Prognostic Implications of Left Ventricular Ejection Fraction and Left Ventricular End-Diastolic Diameter on Clinical Outcomes in Patients with ICD
Abstract
1. Introduction
2. Methods
2.1. Population
2.2. Echocardiography
2.3. Follow-Up and Outcomes
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Follow-Up
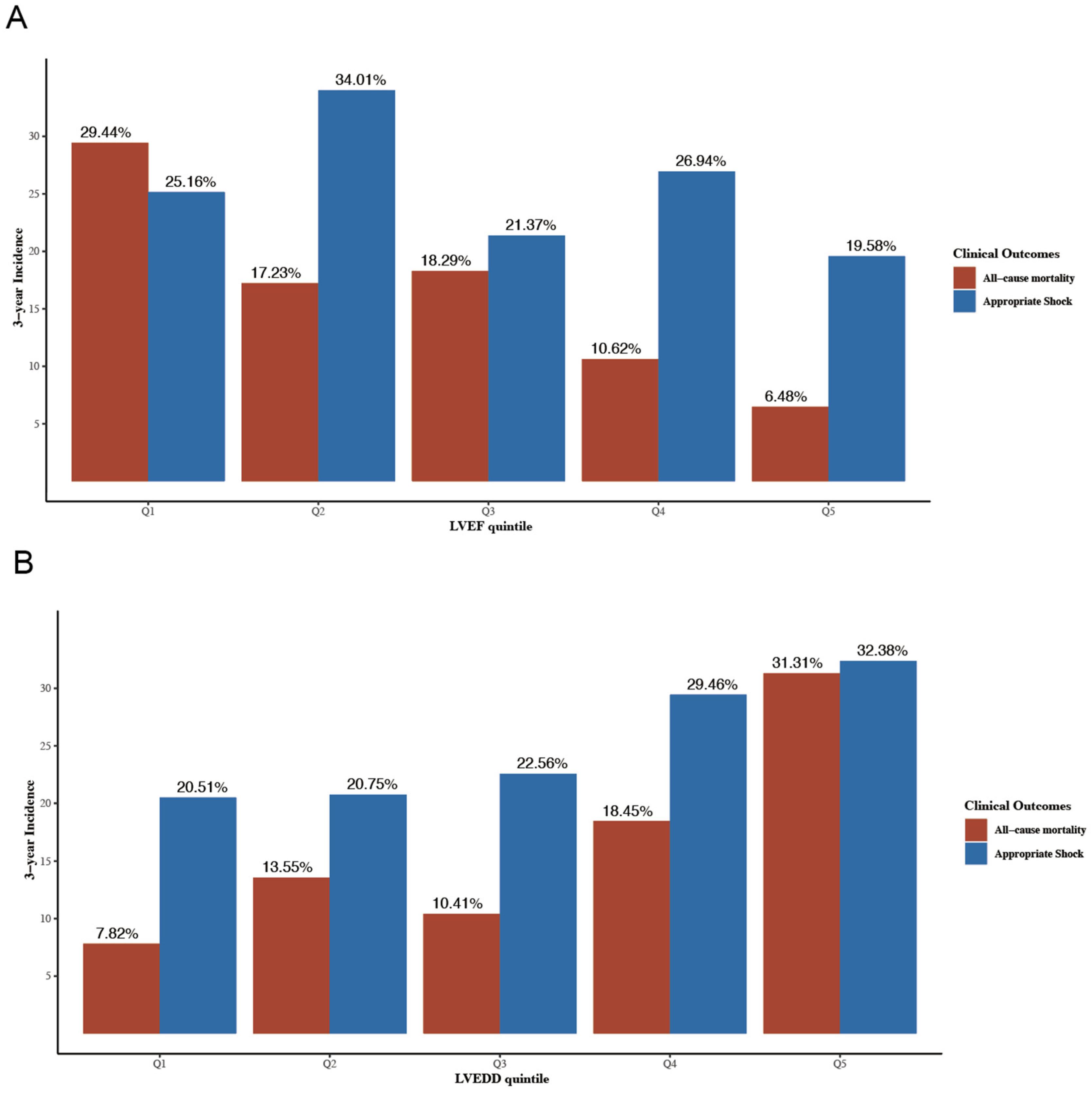
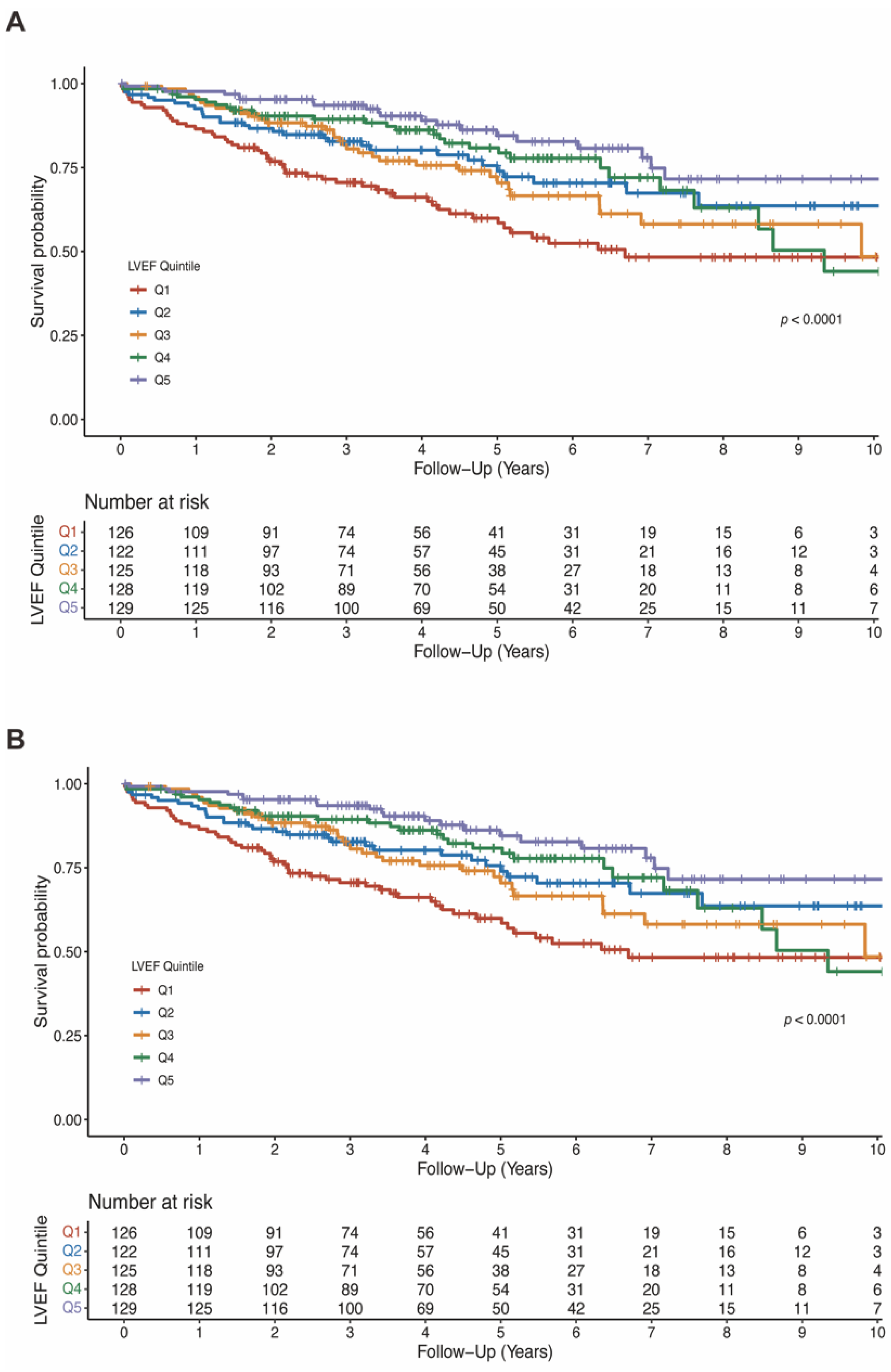
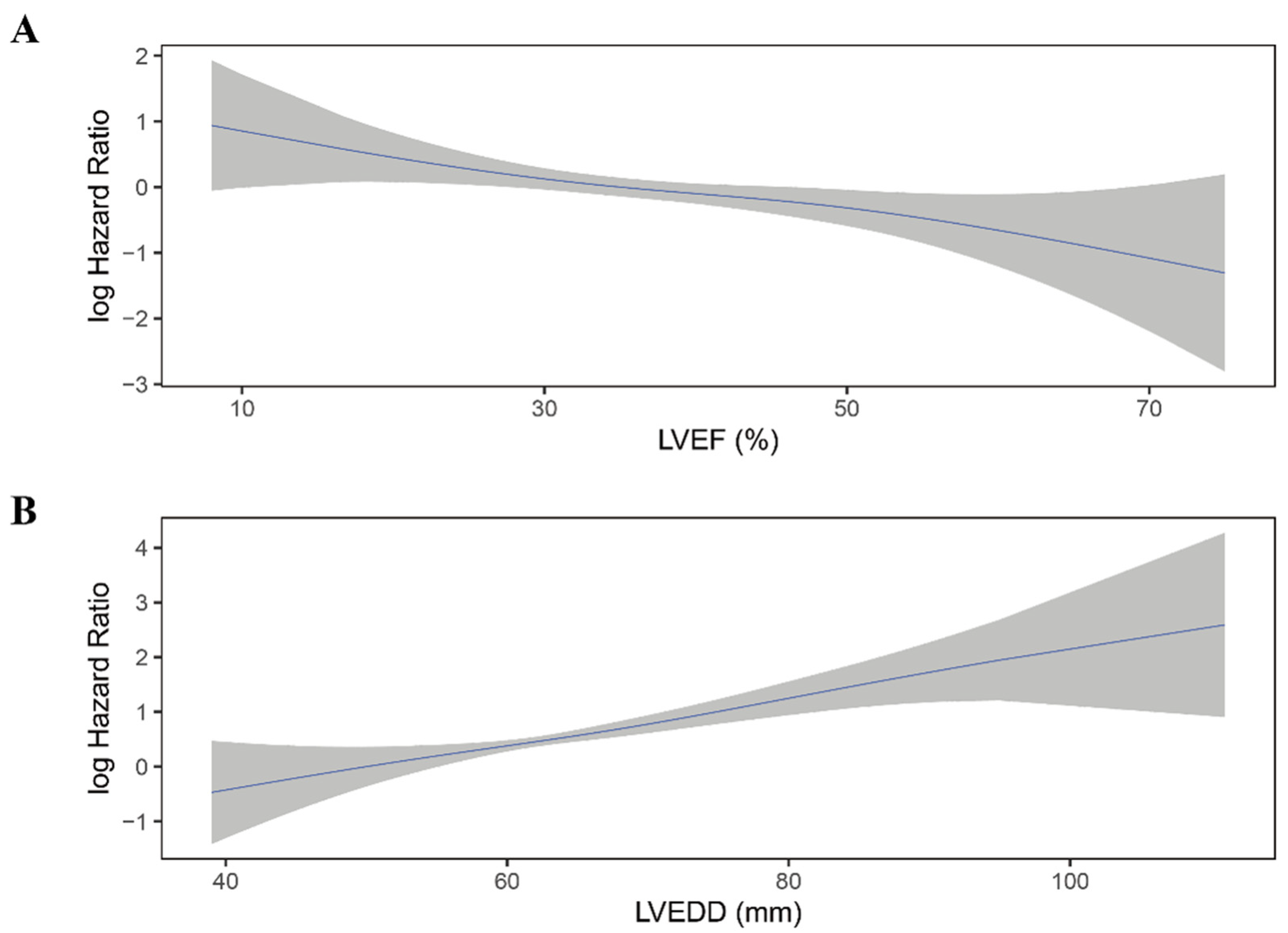
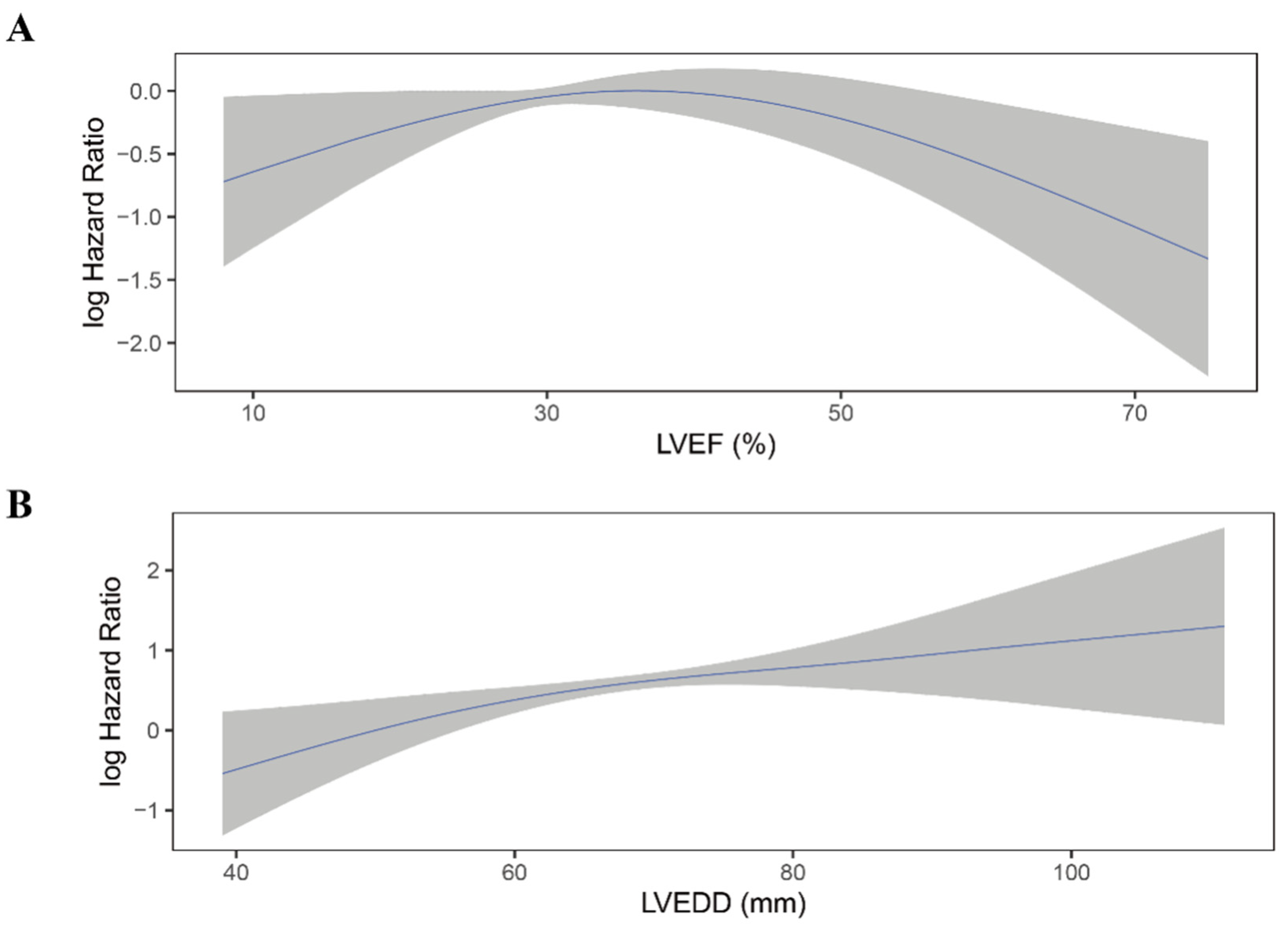
3.3. Association of LVEF with Mortality
3.4. Association of LVEDD with Mortality
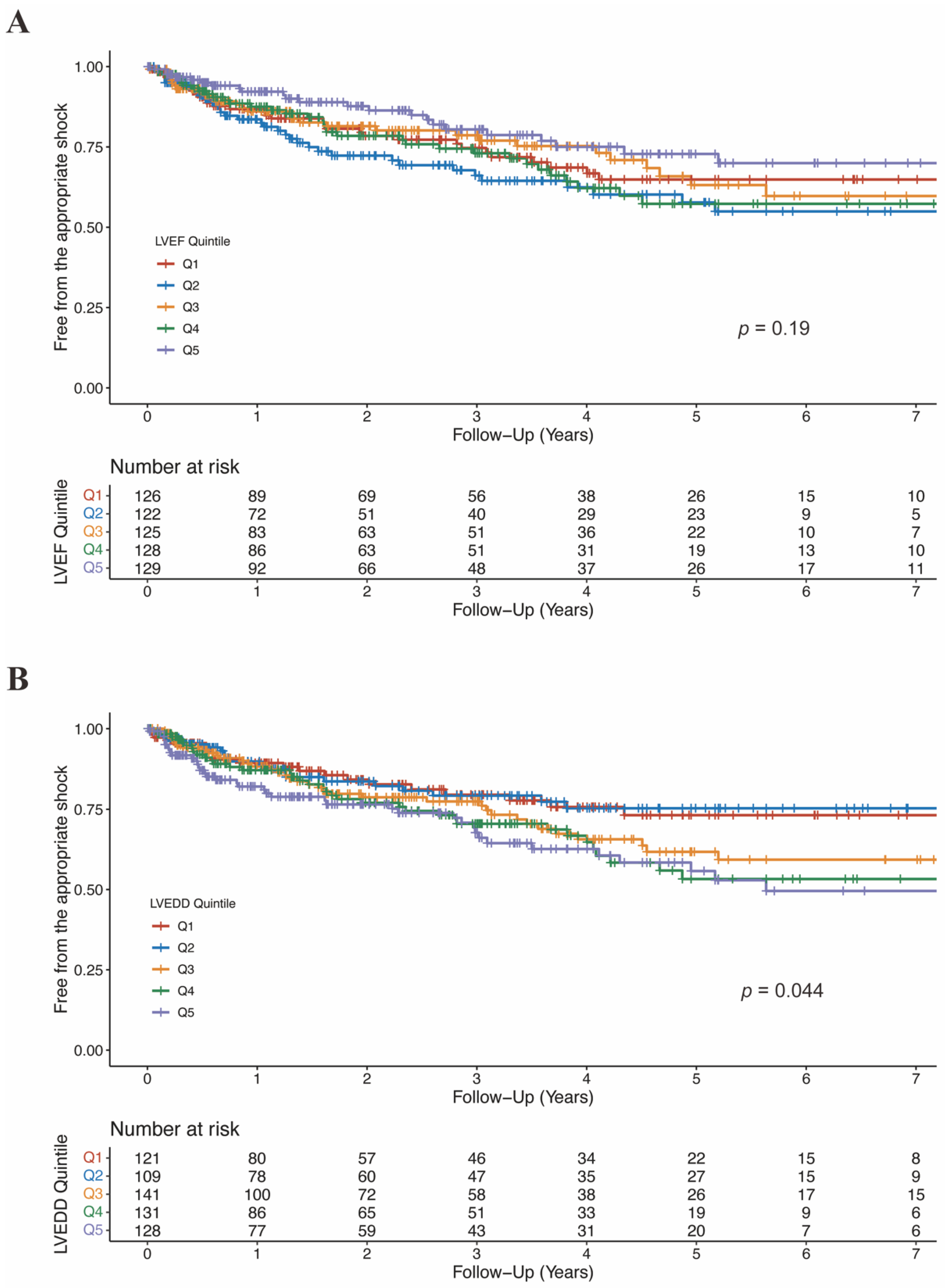
3.5. Association of LVEF and LVEDD with Appropriate Shock
3.6. Incremental Prognostic Value of LVEF and LVEDD in Multivariable Models
3.7. Subgroup and Sensitivity Analyses
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Nonstandard Abbreviations and Acronyms
| ACEI | angiotensin-converting enzyme inhibitor |
| AF | atrial fibrillation |
| ARB | angiotensin II receptor blocker |
| ARNI | angiotensin receptor-neprilysin inhibitor |
| BMI | body mass index |
| CI | confidence interval |
| CLBBB | complete left bundle branch block |
| CRBBB | complete right bundle branch block |
| eGFR | estimated glomerular filtration rate |
| HR | hazard ratio |
| ICD | implantable cardioverter defibrillator |
| ICM | ischemic cardiomyopathy |
| IDI | integrated discrimination index |
| LVEDD | left ventricular end-diastolic diameter |
| LVEF | left ventricular ejection fraction |
| NICM | non-ischemic cardiomyopathy |
| NRI | net reclassification index |
| NT-proBNP | N-terminal pro-brain natriuretic peptide |
| NYHA | New York Heart Association |
| SCD | sudden cardiac death |
References
- Zeppenfeld, K.; Tfelt-Hansen, J.; de Riva, M.; Winkel, B.G.; Behr, E.R.; Blom, N.A.; Charron, P.; Corrado, D.; Dagres, N.; de Chillou, C.; et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur. Heart J. 2022, 26, ehac262. [Google Scholar]
