1. Introduction
Thoracic endovascular aortic repair (TEVAR) has significantly improved the management of complex aortic arch pathologies, offering a less invasive alternative to open surgery. However, the presence of anatomical anomalies such as an aberrant right subclavian artery (ARSA) can complicate procedural planning and execution. ARSA, a congenital vascular variant in which the right subclavian artery (RSA) arises distal to the left subclavian artery (LSA), occurs in approximately 0.16% to 1.8–2% of the population [
1,
2]. While often asymptomatic, its atypical origin and retroesophageal course may limit available proximal landing zones for endograft fixation and increase the risk of neurological or ischemic complications if not adequately addressed.
In recent years, the development of branched stent graft technology, including the Castor single-branched stent graft (CSBSG), has enabled targeted revascularization of critical arch vessels during endovascular procedures. This prosthesis, designed with an integrated side branch, allows for the preservation of perfusion to the LSA, even when its origin must be covered to achieve adequate sealing of the aortic arch.
We present a case in which a hybrid approach was employed to treat a distal aortic arch aneurysm in a patient with ARSA.
2. Case Presentation
A 78-year-old man, who had previously undergone ascending aorta replacement and aortic valve shaving in 2022, was found during follow-up computed tomography angiography (CTA) to have enlargement of a distal aortic arch aneurysm (58 × 57 mm). Additionally, CTA revealed the presence of an ARSA originating distal to the LSA, coursing posteriorly between the esophagus and trachea.
The patient’s medical history was notable for hypertension, dyslipidemia, and a family history of coronary artery disease and cerebrovascular disorders.
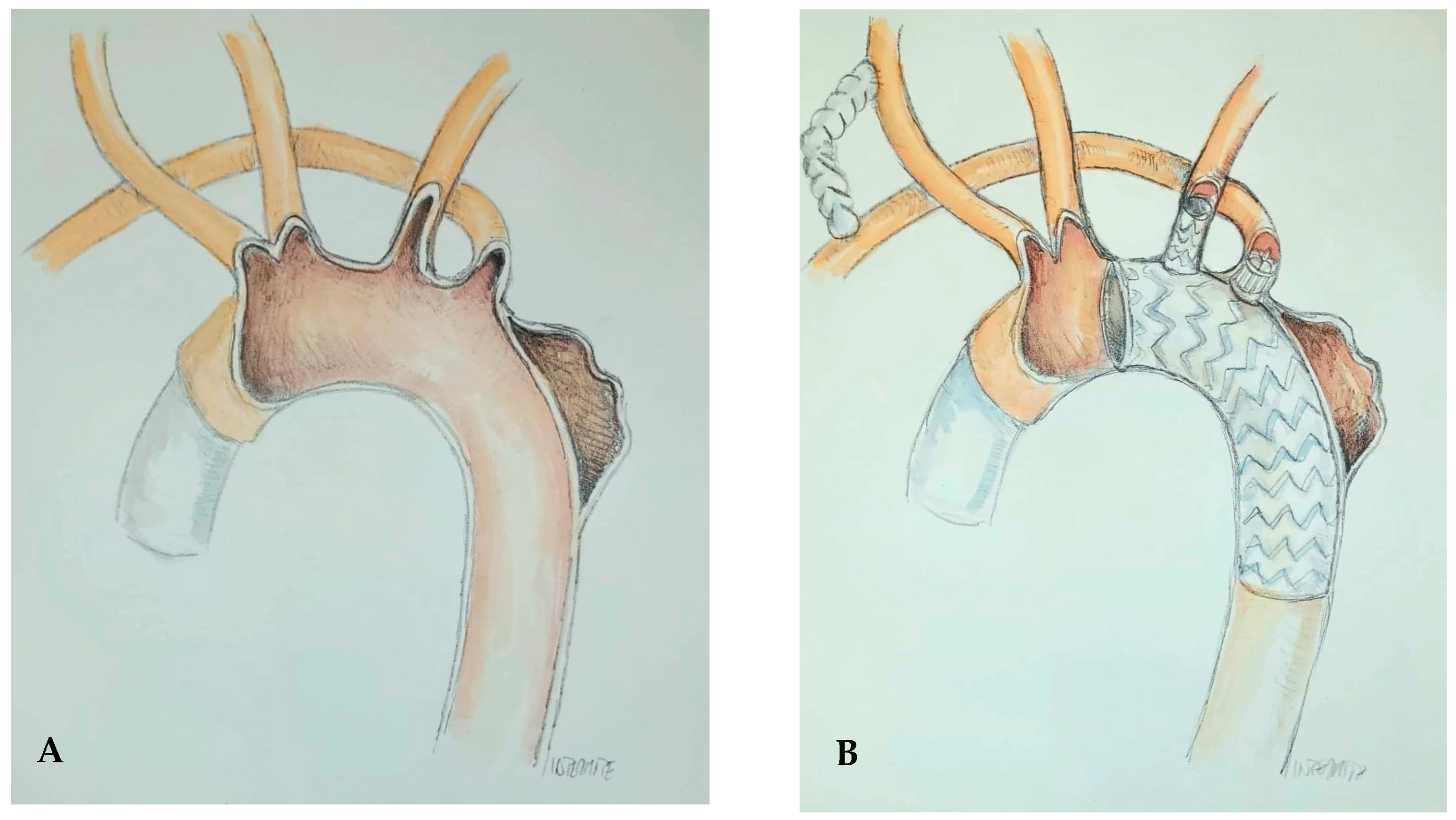
Following multidisciplinary discussion within the Aortic Team, a personalized hybrid strategy was planned to manage the aortic arch aneurysm in the context of ARSA. A schematic representation of the procedure is shown in
Figure 1.
