The Cardiovascular-Mortality-Based Estimate for Normal Range of the Ankle–Brachial Index (ABI)
Abstract
:1. Introduction
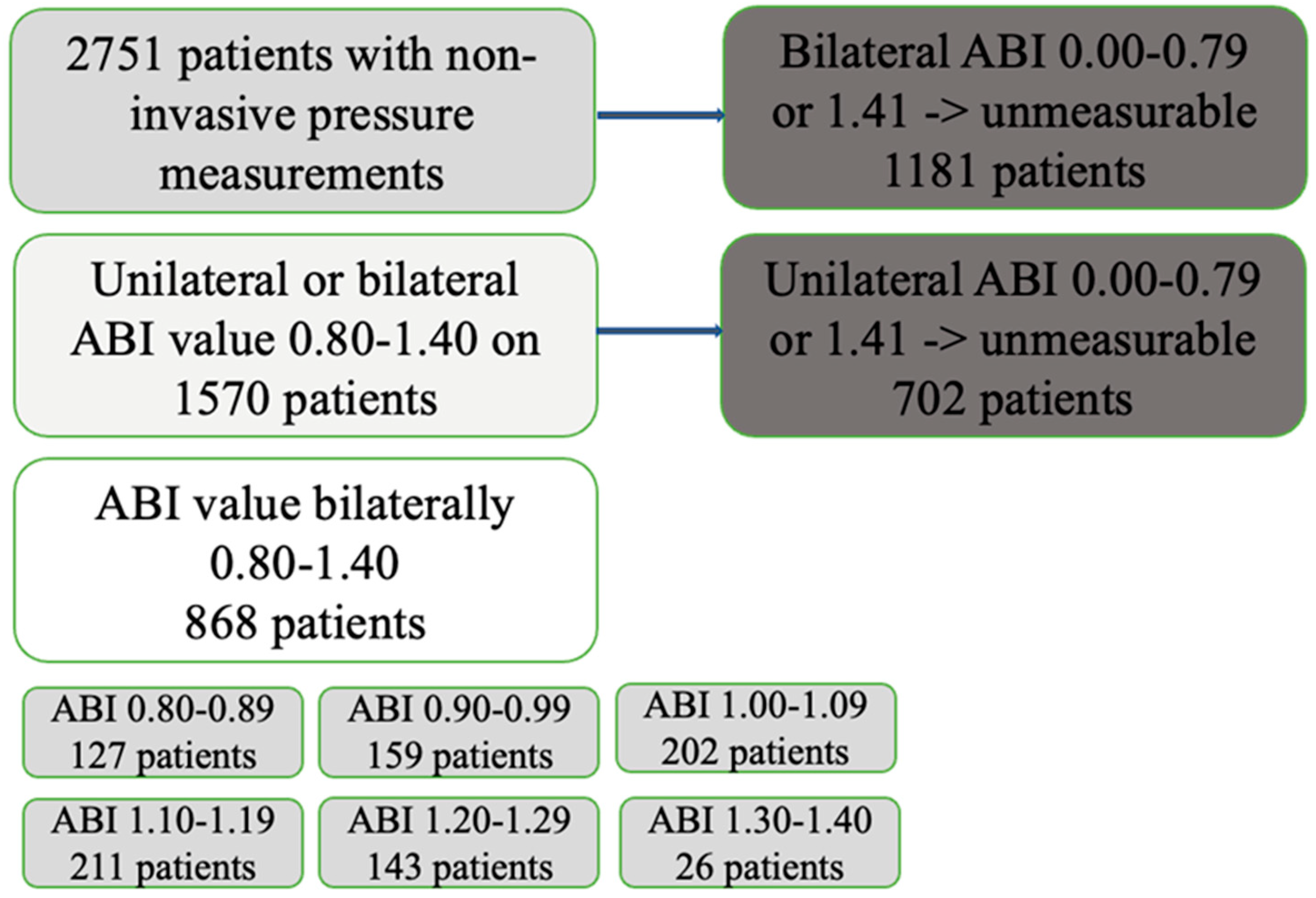
2. Materials and Methods
2.1. Non-Invasive Pressure Measurements
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Study Cohort and Demography
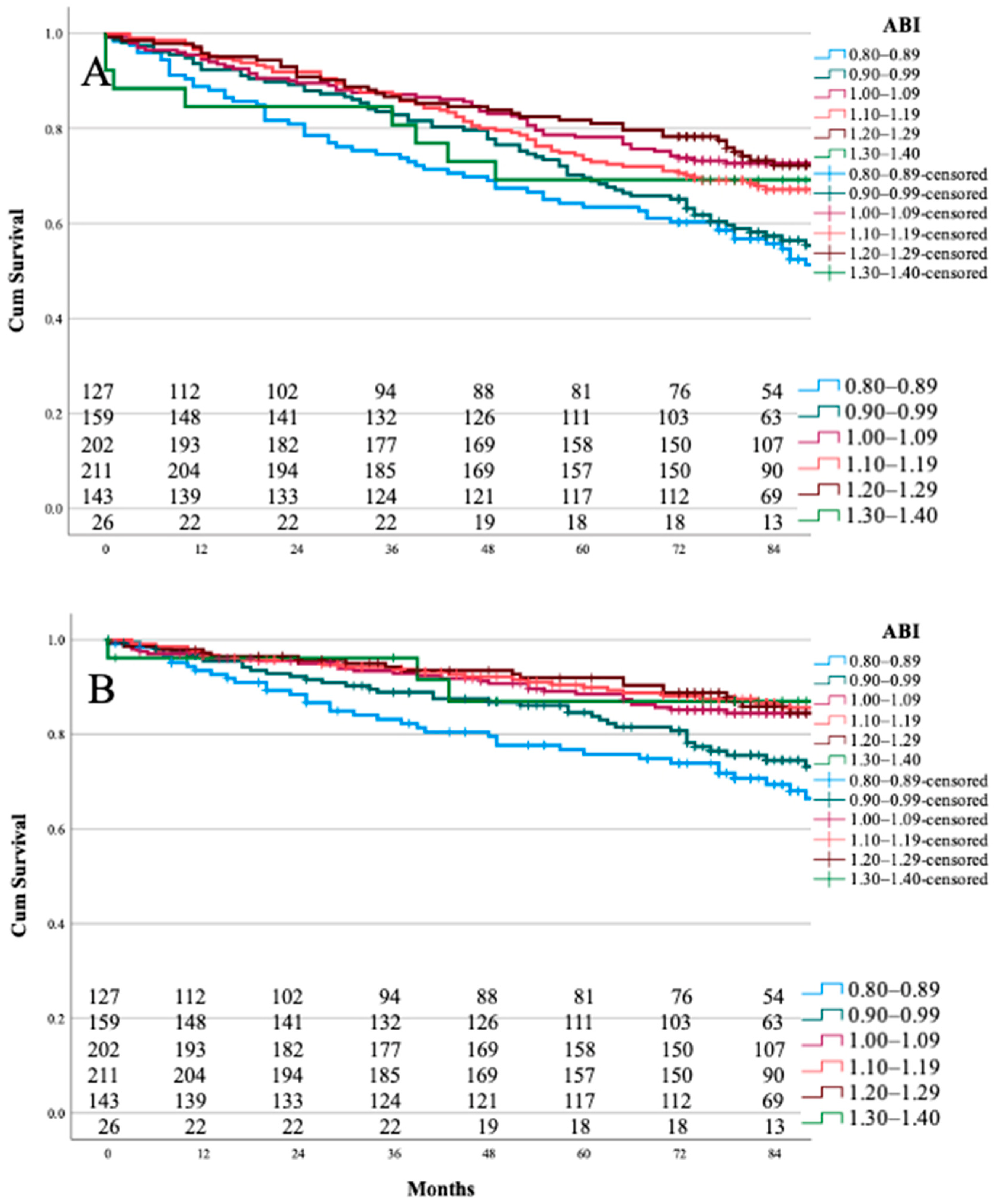
3.2. ABI Range Category and Survival
3.3. TBI and Toe Pressure Values
4. Discussion
4.1. Normal Range for ABI
4.2. Normal TBI
4.3. Normal TP
4.4. Strengths and Limitations
5. Conclusions
6. Patients
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update from the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Aboyans, V.; Ricco, J.B.; Bartelink, M.E.L.; Bjorck, M.; Brodmann, M.; Cohnert, T. Editor’s Choice-2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur. J. Vasc. Endovasc. Surg. 2018, 55, 305–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aboyans, V.; Criqui, M.H.; Abraham, P.; Allison, M.A.; Creager, M.A.; Diehm, C.; Fowkes, F.G.R.; Hiatt, W.R.; Jönsson, B.; Lacroix, P.; et al. Measurement and interpretation of the ankle-brachial index: A scientific statement from the American Heart Association. Circulation 2012, 126, 2890–2909. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerhard-Herman, M.D.; Gornik, H.L.; Barrett, C.; Barshes, N.R.; Corriere, M.A.; Drachman, D.E.; Fleisher, L.A.; Fowkes, F.G.R.; Hamburg, N.M.; Kinlay, S.; et al. 2016 AHA/ACC Guideline on the Management of Patients with Lower Extremity Peripheral Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2017, 135, e726–e779. [Google Scholar]