- Al-Khatib, S.M.; Stevenson, W.G.; Ackerman, M.J.; Bryant, W.J.; Callans, D.J.; Curtis, A.B.; Deal, B.J.; Dickfeld, T.; Field, M.E.; Fonarow, G.C.; et al. 2017 AHA/ACC/HRS Guideline for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death. J. Am. Coll. Cardiol. 2018, 72, e91–e220. [Google Scholar] [CrossRef] [PubMed]
- Moss, A.J.; Wilber, D.J.; Brown, M.W. Prophylactic Implantation of a Defibrillator in Patients with Myocardial Infarction and Reduced Ejection Fraction. N. Engl. J. Med 2002, 346, 877–883. [Google Scholar] [CrossRef] [PubMed]
- Kadish, A.; Quigg, R.; Calkins, H.; Shalaby, A.; Levine, J.H. Prophylactic Defibrillator Implantation in Patients with Nonischemic Dilated Cardiomyopathy. N. Engl. J. Med. 2004, 350, 2151–2158. [Google Scholar] [CrossRef] [PubMed]
- Bardy, G.H.; Boineau, R.; Johnson, G.; Davidson-Ray, L.D.; Ip, J.H. Amiodarone or an Implantable Cardioverter–Defibrillator for Congestive Heart Failure. N. Engl. J. Med. 2005, 352, 225–237. [Google Scholar] [CrossRef] [PubMed]
- Quiñones, M.A.; Greenberg, B.H.; Kopelen, H.A.; Koilpillai, C.; Limacher, M.C.; Shindler, D.M.; Shelton, B.J.; Weiner, D.H.; for the SOLVD Investigators. Echocardiographic predictors of clinical outcome in patients with left ventricular dysfunction enrolled in the SOLVD registry and trials: Significance of left ventricular hypertrophy. J. Am. Coll. Cardiol. 2000, 35, 1237–1244. [Google Scholar] [CrossRef] [PubMed]
- Aleong, R.G.; Mulvahill, M.J.; Halder, I.; Carlson, N.E.; Singh, M.; Bloom, H.L.; Dudley, S.C.; Ellinor, P.T.; Shalaby, A.; Weiss, R.; et al. Left Ventricular Dilatation Increases the Risk of Ventricular Arrhythmias in Patients with Reduced Systolic Function. J. Am. Hear. Assoc. 2015, 4, e001566. [Google Scholar] [CrossRef]
- Watanabe, J.; Shinozaki, T.; Shiba, N.; Fukahori, K.; Koseki, Y.; Karibe, A.; Sakuma, M.; Miura, M.; Kagaya, Y.; Shirato, K. Accumulation of risk markers predicts the incidence of sudden death in patients with chronic heart failure. Eur. J. Heart Fail. 2006, 8, 237–242. [Google Scholar] [CrossRef]
