ICD Outcome in Pediatric Cardiomyopathies
Abstract
:1. Introduction
2. Materials and Methods
2.1. Indications for ICD Implantation
2.2. Implantation Procedure, ICD, and Leads
2.3. Follow-Up
2.4. Statystical Analysis
3. Results
3.1. ICD Programming
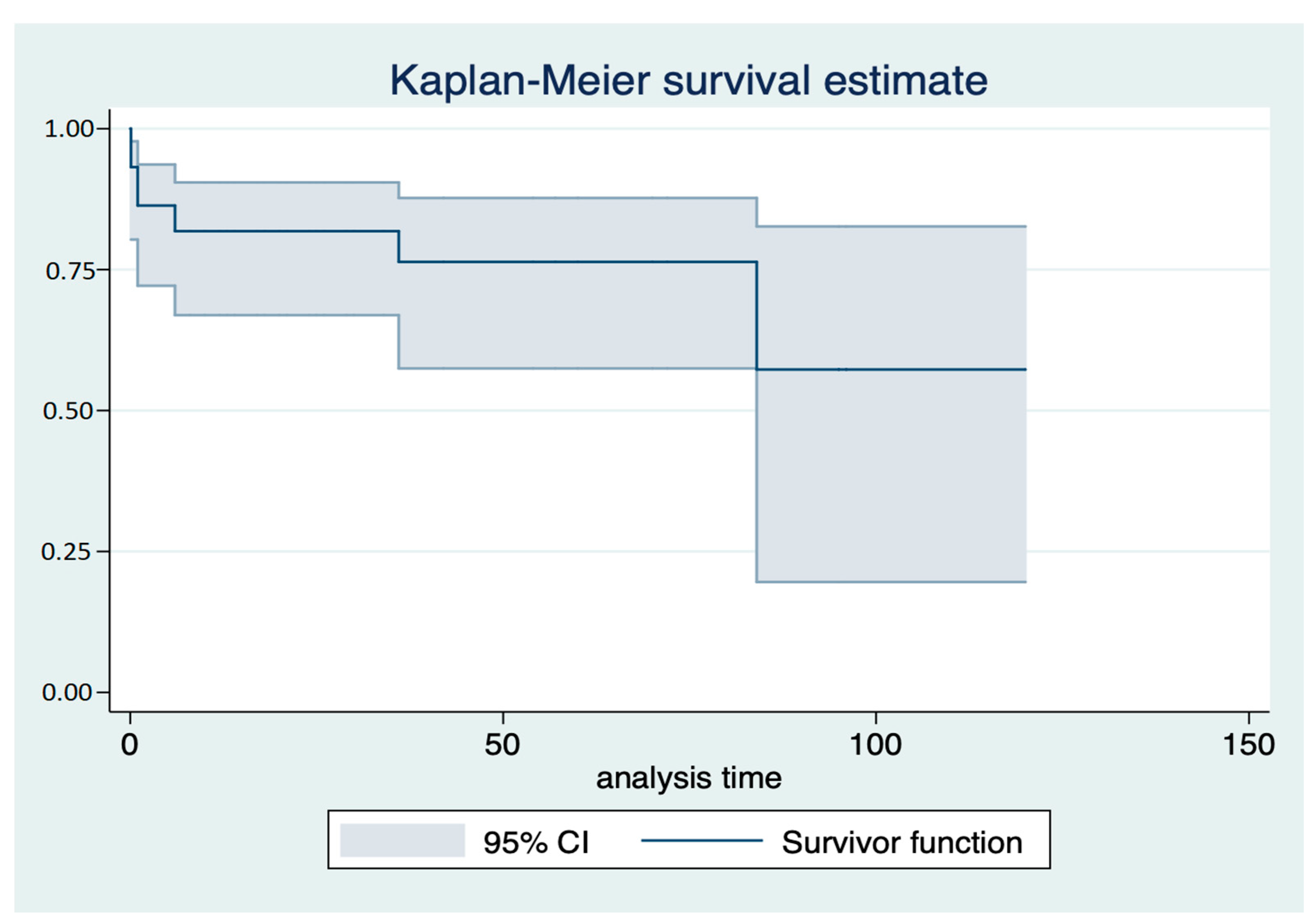
3.2. Follow-Up
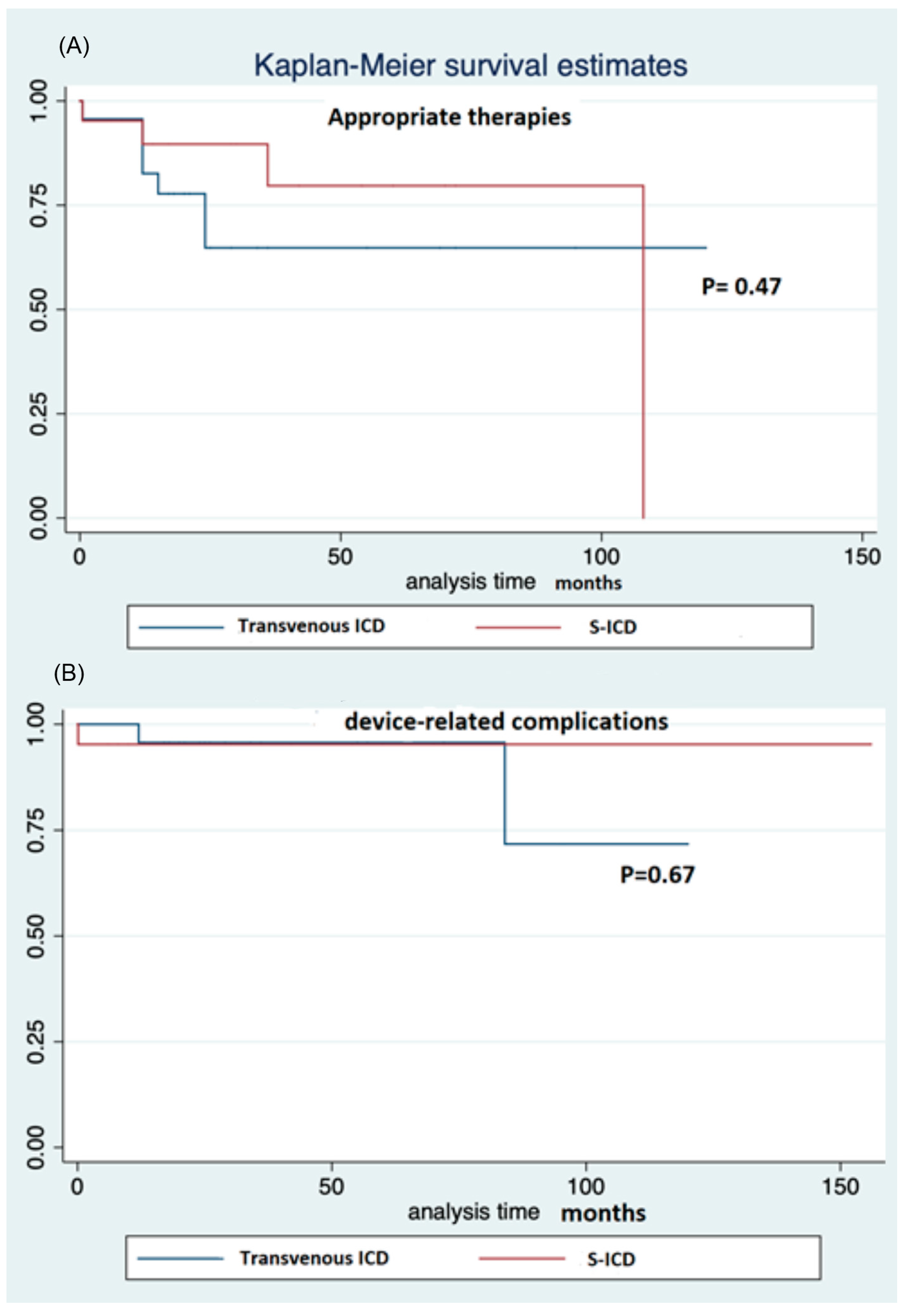
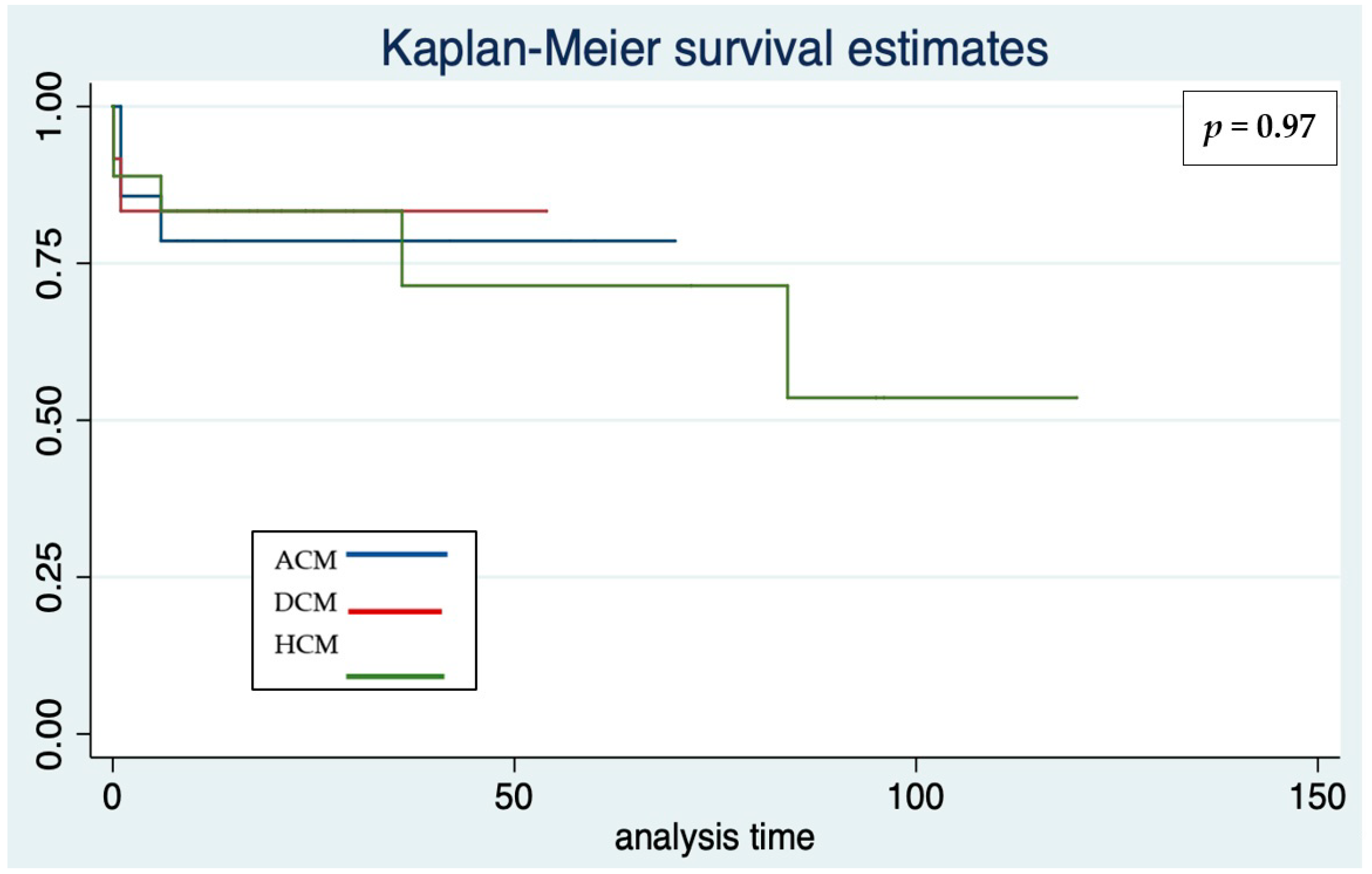
3.3. ICD Therapies
3.4. Device-Related Complications
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, T.M.; Hsu, D.T.; Kantor, P.; Towbin, J.A.; Ware, S.M.; Colan, S.D.; Chung, W.K.; Jefferies, J.L.; Rossano, J.W.; Castleberry, C.D.; et al. Pediatric Cardiomyopathies. Circ. Res. 2017, 121, 855–873. [Google Scholar] [CrossRef] [PubMed]
- Bharucha, T.; Lee, K.J.; Daubeney, P.E.; Nugent, A.W.; Turner, C.; Sholler, G.F.; Robertson, T.; Justo, R.; Ramsay, J.; Carlin, J.B.; et al. NACCS (National Australian Childhood Cardiomyopathy Study) Investigators. Sudden death in childhood cardiomyopathy: Results from a long-term national population-based study. J. Am. Coll. Cardiol. 2015, 65, 2302–2310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Norrish, G.; Cantarutti, N.; Pissaridou, E.; Ridout, D.A.; Limongelli, G.; Elliott, P.M.; Kaski, J.P. Risk factors for sudden cardiac death in childhood hypertrophic cardiomyopathy: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2017, 24, 1220–1230. [Google Scholar] [CrossRef] [Green Version]
- Pahl, E.; Sleeper, L.A.; Canter, C.E.; Hsu, D.T.; Lu, M.; Webber, S.A.; Colan, S.D.; Kantor, P.F.; Everitt, M.D.; Towbin, J.A.; et al. Pediatric Cardiomyopathy Registry Investigators. Incidence of and risk factors for sudden cardiac death in children with dilated cardiomyopathy: A report from the Pediatric Cardiomyopathy Registry. J. Am. Coll. Cardiol. 2012, 59, 607–615. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, M.J.; Silka, M.J.; Silva, J.A.; Balaji, S.; Beach, C.; Benjamin, M.; Berul, C.; Cannon, B.; Cecchin, F.; Cohen, M.; et al. Writing Committee Members. 2021 PACES Expert Consensus Statement on the Indications and Management of Cardiovascular Implantable Electronic Devices in Pediatric Patients. Heart Rhythm 2021, 18, P1888–P1924. [Google Scholar] [CrossRef]
