Tachyarrhythmias in Congenital Heart Diseases: From Ion Channels to Catheter Ablation
Abstract
1. Introduction
2. Arrhythmias Pathophysiology and Genesis in Congenital Heart Disease
2.1. Substrates for Arrhythmias in Congenital Heart Disease
2.1.1. Congenital Heart Disease-Related Substrate
2.1.2. Post-Operative Substrate
2.1.3. Cardiovascular Risk-Related Substrate
2.1.4. Genetic Substrate
2.2. Triggers for Arrhythmias in Congenital Heart Diseases
2.2.1. Abnormal Automaticity and Triggered Activity
2.2.2. Hemodynamic Alterations
2.2.3. Myocardial Ischemia
2.3. Modulators for Arrhythmias in Congenital Heart Diseases
2.3.1. Neurohormonal Perturbations
2.3.2. Chronic Inflammation
3. Management of Arrhythmias in Congenital Heart Disease
3.1. Arrhythmia Diagnosis
3.2. Medical Therapy
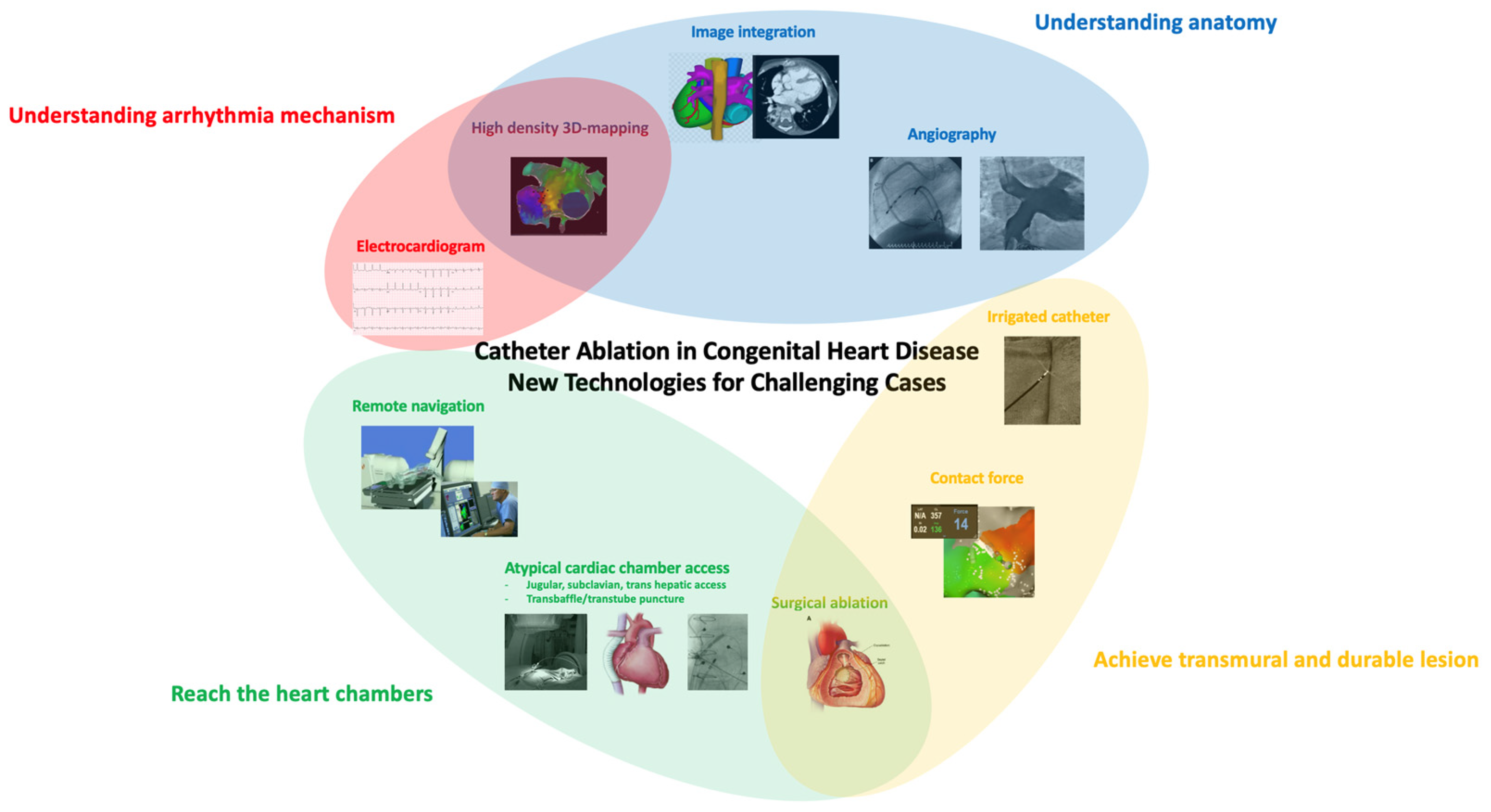
3.3. Catheter Ablation
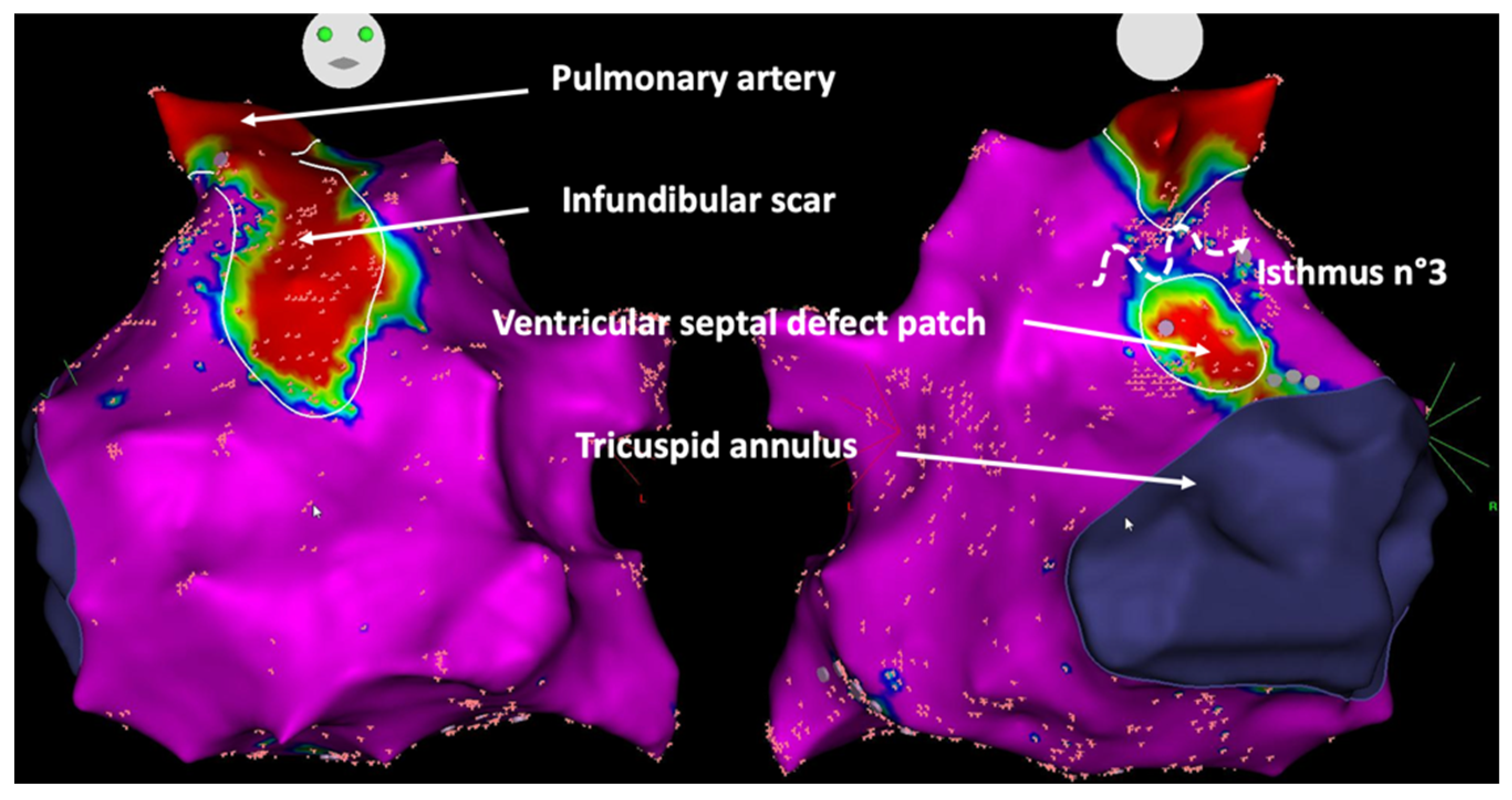
3.3.1. Current Approaches and Outcomes
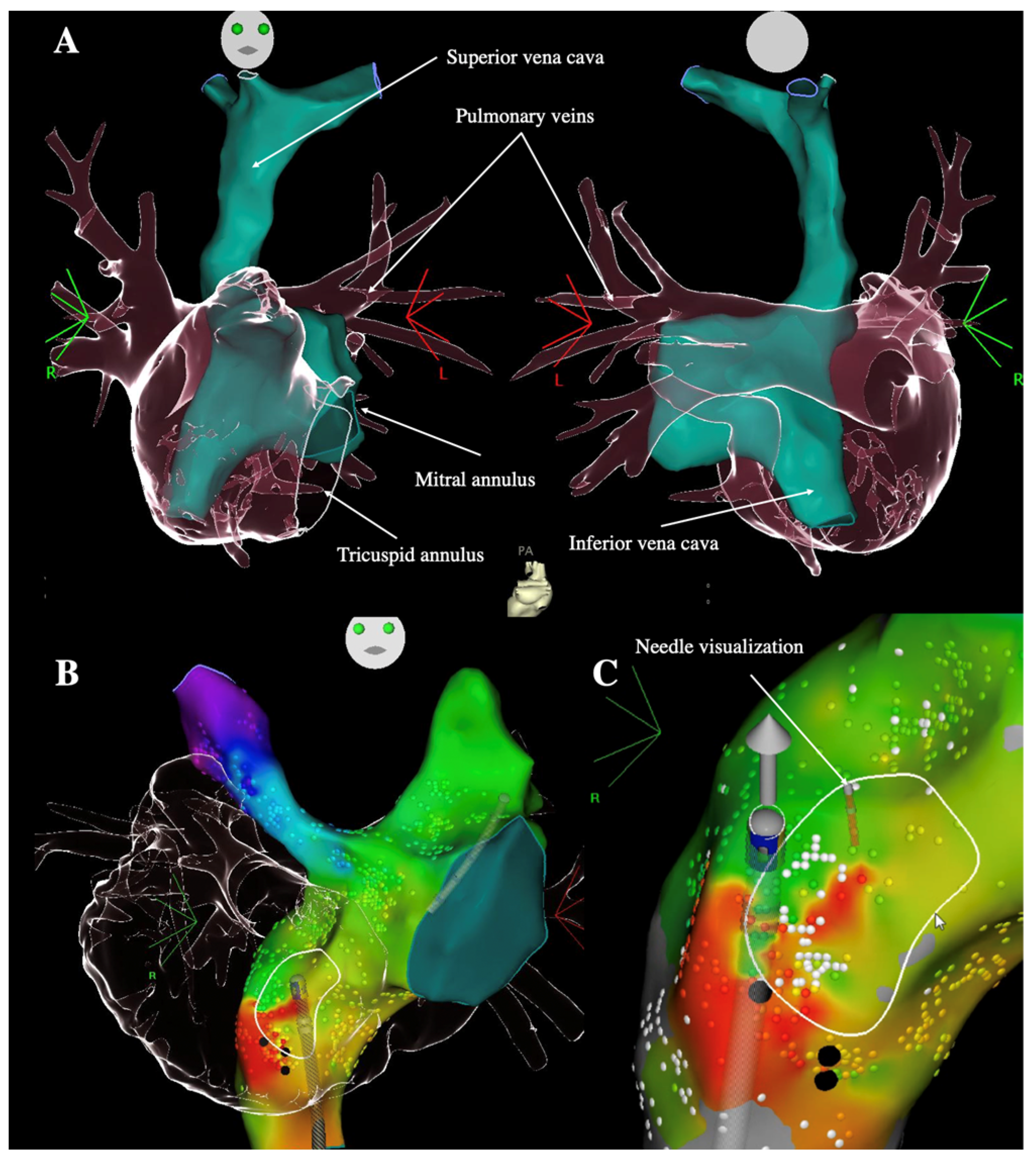
3.3.2. Technical Challenges to Reach Heart Chambers
3.3.3. Perioperative Evaluation of Arrhythmias
3.3.4. Atrial Fibrillation
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Marelli, A.J.; Mackie, A.S.; Ionescu-Ittu, R.; Rahme, E.; Pilote, L. Congenital Heart Disease in the General Population: Changing Prevalence and Age Distribution. Circulation 2007, 115, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Bouchardy, J.; Therrien, J.; Pilote, L.; Ionescu-Ittu, R.; Martucci, G.; Bottega, N.; Marelli, A.J. Atrial Arrhythmias in Adults with Congenital Heart Disease. Circulation 2009, 120, 1679–1686. [Google Scholar] [CrossRef]
- Upadhyay, S.; Marie Valente, A.; Triedman, J.K.; Walsh, E.P. Catheter Ablation for Atrioventricular Nodal Reentrant Tachycardia in Patients with Congenital Heart Disease. Heart Rhythm 2016, 13, 1228–1237. [Google Scholar] [CrossRef] [PubMed]
- Papagiannis, J.; Beissel, D.J.; Krause, U.; Cabrera, M.; Telishevska, M.; Seslar, S.; Johnsrude, C.; Anderson, C.; Tisma-Dupanovic, S.; Connelly, D.; et al. Atrioventricular Nodal Reentrant Tachycardia in Patients With Congenital Heart Disease: Outcome After Catheter Ablation. Circ. Arrhythm. Electrophysiol. 2017, 10, e004869. [Google Scholar] [CrossRef] [PubMed]
- Walsh, E.P.; Cecchin, F. Arrhythmias in Adult Patients With Congenital Heart Disease. Circulation 2007, 115, 534–545. [Google Scholar] [CrossRef] [PubMed]
- Walsh, E.P. Ebstein’s Anomaly of the Tricuspid Valve: A Natural Laboratory for Re-Entrant Tachycardias. JACC Clin. Electrophysiol. 2018, 4, 1271–1288. [Google Scholar] [CrossRef]
- Khairy, P.; Fournier, A.; Dubuc, M. Mönckeberg’s Sling. Can. J. Cardiol. 2003, 19, 717–718. [Google Scholar]
