The Acute-Phase Ambulation Program Improves Clinical Outcome for Acute Heart Failure
Abstract
1. Introduction
2. Methods
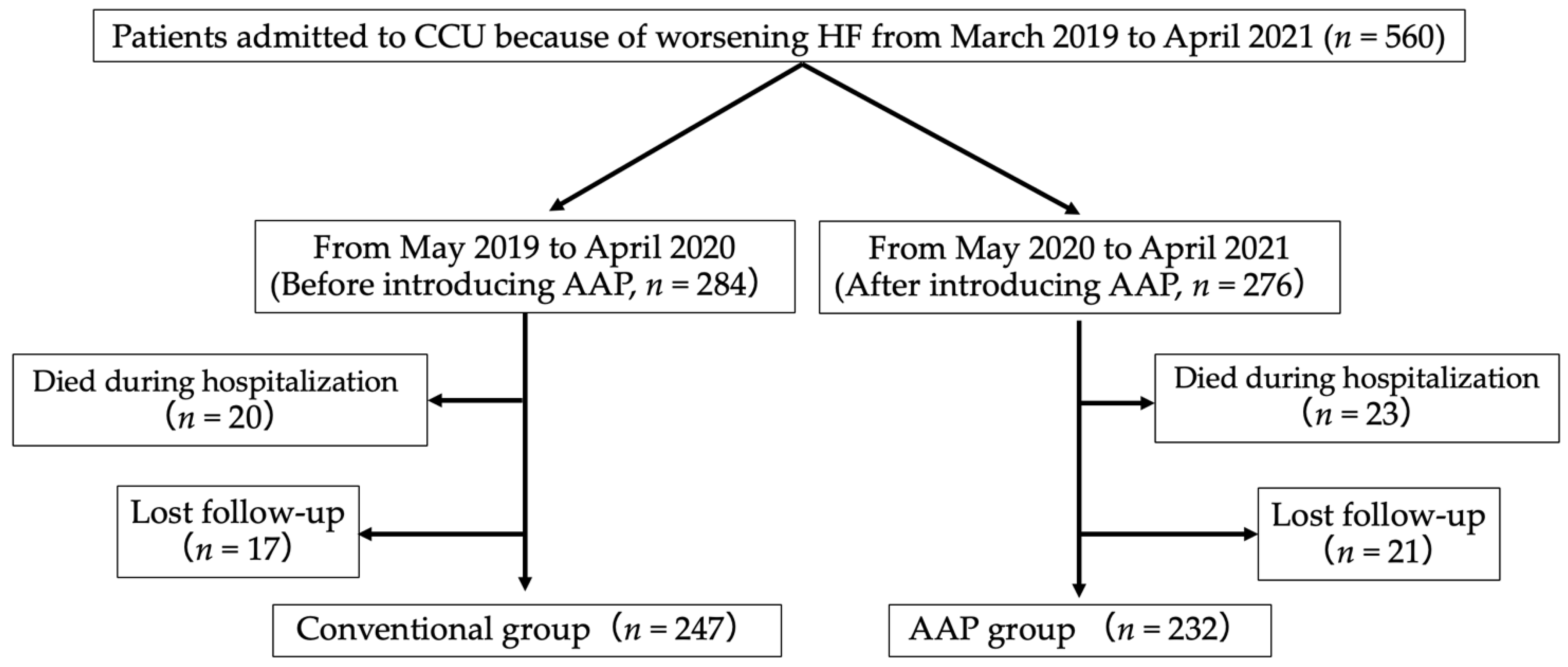
2.1. Patients
2.2. Primary Events and Clinical Characteristics
2.3. Statistical Analysis
3. Results
3.1. Patients’ Clinical Characteristics and Primary Events
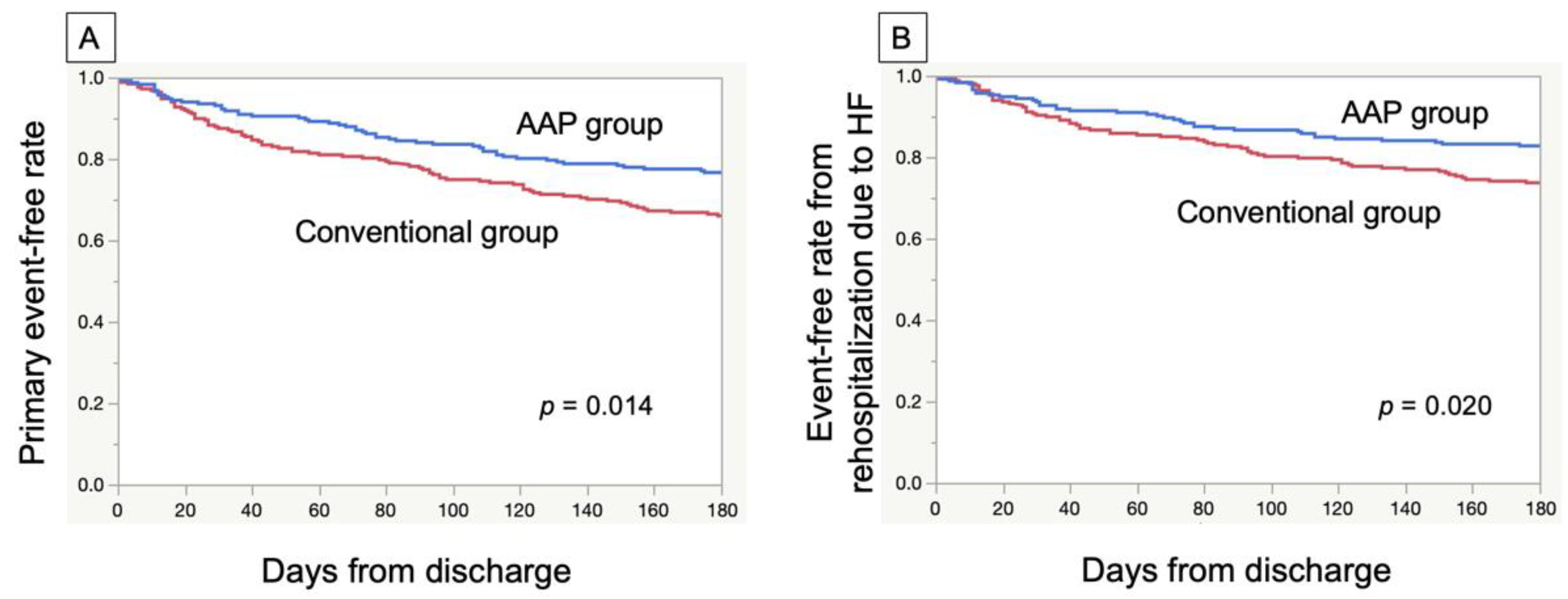
3.2. Survival Analyses
3.3. Univariate and Multivariate Analyses
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shiba, N.; Shimokawa, H. Chronic Heart Failure in Japan: Implications of the CHART Studies. Vasc. Health Risk Manag. 2008, 4, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, Y.; Kohsaka, S.; Sato, N.; Takano, T.; Kitai, T.; Yoshikawa, T.; Matsue, Y. 9-Year Trend in the Management of Acute Heart Failure in Japan: A Report from the National Consortium of Acute Heart Failure Registries. J. Am. Heart Assoc. 2018, 7, e008687. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, T.; Kitai, T.; Miyamoto, T.; Kagiyama, N.; Okumura, T.; Kida, K.; Oishi, S.; Akiyama, E.; Suzuki, S.; Yamamoto, M.; et al. Effect of Optimizing Guideline-Directed Medical Therapy Before Discharge on Mortality and Heart Failure Readmission in Patients Hospitalized with Heart Failure with Reduced Ejection Fraction. Am. J. Cardiol. 2018, 121, 969–974. [Google Scholar] [CrossRef] [PubMed]
- Lamberti, V.; Palermi, S.; Franceschin, A.; Scapol, G.; Lamberti, V.; Lamberti, C.; Vecchiato, M.; Spera, R.; Sirico, F.; Della Valle, E. The Effectiveness of Adapted Personalized Motor Activity (AMPA) to Improve Health in Individuals with Mental Disorders and Physical Comorbidities: A Randomized Controlled Trial. Sports 2022, 10, 30. [Google Scholar] [CrossRef] [PubMed]
- Compagno, S.; Palermi, S.; Pescatore, A.V.; Brugin, E.; Sarto, M.; Marin, R.; Manuele, C.; Moreno, N.; Accurso, S.; Alessandro, A.; et al. Physical and Psychological Reconditioning in Long COVID Syndrome: Results of an out-of-Hospital Exercise and Psychological-Based Rehabilitation Program. IJC Heart Vasc. 2022, 41, 101080. [Google Scholar] [CrossRef] [PubMed]