- Norgren, L.; Hiatt, W.R.; Dormandy, J.A.; Nehler, M.R.; Harris, K.A.; Fowkes, F.G.R. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J. Vasc. Surg. 2007, 45, S5–S67. [Google Scholar] [CrossRef] [Green Version]
- Norgren, L.; Hiatt, W.R.; Dormandy, J.A.; Nehler, M.R.; Harris, K.A.; Fowkes, F.G.; TASC II Working Group; Bell, K.; Caporusso, J.; Durand-Zaleski, I.; et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur. J. Vasc. Endovasc. Surg. 2007, 33, S1–S75. [Google Scholar] [CrossRef] [Green Version]
- Ankle Brachial Index Collaboration. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: A meta-analysis. JAMA 2008, 300, 197–208. [Google Scholar] [CrossRef] [Green Version]
- Criqui, M.H.; McClelland, R.L.; McDermott, M.M.; Allison, M.; Blumenthal, R.S.; Aboyans, V.; Ix, J.H.; Burke, G.L.; Liu, K.; Shea, S. The ankle-brachial index and incident cardiovascular events in the MESA (Multi-Ethnic Study of Atherosclerosis). J. Am. Coll. Cardiol. 2010, 56, 1506–1512. [Google Scholar] [CrossRef]
- Wickström, J.-E.; Laivuori, M.; Aro, E.; Sund, R.; Hautero, O.; Venermo, M.; Jalkanen, J.; Hakovirta, H. Toe Pressure and Toe Brachial Index are Predictive of Cardiovascular Mortality, Overall Mortality, and Amputation Free Survival in Patients with Peripheral Artery Disease. Eur. J. Vasc. Endovasc. Surg. 2017, 53, 696–703. [Google Scholar] [CrossRef] [Green Version]
- Wickström, J.-E.; Virtanen, J.; Laivuori, M.; Jalkanen, J.; Venermo, M.; Hakovirta, H. Data on association of ankle pressure and ankle brachial index of symptomatic and contralateral lower extremities with overall and cardiovascular mortality in patients with lower extremity peripheral artery disease. Data Brief 2018, 20, 691–697. [Google Scholar] [CrossRef]
