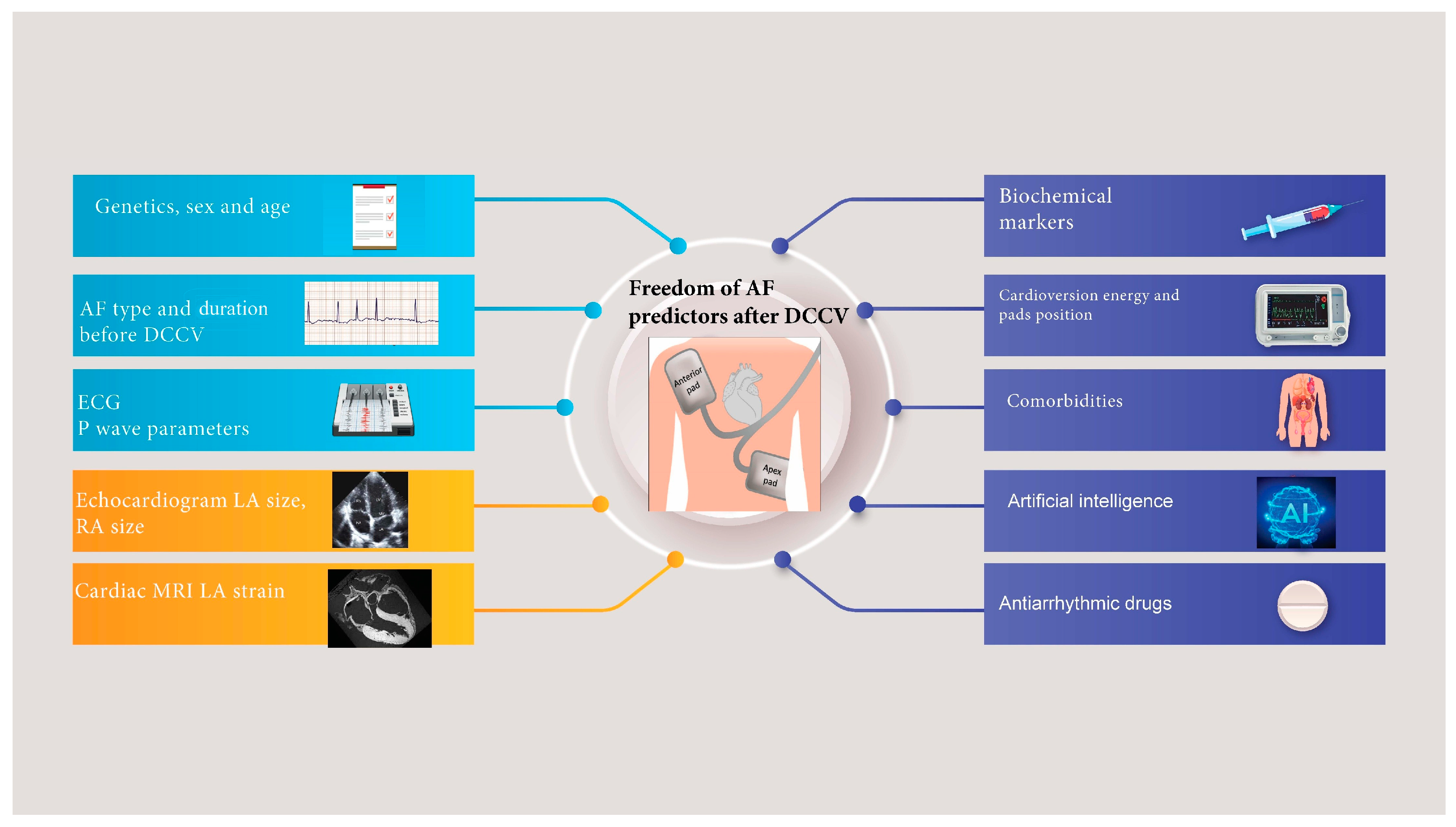
Predicting the Outcomes of External Direct Current Cardioversion for Atrial Fibrillation: A Narrative Review of Current Evidence
Abstract
1. Introduction
1.1. Technical Predictors
1.2. Antiarrhythmic Drugs Use
- Flecainide and Propafenone: Both medications are classified as class IC antiarrhythmics and are known for their efficacy in converting AF to sinus rhythm, particularly in patients with paroxysmal AF. The effectiveness of these agents is comparable, with studies indicating that both flecainide and propafenone can achieve similar conversion rates to SR following DCCV [21]. Furthermore, flecainide is often recommended in clinical guidelines for early pharmacologic cardioversion due to its rapid onset of action and favourable safety profile in selected patients [22]. In addition to their efficacy in restoring sinus rhythm, flecainide and propafenone may influence long-term outcomes following DCCV. Research indicates that early rhythm control strategies, including administering these antiarrhythmics, can reduce the risk of AF recurrence and improve overall cardiovascular outcomes [23]. For instance, a systematic review highlighted that early pharmacologic cardioversion with agents like flecainide not only facilitates immediate conversion but may also serve as a bridge to longer-term rhythm control strategies [23,24].
- 2.
- Amiodarone is a widely utilised antiarrhythmic medication particularly in AF, where it is often administered to improve outcomes following DCCV. The efficacy of amiodarone in facilitating successful conversion from AF to SR has been documented in various studies, highlighting its role as a first-line agent in this setting. Research indicates that amiodarone can significantly enhance the success rate of electrical cardioversion according to a meta-analysis [27]. In addition to its efficacy, amiodarone’s pharmacological properties contribute to its effectiveness in this context. It acts by blocking sodium, calcium, and potassium channels and exhibiting beta-blocking effects, which help stabilise cardiac rhythm and facilitate successful cardioversion [28]. Combining electrical cardioversion with amiodarone administration has been shown to reduce the risk of immediate recurrence of AF following the procedure, thereby improving overall patient outcomes [29]. However, the use of amiodarone is not without concerns. While it is effective, there are potential risks associated with its administration, including the development of torsades de pointes, particularly in patients with underlying heart conditions [30]. Moreover, some studies have indicated that the pre-treatment with amiodarone does not always yield statistically significant improvements in cardioversion success rates compared to those who do not receive the drug, suggesting that its benefits may vary among different patient populations [31].
