Sudden Death in Congenital Heart Disease: The Role of the Autopsy in Determining the Actual Cause
Abstract
1. Introduction
Clinical Challenges in CHD-SCD
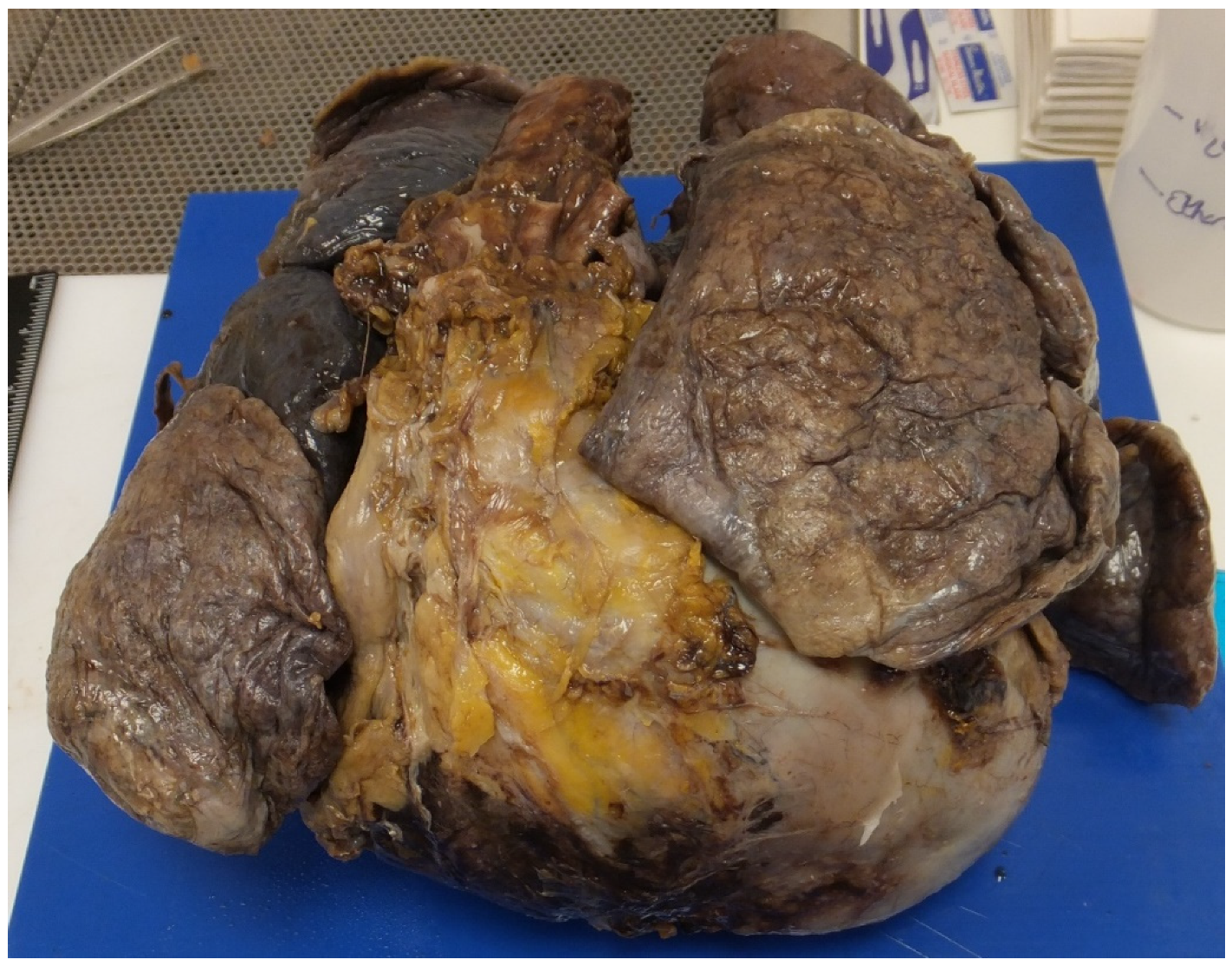
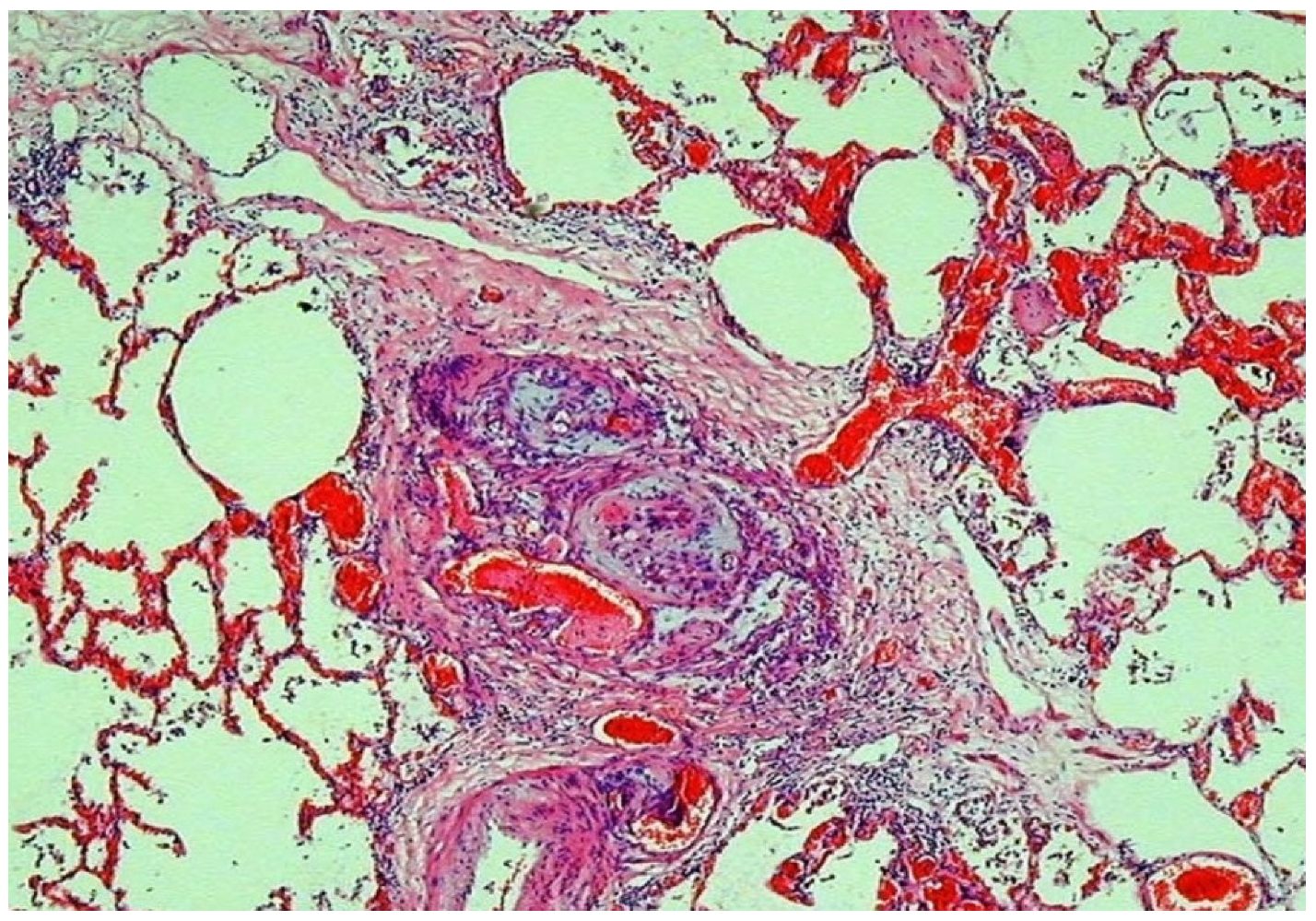
2. Value of the Autopsy in CHD
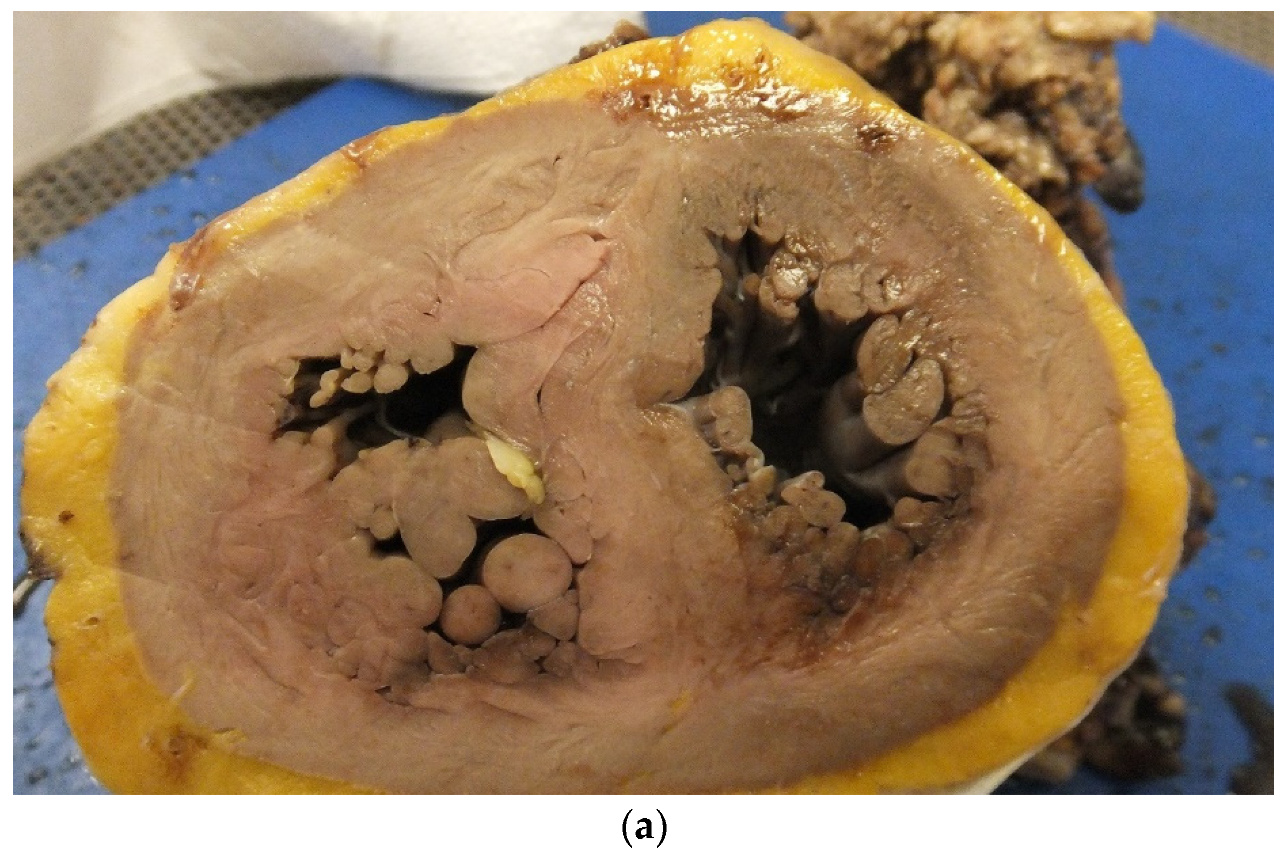
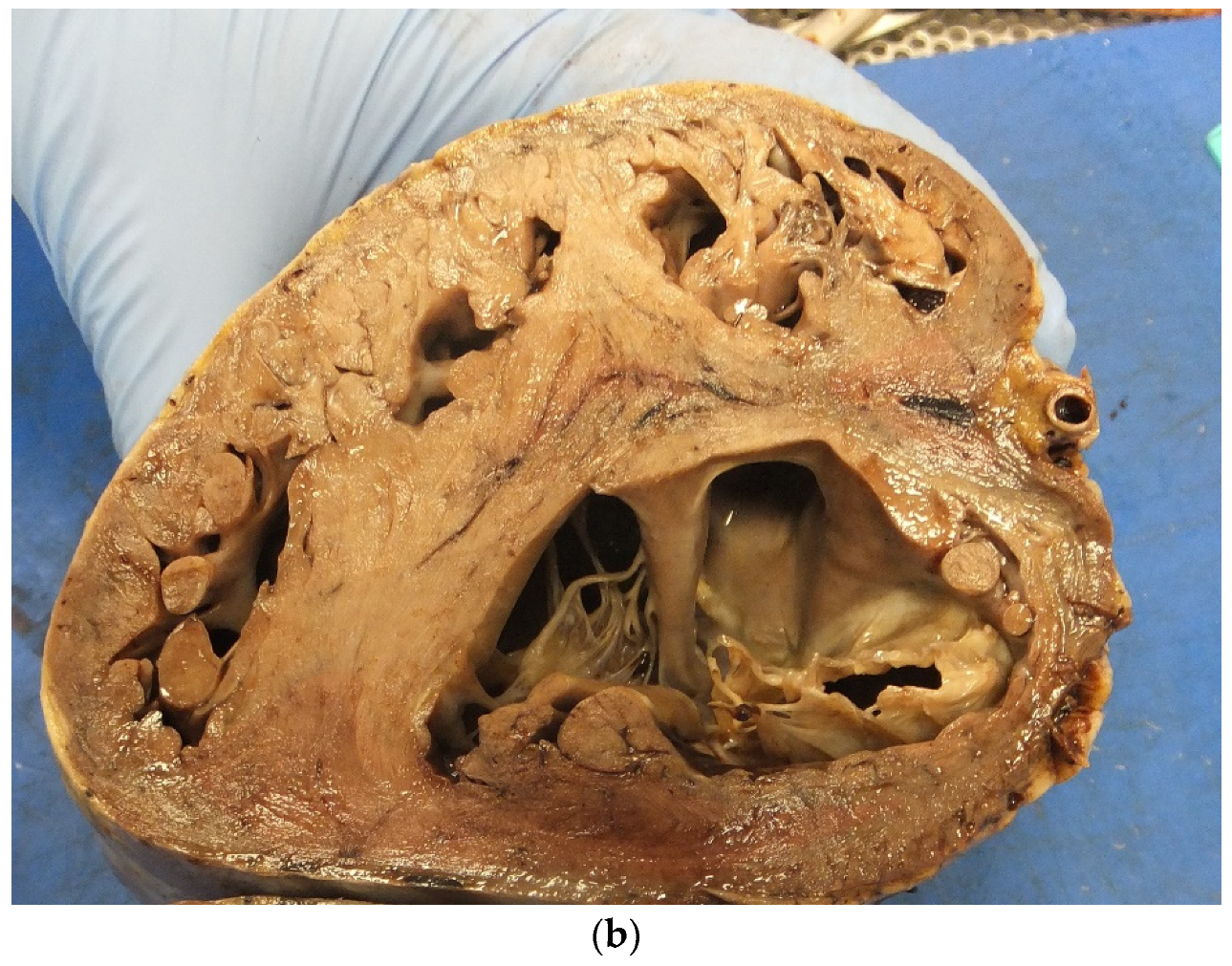
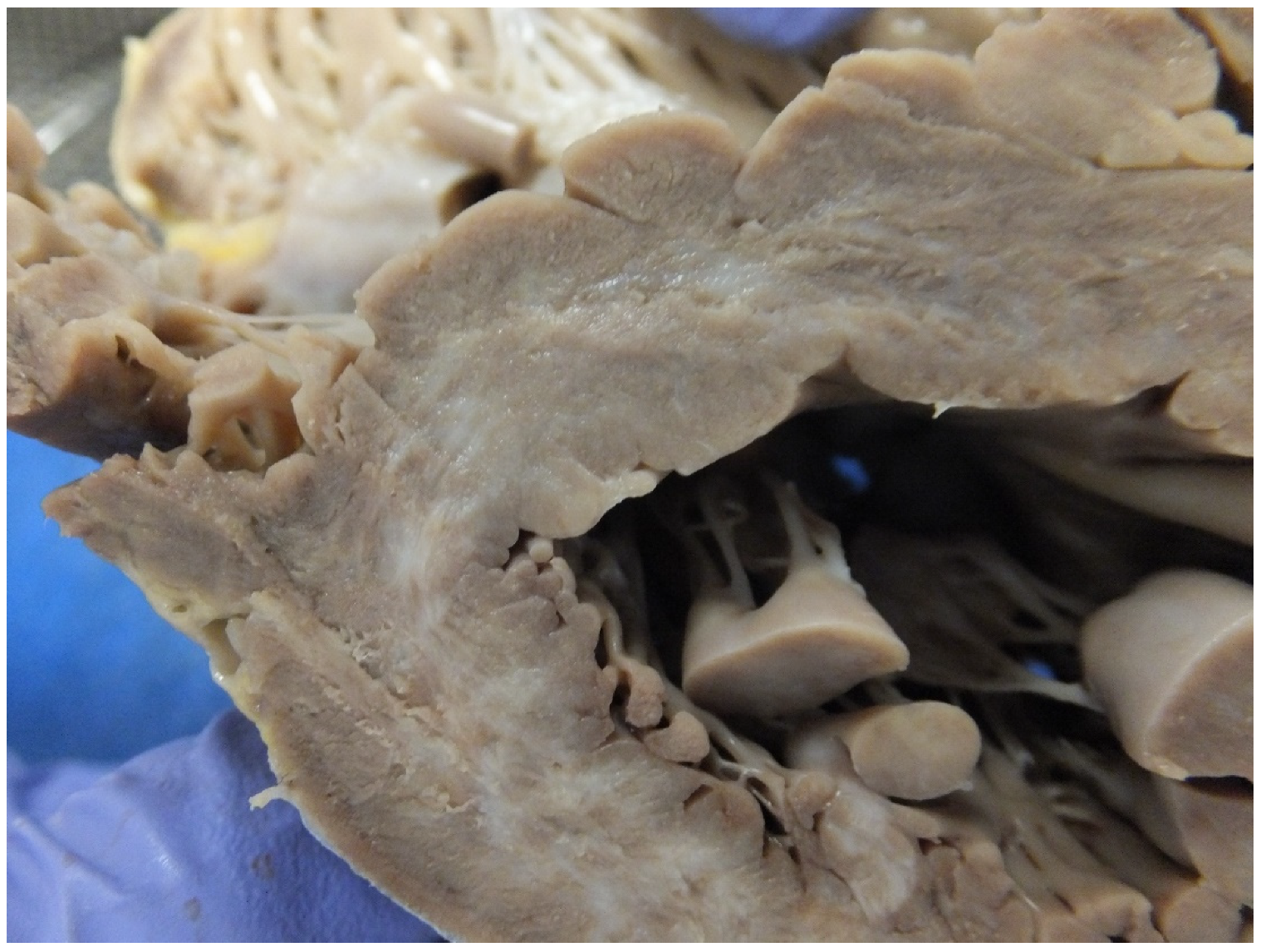
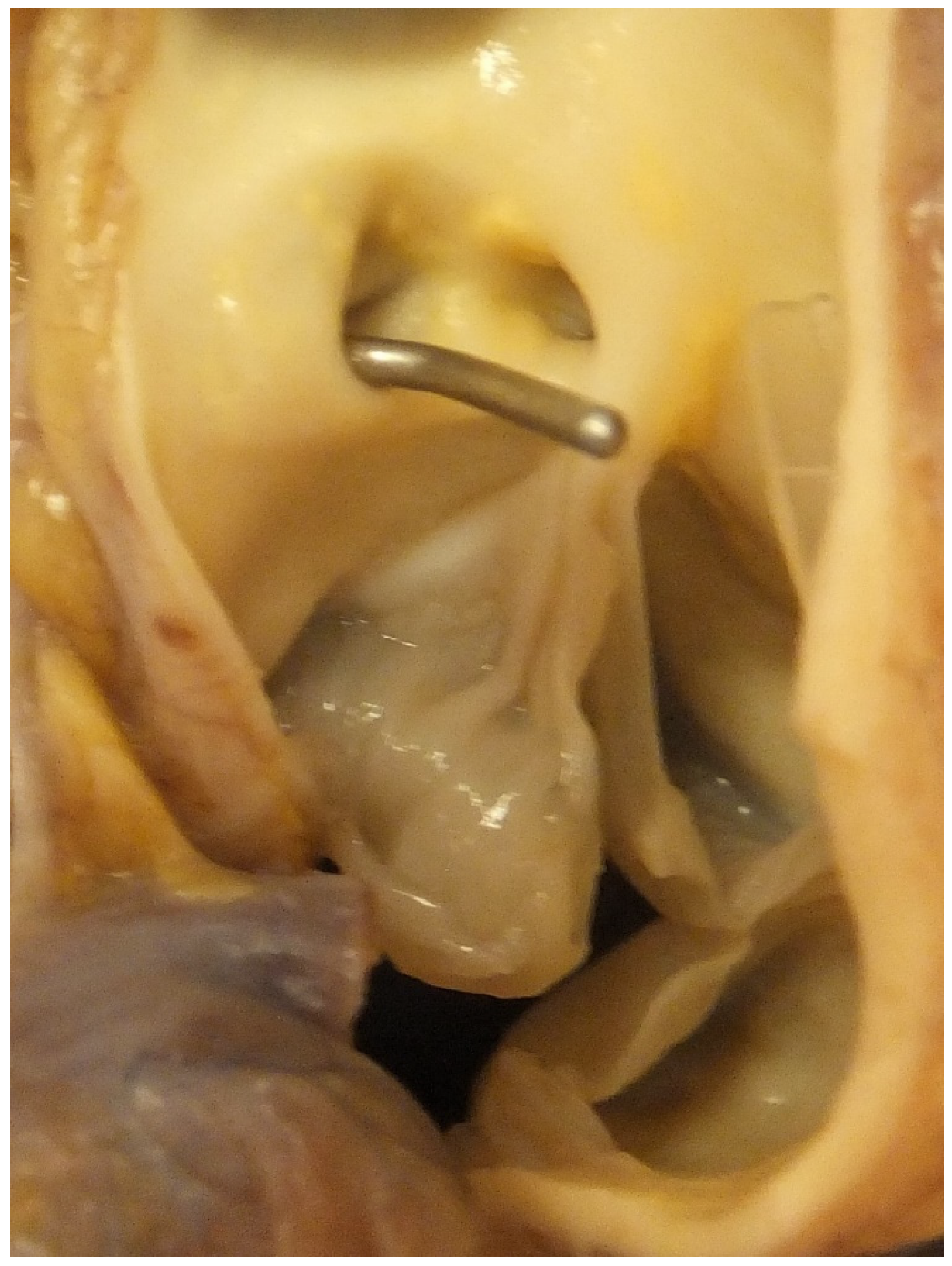
3. Surgical Correction and SCD
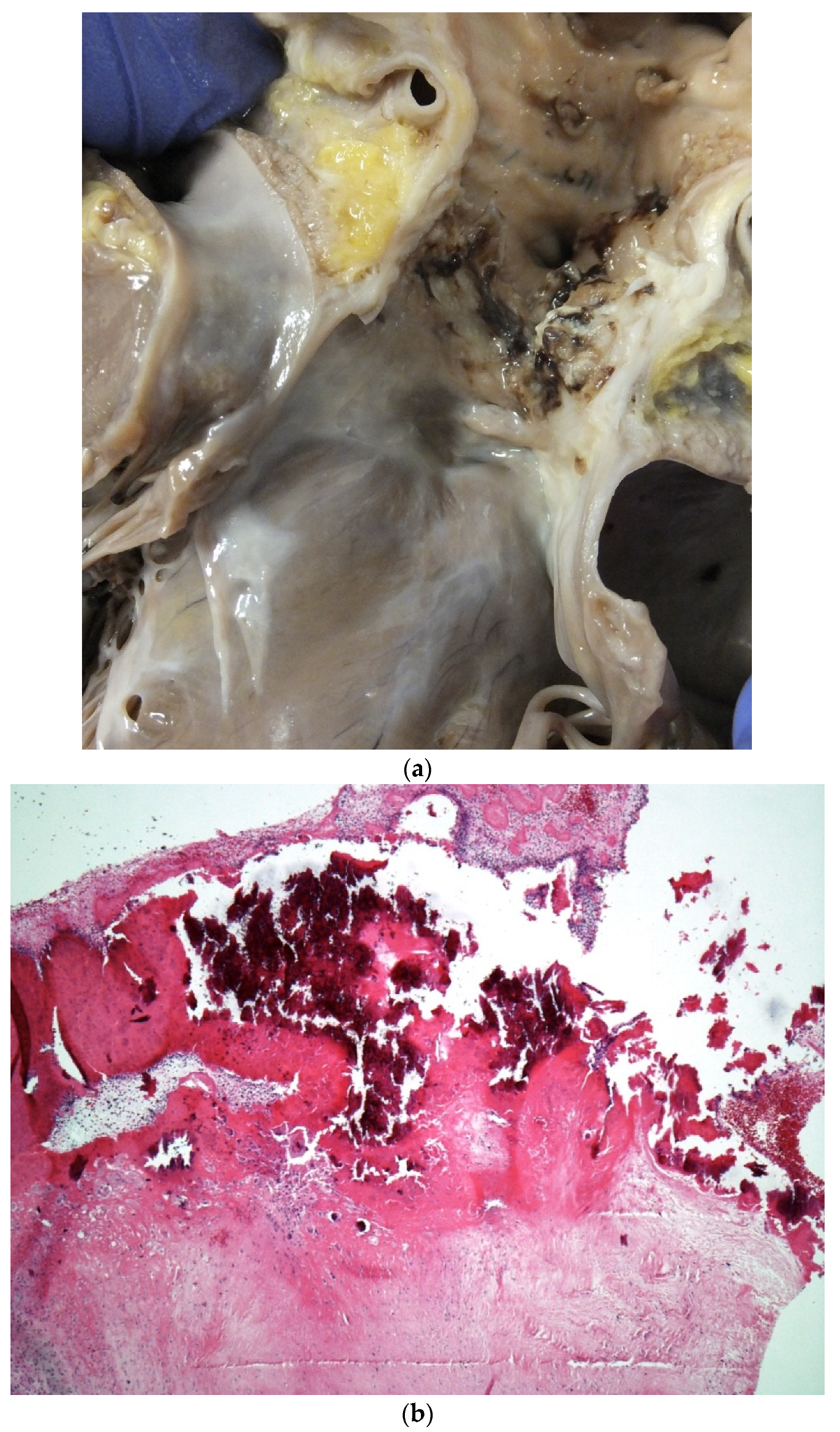
4. Pulmonary Hypertension and SCD
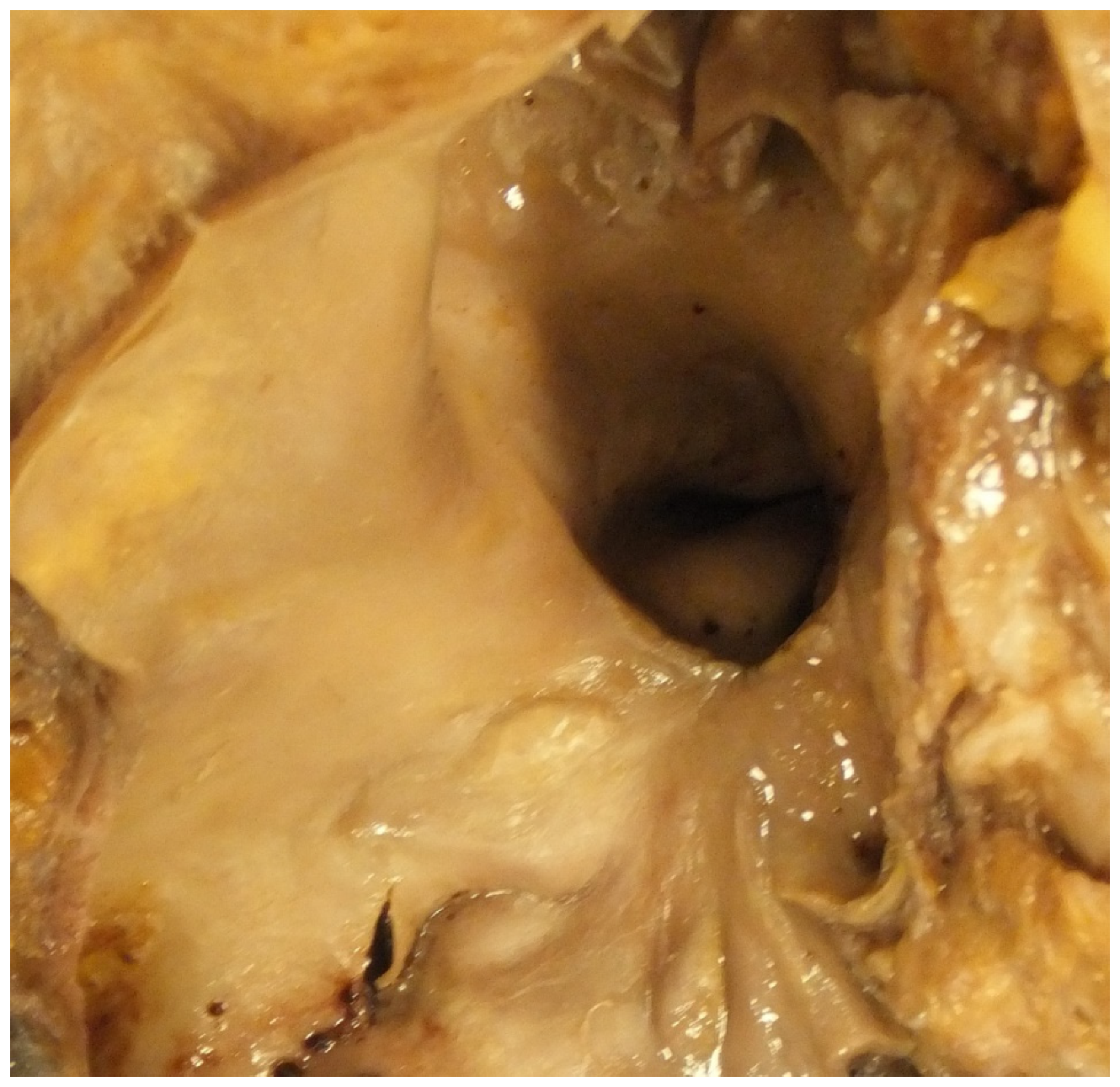
5. CHD and Pregnancy and SCD
6. Coronary Artery Anomalies
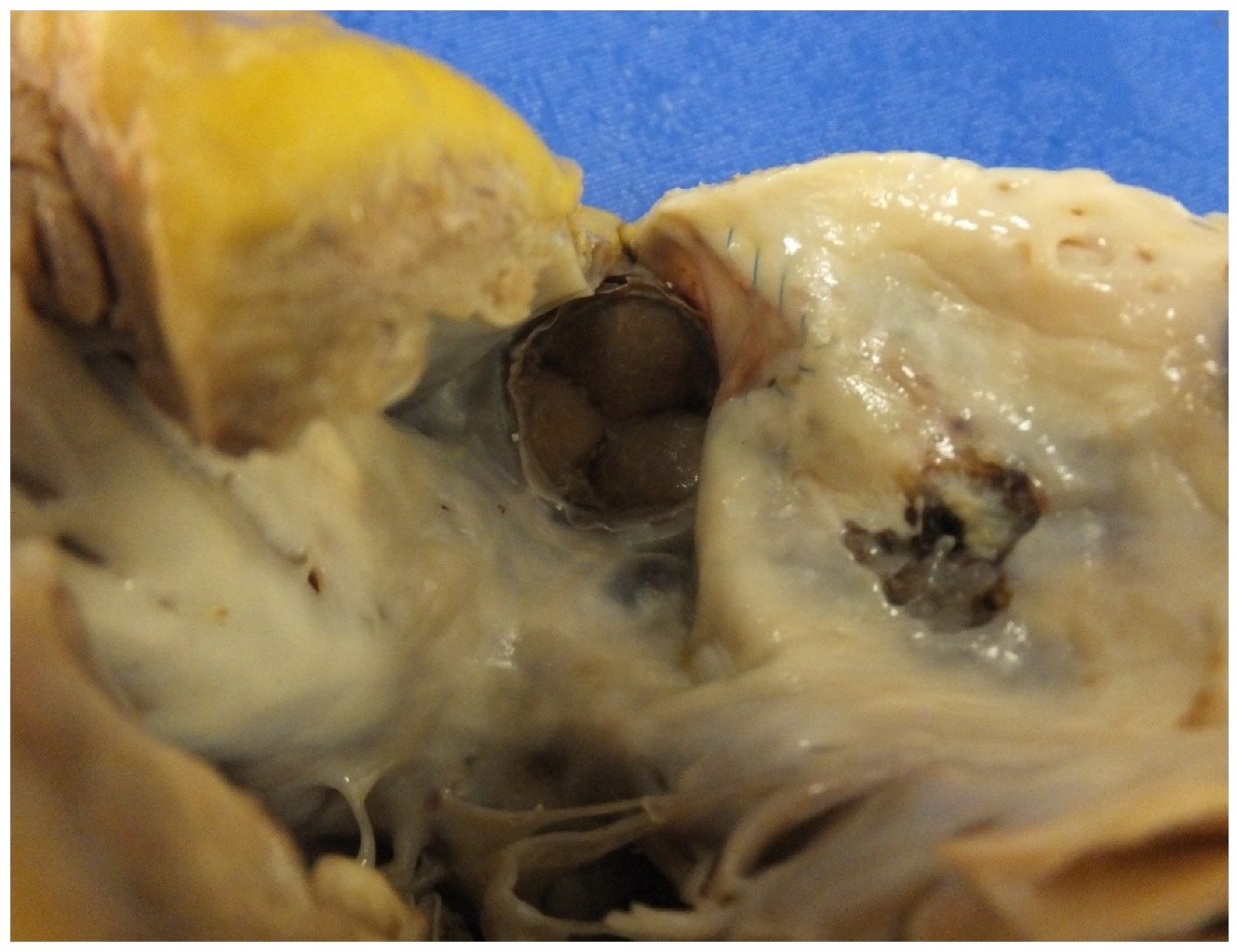
7. Valve Disease and SCD
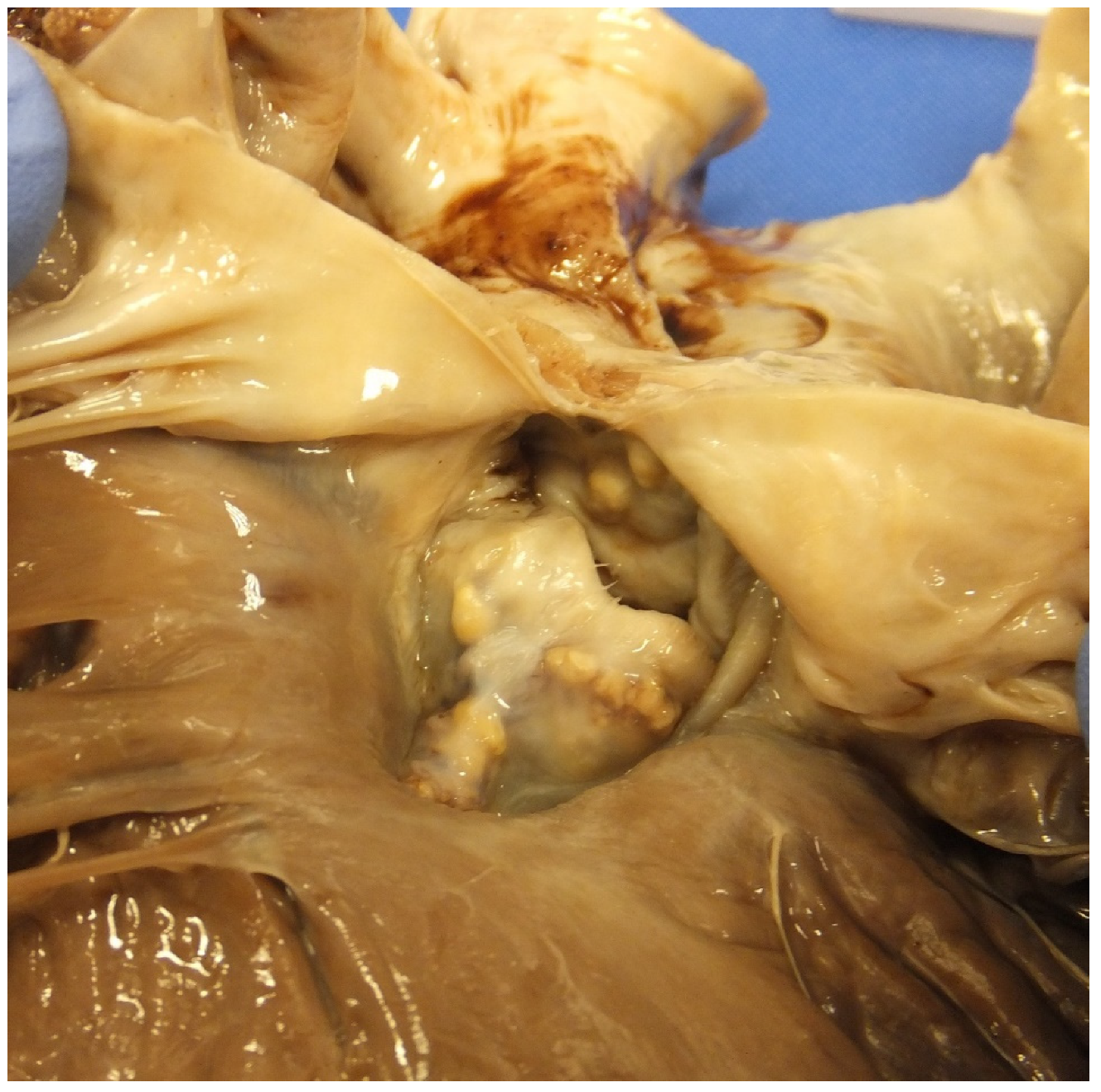
8. Endocarditis and CHD and SCD
9. Coarctation of the Aorta
10. CHD in Our SCD Database
11. Summary
Funding
Conflicts of Interest
References
- Fanaroff, A. Birth Prevalence of Congenital Heart Disease Worldwide: A Systematic Review and Meta-Analysis. Yearb. Neonatal Périnat. Med. 2012, 2012, 101–103. [Google Scholar] [CrossRef]
- Bildirici, I. Faculty Opinions recommendation of 20-year survival of children born with congenital anomalies: A population-based study. In Faculty Opinions—Post-Publication Peer Review of the Biomedical Literature; Faculty Opinions Ltd.: London, UK, 2010; Volume 375, pp. 649–656. [Google Scholar]
- Henning, R.J. Diagnosis and treatment of adults with congenital heart disease. Future Cardiol. 2020, 16, 317–342. [Google Scholar] [CrossRef] [PubMed]
- Brida, M.; Gatzoulis, M.A. Adult congenital heart disease: Past, present and future. Acta Paediatr. 2019, 108, 1757–1764. [Google Scholar] [CrossRef] [PubMed]