- Laivuori, M.; Hakovirta, H.; Kauhanen, P.; Sinisalo, J.; Sund, R.; Albäck, A.; Venermo, M. Toe pressure should be part of a vascular surgeon’s first-line investigation in the assessment of lower extremity artery disease and cardiovascular risk of a patient. J. Vasc. Surg. 2020, 73, 641–649. [Google Scholar] [CrossRef]
- Jalkanen, J.M.; Wickstrom, J.E.; Venermo, M.; Hakovirta, H.H. Data on amputation free survival of patients with lower limb peripheral artery disease classified according TASC II classification and a new crural index. Data Brief 2016, 8, 242–246. [Google Scholar] [CrossRef] [Green Version]
- Hyun, S.; Forbang, N.I.; Allison, M.A.; Denenberg, J.O.; Criqui, M.H.; Ix, J.H. Ankle-brachial index, toe-brachial index, and cardiovascular mortality in persons with and without diabetes mellitus. J. Vasc. Surg. 2014, 60, 390–395. [Google Scholar] [CrossRef] [Green Version]
- Korhonen, P.; Aarnio, P. Borderline peripheral arterial disease. Int. J. Angiol. 2008, 17, 175–177. [Google Scholar] [CrossRef] [Green Version]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; De Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 73, e285–e350. [Google Scholar] [CrossRef]
- Rooke, T.W.; Hirsch, A.T.; Misra, S.; Sidawy, A.N.; Beckman, J.; Findeiss, L.K.; Golzarian, J.; Gornik, H.L.; Halperin, J.L.; Jaff, M.R.; et al. 2011 ACCF/AHA Focused update of the guideline for the management of patients with peripheral artery