Systematic Review on HRV Reference Values
Abstract
1. Introduction
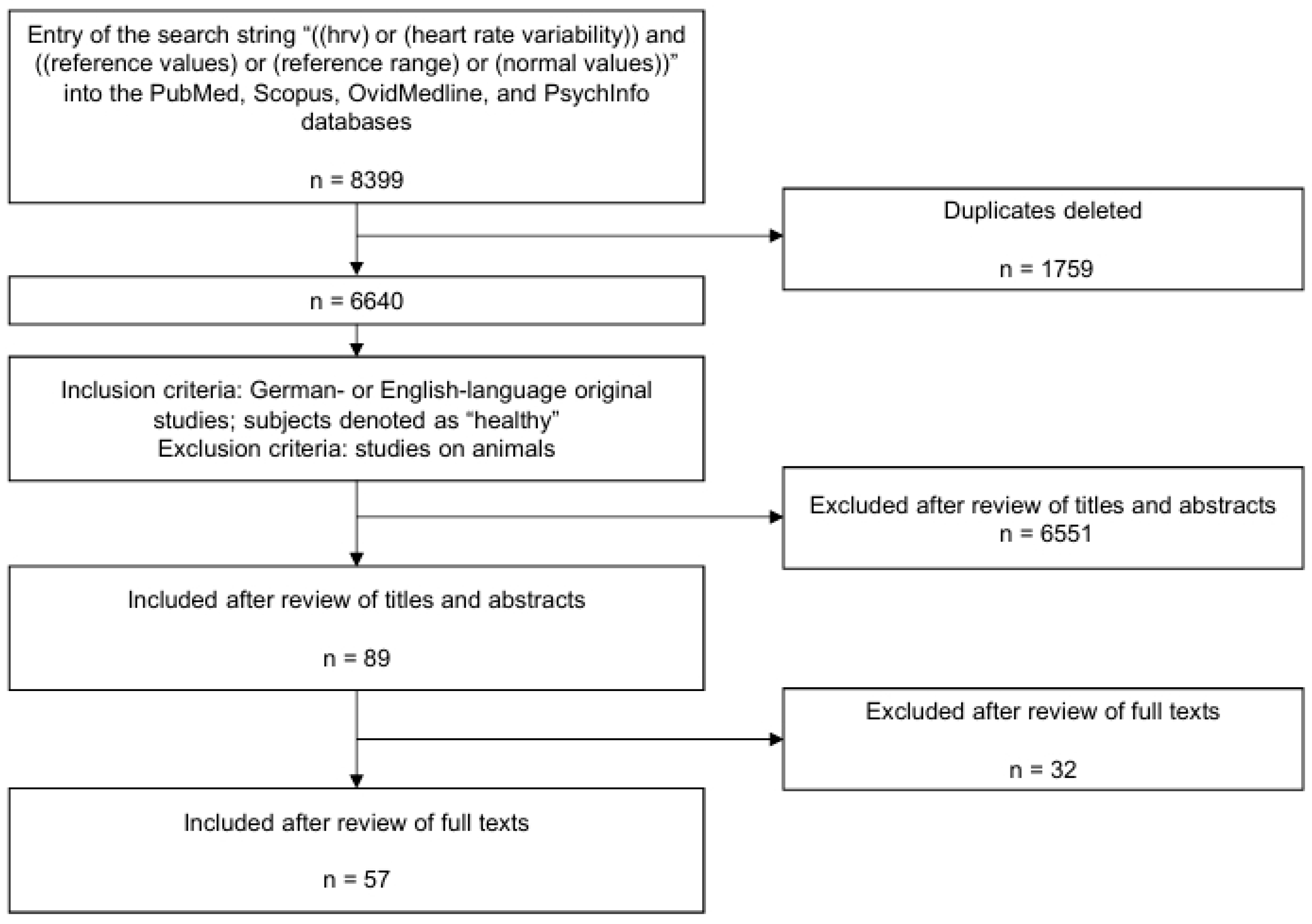
2. Materials and Methods
3. Results
4. Discussion
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HRV | heart rate variability |
| SD | standard deviation |
| RMSSD | Root Mean Square of successive differences |
| SDNN | Standard deviation of NN intervals |
| LF | Low frequency |
| HF | High frequency |
References
- Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Eur. Heart J. 1996, 17, 354–381. [CrossRef]
- Sammito, S.; Bockelmann, I. Reference values for time- and frequency-domain heart rate variability measures. Heart Rhythm 2016, 13, 1309–1316. [Google Scholar] [CrossRef]
- Sassi, R.; Cerutti, S.; Lombardi, F.; Malik, M.; Huikuri, H.V.; Peng, C.-K.; Schmidt, G.; Yamamoto, Y. Advances in heart rate variability signal analysis: Joint position statement by the e-Cardiology ESC Working Group and the European Heart Rhythm Association co-endorsed by the Asia Pacific Heart Rhythm Society. EP Eur. 2015, 17, 1341–1353. [Google Scholar] [CrossRef] [PubMed]
- Sammito, S.; Thielmann, B.; Klussmann, A.; Deußen, A.; Braumann, K.-M.; Böckelmann, I. Guideline for the application of heart rate and heart rate variability in occupational medicine and occupational health science. J. Occup. Med. Toxicol. 2024, 19, 15. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, A.; Vagedes, J. How accurate is pulse rate variability as an estimate of heart rate variability? A review on studies comparing photoplethysmographic technology with an electrocardiogram. Int. J. Cardiol. 2013, 166, 15–29. [Google Scholar] [CrossRef]
- Bigger, J.T.; Fleiss, J.L.; Steinman, R.C.; Rolnitzky, L.M.; Schneider, W.J.; Stein, P.K. RR variability in healthy, middle-aged persons compared with patients with chronic coronary heart disease or recent acute myocardial infarction. Circulation 1995, 91, 1936–1943. [Google Scholar] [CrossRef]
- Nunan, D.; Sandercock, G.R.; Brodie, D.A. A Quantitative Systematic Review of Normal Values for Short-Term Heart Rate Variability in Healthy Adults. Pacing Clin. Electrophysiol. 2010, 33, 1407–1417. [Google Scholar] [CrossRef]
- Kim, G.M.; Woo, J.M. Determinants for Heart Rate Variability in a Normal Korean Population. J. Korean Med. Sci. 2011, 26, 1293–1298. [Google Scholar] [CrossRef]
- Voss, A.; Heitmann, A.; Schroeder, R.; Peters, A.; Perz, S. Short-term heart rate variability-age dependence in healthy subjects. Physiol. Meas. 2012, 33, 1289–1311. [Google Scholar] [CrossRef]
- Voss, A.; Schroeder, R.; Heitmann, A.; Peters, A.; Perz, S. Short-term heart rate variability—Influence of gender and age in healthy subjects. PLoS ONE 2015, 10, e0118308. [Google Scholar] [CrossRef]
- Sammito, S.; Bockelmann, I. Age and gender-related reference values for the use of heart rate variability in motion therapy. Bewegungstherapie Gesundheitssport 2017, 33, 268–275. [Google Scholar] [CrossRef]