- Norrish, G.; Chubb, H.; Field, E.; McLeod, K.; Ilina, M.; Spentzou, G.; Till, J.; Daubeney, P.E.F.; Stuart, A.G.; Matthews, J.; et al. Clinical outcomes and programming strategies of implantable cardioverter-defibrillator devices in paediatric hypertrophic cardiomyopathy: A UK National Cohort Study. Europace 2021, 23, 400–408. [Google Scholar] [CrossRef]
- Rella, V.; Parati, G.; Crotti, L. Sudden cardiac death in children affected by cardiomyopathies: An update on risk factors and indications at transvenous or subcutaneous implantable defibrillators. Front. Pediatr. 2020, 8, 139. [Google Scholar] [CrossRef] [Green Version]
- DeWitt, E.S.; Triedman, J.K.; Cecchin, F.; Mah, D.Y.; Abrams, D.J.; Walsh, E.P.; Gauvreau, K.; Alexander, M.E. Time dependence of risks and benefits in pediatric primary prevention ICD therapy. Circ. Arrhythmia Electrophysiol. 2014, 7, 1057–1063. [Google Scholar] [CrossRef]
- Silvetti, M.S. Cardioverter-defibrillator in children and young patients with congenital heart disease. Time to define ICD selection. Kardiol Pol. 2020, 78, 839–841. [Google Scholar] [CrossRef]
- Dechert, B.E.; Bradley, D.J.; Serwer, G.A.; Dick Ii, M.; Lapage, M.J. Implantable Cardioverter Defibrillator Outcomes in Pediatric and Congenital Heart Disease: Time to System Revision. PACE 2016, 39, 703–708. [Google Scholar] [CrossRef]
- Berul, C.I.; Van Hare, G.F.; Dubin, A.M.; Cecchin, F.; Collins, K.K.; Cannon, B.C.; Alexander, M.E.; Triedman, J.K.; Walsh, E.P.; Friedman, R.A. Results of a multicenter retrospective implantable cardioverter-defibrillator registry of pediatric and congenital heart disease patients. J. Am. Coll. Cardiol. 2008, 51, 1685–1691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jarman, J.W.; Lascelles, K.; Markides, V.; Clague, J.R.; Till, J. Clinical experience of entirely subcutaneous implantable cardioverter-defibrillators in children and adults: Cause for caution. Eur. Heart J. 2012, 33, 1351–1359. [Google Scholar] [CrossRef] [Green Version]