- Bessière, F.; Mongeon, F.-P.; Therrien, J.; Khairy, P. Magnetic-Guided Catheter Ablation of Twin AV Nodal Reentrant Tachycardia in a Patient with Left Atrial Isomerism, Interrupted Inferior Vena Cana, and Kawashima-Fontan Procedure. Clin. Case Rep. 2017, 5, 2105–2110. [Google Scholar] [CrossRef]
- Lukac, P.; Pedersen, A.K.; Mortensen, P.T.; Jensen, H.K.; Hjortdal, V.; Hansen, P.S. Ablation of Atrial Tachycardia after Surgery for Congenital and Acquired Heart Disease Using an Electroanatomic Mapping System: Which Circuits to Expect in Which Substrate? Heart Rhythm 2005, 2, 64–72. [Google Scholar] [CrossRef]
- Kapel, G.F.L.; Sacher, F.; Dekkers, O.M.; Watanabe, M.; Blom, N.A.; Thambo, J.-B.; Derval, N.; Schalij, M.J.; Jalal, Z.; Wijnmaalen, A.P.; et al. Arrhythmogenic Anatomical Isthmuses Identified by Electroanatomical Mapping Are the Substrate for Ventricular Tachycardia in Repaired Tetralogy of Fallot. Eur. Heart J. 2017, 38, 268–276. [Google Scholar] [CrossRef]
- Hager, A.; Zrenner, B.; Brodherr-Heberlein, S.; Steinbauer-Rosenthal, I.; Schreieck, J.; Hess, J. Congenital and Surgically Acquired Wolff-Parkinson-White Syndrome in Patients with Tricuspid Atresia. J. Thorac. Cardiovasc. Surg. 2005, 130, 48–53. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Labombarda, F.; Hamilton, R.; Shohoudi, A.; Aboulhosn, J.; Broberg, C.S.; Chaix, M.A.; Cohen, S.; Cook, S.; Dore, A.; Fernandes, S.M.; et al. Increasing Prevalence of Atrial Fibrillation and Permanent Atrial Arrhythmias in Congenital Heart Disease. J. Am. Coll. Cardiol. 2017, 70, 857–865. [Google Scholar] [CrossRef] [PubMed]
- Rienstra, M.; Hobbelt, A.H.; Alings, M.; Tijssen, J.G.P.; Smit, M.D.; Brügemann, J.; Geelhoed, B.; Tieleman, R.G.; Hillege, H.L.; Tukkie, R.; et al. Targeted Therapy of Underlying Conditions Improves Sinus Rhythm Maintenance in Patients with Persistent Atrial Fibrillation: Results of the RACE 3 Trial. Eur. Heart J. 2018, 39, 2987–2996. [Google Scholar] [CrossRef] [PubMed]
- Pierpont, M.E.; Brueckner, M.; Chung, W.K.; Garg, V.; Lacro, R.V.; McGuire, A.L.; Mital, S.; Priest, J.R.; Pu, W.T.; Roberts, A.; et al. Genetic Basis for Congenital Heart Disease: Revisited: A Scientific Statement From the American Heart Association. Circulation 2018, 138, e653–e711. [Google Scholar] [CrossRef] [PubMed]
- Maury, P.; Gandjbakhch, E.; Baruteau, A.-E.; Bessière, F.; Kyndt, F.; Bouvagnet, P.; Rollin, A.; Bonnet, D.; Probst, V.; Maltret, A. Cardiac Phenotype and Long-Term Follow-Up of Patients With Mutations in NKX2-5 Gene. J. Am. Coll. Cardiol. 2016, 68, 2389–2390. [Google Scholar] [CrossRef]
- Gros, D.; Dupays, L.; Alcoléa, S.; Meysen, S.; Miquerol, L.; Théveniau-Ruissy, M. Genetically Modified Mice: Tools to Decode the Functions of Connexins in the Heart-New Models for Cardiovascular Research. Cardiovasc. Res. 2004, 62, 299–308. [Google Scholar] [CrossRef]
