The Association of Triglyceride to High-Density Lipoprotein Cholesterol Ratio with High-Risk Coronary Plaque Characteristics Determined by CT Angiography and Its Risk of Coronary Heart Disease
Abstract
1. Introduction
2. Materials and Methods
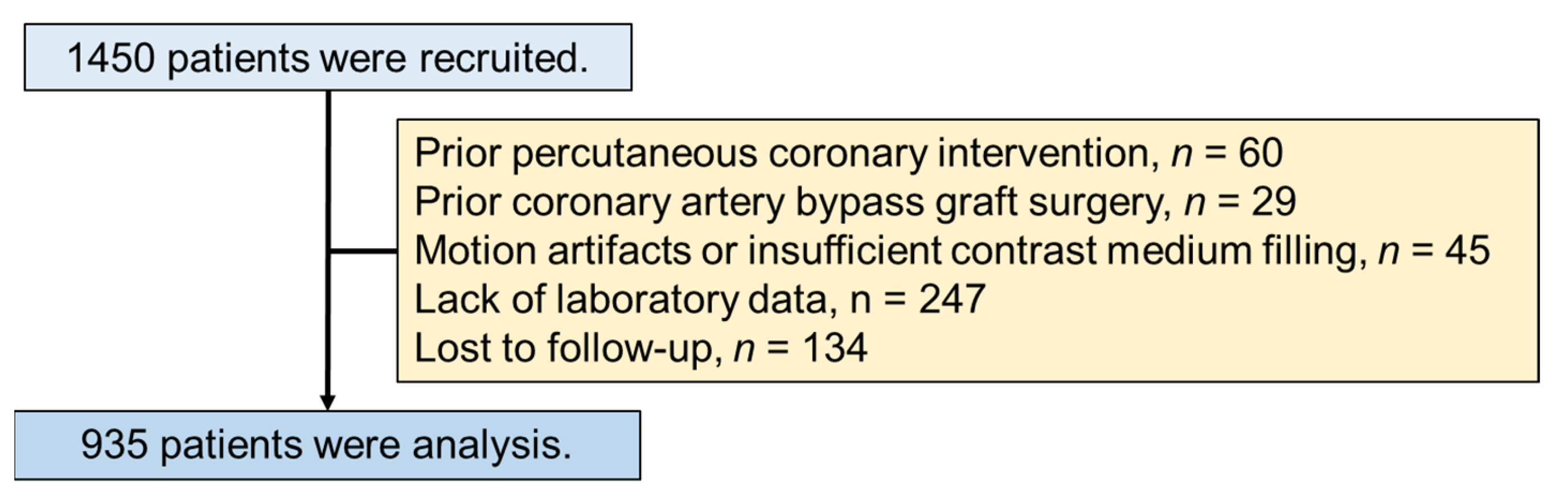
2.1. Study Population
2.2. Computed Tomography Image Acquisition
2.3. Coronary CT Angiography Analysis
2.4. Assessment of Other Risk Factors
2.5. Follow-Up Methods
2.6. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. CCTA Plaque Characteristics
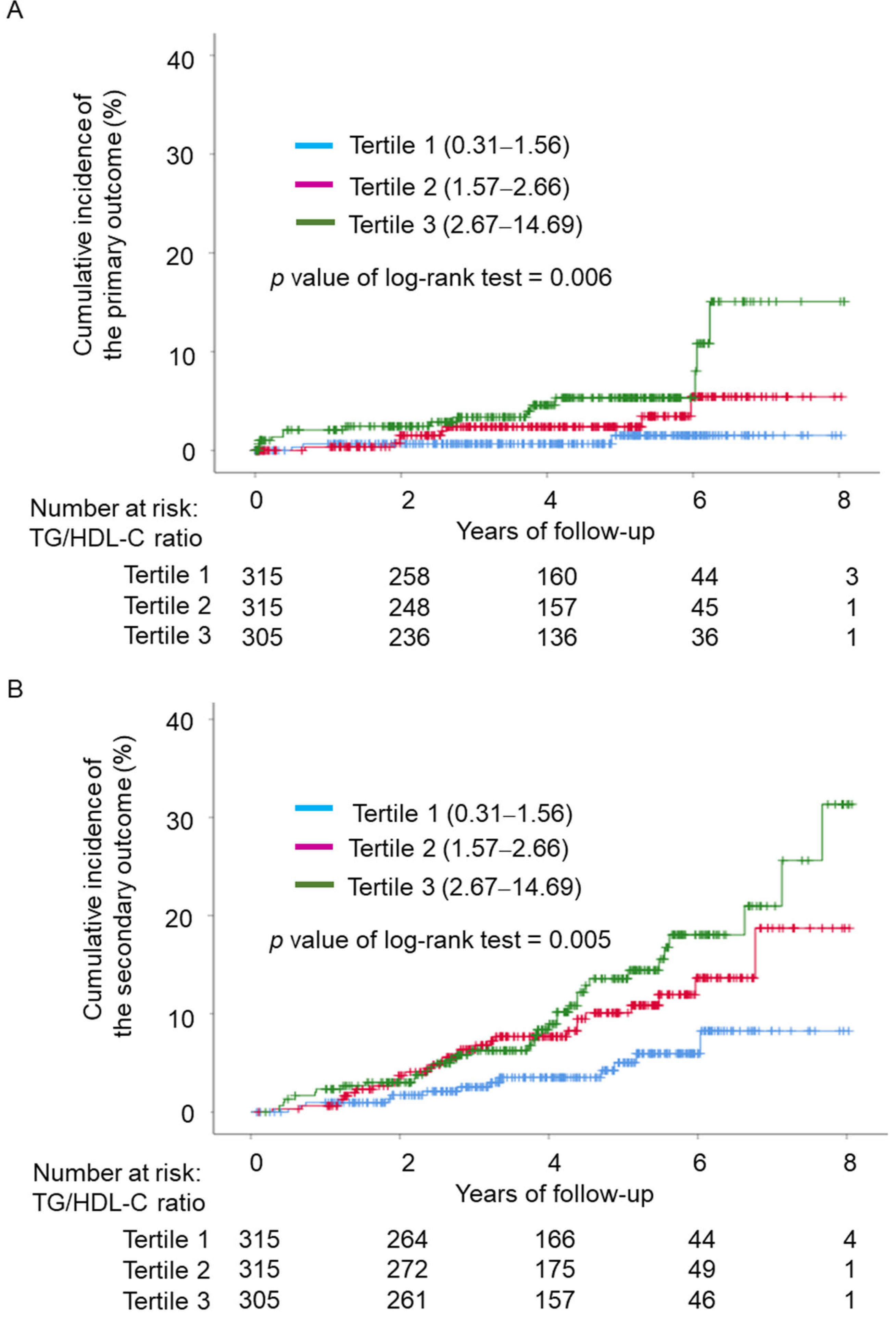
3.3. TG/HDL-C and Cardiovascular Events
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boekholdt, S.M.; Arsenault, B.J.; Mora, S.; Pedersen, T.R.; LaRosa, J.C.; Nestel, P.J.; Simes, R.J.; Durrington, P.; Hitman, G.A.; Welch, K.M.; et al. Association of LDL cholesterol, non-HDL cholesterol, and apolipoprotein B levels with risk of cardiovascular events among patients treated with statins: A meta-analysis. JAMA 2012, 307, 1302–1309. [Google Scholar] [CrossRef]
- Lewington, S.; Whitlock, G.; Clarke, R.; Sherliker, P.; Emberson, J.; Halsey, J.; Qizilbash, N.; Peto, R.; Collins, R. Blood cholesterol and vascular mortality by age, sex, and blood pressure: A meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet 2007, 370, 1829–1839. [Google Scholar] [CrossRef]
- Elshazly, M.B.; Quispe, R.; Michos, E.D.; Sniderman, A.D.; Toth, P.P.; Banach, M.; Kulkarni, K.R.; Coresh, J.; Blumenthal, R.S.; Jones, S.R.; et al. Patient-level discordance in population percentiles of the total cholesterol to high-density lipoprotein cholesterol ratio in comparison with low-density lipoprotein cholesterol and non-high-density lipoprotein cholesterol: The very large database of lipids study (VLDL-2B). Circulation 2015, 132, 667–676. [Google Scholar] [CrossRef]
- Aimo, A.; Chiappino, S.; Clemente, A.; Della Latta, D.; Martini, N.; Georgiopoulos, G.; Panichella, G.; Piagneri, V.; Storti, S.; Monteleone, A.; et al. The triglyceride/HDL cholesterol ratio and TyG index predict coronary atherosclerosis and outcome in the general population. Eur. J. Prev. Cardiol. 2022, 29, e203–e204. [Google Scholar] [CrossRef]
- Murguía-Romero, M.; Jiménez-Flores, J.R.; Sigrist-Flores, S.C.; Espinoza-Camacho, M.A.; Jiménez-Morales, M.; Piña, E.; Méndez-Cruz, A.R.; Villalobos-Molina, R.; Reaven, G.M. Plasma triglyceride/HDL-cholesterol ratio, insulin resistance, and cardiometabolic risk in young adults. J. Lipid Res. 2013, 54, 2795–2799. [Google Scholar] [CrossRef]
