Impact of Revascularization on Major Adverse Cardiovascular Events in Patients Without ST-Elevation Myocardial Infarction in the Arabian Gulf
Abstract
1. Introduction
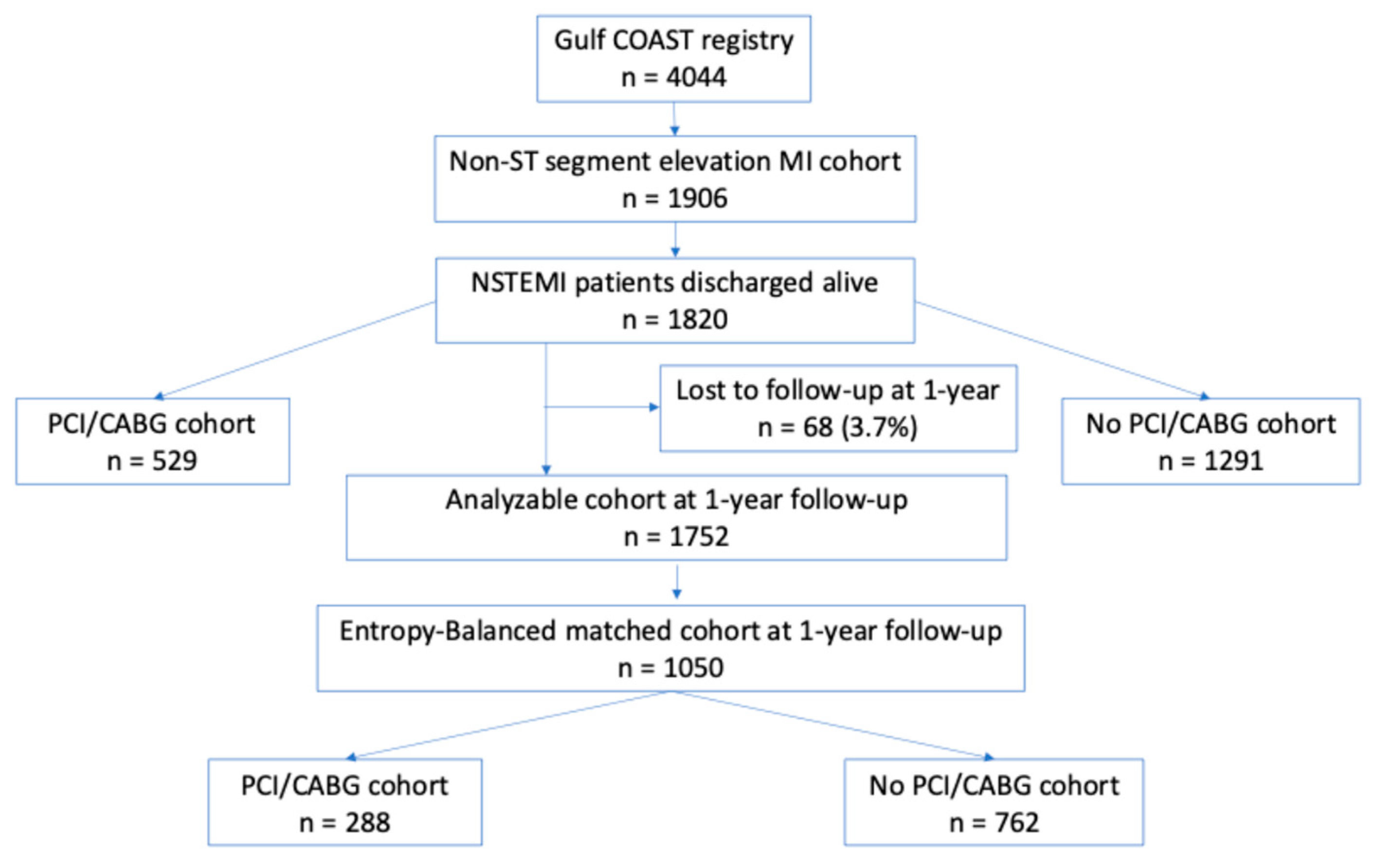
2. Methods
2.1. Study Design, Setting, and Population
2.2. Ethical Approval
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ohira, T.; Iso, H. Cardiovascular disease epidemiology in Asia: An overview. Circ. J. 2013, 77, 1646–1652. [Google Scholar] [CrossRef] [PubMed]
- Vedanthan, R.; Seligman, B.; Fuster, V. Global perspective on acute coronary syndrome: A burden on the young and poor. Circulation 2014, 114, 1959–1975. [Google Scholar] [CrossRef] [PubMed]
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. ESC Scientific Document Group. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart. J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- Amsterdam, E.A.; Brindis, R.G.; Casey, D.E.; Ganiats, T.G.; Holmes, D.R.; Jaffe, A.S.; Jneid, H.; Kelly, R.F.; Kontos, M.C.; Levine, G.N.; et al. ACC/AHA Task Force Members. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014, 130, e344–e426. [Google Scholar] [CrossRef]
- Bavry, A.A.; Kumbhani, D.J.; Rassi, A.N.; Bhatt, D.L.; Askari, A.T. Benefit of early invasive therapy in acute coronary syndromes: A meta-analysis of contemporary randomized clinical trials. J. Am. Coll. Cardiol. 2006, 48, 1319–1325. [Google Scholar] [CrossRef]
- Kirov, H.; Caldonazo, T.; Rahouma, M.; Robinson, N.B.; Demetres, M.; Serruys, P.W.; Biondi-Zoccai, G.; Gaudino, M.; Doenst, D.T. A systematic review and meta-analysis of percutaneous coronary intervention compared to coronary artery bypass grafting in non-ST-elevation acute coronary syndrome. Sci. Rep. 2022, 12, 5138. [Google Scholar] [CrossRef] [PubMed]
- Kakar, H.; Groenland, F.T.W.; Elscot, J.J.; Rinaldi, R.; Scoccia, A.; Kardys, I.; Nuis, R.J.; Wilschut, J.; Den Dekker, W.K.; Daemen, J.; et al. Percutaneous Coronary Intervention Versus Coronary Artery Bypass Grafting in Non-ST-Elevation Coronary Syndromes and Multivessel Disease: A Systematic Review and Meta-Analysis. Am. J. Cardiol. 2023, 195, 70–76. [Google Scholar] [CrossRef]
- Thomas, K.L.; Honeycutt, E.; Shaw, L.K.; Peterson, E.D. Racial differences in long-term survival among patients with coronary artery disease. Am. Heart. J. 2010, 160, 744–751. [Google Scholar] [CrossRef]
- Shaw, L.J.; Shaw, R.E.; Merz, C.N.B.; Brindis, R.G.; Klein, L.W.; Nallamothu, B.; Douglas, P.S.; Krone, R.J.; McKay, C.R.; Block, P.C.; et al. American College of Cardiology-National Cardiovascular Data Registry Investigators. Impact of ethnicity and gender differences on angiographic coronary artery disease prevalence and in-hospital mortality in the American College of Cardiology-National Cardiovascular Data Registry. Circulation 2008, 117, 1787–1801. [Google Scholar] [CrossRef]