Initially, the right common carotid artery (RCCA) and the ARSA were exposed through a cervical incision. An 8 mm Dacron graft was anastomosed end-to-side to the RCCA and then to the ARSA to create a right carotid-subclavian bypass. The right and left common femoral arteries (RCFA and LCFA) were accessed with 6 Fr sheaths. The right and left brachial arteries (RBA and LBA) were cannulated using 8 Fr and 10 Fr sheaths, respectively.
A pre-closure technique was performed in the RCFA using two Perclose™ ProStyle™ suture-mediated closure systems (Abbott Vascular, Santa Clara, CA, USA), and a 24 Fr DrySeal sheath was introduced. Unfractionated heparin was administered at a dose of 100 U/kg, targeting an activated clotting time (ACT) of 300 s.
A Terumo guidewire was advanced from the LBA into the descending thoracic aorta, snared with a gooseneck device, and exteriorized through the DrySeal sheath in the RCFA to establish through-and-through access. A multipurpose A1 (MPA1) catheter was then advanced over this wire from the LBA and exteriorized via the RCFA. The free end of the traction wire attached to the branch of the Castor single-branched stent graft (CSBSG) was introduced into the MPA1 catheter through the RCFA and retrieved from the LBA.
A Lunderquist extra-stiff guidewire (Cook Medical, Bloomington, IN, USA) was inserted into the ascending aorta via femoral access, followed by advancement of the delivery sheath. The CSBSG was rotated to align its branch with the outer curvature of the aortic arch. An angiographic assessment confirmed correct alignment and ensured that the branch traction wire was not entangled.
The stent graft was then carefully advanced and deployed within the arch, with the branch directed into the LSA. During deployment of the main body, systolic blood pressure was pharmacologically reduced to approximately 90 mmHg to enhance placement accuracy. After confirming position under fluoroscopy, the trigger wire was pulled to deploy the main body, followed by deployment of the branch using the traction wire. Once deployment was complete, blood pressure was normalized and angiography confirmed aneurysm exclusion and branch patency.
To prevent a type II endoleak, a vascular plug was delivered via the RBA and deployed at the origin of the ARSA. The RCFA was closed using the previously placed Perclose™ ProStyle™ sutures. Hemostasis at the brachial accesses was achieved with 15 min of manual compression followed by bandaging. The LCFA was closed using the Perclose™ ProStyle™ system.
