother. 2022, 66, e0028322. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Paterson, D.L. Aspergillus infections in transplant recipients. Clinl. Microbiol. Rev. 2005, 18, 44–69. [Google Scholar] [CrossRef]
- Jenks, J.D.; Nam, H.H.; Hoenigl, M. Invasive aspergillosis in critically ill patients: Review of definitions and diagnostic approaches. Mycoses 2021, 64, 1002–1014. [Google Scholar] [CrossRef]
- Calabrese, F.; Lunardi, F.; Baldasso, E.; Pezzuto, F.; Kilitci, A.; Olteanu, G.-E.; Del Vecchio, C.; Fortarezza, F.; Boscolo, A.; Schiavon, M.; et al. Comprehensive bronchoalveolar lavage characterization in COVID-19 associated acute respiratory distress syndrome patients: A prospective cohort study. Respir. Res. 2023, 24, 152. [Google Scholar] [CrossRef]
- Quirino, A.; Scaglione, V.; Marascio, N.; Mazzitelli, M.; Garofalo, E.; Divenuto, F.; Serapide, F.; Bruni, A.; Lionello, R.; Pavia, G.; et al. Role of the T2Dx magnetic resonance assay in patients with suspected bloodstream infection: A single-centre real-world experience. BMC Infect. Dis. 2022, 22, 113. [Google Scholar] [CrossRef]
- Pagano, L.; Cattaneo, C.; Quattrone, M.; Oberti, M.; Mazzitelli, M.; Trecarichi, E.M. Isavuconazole-Animal Data and Clinical Data. J. Fungi 2020, 6, 209. [Google Scholar] [CrossRef]
| Overall (n = 157, 100%) | FI (n = 13, 8%) | Fungal Colonization (n = 36, 23%) | Others (n = 108, 69%) | p-Value | Multivariable Analysis OR [95% CI], p-Value | |
|---|---|---|---|---|---|---|
| Baseline characteristics | ||||||
| Age, years, median (IQR) | 54 (41–60) | 50 (35.5–57.5) | 48 (36.75–60.25) | 55 (46–61) | 0.19 | - |
| Sex, male, n (%) | 102 (65) | 8 (61) | 24 (67) | 70 (65) | 0.94 | - |
| BMI, kg/m2, median (IQR) | 24 (20–26) | 25 (24–25) | 22 (18–28) | 23 (18–27) | 0.61 | - |
| Patients on Corticosteroids, n (%) | 84 (54) | 5 (38) | 21 (58) | 58 (54) | 0.48 | - |
| Patients on O2 therapy, n (%) | 141 (90) | 11 (85) | 33 (92) | 97 (90) | 0.77 | - |
| Diabetes, n (%) | 28 (19) | 1 (7) | 5 (14) | 22 (20) | 0.41 | - |
| Oto score, median (IQR) | 5 (2–44) | 4 (1–6) | 5 (2–24) | 5 (2–50) | 0.35 | - |
| LAS score, median (IQR) | 34 (32–38) | 38 (38–38) | 34 (31–34) | 33 (26–36) | 0.20 | - |
| Time from admission, days, n (%) | 147 (94) | 11 (85) | 34 (94) | 102 (94) | 0.38 | - |
| Underlying disease | ||||||
| Septal a, n (%) | 31 (19) | 3 (23) | 12 (33) | 16 (15) | 0.05 | - |
| Interstitial b, n (%) | 61 (39) | 4 (31) | 11 (31) | 46 (43) | 0.36 | - |
| Obstructive c, n (%) | 23 (15) | 0 (0) | 6 (17) | 17 (16) | 0.29 | - |
| Others d, n (%) | 42 (27) | 6 (46) | 7 (19) | 29 (27) | 0.18 | - |
| Previous colonization | ||||||
| Recipient-related bacteria, n (%) | 41 (26) | 4 (31) | 11 (31) | 26 (24) | 0.045 | 2.23 [0.03–7], p = 0.78 |
| Recipient-related fungi, n (%) | 7 (5) | 2 (15) | 2 (6) | 3 (3) | 0.19 | - |
| Recipient-related virus, n (%) | 35 (22) | 4 (31) | 12 (33) | 19 (18) | 0.003 | 2.48 [1.05–4.61], p = 0.52 |
| Donor-related bacteria, n (%) | 77 (49) | 6 (46) | 17 (47) | 54 (50) | 0.83 | - |
| Donor-related fungi, n (%) | 20 (13) | 1 (8) | 7 (19) | 12 (11) | 0.22 | - |
| Overall (n = 157, 100%) | FI (n = 13, 8%) | Fungal Colonization (n = 36, 23%) | Others (n = 108, 69%) | p-Value | |
|---|---|---|---|---|---|
| Surgical characteristics | |||||
| Time from LT, days, median (IQR) | 420 (365–480) | 430 (382–450) | 435 (378–502) | 420 (359–481) | 0.64 |
| Time of graft ischemia, days, median (IQR) | 560 (441–655) | 563 (461–731) | 575 (433–696) | 553 (452–630) | 0.51 |
| Intraoperative ECMO, n (%) | 103 (66) | 8 (62) | 26 (72) | 77 (71) | 0.75 |
| Surgical revision, n (%) | 29 (18) | 4 (31) | 10 (28) | 15 (14) | 0.09 |
| Prolonged ECMO, n (%) | 29 (18) | 5 (38) | 8 (22) | 16 (15) | 0.22 |
| Duration of prolonged ECMO, days, median (IQR) | 2 (0–3) | 3 (1–8.75) | 3 (2–4) | 1 (0–3) | 0.79 |
| During ICU stay | |||||
| Immunosuppressive therapy +, n (%) | 93 (59) | 9 (69) | 24 (67) | 60 (56) | 0.50 |