- Sammito, S.; Bockelmann, I. New reference values of heart rate variability during ordinary daily activity. Heart Rhythm 2017, 14, 304–307. [Google Scholar] [CrossRef] [PubMed]
- Zeng, F.; Tang, Z.H.; Li, Z.; Yu, X.; Zhou, L. Normative reference of short-term heart rate variability and estimation of cardiovascular autonomic neuropathy prevalence in Chinese people. J. Endocrinol. Investig. 2014, 37, 385–391. [Google Scholar] [CrossRef]
- Sammito, S.; Thielmann, B.; Böckelmann, I. Update: Factors influencing heart rate variability—A narrative review. Front. Physiol. 2024, 15, 1430458. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- van den Berg, M.E.; Rijnbeek, P.R.; Niemeijer, M.N.; Hofman, A.; van Herpen, G.; Bots, M.L.; Hillege, H.; Swenne, C.A.; Eijgelsheim, M.; Stricker, B.H.; et al. Corrigendum: Normal Values of Corrected Heart-Rate Variability in 10-Second Electrocar-diograms for All Ages. Front. Physiol. 2019, 10, 1373. [Google Scholar] [CrossRef]
- van den Berg, M.E.; Rijnbeek, P.R.; Niemeijer, M.N.; Hofman, A.; van Herpen, G.; Bots, M.L.; Hillege, H.; Swenne, C.A.; Eijgelsheim, M.; Stricker, B.H.; et al. Normal Values of Corrected Heart-Rate Variability in 10-Second Electrocardiograms for All Ages. Front. Physiol. 2018, 9, 424. [Google Scholar] [CrossRef]
- Tang, Z.H.; Wang, L.; Zeng, F.F.; Li, Z.T.; Yu, X.L.; Zhang, K.Q.; Zhou, L.N. Bayesian estimation of cardiovascular autonomic neuropathy diagnostic test based on short-term heart rate variability without a gold standard. BMJ Open 2014, 4, e005096. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.F.; Korevaar, D.A.; Altman, D.G.; Bruns, D.E.; Gatsonis, C.A.; Hooft, L.; Irwig, L.; Levine, D.; Reitsma, J.B.; de Vet, H.C.W.; et al. STARD 2015 guidelines for reporting diagnostic accuracy studies: Explanation and elaboration. BMJ Open 2016, 6, e012799. [Google Scholar] [CrossRef]
- Dobbs, W.C.; Fedewa, M.V.; MacDonald, H.V.; Holmes, C.J.; Cicone, Z.S.; Plews, D.J.; Esco, M.R. The Accuracy of Acquiring Heart Rate Variability from Portable Devices: A Systematic Review and Meta-Analysis. Sports Med. 2019, 49, 417–435. [Google Scholar] [CrossRef]
- Urooj, M.; Pillai, K.K.; Tandon, M.; Venkateshan, S.P.; Saha, N. Reference ranges for time domain parameters of heart rate variability in indian population and validation in hypertensive subjects and smokers. Int. J. Pharm. Pharm. Sci. 2011, 3, 36–39. [Google Scholar]
- Acharya U, R.; Kannathal, N.; Sing, O.W.; Ping, L.Y.; Chua, T. Heart rate analysis in normal subjects of various age groups. Biomed. Eng. Online 2004, 3, 24. [Google Scholar] [CrossRef]
- Agelink, M.W.; Malessa, R.; Baumann, B.; Majewski, T.; Akila, F.; Zeit, T.; Ziegler, D. Standardized tests of heart rate variability: Normal ranges obtained from 309 healthy humans, and effects of age, gender, and heart rate. Clin. Auton. Res. 2001, 11, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Baldzer, K.; Dykes, F.D.; Jones, S.A.; Brogan, M.; Carrigan, T.A.; Giddens, D.P. Heart rate variability analysis in full-term infants: Spectral indices for study of neonatal cardiorespiratory control. Pediatr. Res. 1989, 26, 188–195. [Google Scholar] [CrossRef]