- Chen, Z.; Chen, G.; Qin, H.; Cai, Z.; Huang, J.; Chen, H.; Wu, W.; Chen, Z.; Wu, S.; Chen, Y. Higher triglyceride to high-density lipoprotein cholesterol ratio increases cardiovascular risk: 10-year prospective study in a cohort of Chinese adults. J. Diabetes Investig. 2020, 11, 475–481. [Google Scholar] [CrossRef]
- Yang, S.H.; Du, Y.; Li, X.L.; Zhang, Y.; Li, S.; Xu, R.X.; Zhu, C.G.; Guo, Y.L.; Wu, N.Q.; Qing, P.; et al. Triglyceride to high-density lipoprotein cholesterol ratio and cardiovascular events in diabetics with coronary artery disease. Am. J. Med. Sci. 2017, 354, 117–124. [Google Scholar] [CrossRef]
- Bittner, V.; Johnson, B.D.; Zineh, I.; Rogers, W.J.; Vido, D.; Marroquin, O.C.; Bairey-Merz, C.N.; Sopko, G. The triglyceride/high-density lipoprotein cholesterol ratio predicts all-cause mortality in women with suspected myocardial ischemia: A report from the Women’s Ischemia Syndrome Evaluation (WISE). Am. Heart J. 2009, 157, 548–555. [Google Scholar] [CrossRef]
- Sultani, R.; Tong, D.C.; Peverelle, M.; Lee, Y.S.; Baradi, A.; Wilson, A.M. Elevated triglycerides to high-density lipoprotein cholesterol (TG/HDL-C) ratio predicts long-term mortality in high-risk patients. Heart Lung Circ. 2020, 29, 414–421. [Google Scholar] [CrossRef]
- Motoyama, S.; Sarai, M.; Harigaya, H.; Anno, H.; Inoue, K.; Hara, T.; Naruse, H.; Ishii, J.; Hishida, H.; Wong, N.D.; et al. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J. Am. Coll. Cardiol. 2009, 54, 49–57. [Google Scholar] [CrossRef]
- Williams, M.C.; Moss, A.J.; Dweck, M.; Adamson, P.D.; Alam, S.; Hunter, A.; Shah, A.S.V.; Pawade, T.; Weir-McCall, J.R.; Roditi, G.; et al. Coronary artery Plaque Characteristics Associated with Adverse Outcomes in the SCOT-HEART Study. J. Am. Coll. Cardiol. 2019, 73, 291–301. [Google Scholar] [CrossRef]
- Ichikawa, K.; Miyoshi, T.; Osawa, K.; Miki, T.; Nakamura, K.; Ito, H. Prognostic value of coronary computed tomographic angiography in patients with nonalcoholic fatty liver disease. Cardiovasc. Imaging 2020, 13, 1628–1630. [Google Scholar] [CrossRef]
- Ichikawa, K.; Miyoshi, T.; Osawa, K.; Miki, T.; Toda, H.; Ejiri, K.; Yoshida, M.; Nakamura, K.; Morita, H.; Ito, H. Incremental prognostic value of non-alcoholic fatty liver disease over coronary computed tomography angiography findings in patients with suspected coronary artery disease. Eur. J. Prev. Cardiol. 2022, 28, 2059–2066. [Google Scholar] [CrossRef]
- Ichikawa, K.; Miyoshi, T.; Kotani, K.; Osawa, K.; Nakashima, M.; Nishihara, T.; Ito, H. Association between high oxidized high-density lipoprotein levels and increased pericoronary inflammation determined by coronary computed tomography angiography. J. Cardiol. 2022, in press. [Google Scholar] [CrossRef]