- Silvetti, M.S.; Pazzano, V.; Battipaglia, I.; Saputo, F.A.; Albanese, S.; Lovecchio, M.; Valsecchi, S.; Drago, F. S-ICD: Is it ready for use in children and young adults? A single-center study. Europace 2018, 20, 1966–1973. [Google Scholar] [CrossRef] [PubMed]
- von Alvensleben, J.C.; Dechert, B.; Bradley, D.J.; Fish, F.A.; Moore, J.P.; Pilcher, T.A.; Escudero, C.; Ceresnak, S.R.; Kwok, S.Y.; Balaji, S.; et al. Subcutaneous Implantable Cardioverter-Defibrillators in Pediatrics and Congenital Heart Disease: A Pediatric and Congenital Electrophysiology Society Multicenter Review. JACC Clin. Electrophysiol. 2020, 6, 1752–1761. [Google Scholar] [CrossRef] [PubMed]
- Brugada, J.; Blom, N.; Sarquella-Brugada, G.; Blomstrom-Lundqvist, C.; Deanfield, J.; Janousek, J.; Abrams, D.; Bauersfeld, U.; Brugada, R.; Drago, F.; et al. Pharmacological and non-pharmacological therapy for arrhythmias in the pediatric population: EHRA and AEPC-Arrhythmia Working Group joint consensus statement. Europace 2013, 15, 1337–1382. [Google Scholar] [CrossRef]
- Perry, M.; Elliott, P.M.; Anastasakis, A.; Borger, M.A.; Borggrefe, M.; Cecchi, F.; Charron, P.; Hagege, A.A.; Lafont, A.; Limongelli, G.; et al. The Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy. Eur. Heart J. 2014, 35, 2733–2779. [Google Scholar]
- Corrado, D.; Wichter, T.; Link, M.S.; Hauer, R.; Marchlinski, F.; Anastasakis, A.; Bauce, B.; Basso, C.; Brunckhorst, C.; Tsatsopoulou, A.; et al. Treatment of arrhythmogenic right ventricular cardiomyopathy/dysplasia: An international task force consensus statement. Eur. Heart J. 2015, 36, 3227–3237. [Google Scholar] [CrossRef]
- Epstein, A.E.; DiMarco, J.P.; Estes, N.A., 3rd; Freedman, R.A.; Gettes, L.S.; Gillinov, A.M.; Gregoratos, G.; Hammill, S.C.; Hayes, D.L.; Hlatky, M.A.; et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices). J. Am. Coll. Cardiol. 2008, 51, e1–e62. [Google Scholar]
- Silvetti, M.S.; Drago, F.; Di Carlo, D.; Placidi, S.; Brancaccio, G.; Carotti, A. Cardiac pacing in paediatric patients with congenital heart defects: Transvenous or epicardial? Europace 2013, 15, 1280–1286. [Google Scholar] [CrossRef]