disease (updating the 2005 guideline): A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Developed in Collaboration With the Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society for Vascular Medicine, and Society for Vascular Surgery. J. Vasc. Surg. 2011, 54, e32–e58. [Google Scholar] [CrossRef] [Green Version]
- Miura, T.; Minamisawa, M.; Ueki, Y.; Abe, N.; Nishimura, H.; Hashizume, N.; Mochidome, T.; Harada, M.; Oguchi, Y.; Yoshie, K.; et al. Impressive predictive value of ankle-brachial index for very long-term outcomes in patients with cardiovascular disease: IMPACT-ABI study. PLoS ONE 2017, 12, e0177609. [Google Scholar] [CrossRef] [Green Version]
- Tanaka, S.; Kaneko, H.; Kano, H.; Matsuno, S.; Suzuki, S.; Takai, H.; Otsuka, T.; Uejima, T.; Oikawa, Y.; Nagashima, K.; et al. The predictive value of the borderline ankle-brachial index for long-term clinical outcomes: An observational cohort study. Atherosclerosis 2016, 250, 69–76. [Google Scholar] [CrossRef] [Green Version]
- Papamichael, C.M.; Lekakis, J.P.; Stamatelopoulos, K.S.; Papaioannou, T.G.; Alevizaki, M.K.; Cimponeriu, A.T.; Kanakakis, J.E.; Papapanagiotou, A.; Kalofoutis, A.T.; Stamatelopoulos, S.F. Ankle-brachial index as a predictor of the extent of coronary atherosclerosis and cardiovascular events in patients with coronary artery disease. Am. J. Cardiol. 2000, 86, 615–618. [Google Scholar] [CrossRef]
- Finland, S. Statistics Finland-Quality Description: Causes of Death 2013. Available online: http://www.stat.fi/til/ksyyt/2013/ksyyt_2013_2014-12-30_laa_001_en.html (accessed on 30 September 2019).
