Need for Coronary Artery Bypass Grafting in Acute Type A Aortic Dissection: Clinical Insights, Diagnostic Gaps, and Surgical Outcomes
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Definitions
2.4. Statistics
2.5. Surgical Strategy
3. Results
3.1. Patient Characteristics and Preoperative Data
3.2. Preoperative Biomarkers
3.3. Preoperative ECG Abnormalities
3.4. Intraoperative Data
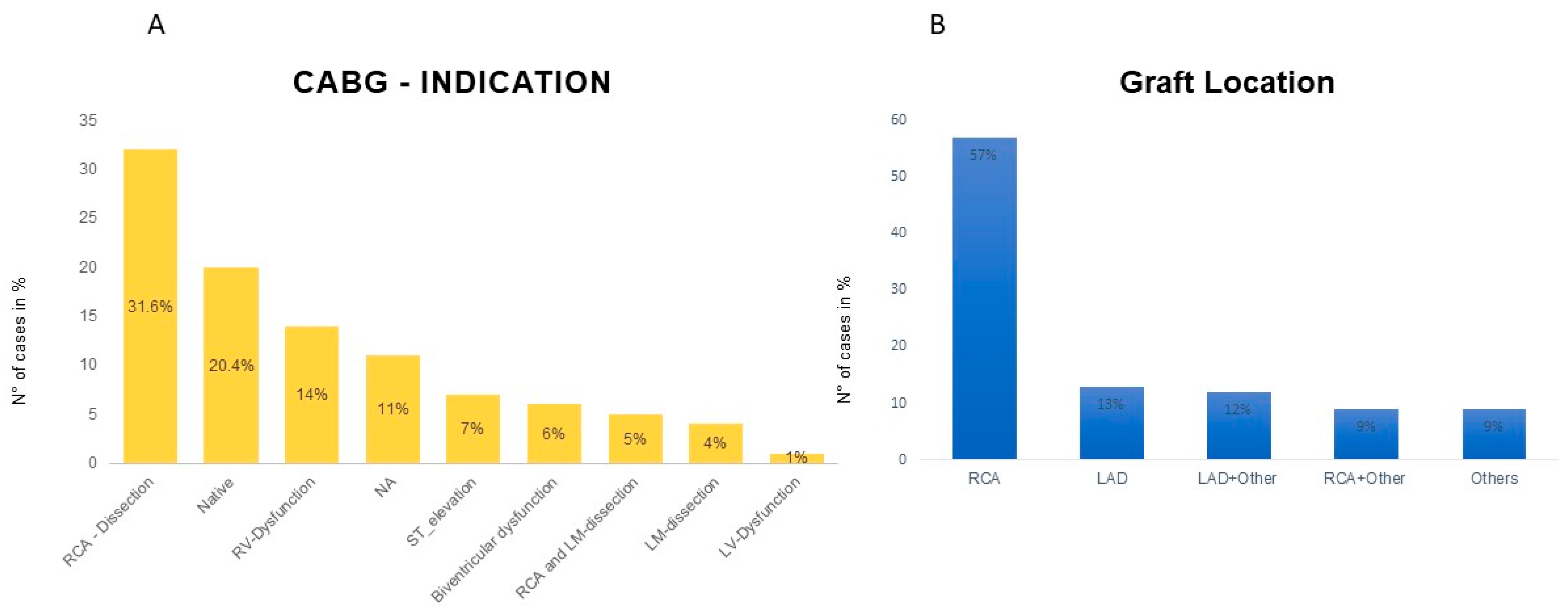
3.5. Blinded Independent Evaluation of Preoperative CT
3.6. Early Outcomes
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AF | Atrial fibrillation |
| ATAAD | Acute type A aortic dissection |
| AV block | Atrioventricular block |
| BMI | Body mass index |
| CABG | Coronary artery bypass grafting |
| CA | Coronary angiography |
| CAD | Coronary artery disease |
| CI | Confidence interval |
| CK | Creatine kinase |
| COPD | Chronic obstructive pulmonary disease |
| CPB | Cardiopulmonary bypass |
| CT | Computed tomography |
| ECLS | Extracorporeal life support |
| INR | International normalized ratio |
| LBBB | Left bundle branch block |
| LCOS | Low cardiac output syndrome |
| MI | Myocardial infarction |
| OR | Odds ratio |
| RBBB | Right bundle branch block |
| RVD | Right ventricular dysfunction |
| VES | Ventricular extrasystoles |
References
- Pape, L.A.; Awais, M.; Woznicki, E.M.; Suzuki, T.; Trimarchi, S.; Evangelista, A.; Myrmel, T.; Larsen, M.; Harris, K.M.; Greason, K.; et al. Presentation, Diagnosis, and Out-comes of Acute Aortic Dissection: 17-Year Trends from the International Registry of Acute Aortic Dissection. J. Am. Coll. Cardiol. 2015, 66, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Zheng, T.A.; Qiao, Z.Y.; Chen, L.; Ou, J.F.; Fang, W.G.; Li, C.N.; Chen, L.; Ma, W.G.; Zheng, J.; et al. Acute Aortic Dissection in Young Adult Patients: Clinical Characteristics, Management, and Perioperative Outcomes. J. Invest. Surg. 2019, 33, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Morjan, M.; Reser, D.; Savic, V.; Sromicki, J.; Maisano, F.; Mestres, C.A. Concomitant Coronary Artery Bypass in Patients with Acute Type A Aortic Dissection. Semin. Thorac. Cardiovasc. Surg. 2022, 34, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Fourth Universal Definition of Myocardial Infarction. J. Am. Coll. Cardiol. 2018, 72, 2231–2264. [Google Scholar] [CrossRef] [PubMed]
- Hicks, K.A.; Mahaffey, K.W.; Mehran RNissen, S.E.; Wiviott, S.D.; Dunn, B.; Solomon, S.D.; Marler, J.R.; Teerlink, J.R.; Farb, A.; Morrow, D.A.; et al. 2017 Cardiovascular and Stroke Endpoint Definitions for Clinical Trials. J. Am. Coll. Cardiol. 2018, 71, 1021–1034. [Google Scholar] [CrossRef] [PubMed]