- Bordachar, P.; Marquié, C.; Pospiech, T.; Pasquié, J.L.; Jalal, Z.; Haissaguerre, M.; Thambo, J.B. Subcutaneous implantable cardioverter defibrillators in children, young adults and patients with congenital heart disease. Int. J. Cardiol. 2016, 203, 251–258. [Google Scholar] [CrossRef]
- Winter, J.; Siekiera, M.; Shin, D.I.; Meyer, C.; Kröpil, P.; Clahsen, H.; O’Connor, S. Intermuscular technique for implantation of the subcutaneous implantable cardioverter defibrillator: Long-term performance and complications. Europace 2017, 19, 2036–2041. [Google Scholar] [CrossRef] [PubMed]
- Knops, R.E.; Olde Nordkamp, L.R.; de Groot, J.R.; Wilde, A.A. Two-incision technique for implantation of the subcutaneous implantable cardioverter-defibrillator. Heart Rhythm 2013, 10, 1240–1243. [Google Scholar] [CrossRef] [PubMed]
- Silvetti, M.S.; Saputo, F.A.; Palmieri, R.; Placidi, S.; Santucci, S.; Di Mambro, C.; Righi, D.; Drago, F. Results of remote follow-up and monitoring in young patients with cardiac implantable electronic devices. Cardiol. Young 2016, 26, 53–60. [Google Scholar] [CrossRef]
- Winkler, F.; Dave, H.; Weber, R.; Gass, M.; Balmer, C. Long-term outcome of epicardial implantable cardioverter-defibrillator systems in children: Results justify its preference in paediatric patients. Europace 2018, 20, 1484–1490. [Google Scholar] [CrossRef]
- Frommeyer, G.; Feder, S.; Debus, V.; Köbe, J.; Reinke, F.; Uebing, A.; Eckardt, L.; Keh, H.G. Long-term single-center experience of defibrillator therapy in children and adolescents. Int. J. Cardiol. 2018, 271, 105–108. [Google Scholar] [CrossRef]
- Muller, M.J.; Dieks, J.K.; Schneider, H.E.; Ruschewski, W.; Tirilomis, T.; Paul, T.; Krause, U. Efficacy and safety of non-transvenous cardioverter defibrillators in infants and young children. J. Interv. Card Electrophysiol. 2019, 54, 151–159. [Google Scholar] [CrossRef]
- Aykan, H.H.; Karagoz, T.; Gulgun, M.; Ertugrul, I.; Aypar, E.; Ozer, S.; Alehan, D.; Celiker, A.; Ozkutlu, S. Midterm results of implantable cardioverter defibrillators in children and young adults from a single center in Turkey. PACE 2016, 39, 1225–1239. [Google Scholar] [CrossRef]