- Cerqueira, M.D.; Weissman, N.J.; Dilsizian, V.; Jacobs, A.K.; Kaul, S.; Laskey, W.K.; Pennell, D.J.; Rumberger, J.A.; Ryan, T.; Verani, M.S.; et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Int. J. Cardiovasc. Imaging 2002, 18, 539–542. [Google Scholar]
- Osawa, K.; Miyoshi, T.; Yamauchi, K.; Koyama, Y.; Nakamura, K.; Sato, S.; Kanazawa, S.; Ito, H. Nonalcoholic hepatic steatosis is a strong predictor of high-risk coronary-artery plaques as determined by multidetector CT. PLoS ONE 2015, 10, e0131138. [Google Scholar] [CrossRef]
- International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes: Response to the International Expert Committee. Diabetes Care 2009, 32, e159. [Google Scholar] [CrossRef]
- Suruga, K.; Miyoshi, T.; Kotani, K.; Ichikawa, K.; Miki, T.; Osawa, K.; Ejiri, K.; Toda, H.; Nakamura, K.; Morita, H.; et al. Higher oxidized high-density lipoprotein to apolipoprotein A-I ratio is associated with high-risk coronary plaque characteristics determined by CT angiography. Int. J. Cardiol. 2021, 324, 193–198. [Google Scholar] [CrossRef]
- Wan, K.; Zhao, J.; Huang, H.; Zhang, Q.; Chen, X.; Zeng, Z.; Zhang, L.; Chen, Y. The association between triglyceride/high-density lipoprotein cholesterol ratio and all-cause mortality in acute coronary syndrome after coronary revascularization. PLoS ONE 2015, 10, e0123521. [Google Scholar] [CrossRef]
- Thomsen, C.; Abdulla, J. Characteristics of high-risk coronary plaques identified by computed tomographic angiography and associated prognosis: A systematic review and meta-analysis. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 120–129. [Google Scholar] [CrossRef]
- Ichikawa, K.; Miyoshi, T.; Osawa, K.; Miki, T.; Morimitsu, Y.; Akagi, N.; Nakashima, M.; Ito, H. Association between higher pericoronary adipose tissue attenuation measured by coronary computed tomography angiography and nonalcoholic fatty liver disease: A matched case-control study. Medicine 2021, 100, e27043. [Google Scholar] [CrossRef]
- McLaughlin, T.; Reaven, G.; Abbasi, F.; Lamendola, C.; Saad, M.; Waters, D.; Simon, J.; Krauss, R.M. Is there a simple way to identify insulin-resistant individuals at increased risk of cardiovascular disease? Am. J. Cardiol. 2005, 96, 399–404. [Google Scholar] [CrossRef]
- Natali, A.; Baldi, S.; Bonnet, F.; Petrie, J.; Trifirò, S.; Tricò, D.; Mari, A.; RISC Investigators. Plasma HDL-cholesterol and triglycerides, but not LDL-cholesterol, are associated with insulin secretion in non-diabetic subjects. Metabolism 2017, 69, 33–42. [Google Scholar] [CrossRef]