| Renal replacement therapy, n (%) | 24 (17) | 3 (23) | 8 (22) | 13 (12) | 0.30 |
| Antifungal therapies * and biomarkers | |||||
| Universal prophylaxis, n (%) | |||||
| (i) Liposomal amphotericin B i.v. plus inhaled amphotericin B lipid complex | 112 (71) | 9 (69) | 25 (69) | 78 (72) | 0.79 |
| (ii) Liposomal amphotericin B i.v. | 33 (21) | 2 (15) | 6 (17) | 25 (23) | 0.79 |
| (iii) Azoles or echinocandins | 12 (8) | 2 (15) | 5 (14) | 5 (5) | 0.79 |
| Mycological culture, n (%) | 49 (31) | 13 (100) | 36 (100) | - | 0.99 |
| BAL galactomannan antigen, ratio | 0 [0–3] | 4 [1–6] | 0 [0–2] | - | <0.001 |
| BAL galactomannan antigen > b1, n (%) | 12 (8) | 6 (46) | 6 (17) | - | 0.17 |
| β-D-glucan (reference > 80 pg/mL), n (%) | 8 (5) | 3 (23) | 5 (14) | - | 0.72 |
| Liposomal Amphotericin B iv. Plus Inhaled Amphotericin B Lipid Complex (n = 112, 71%) | Liposomal Amphotericin B iv. (n = 33, 21%) | Azoles or Echinocandins (n = 12, 8%) | p-Value | |
|---|---|---|---|---|
| Antifungal therapies and biomarkers | ||||
| FI, n (%) | 9 (8) | 2 (6) | 2 (17) | 0.29 |
| Fungal colonization, n (%) | 25 (22) | 6 (16) | 5 (42) | 0.29 |
| Others, n (%) | 78 (70) | 25 (76) | 5 (42) | 0.29 |
| Overall (n = 157, 100%) | FI (n = 13, 8%) | Fungal Colonization (n = 36, 23%) | Others (n = 108, 69%) | p-Value | |
|---|---|---|---|---|---|
| Primary outcome | |||||
| 1-year fungal isolation, n (%) | |||||
| (i) Aspergillus | 26 (17) | 10 (77) | 16 (44) | - | 0.013 |
| (ii) Candida albicans | 16 (10) | 0 (0) | 16 (44) | - | 0.013 |
| (iii) Others | 7 (5) | 3 (23) | 4 (11) | - | 0.013 |
| Time of fungal isolation, days, median (IQR) | 65 (12–142) | 34 (8–143) | 80 (12–142) | - | 0.48 |
| (i) Aspergillus | 110 (27–165) | 35 (11–135) | 122 (53–203) | - | 0.18 |
| (ii) Candida albicans | 12 (4–34) | - | 11 (3–34) | - | 0.18 |
| Other outcomes | |||||
| Re-tracheal intubation and/or tracheostomy, n (%) | 37 (24) | 7 (54) | 10 (28) | 20 (19) | 0.007 |
| Invasive mechanical ventilation, hours, median (IQR) | 36 (21–73) | 23 (10–180) | 42 (19–150) | 36 (22–93) | 0.97 |
| 30-day rejection, n (%) | 27 (17) | 4 (31) | 5 (14) | 18 (17) | 0.67 |
| ICU LOS, days, median (IQR) | 8 (6–16) | 5 [9–25] | 5 (10–26) | 8 (5–16) | 0.29 |
| Hospital LOS, days, median (IQR) | 33 (29–45) | 40 (29–79) | 35 (30–59) | 32 (28–43) | 0.14 |
| Hospital mortality, n (%) | 13 (8) | 2 (15) | 2 (6) | 8 (7) | 0.51 |
| 1-year mortality, n (%) | 36 (23) | 5 (38) | 7 (19) | 24 (22) | 0.64 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boscolo, A.; Cattelan, A.; Marinello, S.; Medici, F.; Pettenon, G.; Congedi, S.; Sella, N.; Presa, N.; Pistollato, E.; Silvestrin, S.; et al. Fungal Infections and Colonization after Bilateral Lung Transplant: A Six-Year Single-Center Experience. J. Fungi 2024, 10, 80. https://doi.org/10.3390/jof10010080
Boscolo A, Cattelan A, Marinello S, Medici F, Pettenon G, Congedi S, Sella N, Presa N, Pistollato E, Silvestrin S, et al. Fungal Infections and Colonization after Bilateral Lung Transplant: A Six-Year Single-Center Experience. Journal of Fungi. 2024; 10(1):80. https://doi.org/10.3390/jof10010080
Chicago/Turabian StyleBoscolo, Annalisa, Annamaria Cattelan, Serena Marinello, Francesca Medici, Giovanni Pettenon, Sabrina Congedi, Nicolò Sella, Nicolò Presa, Elisa Pistollato, Stefano Silvestrin, and et al. 2024. "Fungal Infections and Colonization after Bilateral Lung Transplant: A Six-Year Single-Center Experience" Journal of Fungi 10, no. 1: 80. https://doi.org/10.3390/jof10010080
APA StyleBoscolo, A., Cattelan, A., Marinello, S., Medici, F., Pettenon, G., Congedi, S., Sella, N., Presa, N., Pistollato, E., Silvestrin, S., Biscaro, M., Muraro, L., Peralta, A., Mazzitelli, M., Dell’Amore, A., Rea, F., & Navalesi, P. (2024). Fungal Infections and Colonization after Bilateral Lung Transplant: A Six-Year Single-Center Experience. Journal of Fungi, 10(1), 80. https://doi.org/10.3390/jof10010080