- 3.
- Sotalol: Another class III antiarrhythmic agent commonly used in AF care pre-DCCV. In a systematic review and meta-analysis, sotalol demonstrated significant efficacy in the pharmacologic conversion of AF, with a higher rate of successful cardioversion than placebo [32]. Specifically, one study reported that sotalol had a cardioversion rate of 68% in rhythm control groups, significantly higher than the 42% observed in rate control groups [33]. This highlights Sotalol’s potential as a first-line agent for rhythm control in patients undergoing DCCV. Furthermore, intravenous sotalol has been explored as a rapid loading strategy, which may enhance the speed of achieving therapeutic levels and improve patient outcomes [34,35]. However, the safety profile of sotalol must be considered, particularly regarding its association with QT interval prolongation and the risk of TdP [36,37]. The American Heart Association (AHA) guidelines recommend careful monitoring of patients receiving sotalol, especially those with pre-existing conditions such as heart failure or renal impairment [38]. Despite these concerns, when used appropriately, sotalol has shown to be a safe and effective option for maintaining SR after DCCV, with studies indicating that the risk of adverse effects can be managed through careful patient selection and monitoring protocols [33,36].
1.3. Patient Factors (Demographics and Clinical Parameters)
1.4. Biochemical Markers
1.5. Genetic Predisposition
1.6. Cardiovascular Imaging
1.7. Electrocardiogram Markers
2. The Role of Artificial Intelligence
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lippi, G.; Sanchis-Gomar, F.; Cervellin, G. Global epidemiology of atrial fibrillation: An increasing epidemic and public health challenge. Int. J. Stroke 2021, 16, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Antoun, I.; Alkhayer, A.; Aljabal, M.; Mahfoud, Y.; Alkhayer, A.; Simon, P.; Kotb, A.; Barker, J.; Mavilakandy, A.; Hani, R.; et al. Thirty-Day Unplanned Readmissions Following Hospitalization for Atrial Fibrillation in a Tertiary Syrian Centre: A Real-World Observational Cohort Study. Heart Rhythm O2 2024, 5, 854–859. [Google Scholar] [CrossRef]
- Antoun, I.; Alkhayer, A.; Aljabal, M.; Mahfoud, Y.; Alkhayer, A.; Kotb, A.I.; Barker, J.; Somani, R.; Ng, G.A.; Zakkar, M. Incidence, outcomes, and predictors of new heart failure in syrian conflict-affected population following hospitalization for atrial fibrillation: A retrospective cohort study. Perfusion 2024. Online ahead of print. [Google Scholar] [CrossRef]
- Antoun, I.; Aljabal, M.; Alkhayer, A.; Mahfoud, Y.; Alkhayer, A.; Simon, P.; Kotb, A.; Barker, J.; Mavilakandy, A.; Naseer, M.U.; et al. Atrial fibrillation inpatient management patterns and clinical outcomes during the conflict in Syria: An observational cohort study. Perfusion 2024, 40, 711–719. [Google Scholar] [CrossRef] [PubMed]
- Van Gelder, I.C.; Rienstra, M.; Bunting, K.V.; Casado-Arroyo, R.; Caso, V.; Crijns, H.J.G.M.; De Potter, T.J.R.; Dwight, J.; Guasti, L.; Hanke, T.; et al. 2024 ESC Guidelines for the management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): Developed by the task force for the management of atrial fibrillation of the European Society of Cardiology (ESC), with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Endorsed by the European Stroke Organisation (ESO). Eur. Heart J. 2024, 45, 3314–3414. [Google Scholar] [CrossRef]
- Raniga, D.; Goda, M.; Hattingh, L.; Thorning, S.; Rowe, M.; Howes, L. Left atrial volume index: A predictor of atrial fibrillation recurrence following direct current cardioversion—A systematic review and meta-analysis. Int. J. Cardiol. Heart Vasc. 2024, 51, 101364. [Google Scholar] [CrossRef]
- Antoun, I.; Li, X.; Kotb, A.; Barker, J.; Mavilakandy, A.; Koev, I.; Vali, Z.; Somani, R.; Ng, G.A. Body surface mapping of P-waves in sinus rhythm to predict recurrence following cardioversion for atrial fibrillation. Front. Cardiovasc. Med. 2024, 11, 1417029. [Google Scholar] [CrossRef] [PubMed]
- Maqsood, N.; Cooper, J.M.; Whitman, I.R. Letter by Maqsood Et Al Regarding Article, “Anterior–Lateral Versus Anterior–Posterior Electrode Position for Cardioverting Atrial Fibrillation”. Circulation 2022, 145, 21. [Google Scholar] [CrossRef]
- Schmidt, A.S.; Lauridsen, K.G.; Møller, D.S.; Christensen, P.D.; Dodt, K.K.; Rickers, H.; Løfgren, B.; Albertsen, A.E. Anterior–Lateral Versus Anterior–Posterior Electrode Position for Cardioverting Atrial Fibrillation. Circulation 2021, 144, 1995–2003. [Google Scholar] [CrossRef]
- Kirchhof, P.; Eckardt, L.; Loh, P.; Weber, K.; Fischer, R.-J.; Seidl, K.-H.; Böcker, D.; Breithardt, G.; Haverkamp, W.; Borggrefe, M. Anterior-posterior versus anterior-lateral electrode positions for external cardioversion of atrial fibrillation: A randomised trial. Lancet 2002, 360, 1275–1279. [Google Scholar] [CrossRef]