- Lewandowski, M.; Syska, P.; Kowalik, I. Children and young adults treated with transvenous and subcutaneous implantable cardioverter-defibrillators: A 22-year single-center experience and new perspectives. Kardiol. Pol. 2020, 78, 869–874. [Google Scholar] [CrossRef]
- Pettit, S.J.; McLean, A.; Colquhoun, I.; Connelly, D.; McLeod, K. Clinical experience of subcutaneous and transvenous implantable cardioverter defibrillators in children and teenagers. Pacing Clin. Electrophysiol. 2013, 36, 1532–1538. [Google Scholar] [CrossRef]
- Bettin, M.; Larbig, R.; Fischer, A.; Frommeyer, G.; Reinke, F.; Köbe, J.; Eckardt, L. Long-Term experience with the Subcutaneous Implantable Cardioverter-Defibrillator in teenagers and young adults. JACC Clin. EP 2017, 13, 1499–1506. [Google Scholar] [CrossRef]
- Quast, A.B.E.; Brouwer, T.F.; Kooiman, K.M.; van Dessel, P.F.H.M.; Blom, N.A.; Wilde, A.A.M.; Knops, R.E. Comparison of complications and shocks in paediatric and young transvenous and subcutaneous implantable cardioverter-defibrillator patients. Neth. Heart J. 2018, 26, 612–619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaski, J.P.; Tome Esteban, M.T.; Lowe, M.; Sporton, S.; Rees, P.; Deanfield JEMcKenna, W.J.; Elliott, P.M. Outcomes after implantable cardioverter-defibrillator treatment in children with hypertrophic cardiomyopathy. Heart 2007, 93, 372–374. [Google Scholar] [CrossRef] [Green Version]
- Maron, B.J.; Spirito, P.; Ackerman, M.J.; Casey, S.A.; Semsarian, C.; Estes, N.A., 3rd; Shannon, K.M.; Ashley, E.A.; Day, S.M.; Pacileo, G.; et al. Prevention of sudden cardiac death with implantable cardioverter-defibrillators in children and adolescents with hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2013, 61, 1527–1535. [Google Scholar] [CrossRef]
- Kamp, A.N.; Von Bergen, N.H.; Henrikson, C.A.; Makhoul, M.; Saarel, E.V.; Lapage, M.J.; Russell, M.W.; Strieper, M.; Yu, S.; Dick, M.; et al. Implanted defibrillators in young hypertrophic cardiomyopathy patients: A multicenter study. Pediatr. Cardiol. 2013, 34, 1620–1627. [Google Scholar] [CrossRef]