- Kajimoto, K.; Minami, Y.; Otsubo, S.; Sato, N. Sex Differences in Left Ventricular Cavity Dilation and Outcomes in Acute Heart Failure Patients with Left Ventricular Systolic Dysfunction. Can. J. Cardiol. 2018, 34, 477–484. [Google Scholar] [CrossRef]
- Catanzaro, J.N.; Makaryus, J.N.; Makaryus, A.N.; Sison, C.; Vavasis, C.; Fan, D.; Jadonath, R. Echocardiographic Predictors of Ventricular Tachycardia. Clin. Med. Insights Cardiol. 2015, 8 (Suppl. S4), 37–42. [Google Scholar] [CrossRef]
- Narayanan, K.; Reinier, K.; Teodorescu, C.; Uy-Evanado, A.; Aleong, R.; Chugh, H.; Nichols, G.A.; Gunson, K.; London, B.; Jui, J.; et al. Left Ventricular Diameter and Risk Stratification for Sudden Cardiac Death. J. Am. Heart Assoc. 2014, 3, e001193. [Google Scholar] [CrossRef]
- Mitchell, C.; Rahko, P.S.; Blauwet, L.A.; Canaday, B.; Finstuen, J.A.; Foster, M.C.; Horton, K.; Ogunyankin, K.O.; Palma, R.A.; Velazquez, E.J.; et al. Guidelines for Performing a Comprehensive Transthoracic Echocardiographic Examination in Adults: Recommendations from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2019, 32, 1–64. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.D.; Velazquez, E.; Kober, L.; Pfeffer, M.A. Sudden Death in Patients with Myocardial Infarction and Left Ventricular Dysfunction, Heart Failure, or Both. N. Engl. J. Med. 2005, 352, 2581–2588. [Google Scholar] [CrossRef] [PubMed]
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure. J. Am. Coll. Cardiol. 2022, 79, e263–e421. [Google Scholar] [PubMed]
- Køber, L.; Thune, J.J.; Nielsen, J.C.; Haarbo, J.; Videbæk, L.; Korup, E.; Jensen, G.; Hildebrandt, P.; Steffensen, F.H.; Bruun, N.E.; et al. Defibrillator Implantation in Patients with Nonischemic Systolic Heart Failure. N. Engl. J. Med. 2016, 375, 1221–1230. [Google Scholar] [CrossRef]
- Di Marco, A.; Brown, P.F.; Bradley, J.; Nucifora, G.; Claver, E.; de Frutos, F.; Dallaglio, P.D.; Comin-Colet, J.; Anguera, I.; Miller, C.A.; et al. Improved Risk Stratification for Ventricular Arrhythmias and Sudden Death in Patients with Nonischemic Dilated Cardiomyopathy. J. Am. Coll. Cardiol. 2021, 77, 2890–2905. [Google Scholar] [CrossRef] [PubMed]