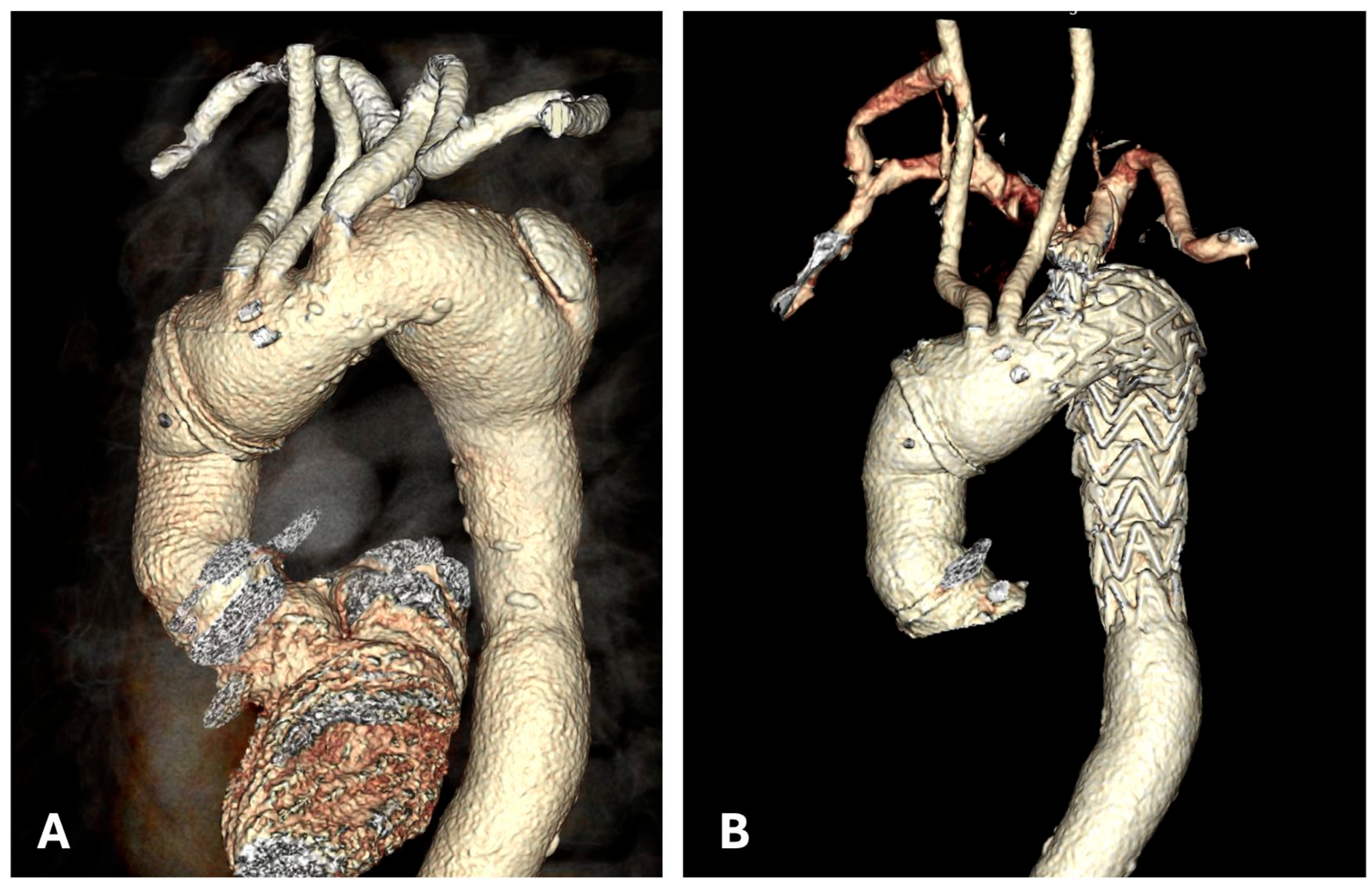
A final angiographic evaluation confirmed successful exclusion of the aneurysm and satisfactory perfusion of the supra-aortic vessels (
Figure 2). The patient was discharged five days later on dual antiplatelet therapy (aspirin 100 mg and clopidogrel 75 mg) for three months, followed by lifelong aspirin monotherapy.
At the three-week follow-up, the patient was asymptomatic with stable hemodynamics and no complications. Follow-up CTA confirmed optimal procedural results (
Figure 3).