- Beckers, F.; Verheyden, B.; Aubert, A.E. Aging and nonlinear heart rate control in a healthy population. Am. J. Physiol. Heart Circ. Physiol. 2006, 290, H2560–H2570. [Google Scholar] [CrossRef]
- Bilan, A.; Witczak, A.; Palusiński, R.; Myśliński, W.; Hanzlik, J. Circadian rhythm of spectral indices of heart rate variability in healthy subjects. J. Electrocardiol. 2005, 38, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Bonnemeier, H.; Wiegand, U.K.; Brandes, A.; Kluge, N.; Katus, H.A.; Richardt, G.; Potratz, J. Circadian profile of cardiac autonomic nervous modulation in healthy subjects: Differing effects of aging and gender on heart rate variability. J. Cardiovasc. Electrophysiol. 2003, 14, 791–799. [Google Scholar] [CrossRef] [PubMed]
- Brinth, L.S.; Jørgensen, T.; Mehlsen, J.; Petersen, M.W.; Gormsen, L.; Linneberg, A.; Fink, P.; Benros, M.E.; Dantoft, T.M. Normative values of short-term heart rate variability in a cross-sectional study of a Danish population. The DanFunD study. Scand. J. Public Health 2022, 52, 48–57. [Google Scholar] [CrossRef]
- Christensen, M.M.; Hansen, C.S.; Fleischer, J.; Vistisen, D.; Byberg, S.; Larsen, T.; Laursen, J.C.; Jorgensen, M.E. Normative data on cardiovascular autonomic function in Greenlandic Inuit. BMJ Open Diabetes Res. Care 2021, 9, e002121. [Google Scholar] [CrossRef]
- Dantas, E.M.; Kemp, A.H.; Andreao, R.V.; Da Silva, V.J.; Brunoni, A.R.; Hoshi, R.A.; Bensenor, I.M.; Lotufo, P.A.; Ribeiro, A.L.; Mill, J.G. Reference values for short-term resting-state heart rate variability in healthy adults: Results from the Brazilian Longitudinal Study of Adult HealthELSA-Brasil study. Psychophysiology 2018, 55, e13052. [Google Scholar] [CrossRef]
- Dietrich, D.F.; Schindler, C.; Schwartz, J.; Barthelemy, J.C.; Tschopp, J.M.; Roche, F.; von Eckardstein, A.; Brandli, O.; Leuenberger, P.; Gold, D.R.; et al. Heart rate variability in an ageing population and its association with lifestyle and cardiovascular risk factors: Results of the SAPALDIA study. EP Eur. 2006, 8, 521–529. [Google Scholar] [CrossRef]
- Ergun, U.; Demirci, M.; Nurlu, G.; Komurcu, F. Power spectral analysis of heart rate variability: Normal values of subjects over 60 years old. Int. J. Neurosci. 2008, 118, 1165–1173. [Google Scholar] [CrossRef] [PubMed]
- Farah, B.Q.; Barros, M.V.; Balagopal, B.; Ritti-Dias, R.M. Heart Rate Variability and Cardiovascular Risk Factors in Adolescent Boys. J. Pediatr. 2014, 165, 945–950. [Google Scholar] [CrossRef]
- Faulkner, M.S.; Hathaway, D.; Tolley, B. Cardiovascular autonomic function in healthy adolescents. Heart Lung 2003, 32, 10–22. [Google Scholar] [CrossRef]
- Finley, J.P.; Nugent, S.T. Heart rate variability in infants, children and young adults. J. Auton. Nerv. Syst. 1995, 51, 103–108. [Google Scholar] [CrossRef]