- Gregory, P.C.; LaVeist, T.A.; Simpson, C. Racial disparities in access to cardiac rehabilitation. Am. J. Phys. Med. Rehabil. 2006, 85, 705–710. [Google Scholar] [CrossRef]
- Trivedi, A.N.; Sequist, T.D.; Ayanian, J.Z. Impact of hospital volume on racial disparities in cardiovascular procedure mortality. J. Am. Coll. Cardiol. 2006, 47, 417–424. [Google Scholar] [CrossRef]
- Pamboukian, S.V.; Funkhouser, E.; Child, I.G.; Allison, J.J.; Weissman, N.W.; Kiefe, C.I. Disparities by insurance status in quality of care for elderly patients with unstable angina. Ethn. Dis. 2006, 16, 799–807. [Google Scholar] [PubMed]
- AlHabib, K.F.; Hersi, A.; Alsheikh-Ali, A.A.; Sulaiman, K.; Alfaleh, H.; Alsaif, S.; Almahmeed, W.; Asaad, N.; Amin, H.; Al-Motarreb, A.; et al. Gulf RACE-2 Investigators. Prevalence, predictors, and outcomes of conservative medical management in non-ST-segment elevation acute coronary syndromes in Gulf RACE-2. Angiology 2012, 63, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Zubaid, M.; Modal, O.; Thani, K.B.; Rashed, W.; Alsheikh-Ali, A.; Alrawahi, N.; Ridha, M.; Akbar, M.; Alenezi, F.; Alhamdan, R.; et al. Gulf COAST investigators. Design and Rationale of Gulf locals with Acute Coronary Syndrome Events (Gulf Coast) Registry. Open. Cardiovasc. Med. J. 2014, 8, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Weintraub, W.S.; Karlsberg, R.P.; Tcheng, J.E.; Boris, J.R.; Buxton, A.E.; Dove, J.T.; Fonarow, G.C.; Goldberg, L.R.; Heidenreich, P.; Hendel, R.C.; et al. ACCF/AHA 2011 key data elements and definitions of a base cardiovascular vocabulary for electronic health records: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Data Standards. J. Am. Coll. Cardiol. 2011, 58, 202–222. [Google Scholar] [CrossRef]
- Al-Zakwani, I.; Al-Maqbali, J.S.; AlMahmeed, W.; AlRawahi, N.; Al-Asmi, A.; Zubaid, M. Association between Non-Steroidal Anti-Inflammatory Drug Use and Major Cardiovascular Outcomes in Patients with Acute Coronary Syndrome in the Arabian Gulf. J. Clin. Med. 2023, 12, 5446. [Google Scholar] [CrossRef]
- Normand, S.T.; Landrum, M.B.; Guadagnoli, E.; Ayanian, J.Z.; Ryan, T.J.; Cleary, P.D.; McNeil, B.J. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: A matched analysis using propensity scores. J. Clin. Epidemiol. 2001, 54, 387–398. [Google Scholar] [CrossRef]
- Rubin, D.B. Using propensity scores to help design observational studies: Application to the tobacco litigation. Health. Serv. Outcomes. Res. Methodol. 2001, 2, 169–188. [Google Scholar]
