Role of Transient Elastography to Stage Fontan-Associated Liver Disease (FALD) in Adults with Single Ventricle Congenital Heart Disease Correction
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients Characteristics
2.2. Methods
2.3. Classification Criteria for FALD Staging
2.4. Statistical Analysis
3. Results
3.1. General and Cardiologic Aspects
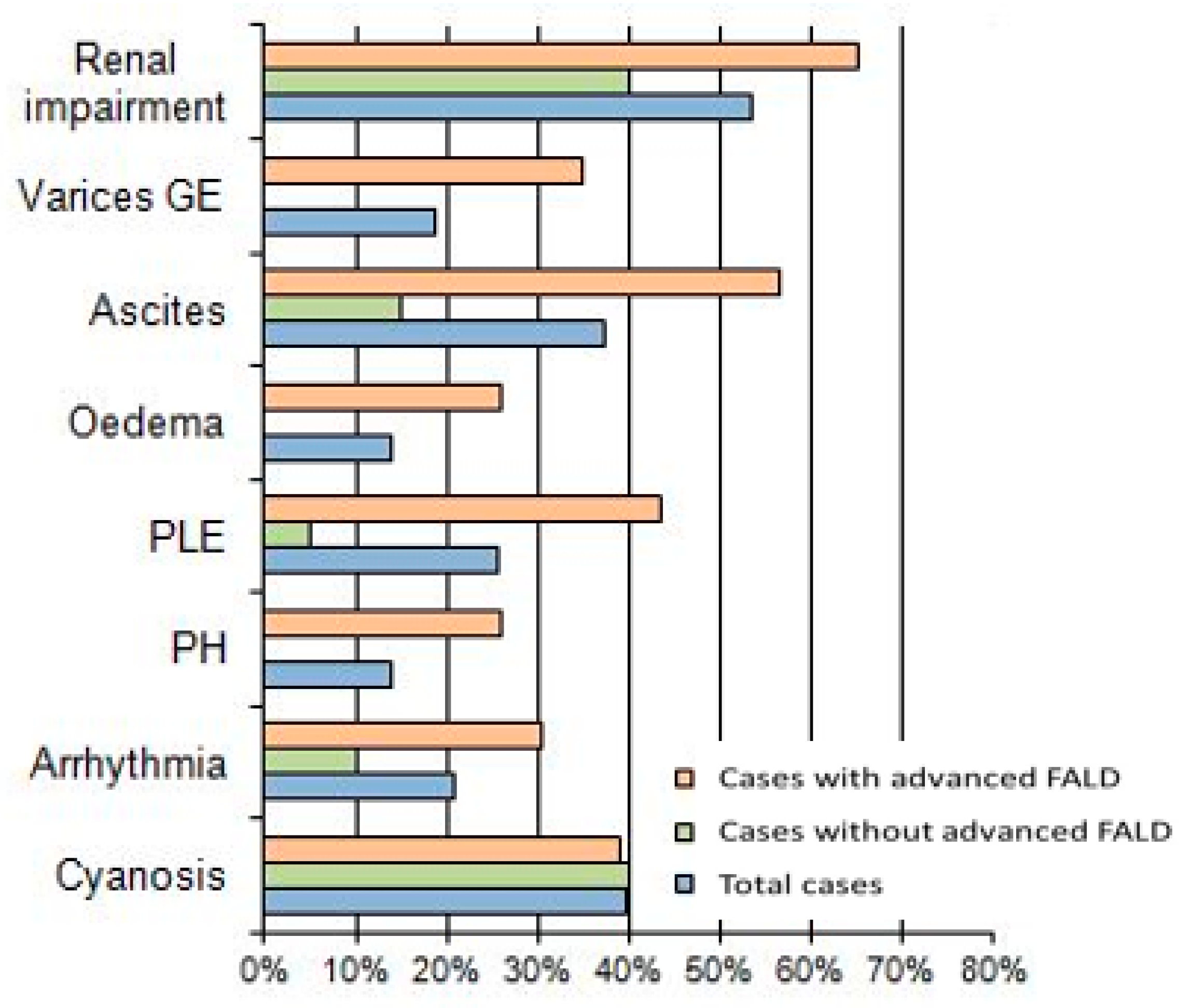
3.2. Case Analysis According to Grouping in without or with Advanced FALD
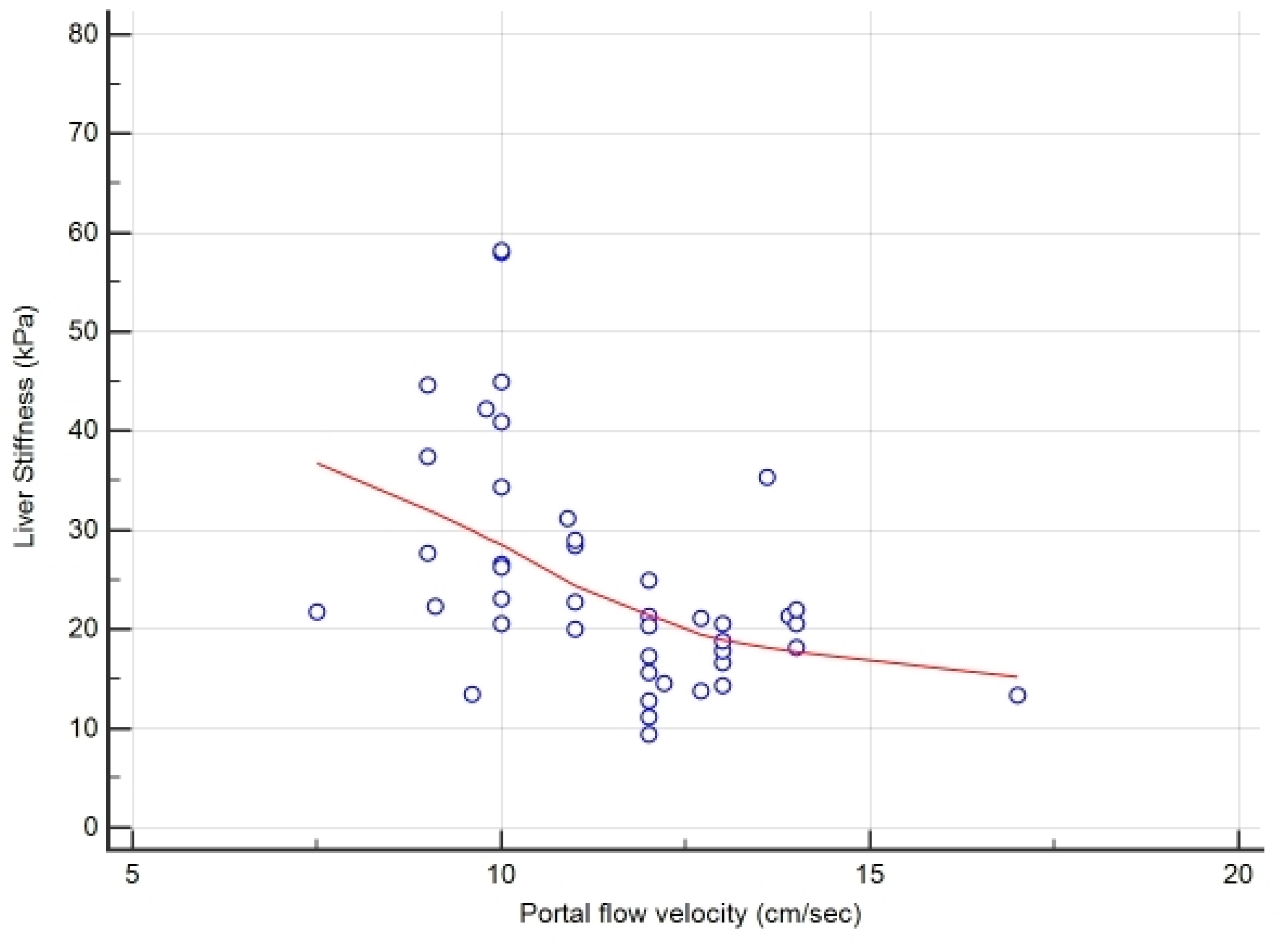
3.3. Definition of Cut-Off Values for FALD Staging
4. Discussion
5. Conclusions
6. Key Points
- FALD is an emerging complication of failing Fontan in cases with rare SV congenital heart defect undergoing Fontan operation in childhood;
- LS may be proposed as a promising non-invasive tool to stage FALD in cases with SV and Fontan circuit;
- Since few and conflictual data exist regarding the effective role of TE in staging the severity of FALD in adult population, we propose the novel values (>22 kPa) of LS for predicting advanced FALD;
- This knowledge may help decision making before major surgical operations, possibly minimizing unexpected liver complications and related risk of mortality.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Glenn, W.W.; Ordway, N.K.; Talner, N.S.; Call, E.P., Jr. Circulatory Bypass of the Right Side of the Heart. Vi. Shunt between Superior Vena Cava and Distal Right Pulmonary Artery; Report of Clinical Application in Thirty-Eight Cases. Circulation 1965, 31, 172–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Norwood, W.I.; Kirklin, J.K.; Sanders, S.P. Hypoplastic left heart syndrome: Experience with palliative surgery. Am. J. Cardiol. 1980, 45, 87–91. [Google Scholar] [CrossRef]
- Gewillig, M. The Fontan circulation. Heart 2005, 91, 839–846. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Téllez, L.; Rodrìguez-Santiago, E.; Albillos, A. Fontan-Associated Liver Disease: A Review. Ann. Hepatol. 2018, 17, 192–204. [Google Scholar] [CrossRef]
- Daniels, C.J.; Bradley, E.A.; Landzberg, M.J.; Aboulhons, J.; Beeckman, R.H.; Book, W.; Gurvitz, M.; John, A.; John, B.; Marelli, A.; et al. Fontan-Associated Liver Disease. JACC 2017, 70, 3173–3194. [Google Scholar] [CrossRef]