- Burnett, J.R.; Hooper, A.J.; Hegele, R.A. Remnant cholesterol and atherosclerotic cardiovascular disease risk. J. Am. Coll. Cardiol. 2020, 76, 2736–2739. [Google Scholar] [CrossRef]
- Pantoja-Torres, B.; Toro-Huamanchumo, C.J.; Urrunaga-Pastor, D.; Guarnizo-Poma, M.; Lazaro-Alcantara, H.; Paico-Palacios, S.; Del Carmen Ranilla-Seguin, V.; Benites-Zapata, V.A.; Insulin Resistance and Metabolic Syndrome Research Group. High triglycerides to HDL-cholesterol ratio is associated with insulin resistance in normal-weight healthy adults. Diabetes Metab. Syndr. 2019, 13, 382–388. [Google Scholar] [CrossRef]
- Sekimoto, T.; Koba, S.; Mori, H.; Arai, T.; Matsukawa, N.; Sakai, R.; Yokota, Y.; Sato, S.; Tanaka, H.; Masaki, R.; et al. Impact of small dense low-density lipoprotein cholesterol on cholesterol crystals in patients with acute coronary syndrome: An optical coherence tomography study. J. Clin. Lipidol. 2022, 16, 438–446. [Google Scholar] [CrossRef]
- Salazar, M.R.; Carbajal, H.A.; Espeche, W.G.; Aizpurúa, M.; Leiva Sisnieguez, C.E.; March, C.E.; Balbín, E.; Stavile, R.N.; Reaven, G.M. Identifying cardiovascular disease risk and outcome: Use of the plasma triglyceride/high-density lipoprotein cholesterol concentration ratio versus metabolic syndrome criteria. J. Intern. Med. 2013, 273, 595–601. [Google Scholar] [CrossRef]
- Vega, G.L.; Barlow, C.E.; Grundy, S.M.; Leonard, D.; DeFina, L.F. Triglyceride-to-high-density-lipoprotein-cholesterol ratio is an index of heart disease mortality and of incidence of type 2 diabetes mellitus in men. J. Investig. Med. 2014, 62, 345–349. [Google Scholar] [CrossRef]
- Pacifico, L.; Bonci, E.; Andreoli, G.; Romaggioli, S.; Di Miscio, R.; Lombardo, C.V.; Chiesa, C. Association of serum triglyceride-to-HDL cholesterol ratio with carotid artery intima-media thickness, insulin resistance and nonalcoholic fatty liver disease in children and adolescents. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 737–743. [Google Scholar] [CrossRef]
- Nakanishi, R.; Ceponiene, I.; Osawa, K.; Luo, Y.; Kanisawa, M.; Megowan, N.; Nezarat, N.; Rahmani, S.; Broersen, A.; Kitslaar, P.H.; et al. Plaque progression assessed by a novel semi-automated quantitative plaque software on coronary computed tomography angiography between diabetes and non-diabetes patients: A propensity-score matching study. Atherosclerosis 2016, 255, 73–79. [Google Scholar] [CrossRef]