- Antzelevitch, C.; Burashnikov, A. Overview of Basic Mechanisms of Cardiac Arrhythmia. Card. Electrophysiol. Clin. 2011, 3, 23–45. [Google Scholar] [CrossRef]
- Nattel, S.; Harada, M. Atrial Remodeling and Atrial Fibrillation: Recent Advances and Translational Perspectives. J. Am. Coll. Cardiol. 2014, 63, 2335–2345. [Google Scholar] [CrossRef]
- Seslar, S.P.; Alexander, M.E.; Berul, C.I.; Cecchin, F.; Walsh, E.P.; Triedman, J.K. Ablation of Nonautomatic Focal Atrial Tachycardia in Children and Adults with Congenital Heart Disease. J. Cardiovasc. Electrophysiol. 2006, 17, 359–365. [Google Scholar] [CrossRef]
- Klehs, S.; Schneider, H.E.; Backhoff, D.; Paul, T.; Krause, U. Radiofrequency Catheter Ablation of Atrial Tachycardias in Congenital Heart Disease: Results With Special Reference to Complexity of Underlying Anatomy. Circ. Arrhythm. Electrophysiol. 2017, 10, e005451. [Google Scholar] [CrossRef]
- Klein, R.C. Ventricular Arrhythmias in Aortic Valve Disease: Analysis of 102 Patients. Am. J. Cardiol. 1984, 53, 1079–1083. [Google Scholar] [CrossRef]
- Cohle, S.D.; Balraj, E.; Bell, M. Sudden Death Due to Ventricular Septal Defect. Pediatr. Dev. Pathol. 1999, 2, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Ueda, A.; Adachi, I.; McCarthy, K.P.; Li, W.; Ho, S.Y.; Uemura, H. Substrates of Atrial Arrhythmias: Histological Insights from Patients with Congenital Heart Disease. Int. J. Cardiol. 2013, 168, 2481–2486. [Google Scholar] [CrossRef] [PubMed]
- Deal, B.J.; Costello, J.M.; Webster, G.; Tsao, S.; Backer, C.L.; Mavroudis, C. Intermediate-Term Outcome of 140 Consecutive Fontan Conversions With Arrhythmia Operations. Ann. Thorac. Surg. 2016, 101, 717–724. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Karam, N.; Bataille, S.; Marijon, E.; Giovannetti, O.; Tafflet, M.; Savary, D.; Benamer, H.; Caussin, C.; Garot, P.; Juliard, J.-M.; et al. Identifying Patients at Risk for Prehospital Sudden Cardiac Arrest at the Early Phase of Myocardial Infarction: The e-MUST Study (Evaluation En Médecine d’Urgence Des Stratégies Thérapeutiques Des Infarctus Du Myocarde). Circulation 2016, 134, 2074–2083. [Google Scholar] [CrossRef] [PubMed]
- Ou, P.; Khraiche, D.; Celermajer, D.S.; Agnoletti, G.; Sang, K.-H.L.Q.; Thalabard, J.C.; Quintin, M.; Raisky, O.; Vouhe, P.; Sidi, D.; et al. Mechanisms of Coronary Complications after the Arterial Switch for Transposition of the Great Arteries. J. Thorac. Cardiovasc. Surg. 2013, 145, 1263–1269. [Google Scholar] [CrossRef] [PubMed]
- Millane, T.; Bernard, E.J.; Jaeggi, E.; Howman-Giles, R.B.; Uren, R.F.; Cartmill, T.B.; Hawker, R.E.; Celermajer, D.S. Role of Ischemia and Infarction in Late Right Ventricular Dysfunction after Atrial Repair of Transposition of the Great Arteries. J. Am. Coll. Cardiol. 2000, 35, 1661–1668. [Google Scholar] [CrossRef]