- Long, L.; Mordi, I.R.; Bridges, C.; Sagar, V.; Davies, E.J.; Coats, A.J.; Dalal, H.; Rees, K.; Singh, S.J.; Taylor, R.S. Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst. Rev. 2019, 1, CD003331. [Google Scholar] [CrossRef] [PubMed]
- Kamiya, K.; Sato, Y.; Takahashi, T.; Tsuchihashi-Makaya, M.; Kotooka, N.; Ikegame, T.; Takura, T.; Yamamoto, T.; Nagayama, M.; Goto, Y.; et al. Multidisciplinary Cardiac Rehabilitation and Long-Term Prognosis in Patients with Heart Failure. Circ. Heart Fail. 2020, 13, e006798. [Google Scholar] [CrossRef] [PubMed]
- Pearson, M.J.; Smart, N.A. Exercise therapy and autonomic function in heart failure patients: A systematic review and meta-analysis. Heart Fail. Rev. 2017, 23, 91–108. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.L.; Poole-Wilson, P.A.; Coats, A.J. Exercise limitation in chronic heart failure: Central role of the periphery. J. Am. Coll. Cardiol. 1996, 28, 1092–1102. [Google Scholar] [CrossRef]
- Drexler, H.; Riede, U.; Münzel, T.; König, H.; Funke, E.; Just, H. Alterations of skeletal muscle in chronic heart failure. Circulation 1992, 85, 1751–1759. [Google Scholar] [CrossRef] [PubMed]
- Izawa, H.; Yoshida, T.; Ikegame, T.; Izawa, K.P.; Ito, Y.; Okamura, H.; Osada, N.; Kinugawa, S.; Kubozono, T.; Kono, Y.; et al. Standard Cardiac Rehabilitation Program for Heart Failure. Circ. J. 2019, 83, 2394–2398. [Google Scholar] [CrossRef]
- Morris, P.E.; Goad, A.; Thompson, C.; Taylor, K.; Harry, B.; Passmore, L.; Ross, A.; Anderson, L.; Baker, S.; Sanchez, M.; et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure*. Crit. Care Med. 2008, 36, 2238–2243. [Google Scholar] [CrossRef] [PubMed]
- Schweickert, W.D.; Pohlman, M.C.; Pohlman, A.S.; Nigos, C.; Pawlik, A.J.; Esbrook, C.L.; Spears, L.; Miller, M.; Franczyk, M.; Deprizio, D.; et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. Lancet 2009, 373, 1874–1882. [Google Scholar] [CrossRef]
- Kakutani, N.; Fukushima, A.; Kinugawa, S.; Yokota, T.; Oikawa, T.; Nishikawa, M.; Nakamura, R.; Tsukada, T.; Mori, S.; Yoshida, I.; et al. Progressive Mobilization Program for Patients with Acute Heart Failure Reduces Hospital Stay and Improves Clinical Outcome. Circ. Rep. 2019, 1, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Burtin, C.; Clerckx, B.; Robbeets, C.; Ferdinande, P.; Langer, D.; Troosters, T.; Hermans, G.; Decramer, M.; Gosselink, R. Early exercise in critically ill patients enhances short-term functional recovery*. Crit. Care Med. 2009, 37, 2499–2505. [Google Scholar] [CrossRef] [PubMed]