- Kirkland, S.; Stiell, I.; AlShawabkeh, T.; Campbell, S.; Dickinson, G.; Rowe, B.H. The efficacy of pad placement for electrical cardioversion of atrial fibrillation/flutter: A systematic review. Acad. Emerg. Med. 2014, 21, 717–726. [Google Scholar] [CrossRef]
- Stiell, I.G.; Sivilotti, M.L.; Taljaard, M.; Birnie, D.; Vadeboncoeur, A.; Hohl, C.M.; McRae, A.D.; Rowe, B.H.; Brison, R.J.; Thiruganasambandamoorthy, V.; et al. Electrical versus pharmacological cardioversion for emergency department patients with acute atrial fibrillation (RAFF2): A partial factorial randomised trial. Lancet 2020, 395, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, S.T.; Belley-Côté, E.P.; Ibrahim, O.; Um, K.J.; Lengyel, A.; Adli, T.; Qiu, Y.; Wong, M.M.; Sibilio, S.; Benz, A.P.; et al. Techniques Improving Electrical Cardioversion Success for Patients with Atrial Fibrillation: A Systematic Review and Meta-Analysis. EP Eur. 2022, 25, 318–330. [Google Scholar] [CrossRef]
- Jacobs, V.; May, H.T.; Bair, T.L.; Crandall, B.G.; Cutler, M.J.; Day, J.D.; Le, V.; Mallender, C.; Osborn, J.S.; Weiss, J.P. The Impact of Repeated Cardioversions for Atrial Fibrillation on Stroke, Hospitalizations, and Catheter Ablation Outcomes. J. Atr. Fibrillation 2019, 11, 2164. [Google Scholar] [PubMed]
- Schmidt, A.S.; Lauridsen, K.G.; Torp, P.; Bach, L.F.; Rickers, H.; Løfgren, B. Maximum-Fixed Energy Shocks for Cardioverting Atrial Fibrillation. Eur. Heart J. 2019, 41, 626–631. [Google Scholar] [CrossRef] [PubMed]
- Khalighi, K.; Talebian, A.; Toor, R.; Mirabbasi, S.A. Successful External Cardioversion via Fluoroscopic Electrode Positioning in Patients With Enlarged Trans-Thoracic Diameter. Am. J. Case Rep. 2018, 19, 171–175. [Google Scholar] [CrossRef]
- Kirchhof, P.; Mönnig, G.; Wasmer, K.; Heinecke, A.; Breithardt, G.; Eckardt, L.; Böcker, D. A trial of self-adhesive patch electrodes and hand-held paddle electrodes for external cardioversion of atrial fibrillation (MOBIPAPA). Eur. Heart J. 2005, 26, 1292–1297. [Google Scholar] [CrossRef]
- Voskoboinik, A.; Moskovitch, J.; Plunkett, G.; Bloom, J.; Wong, G.; Nalliah, C.; Prabhu, S.; Sugumar, H.; Paramasweran, R.; McLellan, A.; et al. Cardioversion of Atrial Fibrillation in Obese Patients: Results From the Cardioversion-BMI Randomized Controlled Trial. J. Cardiovasc. Electrophysiol. 2018, 30, 155–161. [Google Scholar] [CrossRef]
- Fetsch, T.; Bauer, P.; Engberding, R.; Koch, H.P.; Lukl, J.; Meinertz, T.; Oeff, M.; Seipel, L.; Trappe, H.J.; Treese, N. Prevention of atrial fibrillation after cardioversion: Results of the PAFAC trial. Eur. Heart J. 2004, 25, 1385–1394. [Google Scholar] [CrossRef]
- Lafuente-Lafuente, C.; Valembois, L.; Bergmann, J.F.; Belmin, J. Antiarrhythmics for maintaining sinus rhythm after cardioversion of atrial fibrillation. Cochrane Database Syst. Rev. 2015, 3, CD005049. [Google Scholar] [CrossRef]
- Tracevskis, M. Effectiveness of Amiodarone, Propafenone and Synchronized Electrical Cardioversion for Conversion of Atrial Fibrillation Paroxysm to Sinus Rhythm in Rigas Stradins University Hospital Department of Emergency Medicine. Clin. Med. Health Res. J. 2023, 3, 485–488. [Google Scholar] [CrossRef]
- Aliot, E.; Capucci, A.; Crijns, H.J.; Goette, A.; Tamargo, J. Twenty-five years in the making: Flecainide is safe and effective for the management of atrial fibrillation. EP Eur. 2010, 13, 161–173. [Google Scholar] [CrossRef] [PubMed]
- deSouza, I.S.; Tadrous, M.; Sexton, T.; Benabbas, R.; Carmelli, G.; Sinert, R. Pharmacologic Cardioversion of Recent-Onset Atrial Fibrillation and Flutter in the Emergency Department: A Systematic Review and Network Meta-Analysis. Ann. Emerg. Med. 2020, 76, 14–30. [Google Scholar] [CrossRef]
- Castrichini, M.; Restivo, L.; Fabris, E.; Massa, L.; Di Meola, R.; Beltrame, D.; De Luca, A.; Korcova, R.; Milo, M.; Sinagra, G. Prevalence and predictors of persistent sinus rhythm after elective electrical cardioversion for atrial fibrillation. J. Cardiovasc. Med. 2021, 22, 626–630. [Google Scholar] [CrossRef] [PubMed]
- Coppola, G.; Manno, G.; Mignano, A.; Luparelli, M.; Zarcone, A.; Novo, G.; Corrado, E. Management of Direct Oral Anticoagulants in Patients With Atrial Fibrillation Undergoing Cardioversion. Medicina 2019, 55, 660. [Google Scholar] [CrossRef]
- Airaksinen, J. How to Optimize Cardioversion of Atrial Fibrillation. J. Clin. Med. 2022, 11, 3372. [Google Scholar] [CrossRef]
- Um, K.J.; McIntyre, W.F.; Healey, J.S.; Mendoza, P.A.; Koziarz, A.; Amit, G.; Chu, V.A.; Whitlock, R.P.; Belley-Côté, E.P. Pre- and post-treatment with amiodarone for elective electrical cardioversion of atrial fibrillation: A systematic review and meta-analysis. EP Eur. 2019, 21, 856–863. [Google Scholar] [CrossRef]