- Vehmeijer, J.T.; Koyak, Z.; Bokma, J.P.; Budts, W.; Harris, L.; Mulder, B.J.; De Groot, J.R. Sudden cardiac death in adults with congenital heart disease: Does QRS-complex fragmentation discriminate in structurally abnormal hearts? Europace 2017, 20, f122–f128. [Google Scholar] [CrossRef] [PubMed]
- Di Salvo, G.; Miller, O.; Narayan, S.B.; Li, W.; Budts, W.; Buechel, E.R.V.; Frigiola, A.; Bosch, A.E.V.D.; Bonello, B.; Mertens, L.; et al. Imaging the adult with congenital heart disease: A multimodality imaging approach—position paper from the EACVI. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 1077–1098. [Google Scholar] [CrossRef] [PubMed]
- Khairy, P. Arrhythmias in Adults with Congenital Heart Disease: What the Practicing Cardiologist Needs to Know. Can. J. Cardiol. 2019, 35, 1698–1707. [Google Scholar] [CrossRef]
- Moore, J.P.; Khairy, P. Adults with Congenital Heart Disease and Arrhythmia Management. Cardiol. Clin. 2020, 38, 417–434. [Google Scholar] [CrossRef]
- Moore, B.M.; Cao, J.; Cordina, R.L.; McGuire, M.A.; Celermajer, D. Defibrillators in adult congenital heart disease: Long-term risk of appropriate shocks, inappropriate shocks, and complications. Pacing Clin. Electrophysiol. 2020, 43, 746–753. [Google Scholar] [CrossRef]
- Lynge, T.H.; Jeppesen, A.G.; Winkel, B.G.; Glinge, C.; Schmidt, M.R.; Søndergaard, L.; Risgaard, B.; Tfelt-Hansen, J. Nationwide Study of Sudden Cardiac Death in People with Congenital Heart Defects Aged 0 to 35 Years. Circ. Arrhythmia Electrophysiol. 2018, 11, e005757. [Google Scholar] [CrossRef]