- Alzamora, M.T.; Fores, R.; Pera, G.; Baena-Diez, J.M.; Valverde, M.; Toran, P. Low, borderline and normal ankle-brachial index as a predictor of incidents outcomes in the Mediterranean based-population ARTPER cohort after 9 years follow-up. PLoS ONE 2019, 14, e0209163. [Google Scholar] [CrossRef] [Green Version]
- O’Hare, A.M.; Katz, R.; Shlipak, M.G.; Cushman, M.; Newman, A.B. Mortality and cardiovascular risk across the ankle-arm index spectrum: Results from the Cardiovascular Health Study. Circulation 2006, 113, 388–393. [Google Scholar] [CrossRef] [Green Version]
- Alves, L.; Comas-Cufí, M.; Ponjoan, A.; Garcia-Gil, M.; Martí-Lluch, R.; Blanch, J.; Elosua-Bayes, M.; Parramon, D.; Camós, L.; Guzmán, L.E.; et al. Levels of ankle–brachial index and the risk of diabetes mellitus complications. BMJ Open Diabetes Res. Care 2020, 8, e000977. [Google Scholar] [CrossRef] [Green Version]
- Visonà, A.; De Paoli, A.; Fedeli, U.; Tonello, D.; Zalunardo, B.; Zanatta, N.; Martini, R.; Pesavento, R.; Cuppini, S.; Prior, M.; et al. Abnormal ankle-brachial index (ABI) predicts primary and secondary cardiovascular risk and cancer mortality. Eur. J. Intern. Med. 2020, 77, 79–85. [Google Scholar] [CrossRef]
- Hoek, A.G.; Zwakenberg, S.R.; Elders, P.J.; de Jong, P.A.; Spiering, W.; Bartstra, J.W.; Doesburg, T.; van der Heijden, A.A.; van der Schouw, Y.T.; Beulens, J.W.; et al. An elevated ankle-brachial index is not a valid proxy for peripheral medial arterial calcification. Atherosclerosis 2021, 323, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Carter, S.A.; Lezack, J.D. Digital systolic pressures in the lower limb in arterial disease. Circulation 1971, 43, 905–914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Darban Hosseini Amirkhiz, G.; Babaei, M.R.; Madani, N.H.; Khamseh, M.E. Toe-brachial index is beyond a peripheral issue in patients with type 2 diabetes. PLoS ONE 2021, 16, e0253138. [Google Scholar]
| ABI 0.80–1.40 (n = 868) | |
|---|---|
| mean (SD) | |
| Age | 67.9 |
| n (%) | |
| Sex male | 505 (58.2) |
| CAD | 236 (27.2) |
| CHF | 148 (17.1) |
| HT | 466 (53.7) |
| FA | 204 (23.5) |
| CeVD | 103 (11.9) |
| DM | 297 (34.2) |
| DMI | 58 (6.7) |
| DMII | 239 (27.6) |
| Dyslipidaemia | 195 (22.5) |
| CKD | 106 (12.2) |
| COPD | 87 (10.0) |
| Rheumatoid disease | 61 (7.0) |
| Varicose Ulcer | 97 (11.2) |
| CV death | 160 (18.4) |
| ABI Range Categories | |||||||
|---|---|---|---|---|---|---|---|
| 0.80–0.89 | 0.90–0.99 | 1.00–1.09 | 1.10–1.19 | 1.20–1.29 | 1.30–1.40 | p value | |
| Mean | (SD) | ||||||
| Age | 70.8 (11.8) | 68.9 (15.2) | 68.11 (13.1) | 68.38 (13.5) | 64.2 (16.5) | 63.9 (15.0) | <0.001 |
| n | (%) | ||||||
| Sex male | 79 (62.29 | 85 (53.5) | 110 (54.5) | 120 (56.9) | 91 (63.6) | 20 (76.9) | 0.105 |
| CAD | 42 (33.1) | 57 (35.8) | 60 (29.7) | 48 (22.7) | 21 (14.7) | 8 (30.8) | <0.001 |
| CHF | 32 (25.2) | 31 (19.5) | 28 (13.9) | 33 (15.6) | 18 (12.6) | 6 (23.1) | 0.053 |
| HT | 68 (53.5) | 89 (56.0) | 111 (55.0) | 120 (56.9) | 69 (48.3) | 9 (34.6) | 0.238 |
| FA | 32 (25.2) | 36 (22.6) | 47 (23.3) | 53 (25.1) | 29 (20.3) | 7 (26.9) | 0.893 |