- Mehta, R.L.; Kellum, J.A.; Shah, S.V.; Molitoris, B.A.; Ronco, C.; Warnock, D.G.; Levin, A. Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury. Crit. Care 2007, 11, R31. [Google Scholar] [CrossRef] [PubMed]
- Pitts, L.; Kofler, M.; Montagner, M.; Heck, R.; Kurz, S.D.; Sündermann, S.; Falk, V.; Kempfert, J. The role of concomitant coronary artery bypass grafting in acute type A aortic dissection complicated by coronary malperfusion. Eur. J. Cardiothorac. Surg. 2024, 66, ezae248. [Google Scholar] [CrossRef] [PubMed]
- Neri, E.; Toscano, T.; Papalia UFrati, G.; Massetti, M.; Capannini, G.; Tucci, E.; Buklas, D.; Muzzi, L.; Oricchio, L.; Sassi, C. Proximal aortic dissection with coronary malperfusion: Presentation, management, and outcome. J. Thorac. Cardiovasc. Surg. 2001, 121, 552–560. [Google Scholar] [CrossRef] [PubMed]
- Kawahito, K.; Adachi, H.; Murata, S.; Yamaguchi, A.; Ino, T. Coronary malperfusion due to type A aortic dissection: Mechanism and surgical management. Ann. Thorac. Surg. 2003, 76, 1471–1476. [Google Scholar] [CrossRef] [PubMed]
- Kreibich, M.; Bavaria, J.E.; Branchetti, E.; Brown, C.R.; Chen, Z.; Khurshan, F.; Siki, M.; Vallabhajosyula, P.; Szeto, W.Y.; Desai, N.D. Management of Patients With Coronary Artery Malperfusion Secondary to Type A Aortic Dissection. Ann. Thorac. Surg. 2019, 107, 1174–1180. [Google Scholar] [CrossRef] [PubMed]
- Kaul, T.K.; Fields, B.L. Postoperative acute refractory right ventricular failure: Incidence, pathogenesis, management and prognosis. Cardiovasc. Surg. 2000, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Allen, B.S.; Winkelmann, J.W.; Hanafy, H.; Hartz, R.S.; Bolling, K.S.; Ham, J.; Feinstein, S. Retrograde cardioplegia does not ade-quately perfuse the right ventricle. J. Thorac. Cardiovasc. Surg. 1995, 109, 1116–1124. [Google Scholar] [CrossRef] [PubMed]
- Pergola, V.; Continisio, S.; Mantovani, F.; Motta, R.; Mattesi, G.; Marrazzo, G.; Dellino, C.M.; Montonati, C.; De Conti, G.; Galzerano, D.; et al. Spontaneous coronary artery dissection: The emerging role of coronary computed tomography. Eur. Heart J. Cardiovasc. Imaging 2023, 24, 839–850. [Google Scholar] [CrossRef] [PubMed]
- The DISCHARGE Trial Group. CT or invasive coronary angiography in stable chest pain. N. Engl. J. Med. 2022, 386, 1591–1602. [Google Scholar] [CrossRef] [PubMed]
- Moorthy, P.S.K.; Sakijan, A.S. Malperfusion in acute type A aortic dissection: How we handle the challenge? Indian J. Thorac. Cardiovasc. Surg. 2022, 38 (Suppl. 1), 122–131. [Google Scholar] [CrossRef] [PubMed]
- Stefanini, G.G.; Windecker, S. Can coronary computed tomography angiography replace invasive angiography? Cor-onary computed tomography angiography cannot replace invasive angiography. Circulation 2015, 131, 418–425; discussion 426. [Google Scholar] [CrossRef] [PubMed]