- Khairy, P. Sudden Cardiac Death in Transposition of the Great Arteries with a Mustard or Senning Baffle: The Myocardial Ischemia Hypothesis. Curr. Opin. Cardiol. 2017, 32, 101–107. [Google Scholar] [CrossRef]
- Chaix, M.-A.; Chergui, M.; Leduc, C.; Khairy, P. Sudden Death in Transposition of the Great Arteries with Atrial Switch Surgery: Autopsy Evidence of Acute Myocardial Ischemia despite Normal Coronary Arteries. Int. J. Cardiol. 2019, 288, 65–67. [Google Scholar] [CrossRef]
- Giannakoulas, G.; Dimopoulos, K.; Engel, R.; Goktekin, O.; Kucukdurmaz, Z.; Vatankulu, M.A.; Bedard, E.; Diller, G.P.; Papaphylactou, M.; Francis, D.P.; et al. Burden of Coronary Artery Disease in Adults with Congenital Heart Disease and Its Relation to Congenital and Traditional Heart Risk Factors. Am. J. Cardiol. 2009, 103, 1445–1450. [Google Scholar] [CrossRef] [PubMed]
- Olsen, M.; Marino, B.; Kaltman, J.; Laursen, H.; Jakobsen, L.; Mahle, W.; Pearson, G.; Madsen, N. Myocardial Infarction in Adults With Congenital Heart Disease. Am. J. Cardiol. 2017, 120, 2272–2277. [Google Scholar] [CrossRef] [PubMed]
- Shen, M.J.; Zipes, D.P. Role of the Autonomic Nervous System in Modulating Cardiac Arrhythmias. Circ. Res. 2014, 114, 1004–1021. [Google Scholar] [CrossRef] [PubMed]
- Bolger, A.P.; Sharma, R.; Li, W.; Leenarts, M.; Kalra, P.R.; Kemp, M.; Coats, A.J.S.; Anker, S.D.; Gatzoulis, M.A. Neurohormonal Activation and the Chronic Heart Failure Syndrome in Adults with Congenital Heart Disease. Circulation 2002, 106, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Everett, B.M.; Thuren, T.; MacFadyen, J.G.; Chang, W.H.; Ballantyne, C.; Fonseca, F.; Nicolau, J.; Koenig, W.; Anker, S.D.; et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N. Engl. J. Med. 2017, 377, 1119–1131. [Google Scholar] [CrossRef] [PubMed]
- Opotowsky, A.R.; Valente, A.M.; Alshawabkeh, L.; Cheng, S.; Bradley, A.; Rimm, E.B.; Landzberg, M.J. Prospective Cohort Study of C-Reactive Protein as a Predictor of Clinical Events in Adults with Congenital Heart Disease: Results of the Boston Adult Congenital Heart Disease Biobank. Eur. Heart J. 2018, 39, 3253–3261. [Google Scholar] [CrossRef]
- Dodeja, A.K.; Thomas, C.; Daniels, C.J.; Kertesz, N.; Kamp, A. Detection of Arrhythmias in Adult Congenital Heart Disease Patients with LINQTM Implantable Loop Recorder. Congenit. Heart Dis. 2019, 14, 745–751. [Google Scholar] [CrossRef]
- Kobel, M.; Kalden, P.; Michaelis, A.; Markel, F.; Mensch, S.; Weidenbach, M.; Riede, F.T.; Löffelbein, F.; Bollmann, A.; Shamloo, A.S.; et al. Accuracy of the Apple Watch IECG in Children With and Without Congenital Heart Disease. Pediatr Cardiol 2022, 43, 191–196. [Google Scholar] [CrossRef]