- Mellor, G.; Raju, H.; De Noronha, S.V.; Papadakis, M.; Sharma, S.; Behr, E.R.; Sheppard, M. Clinical Characteristics and Circumstances of Death in the Sudden Arrhythmic Death Syndrome. Circ. Arrhythmia Electrophysiol. 2014, 7, 1078–1083. [Google Scholar] [CrossRef]
- Lahrouchi, N.; Raju, H.; Lodder, E.M.; Papatheodorou, E.; Ware, J.S.; Papadakis, M.; Tadros, R.; Cole, D.; Skinner, J.R.; Crawford, J.; et al. Utility of Post-Mortem Genetic Testing in Cases of Sudden Arrhythmic Death Syndrome. J. Am. Coll. Cardiol. 2017, 69, 2134–2145. [Google Scholar] [CrossRef] [PubMed]
- Fabre, A. Sudden adult death syndrome and other non-ischaemic causes of sudden cardiac death. Heart 2005, 92, 316–320. [Google Scholar] [CrossRef] [PubMed]
- De Noronha, S.V.; Behr, E.R.; Papadakis, M.; Ohta-Ogo, K.; Banya, W.; Wells, J.; Cox, S.; Cox, A.; Sharma, S.; Sheppard, M. The importance of specialist cardiac histopathological examination in the investigation of young sudden cardiac deaths. Europace 2013, 16, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Gitto, L.; Serinelli, S.; Arunkumar, P.; White, S.M. Sudden Cardiac Deaths in Adults with Congenital Heart Disease with Structural Abnormalities: A Retrospective Review of Cases in the Cook County Medical Examiner’s Office. J. Forensic. Sci. 2020, 65, 117–127. [Google Scholar] [CrossRef]
- Gatzoulis, M.A.; Sheppard, M.N.; Ho, S.Y. Value and impact of necropsy in paediatric cardiology. Heart 1996, 75, 626–631. [Google Scholar] [CrossRef]