- Nattel, S.; Talajic, M.; Fermini, B.; Roy, D. Amiodarone: Pharmacology, clinical actions, and relationships between them. J. Cardiovasc. Electrophysiol. 1992, 3, 266–280. [Google Scholar] [CrossRef]
- Pye, E. Early Recognition With Capnography, and Successful Resuscitation, of Severe Cardiac Dysfunction in a Horse Receiving Amiodarone During Transvenous Electric Cardioversion (TVEC). Equine Vet. Educ. 2023, 36, e113–e120. [Google Scholar] [CrossRef]
- Nordkin, I.; Levinas, T.; Rosenfeld, I.; Halabi, M. Torsades De Pointes After Prolonged Intravenous Amiodarone Therapy for Atrial Fibrillation. Clin. Case Rep. 2020, 9, 391–394. [Google Scholar] [CrossRef]
- Seo, J.; Singh, M.K. Electrical Cardioversion in a Dog With Atrial Fibrillation and Hypothyroidism. Vet. Rec. Case Rep. 2018, 6, e000583. [Google Scholar] [CrossRef]
- Milan, D.J.; Saul, J.P.; Somberg, J.C.; Molnar, J. Efficacy of Intravenous and Oral Sotalol in Pharmacologic Conversion of Atrial Fibrillation: A Systematic Review and Meta-Analysis. Cardiology 2016, 136, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Sawh, C.; Rashid, S. The Safety and Efficacy of Sotalol in the Management of Acute Atrial Fibrillation: A Retrospective Case Control Study. Interv. Cardiol. 2016, 8, 637–642. [Google Scholar] [CrossRef]
- Lakkireddy, D.; Ahmed, A.; Atkins, D.; Bawa, D.; Garg, J.; Bush, J.; Charate, R.; Bommana, S.; Pothineni, N.V.K.; Kabra, R.; et al. Feasibility and Safety of Intravenous Sotalol Loading in Adult Patients With Atrial Fibrillation (DASH-AF). Jacc Clin. Electrophysiol. 2023, 9, 555–564. [Google Scholar] [CrossRef] [PubMed]
- Feuerborn, M.L.; Dechand, J.; Vadlamudi, R.S.; Torre, M.; Freedman, R.A.; Groh, C.A.; Navaravong, L.; Ranjan, R.; Varela, D.; Bunch, T.J.; et al. Protocol Development and Initial Experience With Intravenous Sotalol Loading for Atrial Arrhythmias. Crit. Pathw. Cardiol. A J. Evid.-Based Med. 2022, 22, 1–4. [Google Scholar] [CrossRef]
- Mascarenhas, D.; Mudumbi, P.C.; Kantharia, B.K. Outpatient Initiation of Sotalol in Patients With Atrial Fibrillation: Utility of Cardiac Implantable Electronic Devices for Therapy Monitoring. Am. J. Cardiovasc. Drugs 2021, 21, 693–700. [Google Scholar] [CrossRef]
- Rabatin, A.; Mj, S.; Jm, B.; Houmsse, M. Safety of Twice Daily Sotalol in Patients With Renal Impairment: A Single Center, Retrospective Review. J. Atr. Fibrillation 2018, 11, 2047. [Google Scholar] [CrossRef]
- Singh, J.P.; Blomström-Lundqvist, C.; Turakhia, M.P.; Fazeli, M.S.; Kreidieh, B.; Crotty, C.P.; Kowey, P.R. Dronedarone Versus Sotalol in Patients With Atrial Fibrillation: A Systematic Literature Review and Network Meta-analysis. Clin. Cardiol. 2023, 46, 589–597. [Google Scholar] [CrossRef]
- Charitakis, E.; Dragioti, E.; Stratinaki, M.; Korela, D.; Tzeis, S.; Almroth, H.; Liuba, I.; Jönsson, A.H.; Charalambous, G.; Karlsson, L.O.; et al. Predictors of recurrence after catheter ablation and electrical cardioversion of atrial fibrillation: An umbrella review of meta-analyses. EP Eur. 2023, 25, 40–48. [Google Scholar] [CrossRef]
- Curtis, A.B.; Karki, R.; Hattoum, A.; Sharma, U.C. Arrhythmias in patients ≥80 years of age: Pathophysiology, management, and outcomes. J. Am. Coll. Cardiol. 2018, 71, 2041–2057. [Google Scholar] [CrossRef]
- Frick, M.; Frykman, V.; Jensen-Urstad, M.; Östergren, J. Factors predicting success rate and recurrence of atrial fibrillation after first electrical cardioversion in patients with persistent atrial fibrillation. Clin. Cardiol. 2001, 24, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Brodsky, M.A.; Allen, B.J.; Capparelli, E.V.; Luckett, C.R.; Morton, R.; Henry, W.L. Factors determining maintenance of sinus rhythm after chronic atrial fibrillation with left atrial dilatation. Am. J. Cardiol. 1989, 63, 1065–1068. [Google Scholar] [CrossRef]
- Westerman, S.; Wenger, N. Gender differences in atrial fibrillation: A review of epidemiology, management, and outcomes. Curr. Cardiol. Rev. 2019, 15, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Suttorp, M.J.; Kingma, J.H.; Koomen, E.M.; van’t Hof, A.; Tijssen, J.G.; Lie, K.I. Recurrence of paroxysmal atrial fibrillation or flutter after successful cardioversion in patients with normal left ventricular function. Am. J. Cardiol. 1993, 71, 710–713. [Google Scholar] [CrossRef] [PubMed]
- Alt, E.; Ammer, R.; Lehmann, G.; Pütter, K.; Ayers, G.M.; Pasquantonio, J.; Schömig, A. Patient characteristics and underlying heart disease as predictors of recurrent atrial fibrillation after internal and external cardioversion in patients treated with oral sotalol. Am. Heart. J. 1997, 134, 419–425. [Google Scholar] [CrossRef]
- van den Berg, M.P.; Tuinenburg, A.E.; van Veldhuisen, D.J.; de Kam, P.J.; Crijns, H.J.G.M. Cardioversion of atrial fibrillation in the setting of mild to moderate heart failure. Int. J. Cardiol. 1998, 63, 63–70. [Google Scholar] [CrossRef]