- Khairy, P.; Landzberg, M.J.; Gatzoulis, M.A.; Lucron, H.; Lambert, J.; Marçon, F.; Alexander, M.E.; Walsh, E.P. Value of Programmed Ventricular Stimulation after Tetralogy of Fallot Repair: A Multicenter Study. Circulation 2004, 109, 1994–2000. [Google Scholar] [CrossRef]
- Baumgartner, H.; De Backer, J.; Babu-Narayan, S.V.; Budts, W.; Chessa, M.; Diller, G.-P.; Lung, B.; Kluin, J.; Lang, I.M.; Meijboom, F.; et al. 2020 ESC Guidelines for the Management of Adult Congenital Heart DiseaseThe Task Force for the Management of Adult Congenital Heart Disease of the European Society of Cardiology (ESC). Eur. Heart J. 2021, 42, 563–645. [Google Scholar] [CrossRef]
- Khairy, P.; Harris, L.; Landzberg, M.J.; Fernandes, S.M.; Barlow, A.; Mercier, L.-A.; Viswanathan, S.; Chetaille, P.; Gordon, E.; Dore, A.; et al. Sudden Death and Defibrillators in Transposition of the Great Arteries with Intra-Atrial Baffles: A Multicenter Study. Circ. Arrhythm. Electrophysiol. 2008, 1, 250–257. [Google Scholar] [CrossRef]
- Khairy, P.; Van Hare, G.F.; Balaji, S.; Berul, C.I.; Cecchin, F.; Cohen, M.I.; Daniels, C.J.; Deal, B.J.; Dearani, J.A.; de Groot, N.; et al. PACES/HRS Expert Consensus Statement on the Recognition and Management of Arrhythmias in Adult Congenital Heart Disease: Developed in Partnership between the Pediatric and Congenital Electrophysiology Society (PACES) and the Heart Rhythm Society (HRS). Endorsed by the Governing Bodies of PACES, HRS, the American College of Cardiology (ACC), the American Heart Association (AHA), the European Heart Rhythm Association (EHRA), the Canadian Heart Rhythm Society (CHRS), and the International Society for Adult Congenital Heart Disease (ISACHD). Heart Rhythm 2014, 11, e102–e165. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Madrid, A.; Paul, T.; Abrams, D.; Aziz, P.F.; Blom, N.A.; Chen, J.; Chessa, M.; Combes, N.; Dagres, N.; Diller, G.; et al. Arrhythmias in Congenital Heart Disease: A Position Paper of the European Heart Rhythm Association (EHRA), Association for European Paediatric and Congenital Cardiology (AEPC), and the European Society of Cardiology (ESC) Working Group on Grown-up Congenital Heart Disease, Endorsed by HRS, PACES, APHRS, and SOLAECE. Europace 2018, 20, 1719–1753. [Google Scholar] [CrossRef] [PubMed]
- Fish, F.A.; Gillette, P.C.; Benson, D.W. Proarrhythmia, Cardiac Arrest and Death in Young Patients Receiving Encainide and Flecainide. The Pediatric Electrophysiology Group. J. Am. Coll. Cardiol. 1991, 18, 356–365. [Google Scholar] [CrossRef]
- Pfammatter, J.P.; Paul, T.; Lehmann, C.; Kallfelz, H.C. Efficacy and Proarrhythmia of Oral Sotalol in Pediatric Patients. J. Am. Coll. Cardiol. 1995, 26, 1002–1007. [Google Scholar] [CrossRef]
- Thorne, S.A.; Barnes, I.; Cullinan, P.; Somerville, J. Amiodarone-Associated Thyroid Dysfunction: Risk Factors in Adults with Congenital Heart Disease. Circulation 1999, 100, 149–154. [Google Scholar] [CrossRef]