- Motallebzadeh, R.; Batas, D.; Valencia, O.; Chandrasekaran, V.; Smith, J.; Brecker, S.; Jahangiri, M. The role of coronary angiography in acute type A aortic dissection. Eur. J. Cardio-thorac. Surg. 2004, 25, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Penn, M.S.; Smedira, N.; Lytle, B.; Brener, S.J. Does coronary angiography before emergency aortic surgery affect in-hospital mortality? J. Am. Coll. Cardiol. 2000, 35, 889–894. [Google Scholar] [CrossRef] [PubMed]

| In-Hospital Death (Group B, n = 26) | In-Hospital Survivors (Group A, n = 72) | p-Value | |
|---|---|---|---|
| Age (y) | 65.94 ± 10.93 | 63.69 ± 13.76 | 0.445 |
| Sex (female, %) | 11 (18.64) | 25 (26.32) | 0.330 |
| BMI (kg/m2) | 26.7 (20.8–42.7) | 25.5 (17.30–49.40) | 0.106 |
| EuroscoreⅡ, % | 22.77 (6.47–67.19) | 13.11 (5.99–69.64) | 0.012 |
| GERAADA-Score, % | 22.55 (7.20–69.40) | 14.7 (6.30–66.60) | 0.002 |
| MI (n,%) | 3 (11.54) | 8 (11.11) | 1.00 |
| Any Organ Malperfusion * (n,%) | 13 (50) | 24 (33.33) | 0.293 |
| Cardiogenic Shock (n,%) | 8 (30.77) | 11 (15.28) | 0.156 |
| AF (n,%) | 4 (15.38) | 9 (12.50) | 0.714 |
| Renal Failure (n,%) | 0 | 2 (2.78) | 0.773 |
| COPD (n,%) | 2 (7.69) | 4 (5.56) | 0.654 |
| Diabetes (n,%) | 3 (11.54) | 5 (6.94) | 0.434 |
| Hypertension (n,%) | 19 (73.08) | 50 (69.44) | 0.806 |
| Stroke in History (n,%) | 4 (15.38) | 8 (11.11) | 0.728 |
| Variables | In-Hospital Death (Group B, n = 26) | In-Hospital Survivors (Group A, n = 72) | p-Value |
|---|---|---|---|
| Bradycardia (n,%) | 5 (19.23) | 13 (18.06) | 0.851 |
| Ventricular fibrillation (n,%) | 1 (3.85) | 0 (0.00%) | 0.215 |
| VES (n,%) | 3 (11.54) | 2 (2.78) | 0.198 |
| AV block (n,%) | 2 (7.69) | 8 (11.11) | 0.735 |
| LBBB/RBBB (n,%) | 4 (15.38) | 9 (12.50) | 0.811 |
| AF (n,%) | 6 (23.08) | 19 (26.39) | 0.780 |
| T-wave inversion (n,%) | 11 (42.31) | 22 (30.56) | 0.517 |
| Variables | In-Hospital Death (n = 26) | In-Hospital Survive (n = 72) | p-Values |
|---|---|---|---|
| Operation Time (min) | 457 (275,847) | 377 (185,749) | 0.478 |
| CPB Time (min) | 304 (272,360) | 177 (108,249) | 0.004 |
| Cross-Clamp Time (min) | 318 (272,384) | 137 (94,224) | 0.006 |
| Antegrade Cerebral Perfusion Time (min) | 30 (19,39) | 18 (12,40) | 0.22 |
| Root Repair (David/Yacoub)(n,%) | 2 (7.69) | 20 (27.78) | 0.107 |
| Conduit Implantation (n,%) | 12 (46.15) | 26 (36.11) | 0.368 |
| Bio-Prothesis (n,%) | 14 (53.85) | 16 (22.22) | 0.011 |
| Mechanical Prothesis (n,%) | 0 | 7 (9.72) | 0.184 |
| Aorta Arch Replacement | |||
| Hemiarch (n,%) | 20 (76.92) | 42 (58.33) | 0,9 |
| Total Arch (n,%) | 3 (11.54) | 8 (11.11) | 1 |
| Inspection—Positive | Inspection—Negative | |
|---|---|---|
| CT—Positive | 25 | 30 |
| CT—Negative | 5 | 12 |
| Variables | In-Hospital Death (Group B, n = 26) | In-Hospital Survivors (Group A, n = 72) | p-Value |