- Caputo, M.; Urselli, R.; Capati, E.; Navarri, R.; Sinesi, L.; Furiozzi, F.; Ballo, P.; Palazzuoli, A.; Favilli, R.; Mondillo, S. Usefulness of left ventricular diastolic dysfunction assessed by pulsed tissue Doppler imaging as a predictor of atrial fibrillation recurrence after successful electrical cardioversion. Am. J. Cardiol. 2011, 108, 698–704. [Google Scholar] [CrossRef]
- Melduni, R.M.; Cullen, M.W. Role of left ventricular diastolic dysfunction in predicting atrial fibrillation recurrence after successful electrical cardioversion. J. Atr. Fibrillation 2012, 5, 654. [Google Scholar]
- Soran, H.; Younis, N.; Currie, P.; Silas, J.; Jones, I.; Gill, G. Influence of diabetes on the maintenance of sinus rhythm after a successful direct current cardioversion in patients with atrial fibrillation. Q.J.M. 2008, 101, 181–187. [Google Scholar] [CrossRef]
- Kanagala, R.; Murali, N.S.; Friedman, P.A.; Ammash, N.M.; Gersh, B.J.; Ballman, K.V.; Shamsuzzaman, A.S.; Somers, V.K. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation 2003, 107, 2589–2594. [Google Scholar] [CrossRef]
- Schmidt, M.; Daccarett, M.; Rittger, H.; Marschang, H.; Holzmann, S.; Jung, P.; Bojanic, D.; Ketteler, M.; Brachmann, J.; Rieber, J. Renal dysfunction and atrial fibrillation recurrence following cardioversion. J. Cardiovasc. Electrophysiol. 2011, 22, 1092–1098. [Google Scholar] [CrossRef] [PubMed]
- Pisters, R.; Nieuwlaat, R.; Prins, M.H.; Le Heuzey, J.-Y.; Maggioni, A.P.; Camm, A.J.; Crijns, H.J.G.M.; Euro Heart Survey Investigators. Clinical correlates of immediate success and outcome at 1-year follow-up of real-world cardioversion of atrial fibrillation: The Euro Heart Survey. Europace 2012, 14, 666–674. [Google Scholar] [CrossRef] [PubMed]
- Kostopoulos, G.; Effraimidis, G. Epidemiology, prognosis, and challenges in the management of hyperthyroidism-related atrial fibrillation. Eur. Thyroid. J. 2024, 13, e230254. [Google Scholar] [CrossRef]
- Siu, C.-W.; Jim, M.-H.; Zhang, X.; Chan, Y.-H.; Pong, V.; Kwok, J.; Kung, A.W.; Lau, C.-P.; Tse, H.-F. Comparison of atrial fibrillation recurrence rates after successful electrical cardioversion in patients with hyperthyroidism-induced versus non-hyperthyroidism-induced persistent atrial fibrillation. Am. J. Cardiol. 2009, 103, 540–543. [Google Scholar] [CrossRef] [PubMed]
- Koleck, T.A.; Mitha, S.A.; Biviano, A.; Caceres, B.A.; Corwin, E.J.; Goldenthal, I.; Creber, R.M.; Turchioe, M.R.; Hickey, K.T.; Bakken, S. Exploring depressive symptoms and anxiety among patients with atrial fibrillation and/or flutter at the time of cardioversion or ablation. J. Cardiovasc. Nurs. 2021, 36, 470–481. [Google Scholar] [CrossRef]
- Mlynarska, A.; Mlynarski, R.; Marcisz, C.; Golba, K.S. Modified frailty as a novel factor in predicting the maintenance of the sinus rhythm after electrical cardioversion of atrial fibrillation in the elderly population. Clin. Interv. Aging 2020, 15, 1193–1199. [Google Scholar] [CrossRef]
- Lange, H.W.; Herrmann-Lingen, C. Depressive symptoms predict recurrence of atrial fibrillation after cardioversion. J. Psychosom. Res. 2007, 63, 509–513. [Google Scholar] [CrossRef]
- García-Izquierdo, E.; Fajardo-Simón, L.; Cruz-Utrilla, A.; Aguilera-Agudo, C.; Jiménez-Sánchez, D.; Sánchez-García, M.; Lobo, A.B.; Escudier-Villa, J.M.; Ortega-Marcos, J.; Silva-Melchor, L. The role of anxiety in patients with persistent atrial fibrillation undergoing elective cardioversion: An observational study. Psychosom. Med. 2020, 82, 744–750. [Google Scholar] [CrossRef]
- Liu, T.; Li, G.; Li, L.; Korantzopoulos, P. Association between C-reactive protein and recurrence of atrial fibrillation after successful electrical cardioversion. J. Am. Coll. Cardiol. 2007, 49, 1642–1648. [Google Scholar] [CrossRef]
- Kawamura, M.; Munetsugu, Y.; Kawasaki, S.; Onishi, K.; Onuma, Y.; Kikuchi, M.; Tanno, K.; Kobayashi, Y. Type III procollagen-N-peptide as a predictor of persistent atrial fibrillation recurrence after cardioversion. EP Eur. 2012, 14, 1719–1725. [Google Scholar] [CrossRef]
- Gürses, K.M.; Yalçın, M.U.; Koçyiğit, D.; Canpınar, H.; Ateş, A.H.; Canpolat, U.; Yorgun, H.; Güç, D.; Aytemir, K. Serum galectin-3 level predicts early recurrence following successful direct-current cardioversion in persistent atrial fibrillation patients. Turk. Kardiyol. Dern. Ars. 2019, 47, 564–571. [Google Scholar] [PubMed]
- Siu, C.-W.; Watson, T.; Lai, W.-H.; Lee, Y.-K.; Chan, Y.-H.; Ng, K.-M.; Lau, C.-P.; Lip, G.Y.H.; Tse, H.-F. Relationship of circulating endothelial progenitor cells to the recurrence of atrial fibrillation after successful conversion and maintenance of sinus rhythm. EP Eur. 2009, 12, 517–521. [Google Scholar] [CrossRef]