- Migliore, F.; Viani, S.; Migliore, F.; Viani, S.; Bongiorni, M.G.; Zorzi, A.; Silvetti, M.S.; Francia, P.; D'Onofrio, A.; De Franceschi, P.; et al. Subcutaneous implantable cardioverter defibrillator in patients with arrhythmogenic right ventricular cardiomyopathy: Results from an Italian multicenter registry. Int. J. Cardiol. 2019, 280, 74–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dubin, A.M.; Berul, C.I.; Bevilacqua, L.M.; Collins, K.K.; Etheridge, S.P.; Fenrich, A.L.; Friedman, R.A.; Hamilton, R.M.; Schaffer, M.S.; Shah, M.; et al. The use of implantable cardioverter- defibrillators in pediatric patients awaiting heart transplantation. J. Card Fail. 2003, 9, 375–379. [Google Scholar] [CrossRef]
- El-Assaad, I.; Al-Kindi, S.G.; Oliveira, G.H.; Boyle, G.J.; Aziz, P.F. Implantable cardioverter-defibrillator and wait-list outcomes in pediatric patients awaiting heart transplantation. Heart Rhythm 2015, 12, 2443–2448. [Google Scholar] [CrossRef]
- Feingold, B.; Arora, G.; Webber, S.A.; Smith, K.J. Cost-effectiveness of implantable cardioverter-defibrillators in children with dilated cardiomyopathy. J. Card Fail. 2010, 16, 734–741. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baban, A.; Lodato, V.; Parlapiano, G.; di Mambro, C.; Adorisio, R.; Bertini, E.S.; Dionisi-Vici, C.; Drago, F.; Martinelli, D. Myocardial and Arrhythmic Spectrum of Neuromuscular Disorders in Children. Biomolecules 2021, 11, 1578. [Google Scholar] [CrossRef] [PubMed]
- McCulloch, M.A.; Lal, A.K.; Knecht, K.; Butts, R.J.; Villa, C.R.; Johnson, J.N.; Conway, J.; Bock, M.J.; Schumacher, K.R.; Law, S.P.; et al. Implantable Cardioverter Defibrillator Use in Males with Duchenne Muscular Dystrophy and Severe Left Ventricular Dysfunction. Pediatr. Cardiol. 2020, 41, 925–931. [Google Scholar] [CrossRef] [PubMed]
- Adorisio, R.; Mencarelli, E.; Cantarutti, N.; Calvieri, C.; Amato, L.; Cicenia, M.; Silvetti, M.S.; D'Amico, A.; Grandinetti, M.; Drago, F.; et al. Duchenne Dilated Cardiomyopathy: Cardiac Management from Prevention to Advanced Cardiovascular Therapies. J. Clin. Med. 2020, 9, E3186. [Google Scholar] [CrossRef] [PubMed]
