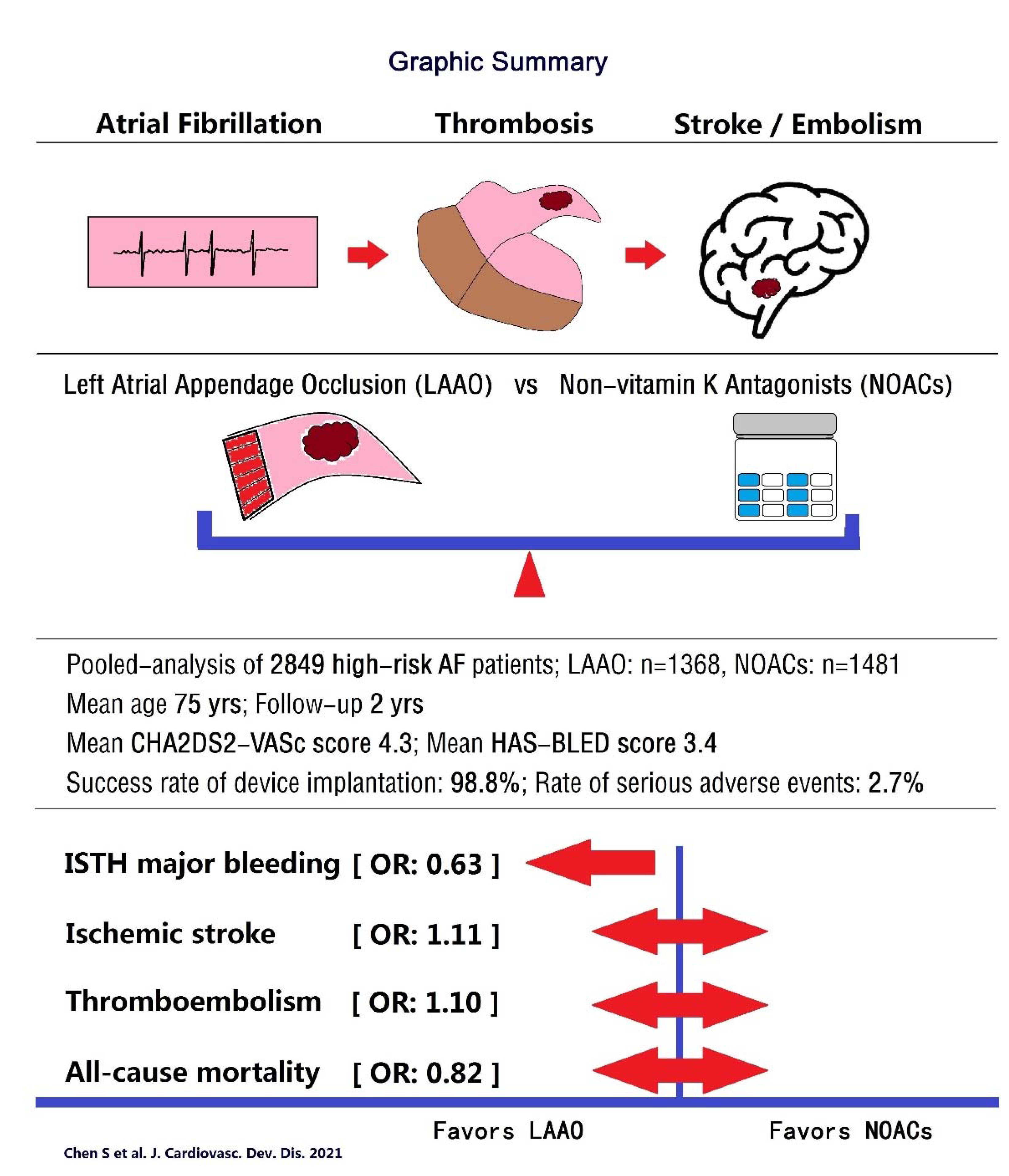
Comparison of Left Atrial Appendage Occlusion versus Non-Vitamin-K Antagonist Oral Anticoagulation in High-Risk Atrial Fibrillation: An Update
Abstract
1. Introduction
2. Methods
Data Collection and Quality Assessment
3. Statistical Analysis
4. Results
4.1. Baseline Characteristics
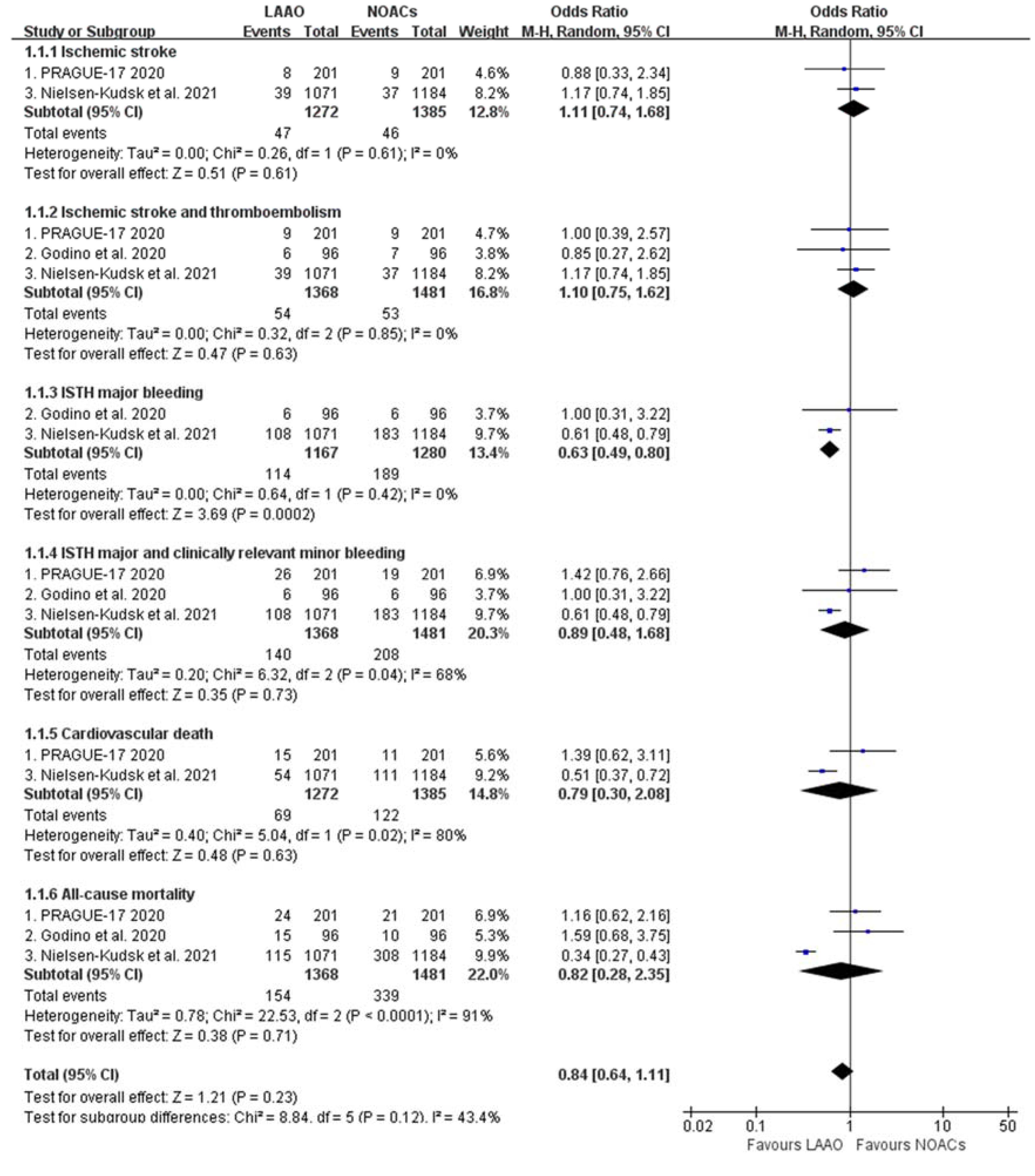
4.2. Clinical Outcomes
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef]
- Reddy, V.Y.; Doshi, S.K.; Kar, S.; Gibson, D.N.; Price, M.J.; Huber, K.; Horton, R.P.; Buchbinder, M.; Neuzil, P.; Gordon, N.T.; et al. 5-Year Outcomes After Left Atrial Appendage Closure: From the PREVAIL and PROTECT AF Trials. J. Am. Coll. Cardiol. 2017, 70, 2964–2975. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [Updated March 2011]; The Cochrane Collaboration: London, UK, 2011; Available online: http://www.cochrane-handbook.org (accessed on 10 June 2021).