- El-Assaad, I.; Al-Kindi, S.G.; Abraham, J.; Sanatani, S.; Bradley, D.J.; Halsey, C.; Law, I.H.; Balaji, S.; Shetty, I.; Aziz, P.F. Use of Dofetilide in Adult Patients with Atrial Arrhythmias and Congenital Heart Disease: A PACES Collaborative Study. Heart Rhythm 2016, 13, 2034–2039. [Google Scholar] [CrossRef]
- Triedman, J.K.; Alexander, M.E.; Love, B.A.; Collins, K.K.; Berul, C.I.; Bevilacqua, L.M.; Walsh, E.P. Influence of Patient Factors and Ablative Technologies on Outcomes of Radiofrequency Ablation of Intra-Atrial Re-Entrant Tachycardia in Patients with Congenital Heart Disease. J. Am. Coll. Cardiol. 2002, 39, 1827–1835. [Google Scholar] [CrossRef]
- Waldmann, V.; Amet, D.; Zhao, A.; Ladouceur, M.; Otmani, A.; Karsenty, C.; Maltret, A.; Ollitrault, J.; Pontnau, F.; Legendre, A.; et al. Catheter Ablation in Adults with Congenital Heart Disease: A 15-Year Perspective from a Tertiary Centre. Arch Cardiovasc. Dis. 2021, 114, 455–464. [Google Scholar] [CrossRef]
- Be’eri, E.; Maier, S.E.; Landzberg, M.J.; Chung, T.; Geva, T. In Vivo Evaluation of Fontan Pathway Flow Dynamics by Multidimensional Phase-Velocity Magnetic Resonance Imaging. Circulation 1998, 98, 2873–2882. [Google Scholar] [CrossRef]
- Sherwin, E.D.; Triedman, J.K.; Walsh, E.P. Update on Interventional Electrophysiology in Congenital Heart Disease: Evolving Solutions for Complex Hearts. Circ. Arrhythm. Electrophysiol. 2013, 6, 1032–1040. [Google Scholar] [CrossRef]
- Combes, N.; Derval, N.; Hascoët, S.; Zhao, A.; Amet, D.; Le Bloa, M.; Maltret, A.; Heitz, F.; Thambo, J.-B.; Marijon, E. Ablation of Supraventricular Arrhythmias in Adult Congenital Heart Disease: A Contemporary Review. Arch. Cardiovasc. Dis. 2017, 110, 334–345. [Google Scholar] [CrossRef]
- Waldmann, V.; Amet, D.; Zhao, A.; Ladouceur, M.; Otmani, A.; Karsenty, C.; Maltret, A.; Soulat, G.; Mousseaux, E.; Lavergne, T.; et al. Catheter Ablation of Intra-Atrial Reentrant/Focal Atrial Tachycardia in Adult Congenital Heart Disease: Value of Final Programmed Atrial Stimulation. Heart Rhythm 2020, 17, 1953–1959. [Google Scholar] [CrossRef]
- Cappato, R.; Schlüter, M.; Weiss, C.; Antz, M.; Koschyk, D.H.; Hofmann, T.; Kuck, K.H. Radiofrequency Current Catheter Ablation of Accessory Atrioventricular Pathways in Ebstein’s Anomaly. Circulation 1996, 94, 376–383. [Google Scholar] [CrossRef] [PubMed]
- Roten, L.; Lukac, P.; DE Groot, N.; Nielsen, J.C.; Szili-Torok, T.; Jensen, H.K.; Zimmermann, M.; Delacrétaz, E. Catheter Ablation of Arrhythmias in Ebstein’s Anomaly: A Multicenter Study. J. Cardiovasc. Electrophysiol. 2011, 22, 1391–1396. [Google Scholar] [CrossRef] [PubMed]