- Marijon, E.; Garcia, R.; Narayanan, K.; Karam, N.; Jouven, X. Fighting against sudden cardiac death: Need for a paradigm shift—Adding near-term prevention and pre-emptive action to long-term prevention. Eur. Heart J. 2022, 43, 1457–1464. [Google Scholar] [CrossRef] [PubMed]
- Zecchin, M. The role of implantable cardioverter defibrillator for primary vs secondary prevention of sudden death in patients with idiopathic dilated cardiomyopathy. Europace 2004, 6, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.; Sarak, B.; Kaplan, A.J.; Oosthuizen, R.; Beardsall, M.; Wulffhart, Z.; Higenbottam, J.; Khaykin, Y. Predictors of Appropriate Implantable Cardioverter Defibrillator (ICD) Therapy in Primary Prevention Patients with Ischemic and Nonischemic Cardiomyopathy. Pacing Clin. Electrophysiol. 2010, 33, 320–329. [Google Scholar] [CrossRef] [PubMed]
- Satake, H.; Fukuda, K.; Sakata, Y.; Miyata, S.; Nakano, M.; Kondo, M.; Hasebe, Y.; Segawa, M.; Shimokawa, H.; on behalf of the CHART-2 Investigators. Current Status of Primary Prevention of Sudden Cardiac Death with Implantable Cardioverter Defibrillator in Patients with Chronic Heart Failure—A Report From the CHART-2 Study. Circ. J. 2015, 79, 381–390. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Chen, K.; Su, Y.; Hua, W.; Yang, J.; Chen, S.; Liang, Z.; Xu, W.; Zhang, S. High incidence of ventricular arrhythmias in patients with left ventricular enlargement and moderate left ventricular dysfunction. Clin. Cardiol. 2016, 39, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C.; Lee, D.S.; Fine, J.P. Introduction to the Analysis of Survival Data in the Presence of Competing Risks. Circulation 2016, 133, 601–609. [Google Scholar] [CrossRef]
- Aiba, T.; Tomaselli, G.F. Electrical remodeling in the failing heart. Curr. Opin. Cardiol. 2010, 25, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Adelstein, E.C.; Schwartzman, D.; Jain, S.; Bazaz, R.; Wang, N.C.; Saba, S. Left ventricular dimensions predict risk of appropriate shocks but not mortality in cardiac resynchronization therapy- defibrillator recipients with left bundle-branch block and non-ischemic cardiomyopathy. Europace 2017, 19, 1689–1694. [Google Scholar] [CrossRef] [PubMed]