- Kammerlander, A.A.; Mayrhofer, T.; Ferencik, M.; Pagidipati, N.J.; Karady, J.; Ginsburg, G.S.; Lu, M.T.; Bittner, D.O.; Puchner, S.B.; Bihlmeyer, N.A.; et al. Association of metabolic phenotypes with coronary artery disease and cardiovascular events in patients with stable chest pain. Diabetes Care 2021, 44, 1038–1045. [Google Scholar] [CrossRef]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines. Circulation 2019, 140, e596–e646. [Google Scholar] [CrossRef]
- Jakob, T.; Nordmann, A.J.; Schandelmaier, S.; Ferreira-González, I.; Briel, M. Fibrates for primary prevention of cardiovascular disease events. Cochrane Database Syst. Rev. 2016, 11, CD009753. [Google Scholar] [CrossRef]
- Gulati, M.; Levy, P.D.; Mukherjee, D.; Amsterdam, E.; Bhatt, D.L.; Birtcher, K.K.; Blankstein, R.; Boyd, J.; Bullock-Palmer, R.P.; Conejo, T.; et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021, 144, e368–e454. [Google Scholar] [CrossRef]
- SCOT-HEART Investigators; Newby, D.E.; Adamson, P.D.; Berry, C.; Boon, N.A.; Dweck, M.R.; Flather, M.; Forbes, J.; Hunter, A.; Lewis, S.; et al. Coronary CT Angiography and 5-Year Risk of Myocardial Infarction. N. Engl. J. Med. 2018, 379, 924–933. [Google Scholar] [CrossRef]
| TG/HDL Ratio | |||||
|---|---|---|---|---|---|
| All | Tertile 1 (0.31–1.56) | Tertile 2 (1.57–2.66) | Tertile 3 (2.67–14.69) | p Value for Trend | |
| n | 935 | 315 | 315 | 305 | |
| Age, years | 64 ± 14 | 63 ± 15 | 64 ± 15 | 63 ± 12 | 0.436 |
| Male | 516 (55) | 152 (48) | 164 (52) | 200 (55) | <0.001 |
| BMI, kg/m2 | 23.8 ± 4.0 | 22.6 ± 3.9 | 23.7 ± 4.1 | 25.1 ± 3.5 | <0.001 |
| Hypertension | 552 (59) | 159 (21) | 187 (59) | 206 (67) | <0.001 |
| Dyslipidemia | 472 (50) | 129 (41) | 153 (48) | 190 (62) | <0.001 |
| Diabetes mellitus | 306 (33) | 84 (27) | 103 (32) | 123 (40) | 0.001 |
| Current smoking | 211 (23) | 53 (17) | 68 (22) | 90 (29) | <0.001 |
| LDL-C, mg/dL | 114 ± 31 | 107 ± 27 | 114 ± 32 | 121 ± 32 | <0.001 |
| TG, mg/dL | 111 (2, 161) | 73 (59, 88] | 111 (96, 129] | 207 ± 79 | <0.001 |
| HDL-C, mg/dL | 58 ± 16 | 71 ± 16 | 56 ± 11 | 46 ± 10 | <0.001 |
| TG/HDL-C | 1.98 (1.30, 3.16) | 1.08 (0.83, 1.31) | 2.00 (1.79, 2.27) | 3.94 [3.18–5.25] | <0.001 |
| HemoglobinA1c, % | 6.3 ± 1.2 | 6.1 ± 1.0 | 6.3 ± 1.2 | 6.4 ± 1.3 | <0.001 |
| eGFR, mL/min/1.73 m2 | 69.7 ± 18 | 71.1 ± 19.0 | 68.4 ± 17.5 | 68.9 ± 16.7 | 0.154 |
| Medications | |||||
| Statins | 318 (34) | 92 (29) | 112 (35) | 114 (37) | 0.078 |
| ACEIs or ARBs | 355 (38) | 102 (32) | 127 (40) | 126 (41) | 0.042 |
| CCBs | 317 (34) | 95 (30) | 109 (35) | 113 (37) | 0.184 |
| Antidiabetic agents | 196 (23) | 46 (15) | 61 (20) | 89 (29) | <0.001 |
| TG/HDL Ratio | |||||
|---|---|---|---|---|---|