- Baban, A.; Cicenia, M.; Magliozzi, M.; Gnazzo, M.; Cantarutti, N.; Silvetti, M.S.; Adorisio, R.; Dallapiccola, B.; Bertini, E.; Novelli, A.; et al. Cardiovascular Involvement in Pediatric Laminopathies. Report of Six Patients and Literature Revision. Front. Pediatr. 2020, 8, 374. [Google Scholar] [CrossRef] [PubMed]


| Number (%) | Number (%) or Median (25th–75th Centiles) | |
|---|---|---|
| Patients | 44 (100%) | |
| Males | 24 (54%) | |
| Age, years | 14 (12–17) | |
| Height, cm | 164 (151–171) | |
| Weight, kg | 54 (44–69) | |
| Hypertrophic cardiomyopathy | 17 (39%) | |
| Arrhythmogenic cardiomyopathy | 14 (32%) | |
| Dilated cardiomyopathy | 12 (27%) | |
| Restrictive cardiomyopathy | 1 (2%) | |
| Primary prevention | 32 (73%) | |
| Secondary prevention | 12 (27%) | |
| Transvenous ICD | 23 (52%) | |
| VVI | 12 (52%) | |
| DDD | 11 (48%) | |
| Pre-pectoral pocket | 16 (70%) | |
| Sub-pectoral pocket | 7 (30%) | |
| Subcutaneous ICD | 21 (48%) | |
| Subcutaneous pocket | 9 (43%) | |
| Intermuscular pocket | 12 (57%) | |
| Follow-up | 29 (14–60) months | |
| Appropriate therapies | 11 (25%) | 12 (12–24) months |
| Total complications | 11 (25%) | 1 (0.6–18) months |
| Complications requiring surgical revision | 8 (18%) | 1 (0.8–12) months |
| Inappropriate shocks | 3 (7%) | 6 (0.1–84) months |
| Pts | Primary Prev. | Height at Impl. cm | Weight at Impl. kg | Age at Impl. yrs | Effective Therapy | Complications Requiring Surgical Revision | Inappropriate Shocks | Follow-Up, Mos. | |
|---|---|---|---|---|---|---|---|---|---|
| HCM | 17 39% | 14 82% | 152 (146–165) | 48 (38–55) | 12 (10–14) | 7 41% | 3 18% | 2 12% | 29 (17–91) |
| DCM | 12 27% | 8 67% | 180 (166–180) | 57 (44–72) | 15 (13–17) | 2 17% | 3 25% | 0 | 22 (13–31) |
| ACM | 14 32% | 10 71% | 163 (155–171) | 61 (50–71) | 15 (14–17) | 2 14% | 2 14% | 1 7% | 49 (18–67) |
| RCM | 1 2% | 0 | 168 | 48 | 14 | 0 | 0 | 0 | 18 |
| ICD | Pts | Primary Prev. | Height at Impl. cm | Weight Impl. kg | Age Impl. yrs | Sub-Cutaneous Pocket | Effective Therapy | Complications Requiring Surgical Revision | Inappropriate Shocks | Follow-Up, Mos. |