- Gasior, J.S.; Sacha, J.; Pawlowski, M.; Zielinski, J.; Jelen, P.J.; Tomik, A.; Ksiazczyk, T.M.; Werner, B.; Dabrowski, M.J. Normative Values for Heart Rate Variability Parameters in School-Aged Children: Simple Approach Considering Differences in Average Heart Rate. Front. Physiol. 2018, 9, 1495. [Google Scholar] [CrossRef]
- Geovanini, G.R.; Vasques, E.R.; Alvim, R.D.; Mill, J.G.; Andreao, R.V.; Vasques, B.K.; Pereira, A.C.; Krieger, J.E. Age and Sex Differences in Heart Rate Variability and Vagal Specific Patterns—Baependi Heart Study. Glob. Heart 2020, 15, 71. [Google Scholar] [CrossRef] [PubMed]
- Gerritsen, J.; TenVoorde, B.J.; Dekker, J.M.; Kingma, R.; Kostense, P.J.; Bouter, L.M.; Heethaar, R.M. Measures of cardiovascular autonomic nervous function: Agreement, reproducibility, and reference values in middle age and elderly subjects. Diabetologia 2003, 46, 330–338. [Google Scholar] [CrossRef]
- Goto, M.; Nagashima, M.; Baba, R.; Nagano, Y.; Yokota, M.; Nishibata, K.; Tsuji, A. Analysis of heart rate variability demonstrates effects of development on vagal modulation of heart rate in healthy children. J. Pediatr. 1997, 130, 725–729. [Google Scholar] [CrossRef]
- Harteveld, L.M.; Nederend, I.; Harkel, A.D.J.T.; Schutte, N.M.; de Rooij, S.R.; Vrijkotte, T.G.; Oldenhof, H.; Popma, A.; Jansen, L.M.; Suurland, J.; et al. Maturation of the Cardiac Autonomic Nervous System Activity in Children and Adolescents. J. Am. Heart Assoc. 2021, 10, e017405. [Google Scholar] [CrossRef]
- Irshad, M.; Bugti, S.; Bugti, H. Variation in Heart Rate Among Healthy Individuals. Indo Am. J. Pharm. Sci. 2018, 5, 11958–11962. [Google Scholar] [CrossRef]
- Jarrin, D.C.; McGrath, J.J.; Poirier, P.; Seguin, L.; Tremblay, R.E.; Montplaisir, J.Y.; Paradis, G.; Seguin, J.R. Short-Term Heart Rate Variability in a Population-Based Sample of 10-Year-Old Children. Pediatr. Cardiol. 2015, 36, 41–48. [Google Scholar] [CrossRef]
- Jensen-Urstad, K.; Storck, N.; Bouvier, F.; Ericson, M.; Lindblad, L.E.; Jensen-Urstad, M. Heart rate variability in healthy subjects is related to age and gender. Acta Physiol. Scand. 1997, 160, 235–241. [Google Scholar] [CrossRef]
- Kobayashi, H.; Park, B.J.; Miyazaki, Y. Normative references of heart rate variability and salivary alpha-amylase in a healthy young male population. J. Physiol. Anthropol. 2012, 31, 9. [Google Scholar] [CrossRef]
- Koskinen, T.; Kahonen, M.; Jula, A.; Laitinen, T.; Keltikangas-Jarvinen, L.K.; Viikari, J.; Valimaki, I.; Raitakari, O.T. Short-term heart rate variability in healthy young adults The Cardiovascular Risk in Young Finns Study. Auton. Neurosci. Basic Clin. 2009, 145, 81–88. [Google Scholar] [CrossRef]
- Latorre-Roman, P.A.; Martinez-Redondo, M.; Salas-Sanchez, J.; Consuegra-Gonzalez, P.J.; Sarabia-Cachadina, E.; Aragon-Vela, J.; Parraga-Montilla, J.A. Cardiac Evaluation of Exercise Testing in a Contemporary Population of Preschool Children: A New Approach Providing Reference Values. Children 2022, 9, 654. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Lee, J.H.; Son, J.W.; Kim, U.; Park, J.S.; Lee, J.; Shin, D.G. Normative Values of Short-Term Heart Rate Variability Parameters in Koreans and Their Clinical Value for the Prediction of Mortality. Heart Lung Circ. 2018, 27, 576–587. [Google Scholar] [CrossRef] [PubMed]