- Bea, J.M.; Jeon, T.Y.; Kim, J.S.; Kim, S.; Hwang, S.M.; Yoo, S.Y.; Kim, J.H. Fontan-associated liver disease: Spectrum of US findings. Eur. J. Radiol. 2016, 7, 850–856. [Google Scholar]
- Sessa, A.; Allaire, M.; Lebray, M.; Medmoun, M.; Tiritilli, A.; Iaria, P.; Cadranel, J.F. From congestive hepatopathy to hepatocellular carcinoma, how can we to improve the management of the patients? J. Hep. Rep. 2021, 27, 100249. [Google Scholar]
- Deorsola, L.; Aidala, E.; Cascarano, M.T.; Valori, A.; Agnoletti, G.; Napoleone, C.P. Liver stiffness modifications shortly after total cavopulmonary connection. Interact. Cardiovasc. Thorac. Surg. 2016, 23, 513–518. [Google Scholar] [CrossRef] [Green Version]
- Fredenburg, T.B.; Johnson, T.R.; Cohen, M.D. The Fontan procedure: Anatomy, complications, and manifestations of failure. RadioGraphics 2011, 31, 453–463. [Google Scholar] [CrossRef]
- Schleiger, A.; Salzmann, M.; Kramer, P.; Danne, F.; Schubert, S.; Bassir, C.; Müller, T.; Müller, H.-P.; Berger, F.; Ovroutski, S. Severity of Fontan-Associated Liver Disease Correlates with Fontan Hemodynamics. Pediatr. Cardiol. 2020, 41, 736–746. [Google Scholar] [CrossRef] [Green Version]
- Deal, B.J.; Jacobs, M.L. Management of failing Fontan circulation. Heart 2012, 98, 1098–1104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kendall, T.J.; Stedman, B.; Hacking, N.; Haw, M.; Vettukattill, J.J.; Salmon, A.P.; Cope, R.; Sheron, N.; Millward-Sadler, H.; Veldtman, G.R.; et al. Hepatic fibrosis and cirrhosis in the Fontan circulation: A detailed morphological study. J. Clin. Pathol. 2007, 61, 504–508. [Google Scholar] [CrossRef] [PubMed]
- Surrey, L.F.; Russo, P.; Rychik, J.; Goldberg, D.J.; Dodds, K.; O’Byrne, M.L.; Glatz, A.C.; Rand, E.B.; Lin, H.C. Prevalence and characterization of fibrosis in surveillance liver biopsies of patients with Fontan circulation. Hum. Pathol. 2016, 57, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.K.; Han, K.-H.; Park, J.Y.; Ahn, S.H.; Kim, J.K.; Paik, Y.H.; Lee, K.S.; Chon, C.Y.; Kim, D.Y. A Liver Stiffness Measurement-Based, Noninvasive Prediction Model for High-Risk Esophageal Varices in B-Viral Liver Cirrhosis. Am. J. Gastroenterol. 2010, 105, 1382–1390. [Google Scholar] [CrossRef] [PubMed]