- Aiba, T.; Hesketh, G.G.; Barth, A.S.; Liu, T.; Daya, S.; Chakir, K.; Dimaano, V.L.; Abraham, T.P.; O’Rourke, B.; Akar, F.G.; et al. Electrophysiological Consequences of Dyssynchronous Heart Failure and Its Restoration by Resynchronization Therapy. Circulation 2009, 119, 1220–1230. [Google Scholar] [CrossRef] [PubMed]
- Gulati, A.; Jabbour, A.; Ismail, T.F.; Guha, K.; Khwaja, J.; Raza, S.; Morarji, K.; Brown, T.D.H.; Ismail, N.A.; Dweck, M.R.; et al. Association of Fibrosis with Mortality and Sudden Cardiac Death in Patients with Nonischemic Dilated Cardiomyopathy. JAMA 2013, 309, 896. [Google Scholar] [CrossRef] [PubMed]
- Klem, I.; Klein, M.; Khan, M.; Yang, E.Y.; Nabi, F.; Ivanov, A.; Bhatti, L.; Hayes, B.; Graviss, E.A.; Nguyen, D.T.; et al. Relationship of LVEF and Myocardial Scar to Long-Term Mortality Risk and Mode of Death in Patients with Nonischemic Cardiomyopathy. Circulation 2021, 143, 1343–1358. [Google Scholar] [CrossRef] [PubMed]
- Goldberger, J.J.; Cain, M.E.; Hohnloser, S.H.; Kadish, A.H.; Knight, B.P.; Lauer, M.S.; Maron, B.J.; Page, R.L.; Passman, R.S.; Siscovick, D.; et al. American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society Scientific Statement on Noninvasive Risk Stratification Techniques for Identifying Patients at Risk for Sudden Cardiac Death. J. Am. Coll. Cardiol. 2008, 52, 1179–1199. [Google Scholar] [CrossRef]
- Grimm, W.; Timmesfeld, N.; Efimova, E. Left ventricular function improvement after prophylactic implantable cardioverter-defibrillator implantation in patients with non-ischaemic dilated cardiomyopathy. Europace 2013, 15, 1594–1600. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ellenbogen, K.A.; Levine, J.H.; Berger, R.D.; Daubert, J.P.; Winters, S.L.; Greenstein, E.; Shalaby, A.; Schaechter, A.; Subacius, H.; Kadish, A.; et al. Are Implantable Cardioverter Defibrillator Shocks a Surrogate for Sudden Cardiac Death in Patients with Nonischemic Cardiomyopathy? Circulation 2006, 113, 776–782. [Google Scholar] [CrossRef] [PubMed]