- Hülsmann, M.; Quittan, M.; Berger, R.; Crevenna, R.; Springer, C.; Nuhr, M.; Mörtl, D.; Moser, P.; Pacher, R. Muscle strength as a predictor of long-term survival in severe congestive heart failure. Eur. J. Heart Fail. 2004, 6, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Jonkman, N.H.; Westland, H.; Groenwold, R.H.H.; Ågren, S.; Atienza, F.; Blue, L.; Bruggink-André de la Porte, P.W.F.; DeWalt, D.A.; Hebert, P.L.; Heisler, M.; et al. Do Self-Management Interventions Work in Patients with Heart Failure? An Individual Patient Data Meta-Analysis. Circulation. 2016, 133, 1189–1198. [Google Scholar] [CrossRef] [PubMed]
- Tohyama, T.; Ide, T.; Ikeda, M.; Kaku, H.; Enzan, N.; Matsushima, S.; Funakoshi, K.; Kishimoto, J.; Todaka, K.; Tsutsui, H. Machine learning-based model for predicting 1 year mortality of hospitalized patients with heart failure. ESC Heart Fail. 2021, 8, 4077–4085. [Google Scholar] [CrossRef] [PubMed]
- Opasich, C.; Pinna, G.D.; Bobbio, M.; Sisti, M.; Demichelis, B.; Febo, O.; Forni, G.; Riccardi, R.; Riccardi, P.G.; Capomolla, S.; et al. Peak Exercise Oxygen Consumption in Chronic Heart Failure: Toward Efficient Use in the Individual Patient. J. Am. Coll. Cardiol. 1998, 31, 766–775. [Google Scholar] [CrossRef]
| Conventional Group (n = 247) | AAP Group (n = 232) | p-Value | |
|---|---|---|---|
| Age (IQR) | 78 (70–85) | 78 (70–84) | 0.808 |
| Male (%) | 149 (60) | 143 (61) | 0.768 |
| Ischemic cardiomyopathy (%) | 51 (20) | 47 (20) | 0.917 |
| Atrial fibrillation (%) | 124 (50) | 96 (41) | 0.052 |
| Hypertension (%) | 168 (68) | 164 (70) | 0.526 |
| Diabetes (%) | 97 (39) | 89 (38) | 0.838 |
| Dyslipidemia (%) | 102 (41) | 93 (40) | 0.788 |
| Chronic kidney disease (%) | 195 (78) | 172 (74) | 0.214 |
| History of hospitalization due to Heart failure (%) | 122 (49) | 93 (40) | 0.041 * |
| BMI (IQR) | 22.2 (19.6–25.3) | 23.1 (20.8–25.6) | 0.045 * |
| SBP at admission (IQR) | 147 (124–169) | 142 (123–164) | 0.561 |