- Angelini, A.; di Gioia, C.; Doran, H.; Fedrigo, M.; de Gouveia, R.H.; Ho, S.Y.; Leone, O.; Sheppard, M.N.; Thiene, G.; Dimopoulos, K.; et al. Association for European Cardiovascular P: Autopsy in adults with congenital heart disease (ACHD). Virchows Arch. 2020, 476, 797–820. [Google Scholar] [CrossRef]
- Westaby, J.D.; Cooper, S.T.; Edwards, K.A.; Anderson, R.H.; Sheppard, M.N. Insights from examination of hearts from adults dying suddenly to the understanding of congenital cardiac malformations. Clin. Anat. 2019, 33, 394–404. [Google Scholar] [CrossRef]
- Lee, M.-C.; Wu, M.-H.; Lin, M.-T.; Chen, H.-C.; Kao, F.-Y.; Huang, S.-K. Incidence and Postnatal Profile of Fontan Patients by Adolescence from a Nationwide Birth Cohort. Acta Cardiol Sin. 2020, 36, 367–374. [Google Scholar]
- Chiriac, A.; Riley, D.C.; Russell, M.; Moore, J.P.; Padmanabhan, D.; Hodge, D.O.; Spiegel, M.R.; Vargas, E.R.; Phillips, S.D.; Ammash, N.M.; et al. Determinants of Sudden Cardiac Death in Adult Patients with Eisenmenger Syndrome. J. Am. Heart Assoc. 2020, 9, e014554. [Google Scholar] [CrossRef]
- Drakopoulou, M.; Nashat, H.; Kempny, A.; Alonso-González, R.; Swan, L.; Wort, S.J.; Price, L.C.; McCabe, C.; Wong, T.A.; Gatzoulis, M.; et al. Arrhythmias in adult patients with congenital heart disease and pulmonary arterial hypertension. Heart 2018, 104, 1963–1969. [Google Scholar] [CrossRef]
- Xu, Z.Y.; Li, Q.Q.; Zhang, C.; Zhang, H.S.; Gu, H. [Risk factors for death and the clinical features of different subtypes of patients with pulmonary arterial hypertension related to congenital heart disease]. Zhonghua Xin Xue Guan Bing Za Zhi 2020, 48, 315–322. [Google Scholar] [PubMed]