- Osmancik, P.; Herman, D.; Neuzil, P.; Hala, P.; Taborsky, M.; Kala, P.; Poloczek, M.; Stasek, J.; Haman, L.; Branny, M.; et al. Left Atrial Appendage Closure Versus Direct Oral Anticoagulants in High-Risk Patients With Atrial Fibrillation. J. Am. Coll. Cardiol. 2020, 75, 3122–3135. [Google Scholar] [CrossRef] [PubMed]
- Godino, C.; Melillo, F.; Bellini, B.; Mazzucca, M.; Pivato, C.A.; Rubino, F.; Figini, F.; Mazzone, P.; Della Bella, P.; Margonato, A.; et al. Percutaneous left atrial appendage closure versus non-vitamin K oral anticoagulants in patients with non-valvular atrial fibrillation and high bleeding risk. EuroIntervention 2020, 15, 1548–1554. [Google Scholar] [CrossRef]
- Nielsen-Kudsk, J.E.; Korsholm, K.; Damgaard, D.; Valentin, J.B.; Diener, H.C.; Camm, A.J.; Johnsen, S.P. Clinical Outcomes Associated With Left Atrial Appendage Occlusion Versus Direct Oral Anticoagulation in Atrial Fibrillation. JACC Cardiovasc. Interv. 2021, 14, 69–78. [Google Scholar] [CrossRef]
- Schmidt, B.; Bordignon, S.; Chen, S.; Chun, K.R.J. What Does the Future Hold?: Ideal Device, Newer Devices, and More. Card. Electrophysiol. Clin. 2020, 12, 125–130. [Google Scholar] [CrossRef]
- Hildick-Smith, D.; Landmesser, U.; Camm, A.J.; Diener, H.C.; Paul, V.; Schmidt, B.; Settergren, M.; Teiger, E.; Nielsen-Kudsk, J.E.; Tondo, C. Left atrial appendage occlusion with the Amplatzer™ Amulet™ device: Full results of the prospective global observational study. Eur. Heart J. 2020, 41, 2894–2901. [Google Scholar] [CrossRef]
- Korsholm, K.; Samaras, A.; Andersen, A.; Jensen, J.M.; Nielsen-Kudsk, J.E. The Watchman FLX Device: First European Experience and Feasibility of Intracardiac Echocardiography to Guide Implantation. JACC Clin. Electrophysiol. 2020, 6, 1633–1642. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Schmidt, B.; Bordignon, S.; Bologna, F.; Nagase, T.; Tsianakas, N.; Perrotta, L.; Chun, K.R.J. Feasibility of percutaneous left atrial appendage closure using a novel LAmbre occluder in patients with atrial fibrillation: Initial results from a prospective cohort registry study. J. Cardiovasc. Electrophysiol. 2018, 29, 291–297. [Google Scholar] [CrossRef]
- Chen, S.; Chun, K.R.J.; Bordignon, S.; Weise, F.K.; Nagase, T.; Perrotta, L.; Bologna, F.; Schmidt, B. Left atrial appendage occlusion using LAmbre Amulet and Watchman in atrial fibrillation. J. Cardiol. 2019, 73, 299–306. [Google Scholar] [CrossRef]
- Chen, S.; Weise, F.K.; Chun, K.R.J.; Schmidt, B. Antithrombotic strategies after interventional left atrial appendage closure: An update. Expert Rev. Cardiovasc. Ther. 2018, 16, 675–678. [Google Scholar] [CrossRef]