- Longin, E.; Schaible, T.; Lenz, T.; Konig, S. Short term heart rate variability in healthy neonates: Normative data and physiological observations. Early Hum. Dev. 2005, 81, 663–671. [Google Scholar] [CrossRef]
- Longin, E.; Dimitriadis, C.; Shazi, S.; Gerstner, T.; Lenz, T.; Konig, S. Autonomic Nervous System Function in Infants and Adolescents: Impact of Autonomic Tests on Heart Rate Variability. Pediatr. Cardiol. 2009, 30, 311–324. [Google Scholar] [CrossRef]
- Massin, M.; von Bernuth, G. Normal ranges of heart rate variability during infancy and childhood. Pediatr. Cardiol. 1997, 18, 297–302. [Google Scholar] [CrossRef]
- Massin, M.M.; Withofs, N.; Maeyns, K.; Ravet, F.; Gerard, P. Normal ranges for the variability in heart rate in young infants while sleeping. Cardiol. Young 2001, 11, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.K.; Super, D.M.; Connuck, D.; Salvator, A.; Singer, L.; Fradley, L.G.; Harcar-Sevcik, R.A.; Kirchner, H.L.; Kaufman, E.S. Heart rate variability in healthy newborn infants. Am. J. Cardiol. 2002, 89, 50–53. [Google Scholar] [CrossRef]
- Michels, N.; Clays, E.; De Buyzere, M.; Huybrechts, I.; Marild, S.; Vanaelst, B.; De Henauw, S.; Sioen, I. Determinants and reference values of short-term heart rate variability in children. Eur. J. Appl. Physiol. 2013, 113, 1477–1488. [Google Scholar] [CrossRef] [PubMed]
- O’Neal, W.T.; Chen, L.Y.; Nazarian, S.; Soliman, E.Z. Reference ranges for short-term heart rate variability measures in individuals free of cardiovascular disease: The Multi-Ethnic Study of Atherosclerosis (MESA). J. Electrocardiol. 2016, 49, 686–690. [Google Scholar] [CrossRef]
- Park, S.B.; Lee, B.C.; Jeong, K.S. Standardized tests of heart rate variability for autonomic function tests in healthy koreans. Int. J. Neurosci. 2007, 117, 1707–1717. [Google Scholar] [CrossRef]
- Patural, H.; Pichot, V.; Flori, S.; Giraud, A.; Franco, P.; Pladys, P.; Beuchee, A.; Roche, F.; Barthelemy, J.C. Autonomic maturation from birth to 2 years: Normative values. Heliyon 2019, 5, e01300. [Google Scholar] [CrossRef] [PubMed]
- Piccirillo, G.; Fimognari, F.L.; Viola, E.; Marigliano, V. Age-adjusted normal confidence intervals for heart rate variability in healthy subjects during head-up tilt. Int. J. Cardiol. 1995, 50, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Pikkujämsä, S.M.; Mäkikallio, T.H.; Juhani Airaksinen, K.E.; Huikuri, H.V. Determinants and interindividual variation of R-R interval dynamics in healthy middle-aged subjects. Am. J. Physiol. Heart Circ. Physiol. 2001, 280, H1400–H1406. [Google Scholar] [CrossRef]
- Ramaekers, D.; Ector, H.; Aubert, A.E.; Rubens, A.; Van de Werf, F. Heart rate variability and heart rate in healthy volunteers. Is the female autonomic nervous system cardioprotective? Eur. Heart J. 1998, 19, 1334–1341. [Google Scholar] [CrossRef]