- Krexi, D.; Sheppard, M. Pulmonary hypertensive vascular changes in lungs of patients with sudden unexpected death. Emphasis on congenital heart disease, Eisenmenger syndrome, postoperative deaths and death during pregnancy and postpartum. J. Clin. Pathol. 2014, 68, 18–21. [Google Scholar] [CrossRef] [PubMed]
- Hull, D.A.; Shinebourne, E.; Gerlis, L.; Nicholson, A.G.; Sheppard, M.N. Rupture of pulmonary aneurysms in association with long-standing Waterston shunts. Cardiol. Young 2001, 11, 123–127. [Google Scholar] [CrossRef]
- Roos-Hesselink, J.; Baris, L.; Johnson, M.; De Backer, J.; Otto, C.; Marelli, A.; Jondeau, G.; Budts, W.; Grewal, J.; Sliwa, K.; et al. Pregnancy outcomes in women with cardiovascular disease: Evolving trends over 10 years in the ESC Registry of Pregnancy And Cardiac disease (ROPAC). Eur. Heart J. 2019, 40, 3848–3855. [Google Scholar] [CrossRef]
- Krexi, D.; Sheppard, M. Cardiovascular causes of maternal sudden death. Sudden Arrhythmic Death Syndrome is leading cause in UK. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 216, 261. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Pomares, J.M.; De La Pompa, J.L.; Franco, D.; Henderson, D.; Ho, S.Y.; Houyel, L.; Kelly, R.G.; Sedmera, D.; Sheppard, M.; Sperling, S.; et al. Congenital coronary artery anomalies: A bridge from embryology to anatomy and pathophysiology—A position statement of the development, anatomy, and pathology ESC Working Group. Cardiovasc. Res. 2016, 109, 204–216. [Google Scholar] [CrossRef] [PubMed]
- Hill, S.F.; Sheppard, M.N. A silent cause of sudden cardiac death especially in sport: Congenital coronary artery anomalies. Br. J. Sports Med. 2014, 48, 1151–1156. [Google Scholar] [CrossRef]