| All Patients (N = 630) | |
|---|---|
| Age, years | 60.7 (11.8) |
| Male | 527 (83.7%) |
| BMI, kg/m2 | 24.9 (3.57) |
| Smoking | 358 (56.8%) |
| Alcohol | 262 (41.6%) |
| Blood pressure | |
| Systolic, mmHg | 119 (17.3) |
| Diastolic, mmHg | 73 (10.7) |
| NYHA functional class, >II | 273 (43.3%) |
| Comorbidity | |
| Diabetes | 139 (22.1%) |
| Hypertension | 290 (46.0%) |
| AF | 182 (28.9%) |
| ICM | 343 (54.4%) |
| Stroke | 41 (6.51%) |
| Hyperlipidemia | 338 (53.7%) |
| CRBBB | 42 (6.67%) |
| CLBBB | 36 (5.71%) |
| Primary prevention | 145 (23.0%) |
| Medication | |
| ACEI/ARB/ARNI | 458 (72.7%) |
| β-blocker | 517 (82.1%) |
| Digoxin | 166 (26.3%) |
| Diuretic | 471 (74.8%) |
| Amiodarone | 217 (34.4%) |
| Biomarker | |
| NT-proBNP a, pg/ml | 936.75 (427.82, 1908.72) |
| eGFR, ml/min/1.73 m2 | 78.5 (23.6) |
| Albumin, g/L | 41.5 (4.96) |
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| HR (95%CI) | p Value | HR (95%CI) | p Value | HR (95%CI) | p Value | HR (95%CI) | p Value | |
| LVEF group | ||||||||
| Q1 | Ref | - | Ref | - | Ref | - | Ref | - |
| Q2 | 0.62 (0.40–0.97) | 0.037 | 0.61 (0.39–0.96) | 0.033 | 0.63 (0.40–0.99) | 0.043 | 0.64 (0.41–1.01) | 0.056 |
| Q3 | 0.65 (0.42–1.02) | 0.059 | 0.63 (0.40–0.99) | 0.045 | 0.66 (0.42–1.03) | 0.068 | 0.72 (0.45–1.15) | 0.165 |
| Q4 | 0.56 (0.34–0.91) | 0.020 | 0.54 (0.33–0.89) | 0.016 | 0.56 (0.34–0.93) | 0.024 | 0.64 (0.38–1.07) | 0.086 |
| Q5 | 0.43 (0.024–0.75) | 0.003 | 0.43 (0.24–0.77) | 0.004 | 0.42 (0.23–0.76) | 0.004 | 0.49 (0.26–0.92) | 0.027 |
| P for trend | - | 0.003 | - | 0.003 | - | 0.004 | - | 0.030 |
| P for non-linearity | - | 0.475 | - | 0.540 | - | 0.561 | - | 0.228 |
| LVEF linear (per 10%) | 0.76 (0.64–0.89) | 0.001 | 0.76 (0.64–0.90) | 0.002 | 0.75 (0.62–0.89) | 0.001 | 0.77 (0.64–0.93) | 0.006 |