- Saleem, S.; Hussain, M.M.; Majeed, S.M.; Khan, M.A. Gender differences of heart rate variability in healthy volunteers. J. Pak. Med. Assoc. 2012, 62, 422–425. [Google Scholar]
- Seppala, S.; Laitinen, T.; Tarvainen, M.P.; Tompuri, T.; Veijalainen, A.; Savonen, K.; Lakka, T. Normal values for heart rate variability parameters in children 6–8 years of age: The PANIC Study. Clin. Physiol. Funct. Imaging 2014, 34, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Silvetti, M.S.; Drago, F.; Ragonese, P. Heart rate variability in healthy children and adolescents is partially related to age and gender. Int. J. Cardiol. 2001, 81, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Sitovskyi, A.M.; Radchenko, O.V.; Dmytruk, V.S.; Andriichuk, O.Y.; Roda, O.B.; Savchuk, I.V. Heart Rate Variability in 12- to 13-Year-Old Adolescents. Neurophysiology 2020, 52, 279–288. [Google Scholar] [CrossRef]
- Sloan, R.P.; Huang, M.-H.; McCreath, H.; Sidney, S.; Liu, K.; Williams, O.D.; Seeman, T. Cardiac autonomic control and the effects of age, race, and sex: The CARDIA study. Auton. Neurosci. 2008, 139, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Sosnowski, M.; Macfarlane, P.W.; Czyz, Z.; Skrzypek-Wanha, J.; Boczkowska-Gaika, E.; Tendera, M. Age-adjustment of HRV measures and its prognostic value for risk assessment in patients late after myocardial infarction. Int. J. Cardiol. 2002, 86, 249–258. [Google Scholar] [CrossRef]
- Tegegne, B.S.; Man, T.F.; van Roon, A.M.; Snieder, H.; Riese, H. Reference values of heart rate variability from 10-second resting electrocardiograms: The Lifelines Cohort Study. Eur. J. Prev. Cardiol. 2020, 27, 2191–2194. [Google Scholar] [CrossRef]
- Tsuji, H.; Venditti, F.J.; Manders, E.S.; Evans, J.C.; Larson, M.G.; Feldman, C.L.; Levy, D. Determinants of heart rate variability. J. Am. Coll. Cardiol. 1996, 28, 1539–1546. [Google Scholar] [CrossRef]
- Umetani, K.; Singer, D.H.; McCraty, R.; Atkinson, M. Twenty-four hour time domain heart rate variability and heart rate: Relations to age and gender over nine decades. J. Am. Coll. Cardiol. 1998, 31, 593–601. [Google Scholar] [CrossRef]
- Ziegler, D.; Laux, G.; Dannehl, K.; Spuler, M.; Muhlen, H.; Mayer, P.; Gries, F.A. Assessment of cardiovascular autonomic function: Age-related normal ranges and reproducibility of spectral analysis, vector analysis, and standard tests of heart rate variation and blood pressure responses. Diabet. Med. 1992, 9, 166–175. [Google Scholar] [CrossRef]
- Ziegler, D.; Piolot, R.; Strassburger, K.; Lambeck, H.; Dannehl, K. Normal ranges and reproducibility of statistical, geometric, frequency domain, and non-linear measures of 24-hour heart rate variability. Horm. Metab. Res. 1999, 31, 672–679. [Google Scholar] [CrossRef]