| CeVD | 16 (12.6) | 21 (13.2) | 21 (10.4) | 23 (10.9) | 18 (12.6) | 4 (15.4) | 0.904 |
| DM | 43 (33.9) | 63 (39.6) | 55 (27.2) | 68 (32.2) | 54 (37.8) | 14 (53.8) | 0.034 |
| DMI | 7 (5.5) | 12 (7.5) | 14 (6.9) | 13 (6.2) | 9 (6.3) | 3 (11.5) | 0.867 |
| DMII | 37 (29.1) | 50 (31.4) | 42 (20.8) | 55 (26.1) | 45 (31.5) | 11 (42.3) | 0.065 |
| Dyslipidaemia | 35 (27.8) | 44 (27.7) | 40 (19.8) | 38 (18.0) | 36 (25.2) | 2 (7.7) | 0.039 |
| CKD | 19 (15.0) | 21 (13.2) | 22 (10.9) | 26 (12.3) | 14 (9.8) | 4 (15.4) | 0.759 |
| COPD | 24 (18.9) | 22 (13.8) | 18 (8.9) | 14 (6.6) | 6 (4.2) | 3 (11.3) | <0.001 |
| Rheumatoid disease | 5 (3.9) | 9 (5.7) | 17 (8.4) | 13 (6.2) | 14 (9.8) | 3 (11.5) | 0.302 |
| Varicose Ulcer | 11 (8.7) | 14 (8.8) | 31 (15.3) | 26 (12.3) | 13 (9.1) | 2 (7.7) | 0.312 |
| CV death | 39 (30.7) | 41 (25.8) | 31 (15.3) | 27 (12.8) | 19 (13.3) | 3 (11.5) | <0.001 |
| A | Mean Survival | Mean CVDFS | ||||
| ABI | Months (SE) | p Value | p Value | Months (SE) | p Value | p Value |
| 0.80–0.89 | 73.0 (3.47) | reference | 0.393 | 84.2 (3.25) | reference | 0.264 |
| 0.90–0.99 | 78.8 (2.76) | 0.393 | reference | 90.0 (2.49) | 0.264 | reference |
| 1.00–1.09 | 87.8 (2.36) | <0.001 | <0.001 | 96.2 (1.91) | <0.001 | 0.013 |
| 1.10–1.19 | 85.1 (2.28) | 0.003 | 0.030 | 97.6 (1.77) | <0.001 | 0.003 |
| 1.20–1.29 | 89.4 (2.65) | <0.001 | <0.001 | 98.0 (2.06) | <0.001 | 0.006 |
| 1.30–1.40 | 80.9 (7.97) | 0.156 | 0.280 | 96.8 (5.57) | 0.071 | 0.176 |
| B | Survival | CVDFS | ||||
| ABI | 1-year | 3-year | 5-year | 1-year | 3-year | 5-year |
| 0.80–0.89 | 81% | 70% | 41% | 88% | 80% | 57% |
| 0.90–0.99 | 89% | 80% | 44% | 92% | 88% | 62% |
| 1.00–1.09 | 90% | 84% | 65% | 95% | 91% | 79% |
| 1.10–1.19 | 92% | 80% | 60% | 96% | 92% | 82% |
| 1.20–1.29 | 93% | 85% | 67% | 96% | 93% | 80% |
| 1.30–1.40 | 85% | 73% | 69% | 96% | 87% | 87% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peltonen, E.; Laivuori, M.; Vakhitov, D.; Korhonen, P.; Venermo, M.; Hakovirta, H. The Cardiovascular-Mortality-Based Estimate for Normal Range of the Ankle–Brachial Index (ABI). J. Cardiovasc. Dev. Dis. 2022, 9, 147. https://doi.org/10.3390/jcdd9050147
Peltonen E, Laivuori M, Vakhitov D, Korhonen P, Venermo M, Hakovirta H. The Cardiovascular-Mortality-Based Estimate for Normal Range of the Ankle–Brachial Index (ABI). Journal of Cardiovascular Development and Disease. 2022; 9(5):147. https://doi.org/10.3390/jcdd9050147
Chicago/Turabian StylePeltonen, Essi, Mirjami Laivuori, Damir Vakhitov, Päivi Korhonen, Maarit Venermo, and Harri Hakovirta. 2022. "The Cardiovascular-Mortality-Based Estimate for Normal Range of the Ankle–Brachial Index (ABI)" Journal of Cardiovascular Development and Disease 9, no. 5: 147. https://doi.org/10.3390/jcdd9050147
APA StylePeltonen, E., Laivuori, M., Vakhitov, D., Korhonen, P., Venermo, M., & Hakovirta, H. (2022). The Cardiovascular-Mortality-Based Estimate for Normal Range of the Ankle–Brachial Index (ABI). Journal of Cardiovascular Development and Disease, 9(5), 147. https://doi.org/10.3390/jcdd9050147