| All | Tertile (0.31–1.56) | Tertile 2 (1.57–2.66) | Tertile 3 (2.67–14.69) | p Value for Trend | |
| n | 935 | 315 | 315 | 305 | |
| Calcified plaque | 608 (65) | 201(56) | 206 (65) | 219 (72) | 0.002 |
| Non-calcified plaque | 462 (49) | 129 (41) | 159 (51) | 174 (57) | <0.001 |
| Positive remodeling | 373 (40) | 95 (30) | 132 (42) | 146 (48) | <0.001 |
| Low density plaque | 277 (30) | 66 (21) | 100 (31) | 111 (36) | <0.001 |
| Spotty calcification | 77 (24) | 108 (34) | 108 (34) | 120 (39) | <0.001 |
| High risk plaque | 136 (15) | 27 (9) | 45 (14) | 64 (21) | <0.001 |
| Significant stenosis | 193 (21) | 53 (17) | 63 (20) | 77 (25) | 0.033 |
| Agatston score | 20 (0, 245) | 5 (0, 210) | 33 (0, 286) | 26 (0, 225) | 0.016 |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p Value | Odds Ratio (95% CI) | p Value | |
| Log TG/HDL-C | 2.009 (1.514–2.666) | <0.001 | 1.581 (1.150–2.173) | 0.005 |
| LDL-C | 0.999 (0.994–1.005) | 0.085 | – | – |
| Age, per year | 1.032 (1.016–1.048) | <0.001 | 1.029 (1.011–1.048) | 0.002 |
| Male | 2.917 (1.925–4.422) | <0.001 | 2.797 (1.773–4.412) | <0.001 |
| Hypertension | 2.543 (1.673–3.876) | <0.001 | 1.129 (0.654–1.949) | 0.664 |
| Dyslipidemia | 1.981 (1.358–2.892) | <0.001 | 1.472 (0.879–2.465) | 0.142 |
| Diabetes mellitus | 1.998 (1.382–2.889) | <0.001 | 1.460 (0.803–2.655) | 0.214 |
| Current smoking | 1.530 (1.020–2.296) | 0.040 | 1.050 (0.655–1.657) | 0.834 |
| Statin | 1.598 (1.103–2.313) | 0.013 | 1.126 (0.682–1.857) | 0.643 |
| ACEIs or ARBs | 2.534 (1.751–3.668) | <0.001 | 1.889 (1.192–2.992) | 0.007 |
| CCB | 1.665 (1.151–2.409) | 0.007 | 1.079 (0.695–1.675) | 0.734 |
| Antidiabetic agents | 2.110 (1.414–3.147) | <0.001 | 1.032 (0.537–1.981) | 0.925 |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p Value | Odds Ratio (95% CI) | p Value | |
| Log TG/HDL-C | 1.551 (1.185–1.927) | <0.001 | 1.183 (0.893–1.568) | 0.242 |
| LDL-C | 1.000 (0.995–1.00) | 0.981 | – | – |
| Age, per year | 1.051 (1.035–1.067) | <0.001 | 1.055 (1.036–1.074) | <0.001 |
| Male | 2.829 (1.988–4.026) | <0.001 | 3.075 (2.064–4.580) | <0.001 |
| Hypertension | 2.051 (1.451–2.898) | <0.001 | 0.980 (0.617–1.557) | 0.932 |
| Dyslipidemia | 2.214 (1.591–3.082) | <0.001 | 2.116 (1.340–3.342) | 0.001 |
| Diabetes mellitus | 2.017 (1.459–2.789) | <0.001 | 1.390 (0.811–2.381) | 0.231 |
| Current smoking | 1.399 (0.975–2.009) | 0.069 | 1.043 (0.687–1.583) | 0.843 |
| Statins | 1.628 (1.177–2.251) | 0.003 | 0.898 (0.574–1.694) | 0.639 |
| ACEIs or ARBs | 1.704 (1.237–2.346) | <0.001 | 1.128 (0.751–1.694) | 0.562 |