- Zografos, T.; Maniotis, C.; Katsivas, A.; Katritsis, D. Relationship between brain natriuretic peptides and recurrence of atrial fibrillation after successful direct current cardioversion: A meta-analysis. Pacing Clin. Electrophysiol. 2014, 37, 1530–1537. [Google Scholar] [CrossRef] [PubMed]
- Rigopoulos, A.G.; Kalogeropoulos, A.S.; Tsoporis, J.N.; Sakadakis, E.A.; Triantafyllis, A.S.; Noutsias, M.; Gupta, S.; Parker, T.G.; Rizos, I. Heat shock protein 70 is associated with cardioversion outcome and recurrence of symptomatic recent onset atrial fibrillation in hypertensive patients. J. Cardiovasc. Pharmacol. 2021, 77, 3. [Google Scholar] [CrossRef]
- Wu, Y.; Kong, X.-J.; Ji, Y.-Y.; Fan, J.; Ji, C.-C.; Chen, X.-M.; Ma, Y.-D.; Tang, A.-L.; Cheng, Y.-J.; Wu, S.-H. Serum electrolyte concentrations and risk of atrial fibrillation: An observational and mendelian randomization study. BMC Genom. 2024, 25, 280. [Google Scholar] [CrossRef]
- Lu, Y.-Y.; Cheng, C.-C.; Chen, Y.-C.; Lin, Y.-K.; Chen, S.-A.; Chen, Y.-J. Electrolyte disturbances differentially regulate sinoatrial node and pulmonary vein electrical activity: A contribution to hypokalemia- or hyponatremia-induced atrial fibrillation. Heart Rhythm. 2016, 13, 781–788. [Google Scholar] [CrossRef] [PubMed]
- Parvez, B.; Shoemaker, M.B.; Muhammad, R.; Richardson, R.; Jiang, L.; Blair, M.A.; Roden, D.M.; Darbar, D. Common genetic polymorphism at 4q25 locus predicts atrial fibrillation recurrence after successful cardioversion. Heart Rhythm. 2013, 10, 849–855. [Google Scholar] [CrossRef]
- Shoemaker, M.B.; Bollmann, A.; Lubitz, S.A.; Ueberham, L.; Saini, H.; Montgomery, J.; Edwards, T.; Yoneda, Z.; Sinner, M.F.; Arya, A. Common genetic variants and response to atrial fibrillation ablation. Circ. Arrhythm. Electrophysiol. 2015, 8, 296–302. [Google Scholar] [CrossRef]
- Verhorst, P.M.; Kamp, O.; Welling, R.C.; Van Eenige, M.J.; Visser, C.A. Transesophageal echocardiographic predictors for maintenance of sinus rhythm after electrical cardioversion of atrial fibrillation. Am. J. Cardiol. 1997, 79, 1355–1359. [Google Scholar] [CrossRef]
- Kostakou, P.; Kostopoulos, V.; Stamatelatou, M.; Tryfou, E.; Mihas, K.; Damaskos, D.; Tsougos, E.; Olympios, C.; Kouris, N. Tissue Doppler imaging of left atrial appendage during transoesophageal echocardiography predicts successful cardioversion in patients with atrial fibrillation. Eur. Heart J. Cardiovasc. Imaging 2021, 22 (Suppl. S1), jeaa356.102. [Google Scholar] [CrossRef]
- Marchese, P.; Bursi, F.; Delle Donne, G.; Malavasi, V.; Casali, E.; Barbieri, A.; Melandri, F.; Modena, M.G. Indexed left atrial volume predicts the recurrence of non-valvular atrial fibrillation after successful cardioversion. Eur. J. Echocardiogr. 2010, 12, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Marchese, P.; Malavasi, V.; Rossi, L.; Nikolskaya, N.; Donne, G.D.; Becirovic, M.; Colantoni, A.; Luciani, A.; Modena, M.G. Indexed left atrial volume is superior to left atrial diameter in predicting nonvalvular atrial fibrillation recurrence after successful cardioversion: A prospective study. Echocardiography 2012, 29, 276–284. [Google Scholar] [CrossRef]
- Marques-Alves, P.; Marinho, A.V.; Domingues, C.; Baptista, R.; Castro, G.; Martins, R.; Gonçalves, L. Left atrial mechanics in moderate mitral valve disease: Earlier markers of damage. Int. J. Cardiovasc. Imaging 2020, 36, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Luong, C.; Thompson, D.J.; Bennett, M.; Gin, K.; Jue, J.; Barnes, M.E.; Colley, P.; Tsang, T.S. Right atrial volume is superior to left atrial volume for prediction of atrial fibrillation recurrence after direct current cardioversion. Can. J. Cardiol. 2015, 16, 29–35. [Google Scholar] [CrossRef]
- Fornengo, C.; Antolini, M.; Frea, S.; Gallo, C.; Grosso Marra, W.; Morello, M.; Gaita, F. Prediction of atrial fibrillation recurrence after cardioversion in patients with left-atrial dilation. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 335–341. [Google Scholar] [CrossRef]
- Toufan, M.; Kazemi, B.; Molazadeh, N. The significance of the left atrial volume index in prediction of atrial fibrillation recurrence after electrical cardioversion. J. Cardiovasc. Thorac. Res. 2017, 9, 54. [Google Scholar] [CrossRef] [PubMed]
- Di Salvo, G.; Caso, P.; Lo Piccolo, R.; Fusco, A.; Martiniello, A.R.; Russo, M.G.; D’Onofrio, A.; Severino, S.; Calabró, P.; Pacileo, G. Atrial myocardial deformation properties predict maintenance of sinus rhythm after external cardioversion of recent-onset lone atrial fibrillation: A color Doppler myocardial imaging and transthoracic and transesophageal echocardiographic study. Circulation 2005, 112, 387–395. [Google Scholar] [CrossRef]
- Opolski, G.; Ścisło, P.; Stanisławska, J.; Górecki, A.; Steckiewicz, R.; Torbicki, A. Detection of patients at risk for recurrence of atrial fibrillation after successful electrical cardioversion by signal-averaged P-wave ECG. Int. J. Cardiol. 1997, 60, 181–185. [Google Scholar] [CrossRef]