- Fidai, A.; Dallaire, F.; Alvarez, N.; Balon, Y.; Clegg, R.; Connelly, M.; Dicke, F.; Fruitman, D.; Harder, J.; Myers, K.; et al. Non-invasive Investigations for the Diagnosis of Fontan-Associated Liver Disease in Pediatric and Adult Fontan Patients. Front. Cardiovasc. Med. 2017, 4, 15. [Google Scholar] [CrossRef]
- Padalino, M.A.; Chemello, L.; Cavalletto, L.; Angelini, A.; Fedrigo, M. Prognostic value of liver and spleen stiffness in patients with Fontan Associated Liver Disease (FALD): A Case Series with Histopathologic Comparison. JCDD 2021, 8, 30. [Google Scholar] [CrossRef]
- Wai, C.T.; Marrero, J.A.; Conjeevaram, H.S.; Lok, A.S.; Greenson, J.K.; Fontana, R.J.; Kalbfleisch, J.D. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology 2003, 38, 518–526. [Google Scholar] [CrossRef] [Green Version]
- Forns, X.; Ampurdanès, S.; Llovet, J.M.; Aponte, J.; Quintó, L.; Martínez-Bauer, E.; Bruguera, M.; Sánchez-Tapias, J.M.; Rodés, J. Identification of chronic hepatitis C patients without hepatic fibrosis by a simple predictive model. Hepatology 2002, 36, 986–992. [Google Scholar] [CrossRef] [Green Version]
- Sterling, R.K.; Lissen, E.; Clumeck, N.; Sola, R.; Correa, M.C.; Montaner, J.; Sulkowski, M.S.; Torriani, F.J.; Dieterich, D.T.; Thomas, D.L.; et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 2006, 43, 1317–1325. [Google Scholar] [CrossRef]
- Grimm, J.C.; Magruder, J.T.; Do, N.; Spinner, J.; Dungan, S.P.; Kilic, A.; Patel, N.; Nelson, K.L.; Jacobs, M.L.; Cameron, D.E.; et al. Modified Model for End-Stage Liver Disease eXcluding INR (MELD-XI) Score Predicts Early Death After Pediatric Heart Transplantation. Ann. Thorac. Surg. 2016, 101, 730–735. [Google Scholar] [CrossRef] [Green Version]
- Komatsu, H.; Inui, A.; Kishiki, K.; Kawai, H.; Yoshio, S.; Osawa, Y.; Kanto, T.; Fujisawa, T. Liver disease secondary to congenital heart disease in children. Expert Rev. Gastroenterol. Hepatol. 2019, 13, 651–666. [Google Scholar] [CrossRef]
- Rychik, J.; Atz, A.M.; Celermajer, D.S.; Deal, B.J.; Gatzoulis, M.A.; Gewillig, M.H.; Hsia, T.-Y.; Hsu, D.T.; Kovacs, A.H.; McCrindle, B.W.; et al. Evaluation and Management of the Child and Adult with Fontan Circulation: A Scientific Statement from the American Heart Association. A Scientific statement from the AHA. Circulation 2019, 140, e234–e284. [Google Scholar] [CrossRef] [PubMed]