- Stone, S.G.; Serrao, G.W.; Mehran, R.; Tomey, M.I.; Witzenbichler, B.; Guagliumi, G.; Peruga, J.Z.; Brodie, B.R.; Dudek, D.; Möckel, M.; et al. Incidence, predictors, and implications of reinfarction after primary percutaneous coronary intervention in ST-segment-elevation myocardial infarction: The Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction Trial. Circ. Cardiovasc. Interv. 2014, 7, 543–551. [Google Scholar] [CrossRef]
- Mehta, S.R.; Granger, C.B.; Boden, W.E.; Steg, P.G.; Bassand, J.-P.; Faxon, D.P.; Afzal, R.; Susan Chrolavicius, R.N.; Jolly, S.S.; Widimsky, P.; et al. TIMACS Investigators. Early versus delayed invasive intervention in acute coronary syndromes. N. Engl. J. Med. 2009, 360, 2165–2175. [Google Scholar] [CrossRef]
- Kofoed, K.F.; Kelbæk, H.; Hansen, P.R.; Torp-Pedersen, C.; Høfsten, D.; Kløvgaard, L.; Holmvang, L.; Helqvist, S.; Jørgensen, E.; Galatius, S.; et al. Early Versus Standard Care Invasive Examination and Treatment of Patients With Non-ST-Segment Elevation Acute Coronary Syndrome. Circulation 2018, 138, 2741–2750. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.; Cha, J.-J.; Lim, S.; Kim, J.H.; Joo, H.J.; Park, J.H.; Hong, S.J.; Yu, C.W.; Lim, D.-S.; Kim, Y.; et al. Early Invasive Strategy Based on the Time of Symptom Onset of Non-ST-Segment Elevation Myocardial Infarction. JACC. Cardiovasc. Interv. 2023, 16, 64–75. [Google Scholar] [CrossRef]
- Chan, M.Y.; Sun, J.L.; Newby, L.K.; Shaw, L.K.; Lin, M.; Peterson, E.D.; Califf, R.M.; Kong, D.F.; Roe, M.T. Long-term mortality of patients undergoing cardiac catheterization for ST-elevation and non-ST-elevation myocardial infarction. Circulation 2009, 119, 3110–3117. [Google Scholar] [CrossRef] [PubMed]
- Murat, B.; Kivanc, E.; Dizman, R.; Mert, G.O.; Murat, S. Gender differences in clinical characteristics and in-hospital and one-year outcomes of young patients with ST-segment elevation myocardial infarction under the age of 40. J. Cardiovasc. Thorac. Res. 2021, 13, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Park, H.W.; Yoonb, C.H.; Kangb, S.-H.; Ahni, Y.-H.; Jeong, M.-H. KAMIR/KorMI Registry. Early- and late-term clinical outcome and their predictors in patients with ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction. Int. J. Cardiol. 2013, 169, 254–261. [Google Scholar] [CrossRef]
- Canton, L.; Suma, N.; Amicone, S.; Impellizzeri, A.; Bodega, F.; Marinelli, V.; Ciarlantini, M.; Casuso, M.; Bavuso, L.; Belà, R.; et al. Clinical impact of multimodality assessment of myocardial viability. Echocardiography 2024, 41, e15854. [Google Scholar] [CrossRef]
- Armillotta, M.; Bergamaschi, L.; Paolisso, P.; Belmonte, M.; Angeli, F.; Sansonetti, A.; Stefanizzi, A.; Bertolini, D.; Bodega, F.; Amicone, S.; et al. Prognostic Relevance of Type 4a Myocardial Infarction and Periprocedural Myocardial Injury in Patients with Non-ST-Segment-Elevation Myocardial Infarction. Circulation 2025, 151, 11. [Google Scholar] [CrossRef]