- Krexi, L.; Sheppard, M.N. Anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA), a forgotten congenital cause of sudden death in the adult. Cardiovasc. Pathol. 2013, 22, 294–297. [Google Scholar] [CrossRef]
- Finocchiaro, G.; Papadakis, M.; Robertus, J.L.; Dhutia, H.; Steriotis, A.K.; Tome, M.; Mellor, G.; Merghani, A.; Malhotra, A.; Behr, E.; et al. Etiology of Sudden Death in Sports: Insights from a United Kingdom Regional Registry. J. Am. Coll. Cardiol. 2016, 67, 2108–2115. [Google Scholar] [CrossRef]
- Finocchiaro, G.; Behr, E.R.; Tanzarella, G.; Papadakis, M.; Malhotra, A.; Dhutia, H.; Miles, C.; Diemberger, I.; Sharma, S.; Sheppard, M.N. Anomalous Coronary Artery Origin and Sudden Cardiac Death: Clinical and Pathological Insights from a National Pathology Registry. JACC Clin. Electrophysiol. 2019, 5, 516–522. [Google Scholar] [CrossRef]
- Hill, S.F.; Sheppard, M.N. Non-atherosclerotic coronary artery disease associated with sudden cardiac death. Heart 2010, 96, 1119–1125. [Google Scholar] [CrossRef] [PubMed]
- Dilaveris, P.; Koutagiar, I.; Alexopoulos, N.; Tsiachris, D.; Gatzoulis, K. Secondary prevention of sudden cardiac death in a 65 year untreated ALCAPA patient. Int. J. Cardiol. 2014, 176, e73–e74. [Google Scholar] [CrossRef] [PubMed]
- Subramaniam, K.; Sheppard, M. Thoracic aortic dissection. Death may not always be due to rupture with haemorrhage. Unusual complications which can be missed at autopsy. J. Forensic Leg. Med. 2018, 54, 127–129. [Google Scholar] [CrossRef]