- Otsuka, K.; Cornelissen, G.; Shinagawa, M.; Nishimura, Y.; Kubo, Y.; Hotta, N.; Fujii, C.; Ishii, T.; Omori, K.; Watanabe, Y.; et al. Circadian Reference Values for Different Endpoints of Heart Rate Variability. In Proceedings of the Computers in Cardiology 1999. Vol. 26 (Cat. No.99CH37004), Hannover, Germany, 26–29 September 1999; pp. 587–590, ISBN 0-7803-5614-4. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Sammito, S.; Sammito, W.; Böckelmann, I. The circadian rhythm of heart rate variability: A systematic review of the literature. Biol. Rhythm Res. 2016, 47, 717–730. [Google Scholar] [CrossRef]
- Dinas, P.C.; Koutedakis, Y.; Flouris, A.D. Effects of active and passive tobacco cigarette smoking on heart rate variability. Int. J. Cardiol. 2013, 163, 109–115. [Google Scholar] [CrossRef]
- Karpyak, V.M.; Romanowicz, M.; Schmidt, J.E.; Lewis, K.A.; Bostwick, J.M. Characteristics of heart rate variability in alcohol-dependent subjects and nondependent chronic alcohol users. Alcohol. Clin. Exp. Res. 2014, 38, 9–26. [Google Scholar] [CrossRef] [PubMed]
- Sandercock, G.R.H.; Bromley, P.D.; Brodie, D.A. Effects of exercise on heart rate variability: Inferences from meta-analysis. Med. Sci. Sports Exerc. 2005, 37, 433–439. [Google Scholar] [CrossRef]
- Carrasco-Poyatos, M.; González-Quílez, A.; Altini, M.; Granero-Gallegos, A. Heart rate variability-guided training in professional runners: Effects on performance and vagal modulation. Physiol. Behav. 2022, 244, 113654. [Google Scholar] [CrossRef]
- Mendes, J.; Pereira, J.; Pereira, T. Variability of Heart Rate in Athletes and Non Athletes. Eur. J. Public Health 2019, 29, ckz034-098. [Google Scholar] [CrossRef]
| Study | Group | n | Mean ± SD |
|---|---|---|---|
| Agelink et al., 2001 [23] | Male, 17–25 years | 58 | 1.65 ± 0.32 |
| Female, 17–25 years | 1.58 ± 0.32 | ||
| Male, 26–35 years | 123 | 1.58 ± 0.22 | |
| Female, 26–35 years | 1.54 ± 0.30 | ||
| Male, 36–45 years | 47 | 1.45 ± 0.30 | |
| Female, 36–45 years | 1.35 ± 0.23 | ||
| Male, 46–55 years | 42 | 1.31 ± 0.21 | |
| Female, 46–55 years | 1.28 ± 0.22 | ||
| Male, 55+ years | 39 | 1.25 ± 0.21 | |
| Female, 55+ years | 1.33 ± 0.27 | ||
| Dantas et al., 2018 [30] | 35–44 years | 982 | 34.9 ± 17.5 |
| 45–55 years | 1252 | 30.0 ± 15.6 | |
| 55–64 years | 536 | 26.7 ± 15.3 | |
| 65–75 years | 104 | 27.7 ± 23.6 | |
| Kim et al., 2011 [8] | 3408 | 29.7 ± 18.1 | |
| Park et al., 2007 [55] | 637 | 27.3 ± 15.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brozat, M.; Böckelmann, I.; Sammito, S. Systematic Review on HRV Reference Values. J. Cardiovasc. Dev. Dis. 2025, 12, 214. https://doi.org/10.3390/jcdd12060214
Brozat M, Böckelmann I, Sammito S. Systematic Review on HRV Reference Values. Journal of Cardiovascular Development and Disease. 2025; 12(6):214. https://doi.org/10.3390/jcdd12060214
Chicago/Turabian StyleBrozat, Maximillian, Irina Böckelmann, and Stefan Sammito. 2025. "Systematic Review on HRV Reference Values" Journal of Cardiovascular Development and Disease 12, no. 6: 214. https://doi.org/10.3390/jcdd12060214
APA StyleBrozat, M., Böckelmann, I., & Sammito, S. (2025). Systematic Review on HRV Reference Values. Journal of Cardiovascular Development and Disease, 12(6), 214. https://doi.org/10.3390/jcdd12060214