- Zender, N.; Weise, F.K.; Bordignon, S.; Herrmann, E.; Konstantinou, A.; Bologna, F.; Nagase, T.; Chen, S.; Chun, K.R.J.; Schmidt, B. Thromboembolism after electrical isolation of the left atrial appendage: A new indication for interventional closure? Europace 2019, 21, 1502–1508. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Schmidt, B.; Bordignon, S.; Bologna, F.; Lindhoff-Last, E.; Chun, K.R.J. Thrombus Formation in Isolated Left Atrial Appendage After Multiple Atrial Fibrillation Ablations Despite Oral Anticoagulation Followed by Percutaneous Appendage Closure. JACC Clin. Electrophysiol. 2019, 5, 398–400. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Schmidt, B.; Tohoku, S.; Trolese, L.; Bordignon, S.; Chun, K.R.J. Transesophageal echocardiography-guided closure of electrically isolated left atrial appendage to constrain a rapidly growing thrombus despite anticoagulation and sinus rhythm. J. Cardiovasc. Electrophysiol. 2020, 31, 247–249. [Google Scholar] [CrossRef] [PubMed]
- Connolly, S.J.; Ezekowitz, M.D.; Yusuf, S.; Eikelboom, J.; Oldgren, J.; Parekh, A.; Pogue, J.; Reilly, P.A.; Themeles, E.; Varrone, J.; et al. Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2009, 361, 1139–1151, Epub 2009 Aug 30; Erratum in: N. Engl. J. Med. 2010, 363, 1877. [Google Scholar] [CrossRef] [PubMed]
- Granger, C.B.; Alexander, J.H.; McMurray, J.J.; Lopes, R.D.; Hylek, E.M.; Hanna, M.; Al-Khalidi, H.R.; Ansell, J.; Atar, D.; Avezum, A.; et al. Apixaban versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2011, 365, 981–992. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.R.; Mahaffey, K.W.; Garg, J.; Pan, G.; Singer, D.E.; Hacke, W.; Breithardt, G.; Halperin, J.L.; Hankey, G.J.; Piccini, J.P.; et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N. Engl. J. Med. 2011, 365, 883–891. [Google Scholar] [CrossRef]
- Giugliano, R.P.; Ruff, C.T.; Braunwald, E.; Murphy, S.A.; Wiviott, S.D.; Halperin, J.L.; Waldo, A.L.; Ezekowitz, M.D.; Weitz, J.I.; Špinar, J.; et al. Edoxaban versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2013, 369, 2093–2104. [Google Scholar] [CrossRef]
- Dentali, F.; Riva, N.; Crowther, M.; Turpie, A.G.; Lip, G.Y.; Ageno, W. Efficacy and safety of the novel oral anticoagulants in atrial fibrillation: A systematic review and meta-analysis of the literature. Circulation 2012, 126, 2381–2391. [Google Scholar] [CrossRef]
- Reddy, V.Y.; Akehurst, R.L.; Amorosi, S.L.; Gavaghan, M.B.; Hertz, D.S.; Holmes, D.R., Jr. Cost-Effectiveness of Left Atrial Appendage Closure with the WATCHMAN Device Compared with Warfarin or Non-Vitamin K Antagonist Oral Anticoagulants for Secondary Prevention in Nonvalvular Atrial Fibrillation. Stroke 2018, 49, 1464–1470. [Google Scholar] [CrossRef]