- Choi, J.-H.; Kwon, H.-J.; Kim, H.R.; Park, S.-J.; Kim, J.S.; On, Y.K.; Park, K.-M. Electrocardiographic predictors of early recurrence of atrial fibrillation. Ann. Noninvasive Electrocardiol. 2021, 26, e12884. [Google Scholar] [CrossRef]
- Dogan, A.; Avsar, A.; Ozturk, M. P-wave dispersion for predicting maintenance of sinus rhythm after cardioversion of atrial fibrillation. Am. J. Cardiol. 2004, 93, 368–371. [Google Scholar] [CrossRef]
- Stafford, P.J.; Kamalvand, K.; Tan, K.; Vincent, R.; Sulke, N. Prediction of maintenance of sinus rhythm after cardioversion of atrial fibrillation by analysis of serial signal-averaged P waves. Pacing Clin. Electrophysiol. 1998, 21, 1387–1395. [Google Scholar] [CrossRef] [PubMed]
- Aytemir, K.; Aksoyek, S.; Yildirir, A.; Ozer, N.; Oto, A. Prediction of atrial fibrillation recurrence after cardioversion by P wave signal-averaged electrocardiography. Int. J. Cardiol. 1999, 70, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Raitt, M.H.; Ingram, K.D.; Thurman, S.M. Signal-averaged P wave duration predicts early recurrence of atrial fibrillation after cardioversion. Pacing. Clin. Electrophysiol. 2000, 23, 259–265. [Google Scholar] [CrossRef]
- Dixen, U.; Joens, C.; Parner, J.; Rasmussen, V.; Pehrson, S.; Jensen, G. Prolonged signal-averaged P wave duration after elective cardioversion increases the risk of recurrent atrial fibrillation. Scand. Cardiovasc. J. 2004, 38, 147–151. [Google Scholar] [CrossRef]
- Guo, X.H.; Gallagher, M.M.; Poloniecki, J.; Yi, G.; Camm, A.J. Prognostic significance of serial P wave signal-averaged electrocardiograms following external electrical cardioversion for persistent atrial fibrillation: A prospective study. Pacing Clin. Electrophysiol. 2003, 26, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Ehrlich, J.; Schadow, K.; Steul, K.; Zhang, G.; Israel, C.; Hohnloser, S. Prediction of early recurrence of atrial fibrillation after external cardioversion by means of P wave signal-averaged electrocardiogram. Z. Kardiol. 2003, 92, 540–546. [Google Scholar] [CrossRef]
- Perzanowski, C.; Ho, A.T.; Jacobson, A.K. Increased P-wave dispersion predicts recurrent atrial fibrillation after cardioversion. J. Electrocardiol. 2005, 38, 43–46. [Google Scholar] [CrossRef]
- Budeus, M.; Hennersdorf, M.; Perings, C.; Wieneke, H.; Erbel, R.; Sack, S. Prediction of the recurrence of atrial fibrillation after successful cardioversion with P wave signal-averaged ECG. Ann. Noninvasive Electrocardiol. 2005, 10, 414–419. [Google Scholar] [CrossRef]
- Başar, N.; Malçok Gürel, O.; Ozcan, F.; Ozlü, M.F.; Biçer Yeşilay, A.; Cağlı, K.; Sen, N.; Işleyen, A.; Uygur, B.; Akpınar, I.; et al. Diagnostic accuracy of P-wave dispersion in prediction of maintenance of sinus rhythm after external cardioversion of atrial fibrillation. Anadolu. Kardiyol. Derg. 2011, 11, 34–38. [Google Scholar] [CrossRef]
- Gonna, H.; Gallagher, M.M.; Guo, X.H.; Yap, Y.G.; Hnatkova, K.; Camm, A.J. P-wave abnormality predicts recurrence of atrial fibrillation after electrical cardioversion: A prospective study. Ann. Noninvasive Electrocardiol. 2014, 19, 57–62. [Google Scholar] [CrossRef]
- Blanche, C.; Tran, N.; Carballo, D.; Rigamonti, F.; Burri, H.; Zimmermann, M. Usefulness of P-wave signal averaging to predict atrial fibrillation recurrences after electrical cardioversion. Ann. Noninvasive Electrocardiol. 2014, 19, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, Y.; Yodogawa, K.; Maru, Y.-J.; Oka, E.; Hayashi, H.; Yamamoto, T.; Iwasaki, Y.-K.; Hayashi, M.; Shimizu, W. Advanced interatrial block is an electrocardiographic marker for recurrence of atrial fibrillation after electrical cardioversion. Int. J. Cardiol. 2018, 272, 113–117. [Google Scholar] [CrossRef] [PubMed]
- German, D.M.; Kabir, M.M.; Dewland, T.A.; Henrikson, C.A.; Tereshchenko, L.G. Atrial fibrillation predictors: Importance of the electrocardiogram. Ann. Noninvasive Electrocardiol. 2016, 21, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.; Lee, E.; Ju, H.; Ahn, H.-J.; Lee, S.-R.; Choi, E.-K.; Suh, J.; Oh, S.; Rhee, W. Machine learning prediction for the recurrence after electrical cardioversion of patients with persistent atrial fibrillation. Korean Circ. J. 2023, 53, 677–689. [Google Scholar] [CrossRef]
- Nunez-Garcia, J.C.; Sanchez-Puente, A.; Sampedro-Gómez, J.; Vicente-Palacios, V.; Jiménez-Navarro, M.; Oterino-Manzanas, A.; Jimenez-Candil, J.; Dorado-Diaz, P.I.; Sanchez, P.L. Outcome analysis in elective electrical cardioversion of atrial fibrillation patients: Development and validation of a machine learning prognostic model. J. Clin. Med. 2022, 11, 2636. [Google Scholar] [CrossRef]

| Study | Study Identified Demographic or Clinical Factor Associayed with DCCV Failure |