- Laredo, M.; Frank, R.; Waintraub, X.; Gandjbakhch, E.; Iserin, L.; Hascoët, S.; Himbert, C.; Gallais, Y.; Hidden-Lucet, F.; Duthoit, G. Ten-Year Outcomes of Monomorphic Ventricular Tachycardia Catheter Ablation in Repaired Tetralogy of Fallot. Arch. Cardiovasc. Dis. 2017, 110, 292–302. [Google Scholar] [CrossRef]
- Ueda, A.; Suman-Horduna, I.; Mantziari, L.; Gujic, M.; Marchese, P.; Ho, S.Y.; Babu-Narayan, S.V.; Ernst, S. Contemporary Outcomes of Supraventricular Tachycardia Ablation in Congenital Heart Disease: A Single-Center Experience in 116 Patients. Circ. Arrhythm. Electrophysiol. 2013, 6, 606–613. [Google Scholar] [CrossRef]
- Laredo, M.; Waldmann, V.; Soulat, G.; Amet, D.; Marijon, E.; Iserin, L.; Ladouceur, M.; Zhao, A. Transbaffle/Transconduit Puncture Using a Simple CARTO-Guided Approach without Echocardiography in Patients with Congenital Heart Disease. J. Cardiovasc. Electrophysiol. 2020, 31, 2049–2060. [Google Scholar] [CrossRef] [PubMed]
- Guarguagli, S.; Cazzoli, I.; Kempny, A.; Gatzoulis, M.A.; Ernst, S. Initial Experience Using the Radiofrequency Needle Visualization on the Electroanatomical Mapping System for Transseptal Puncture. Cardiol. Res. Pract. 2020, 2020, 5420909. [Google Scholar] [CrossRef]
- Cuculich, P.S.; Schill, M.R.; Kashani, R.; Mutic, S.; Lang, A.; Cooper, D.; Faddis, M.; Gleva, M.; Noheria, A.; Smith, T.W.; et al. Noninvasive Cardiac Radiation for Ablation of Ventricular Tachycardia. N. Engl. J. Med. 2017, 377, 2325–2336. [Google Scholar] [CrossRef]
- Combes, N.; Bartoletti, S.; Heitz, F.; Waldmann, V. Critical Isthmus of Ventricular Tachycardia Covered by Transcatheter Pulmonary Valve in a Patient with Tetralogy of Fallot. Eur. Heart J. 2020, 41, 723. [Google Scholar] [CrossRef]
- Bouzas, B.; Kilner, P.J.; Gatzoulis, M.A. Pulmonary Regurgitation: Not a Benign Lesion. Eur. Heart J. 2005, 26, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Zeltser, I.; Gaynor, J.W.; Petko, M.; Myung, R.J.; Birbach, M.; Waibel, R.; Ittenbach, R.F.; Tanel, R.E.; Vetter, V.L.; Rhodes, L.A. The Roles of Chronic Pressure and Volume Overload States in Induction of Arrhythmias: An Animal Model of Physiologic Sequelae after Repair of Tetralogy of Fallot. J. Thorac. Cardiovasc. Surg. 2005, 130, 1542–1548. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Babu-Narayan, S.V.; Kilner, P.J.; Li, W.; Moon, J.C.; Goktekin, O.; Davlouros, P.A.; Khan, M.; Ho, S.Y.; Pennell, D.J.; Gatzoulis, M.A. Ventricular Fibrosis Suggested by Cardiovascular Magnetic Resonance in Adults with Repaired Tetralogy of Fallot and Its Relationship to Adverse Markers of Clinical Outcome. Circulation 2006, 113, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Bessière, F.; Gardey, K.; Bouzeman, A.; Duthoit, G.; Koutbi, L.; Labombarda, F.; Marquié, C.; Gourraud, J.B.; Mondoly, P.; Sellal, J.M.; et al. Impact of Pulmonary Valve Replacement on Ventricular Arrhythmias in Patients With Tetralogy of Fallot and Implantable Cardioverter-Defibrillator. JACC Clin. Electrophysiol. 2021, 7, 1285–1293. [Google Scholar] [CrossRef] [PubMed]