- Saw, J.; Bennell, M.C.; Singh, S.M.; Wijeysundera, H.C. Cost-Effectiveness of Left Atrial Appendage Closure for Stroke Prevention in Atrial Fibrillation Patients With Contraindications to Anticoagulation. Can. J. Cardiol. 2016, 32, 1355.e9–1355.e14. [Google Scholar] [CrossRef] [PubMed]
| PRAGUE-17 Trial 2020 | Godino et al., 2020 | Nielsen-Kudsk et al., 2021 | ||||
|---|---|---|---|---|---|---|
| Design | Randomized Trial | Propensity-Score Matching | Propensity-Score Matching | |||
| Intervention | LAAO | NOACs | LAAO | NOACs | LAAO | NOACs |
| Sample size | 201 | 201 | 96 | 96 | 1071 | 1184 |
| Age, yrs | 73.4 ± 6.7 | 73.2 ± 7.2 | 73.8 ± 7.1 | 75.3 ± 6.8 | 75.1 ± 8.5 | 75.1 ± 10.5 |
| Male, n (%) | 134 (66.7) | 130 (64.7) | 54 (56.2) | 78 (81.3) | 687 (64.2) | 727 (61.4) |
| Weight, kg | 86.9 ± 17.6 | 88.1 ± 16.2 | / | / | / | / |
| BMI, kg/m2 | / | / | 25.7 ± 3.6 | 26.4 ± 4.3 | / | / |
| Indication for treatment | AF | AF | AF | AF | AF | AF |
| CHA2DS2-VASc | 4.7 ± 1.5 | 4.7 ± 1.5 | 4.3 ± 1.5 | 4.3 ± 1.5 | 4.2 ± 1.6 | 4.3 ± 1.7 |
| HAS-BLED | 3.1 ± 0.9 | 3.0 ± 0.9 | 3.5 ± 0.7 | 3.5 ± 0.6 | 3.3 ±1.0 | 3.4 ± 1.2 |
| Heart failure | 88 (43.8) | 90 (44.8) | / | / | 178 (16.6) | 223 (18.9) |
| LVEF, % | 53.3 ± 12.6 | 52.9 ± 12.1 | 51.3 ± 10.8 | 52.1 ± 11.7 | / | / |
| Hypertension | 186 (92.5) | 186 (92.5) | 80 (83.3) | 90 (93.8) | 896 (83.7) | 1023 (86.5) |
| Diabetes mellitus | 73 (36.3) | 90 (44.8) | 24 (25) | 23 (24) | 333 (31.1) | 424 (35.8) |
| History of ischemic Stroke/TIA | 66 (32.8) | 63 (31.3) | 41 (43.2) | 37 (38.5) | 333 (31.1) | 376 (31.8) |
| Coronary artery disease | / | / | / | / | 346 (32.3) | 402 (33.9) |
| History of MI | 30 (14.9) | 39 (19.4) | 11 (11.5) | 23 (24.5) | / | / |
| Renal dysfunction | / | / | 36 (46.8) | 34 (35.4) | 149(13.9) | 169 (14.3) |
| Liver dysfunction | / | / | 4 (4.2) | 4 (4.2) | 51 (4.8) | 77 (6.5) |
| Renal or liver dysfunction | 47 (23.4%) | 44 (21.9%) | / | / | / | / |
| Devices/NOACs | Amulet (61.3%) Watchman (35.9%) Watchman-FLX (2.8%) | Dabigatran (4%) Apixaban (95.5%) Rivaroxaban (0.5%) | Watchman (33.7%) AMPLATZER (22.3%) Amulet (44%) | Dabigatran (41%) Apixaban (41%) Rivaroxaban (18%). | Amulet (100%) | NOACs |
| Procedural LAAO leak >5mm | 4(2.2%) | 0 | 0.7% (>3 mm) | |||
| Success rate of LAAO | 96.8% | 100% | 99.1% | |||
| LAAO | NOACs | |
|---|---|---|
| Sample Size | 1368 | 1481 |
| Age, yrs | 74.8 ± 8.2 | 74.9 ± 9.9 |
| Male, n (%) | 875 (64%) | 935 (63%) |
| Weight, kg | 86.9 ± 17.6 (n = 201) | 88.1 ± 16.2 (n = 201) |
| BMI, kg/m2 | 25.7 ± 3.6 (n = 96) | 26.4 ± 4.3 (n = 96) |
| CHA2DS2-VASc | 4.3 ± 1.6 | 4.4 ± 1.7 |
| HAS-BLED | 3.3 ± 1 | 3.3 ±1.1 |
| Heart Failure | 266 (20.9%) (n = 1272) | 313 (22.6%) (n = 1385) |
| LVEF, % | 52.7 ± 12.1 (n = 297) | 52.6 ± 12 (n = 297) |
| Hypertension | 1162 (84.9%) | 1299 (87.7%) |
| Diabetes Mellitus | 430 (31.4%) | 537 (36.3%) |