|---|---|---|---|---|---|---|---|---|---|---|
| Trans-venous | 23 | 13 56% | 161 (146–180) | 48 (38–67) | 14 (12–17) | 16 70% | 7 30% | 4 17% | 2 9% | 26 (19–63) |
| Sub-cutaneous | 21 | 19 90% | 164 (155–171) | 58 (52–69) | 14 (12–17) | 9 43% | 4 19% | 4 19% | 1 5% | 30 (14–60) |
| Complications | n. | Time to Complication, Months | Device | Cardiomyopathy | Treatment |
|---|---|---|---|---|---|
| Inappropriate shock | 3 | 6 (0.1–84) | 2 TV-ICD 1 S-ICD | 2 HCM 1 ACM | 2 reprogramming (+1 drug treatment), none |
| Pocket/wound related | 3 | 6 (3–21) | 3 S-ICD | 2 HCM 1 ACM | 2 revision, 1 explant |
| Lead related | 4 | 1 (0.7–8) | 3 TV-ICD 1 S-ICD | 2 DCM 1 ACM 1 HCM | Lead repositioning |
| Pericardial effusion | 1 | 0.1 | TV-ICD | DCM | Drainage |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silvetti, M.S.; Tamburri, I.; Campisi, M.; Saputo, F.A.; Cazzoli, I.; Cantarutti, N.; Cicenia, M.; Adorisio, R.; Baban, A.; Ravà, L.; et al. ICD Outcome in Pediatric Cardiomyopathies. J. Cardiovasc. Dev. Dis. 2022, 9, 33. https://doi.org/10.3390/jcdd9020033
Silvetti MS, Tamburri I, Campisi M, Saputo FA, Cazzoli I, Cantarutti N, Cicenia M, Adorisio R, Baban A, Ravà L, et al. ICD Outcome in Pediatric Cardiomyopathies. Journal of Cardiovascular Development and Disease. 2022; 9(2):33. https://doi.org/10.3390/jcdd9020033
Chicago/Turabian StyleSilvetti, Massimo Stefano, Ilaria Tamburri, Marta Campisi, Fabio Anselmo Saputo, Ilaria Cazzoli, Nicoletta Cantarutti, Marianna Cicenia, Rachele Adorisio, Anwar Baban, Lucilla Ravà, and et al. 2022. "ICD Outcome in Pediatric Cardiomyopathies" Journal of Cardiovascular Development and Disease 9, no. 2: 33. https://doi.org/10.3390/jcdd9020033
APA StyleSilvetti, M. S., Tamburri, I., Campisi, M., Saputo, F. A., Cazzoli, I., Cantarutti, N., Cicenia, M., Adorisio, R., Baban, A., Ravà, L., & Drago, F. (2022). ICD Outcome in Pediatric Cardiomyopathies. Journal of Cardiovascular Development and Disease, 9(2), 33. https://doi.org/10.3390/jcdd9020033