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| HR (95%CI) | p Value | HR (95%CI) | p Value | HR (95%CI) | p Value | HR (95%CI) | p Value | |
| LVEDD group | ||||||||
| Q1 | 0.37 (0.21–0.63) | <0.001 | 0.36 (0.20–0.64) | <0.001 | 0.35 (0.19–0.63) | <0.001 | 0.39 (0.22–0.70) | 0.002 |
| Q2 | 0.57 (0.35–0.93) | 0.024 | 0.56 (0.34–0.92) | 0.023 | 0.56 (0.34–0.92) | 0.022 | 0.61 (0.36–1.02) | 0.058 |
| Q3 | 0.44 (0.28–0.69) | <0.001 | 0.40 (0.25–0.64) | <0.001 | 0.40 (0.25–0.63) | <0.001 | 0.41 (0.26–0.66) | <0.001 |
| Q4 | 0.59 (0.38–0.91) | 0.018 | 0.55 (0.36–0.86) | <0.001 | 0.54 (0.35–9.85) | 0.008 | 0.54 (0.35–0.85) | 0.008 |
| Q5 | Ref | - | Ref | - | Ref | - | Ref | - |
| P for trend | - | <0.001 | - | <0.001 | - | <0.001 | - | <0.001 |
| P for nonlinearity | - | 0.663 | - | 0.696 | - | 0.689 | - | 0.466 |
| LVEDD linear (per 10 mm) | 1.54 (1.30–1.82) | <0.001 | 1.56 (1.31–1.87) | <0.001 | 1.57 (1.31–1.88) | <0.001 | 1.54 (1.27–1.85) | <0.001 |
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| HR (95%CI) | p Value | HR (95%CI) | p Value | HR (95%CI) | p Value | HR (95%CI) | p Value | |
| LVEF group | ||||||||
| Q1 | Ref | - | Ref | - | Ref | - | Ref | - |
| Q2 | 1.50 (0.95–2.39) | 0.084 | 1.62 (1.00–2.60) | 0.049 | 1.55 (0.95–2.53) | 0.082 | 1.59 (0.97–2.60) | 0.064 |
| Q3 | 1.04 (0.63–1.72) | 0.878 | 1.19 (0.70–2.03) | 0.518 | 1.16 (0.69–1.96) | 0.567 | 1.21 (0.72–2.04) | 0.468 |
| Q4 | 1.20 (0.72–1.98) | 0.484 | 1.33 (0.79–2.25) | 0.287 | 1.24 (0.73–2.10) | 0.425 | 1.31 (0.77–2.20) | 0.320 |
| Q5 | 0.73 (0.41–1.27) | 0.263 | 0.81 (0.45–1.47) | 0.494 | 0.72 (0.40–1.32) | 0.289 | 0.77 (0.42–1.41) | 0.393 |
| P for trend | - | 0.475 | - | 0.796 | - | 0.590 | - | 0.761 |
| P for non-linearity | - | 0.233 | - | 0.161 | - | 0.165 | - | 0.148 |
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| HR (95%CI) | p Value | HR (95%CI) | p Value | HR (95%CI) | p Value | HR (95%CI) | p Value | |
| LVEDD group | ||||||||
| Q1 | 0.51 (0.29–0.90) | 0.021 | 0.59 (0.33–1.06) | 0.078 | 0.54 (0.30–0.96) | 0.037 | 0.55 (0.31–0.99) | 0.048 |