- Schleiger, A.; Kramer, P.; Salzmann, M.; Danne, F.; Schubert, S.; Bassir, C.; Müller, T.; Tacke, F.; Müller, H.-P.; Berger, F.; et al. Evaluation of Fontan failure by classifying the severity of Fontan-associated liver disease: A single-centre cross-sectional study. Eur. J. Cardio-Torac. Surg. 2021, 59, 341–348. [Google Scholar] [CrossRef]
- Wu, F.M.; Kogon, B.; Earing, M.G.; Aboulhosn, J.A.; Broberg, C.S.; John, A.S.; Harmon, A.; Sainani, N.I.; Hill, A.J.; Odze, R.D.; et al. Liver health in adults with Fontan circulation: A multicenter cross-sectional study. J. Thorac. Cardiovasc. Surg. 2017, 153, 656–664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldberg, D.J.; Surrey, L.F.; Glatz, A.C.; Dodds, K.; O’Byrne, M.L.; Lin, H.C.; Fogel, M.; Rome, J.J.; Rand, E.B.; Russo, P.; et al. Hepatic Fibrosis Is Universal Following Fontan Operation, and Severity is Associated with Time from Surgery: A Liver Biopsy and Hemodynamic Study. J. Am. Heart Assoc. 2017, 6, 179–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, T.H.; Yang, H.K.; Jang, H.J.; Yoo, S.J.; Khalili, K.; Kim, T.K. Abdominal findings in adult patients with Fontan circulation. Insights Imaging 2018, 9, 357–367. [Google Scholar] [CrossRef] [Green Version]
- Ellis, E.L.; Mann, D.A. Clinical evidence of regression of liver fibrosis. J. Hepatol. 2012, 56, 1171–1180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dichtl, W.; Vogel, W.; Dunst, K.M.; Grander, W.; Alber, H.F.; Frick, M.; Antretter, H.; Laufer, G.; Pachinger, O.; Polzl, G. Cardiac hepatopathy before and after heart transplantation. Transpl. Int. 2005, 18, 697–702. [Google Scholar] [CrossRef]

| Total Cases | Cases without Advanced FALD | Cases with Advanced FALD | p | ||
|---|---|---|---|---|---|
| General and Cardiologic characteristics | |||||
| N° Cases (male/female) | 43 (26/17) | 20 (10/10) | 23 (16/7) | ns | |
| Age (mean years ± SD) | 30 ± 9 | 27.5 ± 7.1 | 33.0 ± 10.2 | <0.05 | |
| Type of CHD | ns | ||||
| TA valve | 25 | 12 (60%) | 13 (56.6%) | ||
| S or RV-UH | 11 | 5 (25%) | 6 (26%) | ||