- Waldmann, V.; Laredo, M.; Abadir, S.; Mondésert, B.; Khairy, P. Atrial Fibrillation in Adults with Congenital Heart Disease. Int. J. Cardiol. 2019, 287, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.-Y.; Lo, L.-W.; Lin, Y.-J.; Chang, S.-L.; Hu, Y.-F.; Li, C.-H.; Chao, T.-F.; Chung, F.-P.; Ha, T.L.; Singhal, R.; et al. Long-Term Outcome of Catheter Ablation in Patients with Atrial Fibrillation Originating from Nonpulmonary Vein Ectopy. J. Cardiovasc. Electrophysiol. 2013, 24, 250–258. [Google Scholar] [CrossRef]
- Liang, J.J.; Frankel, D.S.; Parikh, V.; Lakkireddy, D.; Mohanty, S.; Burkhardt, J.D.; Natale, A.; Szilagyi, J.; Gerstenfeld, E.P.; Moore, J.P.; et al. Safety and Outcomes of Catheter Ablation for Atrial Fibrillation in Adults with Congenital Heart Disease: A Multicenter Registry Study. Heart Rhythm 2019, 16, 846–852. [Google Scholar] [CrossRef]
- De Groot, N.M.S.; Zeppenfeld, K.; Wijffels, M.C.; Chan, W.K.; Blom, N.A.; Van der Wall, E.E.; Schalij, M.J. Ablation of Focal Atrial Arrhythmia in Patients with Congenital Heart Defects after Surgery: Role of Circumscribed Areas with Heterogeneous Conduction. Heart Rhythm 2006, 3, 526–535. [Google Scholar] [CrossRef]


| Substrate and Trigger | Pathophysiology | Comments |
|---|---|---|
| CHD-related substrate |
|
|
| post-operative substrate |
|
|
| cardiovascular risk-related substrate |
|
|
| genetic substrate |
| |
| triggers for arrhythmias |
|
|
| Item | Management | Comments |
|---|---|---|
| diagnosis |
|
|
| medical therapy |
|
|
| catheter ablation |
|
|
| perioperative assessment |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Waldmann, V.; Guichard, J.-B.; Marijon, E.; Khairy, P. Tachyarrhythmias in Congenital Heart Diseases: From Ion Channels to Catheter Ablation. J. Cardiovasc. Dev. Dis. 2022, 9, 39. https://doi.org/10.3390/jcdd9020039
Waldmann V, Guichard J-B, Marijon E, Khairy P. Tachyarrhythmias in Congenital Heart Diseases: From Ion Channels to Catheter Ablation. Journal of Cardiovascular Development and Disease. 2022; 9(2):39. https://doi.org/10.3390/jcdd9020039
Chicago/Turabian StyleWaldmann, Victor, Jean-Baptiste Guichard, Eloi Marijon, and Paul Khairy. 2022. "Tachyarrhythmias in Congenital Heart Diseases: From Ion Channels to Catheter Ablation" Journal of Cardiovascular Development and Disease 9, no. 2: 39. https://doi.org/10.3390/jcdd9020039
APA StyleWaldmann, V., Guichard, J.-B., Marijon, E., & Khairy, P. (2022). Tachyarrhythmias in Congenital Heart Diseases: From Ion Channels to Catheter Ablation. Journal of Cardiovascular Development and Disease, 9(2), 39. https://doi.org/10.3390/jcdd9020039