3. Discussion
This case report highlights a TEVAR performed for a distal arch aneurysm in a patient with an ARSA that originates distal to LSA. Notable aspects of this case include: (1) the use of the CSBSG for aneurysm exclusion, which effectively maintains patency of the LSA; (2) the creation of a right carotid-subclavian bypass involving the ARSA to ensure perfusion to the right upper vascular structures; (3) the implantation of a plug at the origin of the ARSA to prevent type 2 endoleaks. Significant advancements in endovascular stent graft design have facilitated their application in the distal aortic arch and proximal descending aorta [
3]. However, the length of the proximal landing zone remains a critical limitation for TEVAR, especially concerning the LSA [
4]. Several studies have indicated that covering the LSA can heighten risks of arm ischemia, vertebrobasilar insufficiency, anterior circulation strokes, and paraplegia [
5]. Therefore, the European Society for Vascular Surgery guidelines advocate routine LSA revascularization during TEVAR, particularly for patients at high risk of neurological complications [
6]. Various techniques for LSA revascularization have been proposed, such as carotid-subclavian bypass, fenestrated devices, chimney techniques, and hybrid approaches [
7]. Among them, the Castor single-branched stent graft (Microport Medical) has proven to be highly feasible and efficient, securing an adequate proximal landing zone while preserving necessary LSA perfusion, with favorable outcomes observed at one-year follow-up [
8,
9].
In our case, the Castor stent graft was employed with the side branch introduced into the LSA to ensure patency and provide an adequate landing zone; the main body was positioned to exclude the aneurysm of the distal arch. The presence of a complex anatomical variant, specifically the ARSA, necessitated the creation of a single right carotid-subclavian bypass to assure perfusion to the right-sided territories. In this instance, the ARSA originated distal to the LSA; therefore, the deployment of the Castor stent graft adequately covered its origin from the arch. To prevent ischemia in the territories supplied by the ARSA, we proceeded with the preventive creation of the aforementioned right carotid-subclavian bypass.
Our team previously described a case involving a double carotid-subclavian bypass followed by the endovascular exclusion of a Kommerell diverticulum and bilateral subclavian artery occlusion in a right-sided aortic arch with an aberrant LSA, although this was executed without utilizing the Castor prosthesis [
8].
On the other hand, in the present case to thwart the occurrence of type 2 endoleak a plug was implanted at the origin of the ARSA via the brachial artery, ensuring a secure closure of this anatomical anomaly.
In our scenario an endovascular approach was preferred over open surgery, as the patient had undergone a surgical replacement of the ascending aorta and aortic valve repair two years prior. Engaging in a redo surgical intervention would have represented a higher risk for the patient.
To the best of our knowledge, this is the first case involving the deployment of a single-branched Castor stent graft in a patient with a distal aortic arch aneurysm and ARSA, revascularized through a single right carotid-subclavian bypass.
4. Conclusions
This case highlights the value of a customized hybrid approach in the management of distal aortic arch aneurysms, particularly in the presence of complex anatomical variants such as ARSA. By combining surgical revascularization with the use of a CSBSG, it is possible to achieve effective aneurysm exclusion while preserving perfusion to both subclavian arteries. This strategy significantly reduced the risk of neurological and ischemic complications, in line with current guidelines advocating for routine LSA revascularization during TEVAR. To our knowledge, this represents the first documented case employing this specific hybrid configuration for ARSA-associated aortic arch pathology. Our experience underscores the importance of individualized procedural planning and the potential of branched endografts in treating patients with complex aortic anatomy safely and effectively.
Author Contributions
Conceptualization: A.R., M.C., A.B., and G.T.; Data curation: M.C., A.B., and G.T.; Project administration: A.R., S.D.S., M.C., A.B., G.T., M.M., P.F., C.P., M.S., and S.B.; Supervision: S.D.S., M.M., P.F., C.P., M.S., S.B., and A.R.; Visualization: M.C., A.B., and G.T.; Writing—original draft: A.B.; Writing—review and editing: A.R., M.C., and G.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
All procedures performed were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. The local Ethics Committee (Comitato Etico di Area Vasta Nord Ovest [CEAVNO], Study ID No. 26429/2024).