| History of Ischemic Stroke/TIA | 440 (32.2%) | 476 (32.1%) |
| Ischemic Heart Disease | 387 (28.3%) | 464 (31.3%) |
| Renal Dysfunction | 185 (15.9%) (n = 1167) | 203 (15.9%) (n = 1280) |
| Liver Dysfunction | 55 (4.7%) (n = 1167) | 81 (6.3%) (n = 1280) |
| Pooled | |
|---|---|
| Sample Size | 1368 |
| Implant Success Rate | 98.8% |
| Pericardial Effusion/Tamponade | 15 (1.1%) |
| Thromboembolism | 5 (0.37%) |
| Device Dislodgement | 3 (0.22%) |
| Puncture Site Complications Requiring Intervention | 9 (0.66%) |
| Death | 5 (0.37%) |
| Reasons of Death | 2 from tamponade 2 from myocardial infarction 1 from cardiorespiratory arrest |
| Trials | Trial Number | Design | Comparison | Sample Size | Planned Follow-Up |
|---|---|---|---|---|---|
| OPTION | (NCT03795298) | Randomized | WATCHMAN FLX LAAO vs. OACs | 1600 | 36 months |
| OCCLUSION-AF | (NCT03642509) | Randomized | Amulet or Watchman LAAO vs. NOACs | 750 | 5 years |
| CLOSURE-AF | (NCT03463317) | Randomized | LAAO devices vs. OACs | 1512 | 24 months |
| CATALYST | (NCT04226547) | Randomized | Amulet LAAO vs. NOACs | 2650 | 2 years |
| CHAMPION-AF | (NCT04394546) | Randomized | WATCHMAN FLX LAAO vs. NOACs | 3000 | 36 months |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, S.; Chun, K.R.J.; Ling, Z.; Liu, S.; Zhu, L.; Wang, J.; Schratter, A.; Acou, W.-J.; Kiuchi, M.G.; Yin, Y.; et al. Comparison of Left Atrial Appendage Occlusion versus Non-Vitamin-K Antagonist Oral Anticoagulation in High-Risk Atrial Fibrillation: An Update. J. Cardiovasc. Dev. Dis. 2021, 8, 69. https://doi.org/10.3390/jcdd8060069
Chen S, Chun KRJ, Ling Z, Liu S, Zhu L, Wang J, Schratter A, Acou W-J, Kiuchi MG, Yin Y, et al. Comparison of Left Atrial Appendage Occlusion versus Non-Vitamin-K Antagonist Oral Anticoagulation in High-Risk Atrial Fibrillation: An Update. Journal of Cardiovascular Development and Disease. 2021; 8(6):69. https://doi.org/10.3390/jcdd8060069
Chicago/Turabian StyleChen, Shaojie, K. R. Julian Chun, Zhiyu Ling, Shaowen Liu, Lin Zhu, Jiazhi Wang, Alexandra Schratter, Willem-Jan Acou, Márcio Galindo Kiuchi, Yuehui Yin, and et al. 2021. "Comparison of Left Atrial Appendage Occlusion versus Non-Vitamin-K Antagonist Oral Anticoagulation in High-Risk Atrial Fibrillation: An Update" Journal of Cardiovascular Development and Disease 8, no. 6: 69. https://doi.org/10.3390/jcdd8060069
APA StyleChen, S., Chun, K. R. J., Ling, Z., Liu, S., Zhu, L., Wang, J., Schratter, A., Acou, W.-J., Kiuchi, M. G., Yin, Y., & Schmidt, B. (2021). Comparison of Left Atrial Appendage Occlusion versus Non-Vitamin-K Antagonist Oral Anticoagulation in High-Risk Atrial Fibrillation: An Update. Journal of Cardiovascular Development and Disease, 8(6), 69. https://doi.org/10.3390/jcdd8060069