|---|---|---|---|
| ICU stay (h) | 54.35 (6–1562) | 191.5 (14–1637) | 0.001 |
| Hospital stay (d) | 2 (0–77) | 19 (5–198) | 0.001 |
| Ventilation time (h) | 64.63 (18–518) | 92.75 (13–1323) | 0.066 |
| Postoperative LCOS (n,%) | 16 (61.54) | 14 (19.44) | 0.001 |
| ECLS (n,%) | 14 (53.85) | 4 (5.56) | 0.001 |
| Neurological events (n,%) | 15 (57.69) | 48 (66.67) | 0.001 |
| Reintubation (n,%) | 2 (7.69) | 24 (33.33) | 0.030 |
| New dissection (n,%) | 1 (3.85) | 3 (4.17) | 1.000 |
| Infections (n,%) | 6 (23.08) | 45 (62.50) | 0.001 |
| Malperfusion (n,%) | 18 (69.23) | 44 (61.11) | 0.025 |
| Dialysis/CVVHD (n,%) | 12 (46.15) | 25 (34.72) | 0.349 |
| Variables | B | SE | Wald | OR | OR: 95%CI | p-Values |
|---|---|---|---|---|---|---|
| Age | 0.026 | 0.029 | 0.801 | 1.026 | 0.970–1.085 | 0.371 |
| Sex | 1.024 | 0.718 | 2.032 | 2.784 | 0.681–11.382 | 0.154 |
| INR | 2.325 | 1.227 | 3.591 | 10.227 | 0.924–113.257 | 0.058 |
| CK(U/L) | 0.002 | 0.001 | 4.048 | 1.003 | 1.000–1.005 | 0.044 |
| Troponin(ng/dL) | −0.001 | 0.001 | 1.072 | 0.999 | 0.998–1.001 | 0.301 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morjan, M.; Jürgens, C.P.; Li, T.; Vallejo Castano, L.J.; Jenkins, F.; Thwairan, A.; Weyers, V.; Dalyanoglu, H.; Reinartz, S.D.; Lichtenberg, A. Need for Coronary Artery Bypass Grafting in Acute Type A Aortic Dissection: Clinical Insights, Diagnostic Gaps, and Surgical Outcomes. J. Cardiovasc. Dev. Dis. 2025, 12, 336. https://doi.org/10.3390/jcdd12090336
Morjan M, Jürgens CP, Li T, Vallejo Castano LJ, Jenkins F, Thwairan A, Weyers V, Dalyanoglu H, Reinartz SD, Lichtenberg A. Need for Coronary Artery Bypass Grafting in Acute Type A Aortic Dissection: Clinical Insights, Diagnostic Gaps, and Surgical Outcomes. Journal of Cardiovascular Development and Disease. 2025; 12(9):336. https://doi.org/10.3390/jcdd12090336
Chicago/Turabian StyleMorjan, Mohammed, Charlotte Philippa Jürgens, Tong Li, Luis Jaime Vallejo Castano, Freya Jenkins, Amin Thwairan, Vivien Weyers, Hannan Dalyanoglu, Sebastian Daniel Reinartz, and Artur Lichtenberg. 2025. "Need for Coronary Artery Bypass Grafting in Acute Type A Aortic Dissection: Clinical Insights, Diagnostic Gaps, and Surgical Outcomes" Journal of Cardiovascular Development and Disease 12, no. 9: 336. https://doi.org/10.3390/jcdd12090336
APA StyleMorjan, M., Jürgens, C. P., Li, T., Vallejo Castano, L. J., Jenkins, F., Thwairan, A., Weyers, V., Dalyanoglu, H., Reinartz, S. D., & Lichtenberg, A. (2025). Need for Coronary Artery Bypass Grafting in Acute Type A Aortic Dissection: Clinical Insights, Diagnostic Gaps, and Surgical Outcomes. Journal of Cardiovascular Development and Disease, 12(9), 336. https://doi.org/10.3390/jcdd12090336