| CCB | 1.778 (1.286–2.457) | <0.001 | 1.442 (0.969–2.147) | 0.071 |
| Antidiabetic agents | 2.106 (1.472–3.013) | <0.001 | 1.182 (0.653–2.139) | 0.581 |
| Univariate Analysis | Multivariate Analysis: Model 1 | Multivariate Analysis: Model 2 | ||||
|---|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value | |
| TG/HDL-C ratio | ||||||
| Tertile 1 (0.31–1.56) | reference | − | reference | − | reference | − |
| Tertile 2 (1.57–2.66) | 2.733 (0.725–10.305) | 0.138 | 2.339 (0.614–8.961) | 0.213 | 2.308 (0.601–8.868) | 0.223 |
| Tertile 3 (2.67–14.69) | 5.545 (1.605–19.159) | 0.007 | 3.752 (1.043–13.501) | 0.043 | 3.295 (0.994–12.003) | 0.071 |
| LDL-C, per 1 mg/dL | 1.006 (0.994–1.018) | 0.337 | 1.006 (0.993–1.020) | 0.361 | 1.007 (0.994–1.020) | 0.312 |
| Age, per year | 1.019 (0.987–1.053) | 0.248 | 1.018 (0.981–1.056) | 0.355 | 1.013 (0.976–1.051) | 0.506 |
| Male | 2.349 (1.013–5.448) | 0.047 | 1.452 (0.585–3.608) | 0.421 | 1.212 (0.478–3.075) | 0.686 |
| Hypertension | 3.039 (1.146–8.060) | 0.026 | 1.961 (0.698–5.509) | 0.201 | 1.822 (0.650–5.102) | 0.254 |
| Dyslipidemia | 1.606 (0.728–3.539) | 0.240 | − | − | − | − |
| Diabetes mellitus | 3.204 (1.452–7.073) | 0.004 | 2.707 (1.178–6.233) | 0.019 | 2.342 (1.009–5.440) | 0.048 |
| Current smoking | 2.283 (1.033–5.045) | 0.041 | 1.791 (0.749–4.278) | 0.190 | 1.947 (0.817–4.639) | 0.132 |
| Statins | 1.028 (0.458–2.306) | 0.947 | 0.720 (0.309–1.679) | 0.447 | 0.888 (0.387–2.037) | 0.779 |
| ACEIs or ARBs | 2.731 (1.238–6.024) | 0.013 | − | − | − | − |
| CCBs | 1.712 (0.782–3.745) | 0.178 | − | − | − | − |
| Antidiabetic agents | 2.237 (1.013–4.938) | 0.046 | − | − | − | − |
| High-risk plaque | 2.952 (1.283–6.794) | 0.011 | − | − | 1.625 (0.645–4.091) | 0.303 |
| Significant stenosis | 3.552 (1.566–8.058) | 0.002 | − | − | 1.853 (0.731–4.678) | 0.192 |
| Univariate Analysis | Multivariate Analysis: Model 1 | Multivariate Analysis: Model 2 | ||||
|---|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value | |
| TG/HDL-C ratio | ||||||
| Tertile 1 (0.31–1.56) | reference | − | reference | − | reference | − |
| Tertile 2 (1.57–2.66) | 2.133 (1.109–4.103) | 0.023 | 1.843 (0.950–3.578) | 0.071 | 1.762 (0.906–3.427) | 0.095 |
| Tertile 3 (2.67–14.69) | 2.754 (1.459–5.200) | 0.002 | 2.085 (1.075–4.046) | 0.030 | 1.884 (0.964–3.681) | 0.064 |
| LDL-C, per 1 mg/dL | 1.003 (0.996–1.011) | 0.356 | 1.005 (0.997–1.012) | 0.257 | 1.004 (0.996–1.012) | 0.319 |
| Age, per year | 1.032 (1.011–1.053) | 0.003 | 1.033 (1.010–1.056) | 0.004 | 1.027 (1.004–1.051) | 0.021 |