Informed Consent Statement
Written informed consent was obtained from the patient for the publication of this casereport and any accompanying images. No identifiable patient information is included in this report. Ethical approval for the publication of this case report was not required as it is based on a single anonymized patient case, in line with institutional guidelines for case report publication.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Abbreviations
The following abbreviations are used in this manuscript:
| TEVAR | Thoracic Endovascular Aortic Repair |
| ARSA | Aberrant Right Subclavian Artery |
| RSA | Right Subclavian Artery |
| LSA | Left Subclavian Artery |
| CSBSG | Castor Single-Branched Stent Graft |
| CTA | Computed Tomography Angiography |
| RCCA | Right Common Carotid Artery |
| RCFA | Right Common Femoral Artery |
| LCFA | Left Common Femoral Artery |
| RBA | Right Brachial Artery |
| LBA | Left Brachial Artery |
| MPA1 | Multipurpose A1 (catheter) |
| ACT | Activated Clotting Time |
References
- Choi, Y.; Chung, S.B.; Kim, M.S. Prevalence and Anatomy of Aberrant Right Subclavian Artery Evaluated by Computed Tomographic Angiography at a Single Institution in Korea. J. Korean Neurosurg. Soc. 2019, 62, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Heye, T.; Greiten, L.; Story-Hefta, L.; Reemtsen, B.; Moursi, M. Aberrant right subclavian artery: A novel approach and an overview of operative techniques. J. Vasc. Surg. Cases Innov. Tech. 2023, 9, 101327. [Google Scholar] [CrossRef] [PubMed]
- Luo, Z.-R.; Zhang, J.-X.; Huang, Z.-Y.; Chen, L.-W. Endovascular repair of aortic pathologies involving the aortic arch using castor stent-graft combined with in-vitro fenestration technology. BMC Cardiovasc. Disord. 2023, 23, 107. [Google Scholar] [CrossRef] [PubMed]
- Yoon, W.J.; Mell, M.W. Outcome comparison of thoracic endovascular aortic repair performed outside versus inside proximal landing zone length recommendation. J. Vasc. Surg. 2020, 72, 1883–1890. [Google Scholar] [CrossRef] [PubMed]
- Rizvi, A.Z.; Murad, M.H.; Fairman, R.M.; Erwin, P.J.; Montori, V.M. The effect of left subclavian artery coverage on morbidity and mortality in patients undergoing endovascular thoracic aortic interventions: A systematic review and meta-analysis. J. Vasc. Surg. 2009, 50, 1159–1169. [Google Scholar] [CrossRef] [PubMed]
- Riambau, V.; Böckler, D.; Brunkwall, J.; Cao, P.; Chiesa, R.; Coppi, G.; Czerny, M.; Fraedrich, G.; Haulon, S.; Jacobs, M.; et al. Editor’s Choice—Management of Descending Thoracic Aorta Diseases. Eur. J. Vasc. Endovasc. Surg. 2017, 53, 4–52. [Google Scholar] [CrossRef] [PubMed]
- D’Oria, M.; Mani, K.; DeMartino, R.; Czerny, M.; Donas, K.P.; Wanhainen, A.; Lepidi, S. Narrative review on endovascular techniques for left subclavian artery revascularization during thoracic endovascular aortic repair and risk factors for postoperative stroke. Interact. Cardiovasc. Thorac. Surg. 2021, 32, 764–772. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; He, X.; Liu, B.; Liu, P.; Jiang, X.; Yang, Y.; Zhang, L. Outcomes of Castor Single-Branched Stent Graft for Reconstruction of Multiple Supra-Aortic Branches in Aortic Arch Disease. J. Endovasc. Ther. 2023. [Google Scholar] [CrossRef] [PubMed]
- Rizza, A.; Trimarchi, G.; Di Sibio, S.; Bastiani, L.; Murzi, M.; Palmieri, C.; Foffa, I.; Berti, S. Preliminary Outcomes of Zone 2 Thoracic Endovascular Aortic Repair Using Castor Single-Branched Stent Grafts: A Single-Center Experience. J. Clin. Med. 2023, 12, 7593. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).