| DILV | 7 | 3 (15%) | 4 (17.4%) | ||
| Type of systemic camera | ns | ||||
| Right ventricle (RV) | 11 (25.6%) | 5 (25%) | 6 (26%) | ||
| Left ventricle (LV) | 32 (74.4%) | 15 (75%) | 17 (73%) | ||
| Age at Fontan (years ± SD) | 3.5 ± 6.3 | 2.1 ± 3.2 | 5.2 ± 7.6 | ns | |
| Type of Fontan conduit | ns | ||||
| Extra cardiac conduit (ECC) | 20 (46.5%) | 9 (45%) | 11 (47.8%) | ||
| Lateral-tunnel (LL) | 19 (44.2%) | 10 (50%) | 9 (39.1%) | ||
| Others | 4 (9.4%) | 1 (5%) | 3 (13.1%) | ||
| Time from Fontan (years ± SD) | 26 ± 6.5 | 25.3 ± 5.8 | 27.8 ± 7.5 | ns | |
| 10 to 20 years | 8 (18.6%) | 3 (15%) | 5 (21.7%) | ||
| over 20 years | 35 (81.4%) | 17 (85%) | 18 (78.3%) | ||
| Upper Abdominal US Doppler parameters | |||||
| Hepatic veins | <0.05 | ||||
| without dilation | 16 (37.2%) | 11 (55%) | 5 (21.7%) | ||
| with dilation (>10 mm) | 27 (62.8%) | 9 (45%) | 18 (78.3%) | ||
| Spleen diameter (cm) | 12.8 ± 2.3 | 11.7 ± 1.5 | 13.8 ± 2.5 | <0.01 | |
| Porta vein diameter (mm) | 12.6 ± 1.8 | 11.7 ± 1.8 | 13.4 ± 1.4 | <0.001 | |
| Portal flow velocity (cm/sec) | 11.5 ± 1.9 | 12.9 ± 1.3 | 10.2 ± 1.2 | <0.001 | |
| with normal flow | 22 (51.2%) | 19 (95%) | 3 (13.1%) | ||
| with slowed flow (<12 cm/s) | 21 (48.9%) | 1 (5%) | 20 (86.9%) | ||
| IVC diameter (mm) | 20 ± 4.5 | 17.9 ± 3.3 | 21.8 ± 4.7 | <0.01 <0.001 | |
| without dilation | 11 (25.6%) | 9 (45%) | 2 (8.7%) | ||
| with dilation (≥17 mm) | 32 (74.4%) | 11 (55%) | 21 (91.3%) | ||
| Transient Elastography (FibroScan®) | |||||
| Liver stiffness (kPa) | 24.9 ± 11.8 | 17.5 ± 4.4 | 31.6 ± 12 | <0.001 | |
| Echocardiography evaluation | |||||
| Systolic pressure (mmHg) | 114 ± 23 | 120 ± 16 | 109 ± 26 | ns | |
| Heart rate (bpm) | 72 ± 19 | 69 ± 17 | 76 ± 20 | ns | |
| O2 saturation (%) | 91.2 ± 4.,9 | 91.5 ± 5.7 | 91 ± 4.1 | ns | |
| IVC diameter (mm) | 20.2 ± 5.1 | 17.9 ± 3.9 | 22.3 ± 5.1 | <0.01 | |
| Ejection fraction (%) | 53.4 ± 11.4 | 56 ± 12.2 | 51.2 ± 10.2 | ns | |
| Stroke volume (L/min) | 5.3 ± 3.1 | 4.2 ± 2.0 | 6.2 ± 3.7 | ns | |
| Cardiac index (L/min/m2) | 3.0 ± 1.7 | 2.5 ± 1.1 | 3.6 ± 2.0 | ns | |
| NYHA | class I | 6 (14%) | 6 (30%) | 0 | <0.05 |
| class II | 30 (69.7%) | 13 (65%) | 17 (73.9%) | ||