| Male | 2.311 (1.411–2.786) | <0.001 | 1.858 (1.083–3.186) | 0.024 | 1.539 (0.887–2.669) | 0.125 |
| Hypertension | 1.740 (1.062–2.850) | 0.028 | 1.211 (0.711–2.063) | 0.480 | 1.118 (0.656–1.907) | 0.682 |
| Dyslipidemia | 1.377 (0.874–2.167) | 0.168 | − | − | − | − |
| Diabetes mellitus | 1.947 (1.249–3.036) | 0.003 | 1.750 (1.099–2.789) | 0.019 | 1.642 (1.027–2.625) | 0.038 |
| Current smoking | 1.875 (1.176–2.990) | 0.008 | 1.552 (0.945–2.547) | 0.082 | 1.552 (0.945–2.555) | 0.083 |
| Statins | 1.690 (1.225–2.331) | <0.001 | 0.837 (0.508–1.379) | 0.485 | 0.798 (0.483–1.318) | 0.378 |
| ACEIs or ARBs | 1.791 (1.149–2.793) | 0.010 | − | − | − | − |
| CCBs | 1.856 (1.190–2.895) | 0.006 | − | − | − | − |
| Antidiabetic agents | 1.454 (0.887–2.385) | 0.138 | − | − | − | − |
| High-risk plaque | 3.033 (1.901–4.840) | <0.001 | − | − | 1.741 (1.041–2.910) | 0.034 |
| Significant stenosis | 2.979 (1.897–4.676) | <0.001 | − | − | 1.706 (1.029–2.828) | 0.038 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koide, Y.; Miyoshi, T.; Nishihara, T.; Nakashima, M.; Ichikawa, K.; Miki, T.; Osawa, K.; Ito, H. The Association of Triglyceride to High-Density Lipoprotein Cholesterol Ratio with High-Risk Coronary Plaque Characteristics Determined by CT Angiography and Its Risk of Coronary Heart Disease. J. Cardiovasc. Dev. Dis. 2022, 9, 329. https://doi.org/10.3390/jcdd9100329
Koide Y, Miyoshi T, Nishihara T, Nakashima M, Ichikawa K, Miki T, Osawa K, Ito H. The Association of Triglyceride to High-Density Lipoprotein Cholesterol Ratio with High-Risk Coronary Plaque Characteristics Determined by CT Angiography and Its Risk of Coronary Heart Disease. Journal of Cardiovascular Development and Disease. 2022; 9(10):329. https://doi.org/10.3390/jcdd9100329
Chicago/Turabian StyleKoide, Yuji, Toru Miyoshi, Takahiro Nishihara, Mitsutaka Nakashima, Keishi Ichikawa, Takashi Miki, Kazuhiro Osawa, and Hiroshi Ito. 2022. "The Association of Triglyceride to High-Density Lipoprotein Cholesterol Ratio with High-Risk Coronary Plaque Characteristics Determined by CT Angiography and Its Risk of Coronary Heart Disease" Journal of Cardiovascular Development and Disease 9, no. 10: 329. https://doi.org/10.3390/jcdd9100329
APA StyleKoide, Y., Miyoshi, T., Nishihara, T., Nakashima, M., Ichikawa, K., Miki, T., Osawa, K., & Ito, H. (2022). The Association of Triglyceride to High-Density Lipoprotein Cholesterol Ratio with High-Risk Coronary Plaque Characteristics Determined by CT Angiography and Its Risk of Coronary Heart Disease. Journal of Cardiovascular Development and Disease, 9(10), 329. https://doi.org/10.3390/jcdd9100329