|---|---|
| Frick et al., 2001, Brodsky et al., 1989 [41,42] | Obesity, Increasing AF duration |
| Suttorp et al., 1993 [44] | Females, Ischaemic heart disease |
| Alt et al., 1997 [45] | Increasing age |
| van den Berg et al., 1998, Caputo et al., 2011, Melduni and Cullen, 2012 [46,47,48] | Heart failure (reduced and preserved ejection fraction) |
| Lange and Herrmann-Lingen, 2007 [57] | Low mood |
| Soran et al., 2008 [49] | Diabetes melitus |
| Kanagala et al., 2003 [50] | Obstructive sleep apnoea |
| Schmidt et al., 2011 [51] | Renal impairment |
| Pisters et al., 2012 [52] | Chronic obstructive lung disease |
| Mlynarska et al., 2020 [56] | High frailty score |
| García-Izquierdo et al., 2020 [58] | Anxiety |
| Study | Biochemical Markers Relation to Direct Current Cardioversion Failure |
|---|---|
| Liu et al., 2007 [59] | Increased C-reactive protein |
| Siu et al., 2009 [62] | Circulating endothelial progenitor cell count ↓ (fibrotic marker) |
| Kawamura et al., 2012 [60] | Type III procollagen-N-peptide ↑ (fibrotic marker) |
| Parvez et al., 2013, Shoemaker et al., 2015 [67,68] | Polymorphisms on the 4q25 chromosome |
| Zografos et al., 2014 [63] | Increased B-type natriuretic peptide |
| Gürses et al., 2019 [61] | Galectin 3 (fibrotic marker) |
| Rigopoulos et al., 2021 [64] | Serum interleukin 2 ↑, heat shock protein 70 ↑ (involved in cellular protein folding) |
| Study | Imaging Correlation with DCCV Failure |
|---|---|
| Verhorst et al., 1997, Kostakou et al., 2021 [69,70] | LA appendage flow ↓ |
| Di Salvo et al., 2005 [77] | Atrial strain ↓ |
| Marchese et al., 2010, Marchese et al., 2012 [71,72] | LAVI ↑ |
| Luong et al., 2015 [74] | RA volume ↑ > LAVI ↑ |
| Fornengo et al., 2015, Toufan et al., 2017 [75,76] | LA dilation |
| Marques-Alves et al., 2020 [73] | Mitral valve disease |
| Author and Year | AF | n | Follow-up | ECG | Parameter | Recurrence Change | Recurrence Cut-off |
|---|---|---|---|---|---|---|---|
| Opolski et al., 1997 [78] | PersAF | 35 | 6 months | SAECG | PWD | ↑ | >137 ms |
| Stafford et al., 1998 [81] | PersAF (77%) | 31 | 1 week | SAECG | P wave energy | ↑ | 25%> drop |
| Aytemir et al., 1999 [82] | PersAF | 73 | 6 months | SAECG | Filtered PWD | ↑ | >128 ms |
| Raitt et al., 2000 [83] | PersAF | 20 | 1 year | SAECG | PWD | ↑ | >130-140 ms |
| Guo et al., 2003 [85] | PersAF | 60 | 6 months | SAECG | Filtered PWD | ↑ | Nil |
| Ehrlich et al., 2003 [86] | No mention | 111 | 1 week | SAECG | PWD | ↑ | >145 ms |
| Dixen et al., 2004 [84] | PersAF | 131 | 1 month | SAECG | PWD | ↑ | >160 ms |
| Dogan et al., 2004 [80] | PersAF (45%) | 64 | 6 months | SAECG | PWDisp | ↑ | >46 ms |
| Perzanowski et al., 2005 [87] | PersAF | 45 | 6 months | SAECG | PWDisp | ↑ | >80 ms |
| Budeus et al., 2005 [88] | PersAF | 141 | 1 year | SAECG | PWD | ↑ | >126 ms |
| Başar et al., 2011 [89] | PersAF | 26 | 1 year | 12 leads | PWDisp | ↑ | |
| Gonna et al., 2014 [90] | PersAF | 77 | 1 month | 12 leads | PWD | ↑ | >125 ms |
| Blanche et al., 2014 [91] | PersAF | 133 | 9 months | SAECG | Nil | Nil | Nil |
| Fujimoto et al., 2018 [92] | PersAF | 141 | 1 month | 12 leads | PWDisp | ↑ | Nil |
| Choi et al., 2021 [79] | PersAF | 272 | 2 months | 12 leads | PWD, PTFV1 | ↑ | >134 ms, >50 ms.mm |
| Antoun et al., 2024 [7] | PersAF | 52 | 12 months | Body surface mapping | PWD | ↑ | >161 ms |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antoun, I.; Layton, G.R.; Abdelrazik, A.; Eldesouky, M.; Altoukhy, S.; Zakkar, M.; Somani, R.; Ng, G.A. Predicting the Outcomes of External Direct Current Cardioversion for Atrial Fibrillation: A Narrative Review of Current Evidence. J. Cardiovasc. Dev. Dis. 2025, 12, 168. https://doi.org/10.3390/jcdd12050168
Antoun I, Layton GR, Abdelrazik A, Eldesouky M, Altoukhy S, Zakkar M, Somani R, Ng GA. Predicting the Outcomes of External Direct Current Cardioversion for Atrial Fibrillation: A Narrative Review of Current Evidence. Journal of Cardiovascular Development and Disease. 2025; 12(5):168. https://doi.org/10.3390/jcdd12050168
Chicago/Turabian StyleAntoun, Ibrahim, Georgia R. Layton, Ahmed Abdelrazik, Mahmoud Eldesouky, Sherif Altoukhy, Mustafa Zakkar, Riyaz Somani, and G. André Ng. 2025. "Predicting the Outcomes of External Direct Current Cardioversion for Atrial Fibrillation: A Narrative Review of Current Evidence" Journal of Cardiovascular Development and Disease 12, no. 5: 168. https://doi.org/10.3390/jcdd12050168
APA StyleAntoun, I., Layton, G. R., Abdelrazik, A., Eldesouky, M., Altoukhy, S., Zakkar, M., Somani, R., & Ng, G. A. (2025). Predicting the Outcomes of External Direct Current Cardioversion for Atrial Fibrillation: A Narrative Review of Current Evidence. Journal of Cardiovascular Development and Disease, 12(5), 168. https://doi.org/10.3390/jcdd12050168