- Tutarel, O.; Alonso-Gonzalez, R.; Montanaro, C.; Schiff, R.; Uribarri, A.; Kempny, A.; Grübler, M.R.; Uebing, A.; Swan, L.; Diller, G.-P.; et al. Infective endocarditis in adults with congenital heart disease remains a lethal disease. Heart 2017, 104, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Cooper, S.T.; Westaby, J.D.; Griffin, K.J.; Sheppard, M. The role of endocarditis in sudden cardiac death: Highlighting the value of the autopsy, pathological features and cardiac complications. Cardiovasc. Pathol. 2020, 50, 107292. [Google Scholar] [CrossRef] [PubMed]
- Wijesekera, N.T.; Sheppard, M.N.; Mullen, M.J. Candida endocarditis with mycotic pulmonary emboli following re-do Rastelli operation. Heart 2004, 90, e34. [Google Scholar] [CrossRef] [PubMed]
- Moore, B.; Cao, J.; Kotchetkova, I.; Celermajer, D.S. Incidence, predictors and outcomes of infective endocarditis in a contemporary adult congenital heart disease population. Int. J. Cardiol. 2017, 249, 161–165. [Google Scholar] [CrossRef]
- Lee, M.G.Y.; Babu-Narayan, S.V.; Kempny, A.; Uebing, A.; Montanaro, C.; Shore, D.F.; D’Udekem, Y.A.; Gatzoulis, M. Long-term mortality and cardiovascular burden for adult survivors of coarctation of the aorta. Heart 2019, 105, 1190–1196. [Google Scholar] [CrossRef]
- Oliver, J.M.; Gallego, P.; Gonzalez, A.E.; Avila, P.; Alonso, A.; Garcia-Hamilton, D.; Peinado, R.; Dos-Subirà, L.; Pijuan-Domenech, A.; Rueda, J.; et al. Predicting sudden cardiac death in adults with congenital heart disease. Heart 2020, 107, 67–75. [Google Scholar] [CrossRef]
- Yu, C.; Moore, B.M.; Kotchetkova, I.; Cordina, R.L.; Celermajer, D.S. Causes of death in a contemporary adult congenital heart disease cohort. Heart 2018, 104, 1678–1682. [Google Scholar] [CrossRef]