| Q2 | 0.49 (0.28–0.85) | 0.011 | 0.50 (0.29–0.89) | 0.017 | 0.46 (0.26–0.82) | 0.008 | 0.47 (0.26–0.85) | 0.013 |
| Q3 | 0.78 (0.51–1.20) | 0.265 | 0.84 (0.54–1.30) | 0.437 | 0.81 (0.53–1.24) | 0.335 | 0.83 (0.53–1.29) | 0.405 |
| Q4 | 0.81 (0.53–1.25) | 0.341 | 0.83 (0.54–1.29) | 0.409 | 0.77 (0.50–1.24) | 0.248 | 0.78 (0.50–1.20) | 0.260 |
| Q5 | Ref | - | Ref | - | Ref | - | Ref | - |
| P for trend | - | 0.004 | - | 0.019 | - | 0.008 | - | 0.014 |
| P for non-linearity | - | 0.325 | - | 0.424 | - | 0.464 | - | 0.446 |
| LVEDD linear (per 10 mm) | 1.28 (1.09–1.50) | 0.002 | 1.24 (1.04–1.46) | 0.012 | 1.29 (1.08–1.53) | 0.004 | 1.27 (1.06–1.52) | 0.008 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, S.; Deng, Y.; Huang, H.; Liu, X.; Yu, Y.; Chen, X.; Gu, M.; Niu, H.; Hua, W. Prognostic Implications of Left Ventricular Ejection Fraction and Left Ventricular End-Diastolic Diameter on Clinical Outcomes in Patients with ICD. J. Cardiovasc. Dev. Dis. 2022, 9, 421. https://doi.org/10.3390/jcdd9120421
Cheng S, Deng Y, Huang H, Liu X, Yu Y, Chen X, Gu M, Niu H, Hua W. Prognostic Implications of Left Ventricular Ejection Fraction and Left Ventricular End-Diastolic Diameter on Clinical Outcomes in Patients with ICD. Journal of Cardiovascular Development and Disease. 2022; 9(12):421. https://doi.org/10.3390/jcdd9120421
Chicago/Turabian StyleCheng, Sijing, Yu Deng, Hao Huang, Xi Liu, Yu Yu, Xuhua Chen, Min Gu, Hongxia Niu, and Wei Hua. 2022. "Prognostic Implications of Left Ventricular Ejection Fraction and Left Ventricular End-Diastolic Diameter on Clinical Outcomes in Patients with ICD" Journal of Cardiovascular Development and Disease 9, no. 12: 421. https://doi.org/10.3390/jcdd9120421
APA StyleCheng, S., Deng, Y., Huang, H., Liu, X., Yu, Y., Chen, X., Gu, M., Niu, H., & Hua, W. (2022). Prognostic Implications of Left Ventricular Ejection Fraction and Left Ventricular End-Diastolic Diameter on Clinical Outcomes in Patients with ICD. Journal of Cardiovascular Development and Disease, 9(12), 421. https://doi.org/10.3390/jcdd9120421