| HR at admission (IQR) | 102 (85–119) | 95 (80–115) | 0.028 |
| LVEF (IQR) | 36 (27–51) | 40 (30–54) | 0.063 |
| Serum hemoglobin (IQR) | 11.7 (10.2–13.3) | 11.6 (9.8–13.4) | 0.835 |
| Serum total protein (IQR) | 6.4 (5.9–6.8) | 6.4 (5.9–6.8) | 0.998 |
| NT-proBNP (IQR) | 5991 (2884–12371) | 5491 (2932–13449) | 0.804 |
| Medicine at discharge (%) | |||
| ACE inhibitor or ARB | 115 (47) | 123 (53) | 0.158 |
| Beta blocker | 171 (69) | 155 (67) | 0.570 |
| Diuretics | 204 (83) | 187 (80) | 0.575 |
| Statin | 95 (38) | 98 (42) | 0.399 |
| MRA | 153 (62) | 130 (56) | 0.189 |
| SGLT2 inhibitor | 10 (4) | 33 (14) | 0.001 * |
| ARNI | 0 (0) | 5 (2) | 0.007 * |
| Hazard Ratio | p | |
|---|---|---|
| Univariable | 0.58 (0.39–0.88) | 0.010 * |
| Multivariable | 0.62 (0.41–0.95) | 0.028 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Funato, Y.; Kono, Y.; Kawai, H.; Hoshino, M.; Yamada, A.; Muramatsu, T.; Harada, M.; Takahashi, H.; Otaka, Y.; Yanase, M.; et al. The Acute-Phase Ambulation Program Improves Clinical Outcome for Acute Heart Failure. J. Cardiovasc. Dev. Dis. 2022, 9, 314. https://doi.org/10.3390/jcdd9100314
Funato Y, Kono Y, Kawai H, Hoshino M, Yamada A, Muramatsu T, Harada M, Takahashi H, Otaka Y, Yanase M, et al. The Acute-Phase Ambulation Program Improves Clinical Outcome for Acute Heart Failure. Journal of Cardiovascular Development and Disease. 2022; 9(10):314. https://doi.org/10.3390/jcdd9100314
Chicago/Turabian StyleFunato, Yusuke, Yuji Kono, Hideki Kawai, Meiko Hoshino, Akira Yamada, Takashi Muramatsu, Masahide Harada, Hiroshi Takahashi, Yohei Otaka, Masanobu Yanase, and et al. 2022. "The Acute-Phase Ambulation Program Improves Clinical Outcome for Acute Heart Failure" Journal of Cardiovascular Development and Disease 9, no. 10: 314. https://doi.org/10.3390/jcdd9100314
APA StyleFunato, Y., Kono, Y., Kawai, H., Hoshino, M., Yamada, A., Muramatsu, T., Harada, M., Takahashi, H., Otaka, Y., Yanase, M., & Izawa, H. (2022). The Acute-Phase Ambulation Program Improves Clinical Outcome for Acute Heart Failure. Journal of Cardiovascular Development and Disease, 9(10), 314. https://doi.org/10.3390/jcdd9100314