- Baumgartner, H.; De De Backer, J.; Babu-Narayan, S.V.; Budts, W.; Chessa, M.; Diller, G.-P.; Lung, B.; Kluin, J.; Lang, I.M.; Meijboom, F.; et al. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur. Heart J. 2020. [Google Scholar] [CrossRef] [PubMed]
- Vehmeijer, J.T.; Koyak, Z.; Zwinderman, A.H.; Harris, L.; Peinado, R.; Oechslin, E.N.; Silversides, C.K.; Bouma, B.J.; Budts, W.; Van Gelder, I.C.; et al. PREVENTION-ACHD: PRospEctiVE study on implaNTable cardioverter-defibrillator therapy and suddeN cardiac death in Adults with Congenital Heart Disease; Rationale and Design. Neth. Heart J. 2019, 27, 474–479. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sheppard, M.N. Sudden Death in Congenital Heart Disease: The Role of the Autopsy in Determining the Actual Cause. J. Cardiovasc. Dev. Dis. 2020, 7, 58. https://doi.org/10.3390/jcdd7040058
Sheppard MN. Sudden Death in Congenital Heart Disease: The Role of the Autopsy in Determining the Actual Cause. Journal of Cardiovascular Development and Disease. 2020; 7(4):58. https://doi.org/10.3390/jcdd7040058
Chicago/Turabian StyleSheppard, Mary N. 2020. "Sudden Death in Congenital Heart Disease: The Role of the Autopsy in Determining the Actual Cause" Journal of Cardiovascular Development and Disease 7, no. 4: 58. https://doi.org/10.3390/jcdd7040058
APA StyleSheppard, M. N. (2020). Sudden Death in Congenital Heart Disease: The Role of the Autopsy in Determining the Actual Cause. Journal of Cardiovascular Development and Disease, 7(4), 58. https://doi.org/10.3390/jcdd7040058