| class III | 7 (16.3%) | 1 (5%) | 6 (26.1%) | ||
| Scores | Cut-Off for Cases with Liver Disease * | Cut-Off for Cases with A-FALD ** | Sensitivity- Specificity | AUC ± SE | 95% CI | p |
|---|---|---|---|---|---|---|
| APRI | >0.7 for SF; >1 for cirrhosis | >0.49 | 65.2–65% | 0.70 ± 0.07 | 0.55–0.83 | <0.01 |
| FORNS | <4.2 without SF; >6.9 with SF | >5.35 | 61–85% | 0.75 ± 0.07 | 0.60–0.87 | <0.001 |
| FIB-4 | <1.45 without AF; >3.2 with AF | >1.66 | 48–95% | 0.72 ± 0.07 | 0.56–0.85 | 0.005 |
| MELD-XI | >12 for transplant referral | >9 | 70–80% | 0.70 ± 0.08 | 0.54–0.08 | <0.03 |
| LS | >12 kPa for cirrhosis | >22 kPa | 83–95% | 0.93 ± 0.03 | 0.81–0.98 | <0.0001 |
| LSPS | >1.1 for portal hypertension | >1.31 | 91.3–75% | 0.87 ± 0.06 | 0.73–0.95 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chemello, L.; Padalino, M.; Zanon, C.; Benvegnu’, L.; Biffanti, R.; Mancuso, D.; Cavalletto, L. Role of Transient Elastography to Stage Fontan-Associated Liver Disease (FALD) in Adults with Single Ventricle Congenital Heart Disease Correction. J. Cardiovasc. Dev. Dis. 2021, 8, 117. https://doi.org/10.3390/jcdd8100117
Chemello L, Padalino M, Zanon C, Benvegnu’ L, Biffanti R, Mancuso D, Cavalletto L. Role of Transient Elastography to Stage Fontan-Associated Liver Disease (FALD) in Adults with Single Ventricle Congenital Heart Disease Correction. Journal of Cardiovascular Development and Disease. 2021; 8(10):117. https://doi.org/10.3390/jcdd8100117
Chicago/Turabian StyleChemello, Liliana, Massimo Padalino, Chiara Zanon, Luisa Benvegnu’, Roberta Biffanti, Daniela Mancuso, and Luisa Cavalletto. 2021. "Role of Transient Elastography to Stage Fontan-Associated Liver Disease (FALD) in Adults with Single Ventricle Congenital Heart Disease Correction" Journal of Cardiovascular Development and Disease 8, no. 10: 117. https://doi.org/10.3390/jcdd8100117
APA StyleChemello, L., Padalino, M., Zanon, C., Benvegnu’, L., Biffanti, R., Mancuso, D., & Cavalletto, L. (2021). Role of Transient Elastography to Stage Fontan-Associated Liver Disease (FALD) in Adults with Single Ventricle Congenital Heart Disease Correction. Journal of Cardiovascular Development and Disease, 8(10), 117. https://doi.org/10.3390/jcdd8100117