| Characteristic | Original Unmatched Cohort (n = 1820) | EB Matched Cohort (n = 1050) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PCI/CABG | PCI/CABG | |||||||||
| All (n = 1820) | With (n = 529) | Without (n = 1291) | p-Value | SMD | All (n = 1050) | With (n = 288) | Without (n = 762) | p-Value | SMD | |
| Demographic, n (%) unless stated otherwise | ||||||||||
| Age, years | 61.7 | 59.7 | 62.5 | <0.001 | −19.7 * | 62.2 | 60.4 | 60.5 | 0.954 | −0.5 |
| Male gender, n (%) | 65.4 | 71.5 | 62.9 | <0.001 | 19.8 * | 64.9 | 72.0 | 71.9 | 0.982 | 0.2 |
| BMI, kg/m2 | 28.5 | 28.5 | 28.5 | 0.916 | 0 | 28.7 | 28.7 | 28.7 | 0.916 | 0.9 |
| Smoker, n (%) | 20.7 | 25.0 | 19.0 | 0.004 | 19.1 * | 20.0 | 26.7 | 25.3 | 0.712 | 3.2 |
| Clinical, n (%) unless stated otherwise | ||||||||||
| GRACE risk score | 132.1 | 123.6 | 135.6 | <0.001 | −25.6 * | 127.7 | 127.8 | 127.7 | 0.956 | 0.4 |
| Atrial fibrillation | 4.6 | 2.1 | 5.7 | 0.005 | −21.2 * | 2.1 | 2.0 | 2.0 | 0.962 | −0.3 |
| Trop, ng/mL | 26.5 | 35.5 | 22.9 | 0.018 | 9.4 | 30.7 | 29.9 | 30.7 | 0.937 | −0.7 |
| Diabetes mellitus | 57.6 | 55.2 | 58.6 | 0.188 | −2.0 | 55.9 | 56.8 | 55.9 | 0.836 | 1.7 |
| Hypertension | 70.5 | 68.2 | 71.4 | 0.177 | 0.9 | 71.9 | 72.0 | 71.9 | 0.982 | 0.2 |
| Dyslipidemia | 59.7 | 69.9 | 55.5 | <0.001 | 28.0 * | 67.8 | 68.6 | 67.7 | 0.821 | 1.8 |
| Killip class II/III/IV | 25.2 | 15.1 | 29.4 | <0.001 | −29.6 * | 19.1 | 19.3 | 19.1 | 0.961 | 0.4 |
| LVEF < 40% | 23.3 | 19.4 | 24.8 | 0.05 | −14.3 * | 18.8 | 19.3 | 18.8 | 0.876 | 1.2 |
| CVD | 38.8 | 35.7 | 40.1 | 0.086 | −5.2 | 35.4 | 34.8 | 35.4 | 0.876 | −1.3 |
| Cardiogenic shock | 2.8 | 4.4 | 2.1 | 0.007 | 20.3 * | 5.2 | 5.7 | 5.2 | 0.777 | 2.8 |
| Renal failure | 9.8 | 6.8 | 11.0 | 0.006 | −11.3 * | 8.3 | 8.1 | 8.3 | 0.921 | −0.8 |
| Prior PCI/CABG | 28.5 | 31.6 | 27.2 | 0.06 | 17.3 * | 32.0 | 32.1 | 31.9 | 0.969 | 0.3 |
| In-hospital medications, n (%) | ||||||||||
| UFH/LMWH | 85.9 | 83.9 | 86.8 | 0.116 | −11.5 * | 84.7 | 84.5 | 84.7 | 0.93 | −0.8 |
| GP IIb/IIIa blocker | 5.6 | 15.5 | 1.5 | <0.001 | 56.3 * | 15.7 | 17.9 | 15.6 | 0.462 | 7.9 |
| Thrombolytic | 0.2 | 0 | 0.2 | 0.267 | −8.7 | 0 | 0 | 0 | 1.000 | 0 |
| Inotropes | 5.4 | 8.5 | 4.1 | <0.001 | 27.4 * | 9.8 | 10.8 | 9.7 | 0.666 | 4.2 |
| Medications at discharge, n (%) | ||||||||||
| Aspirin | 92.1 | 98.5 | 89.5 | <0.001 | 32.8 * | 98.3 | 98.3 | 98.2 | 0.965 | 0.2 |
| Platelet inhibitor | 70.9 | 93.8 | 61.5 | <0.001 | 71.4 * | 91.7 | 91.9 | 91.7 | 0.921 | 0.6 |
| RAS blocker | 74.7 | 73.5 | 77.7 | 0.062 | 6.4 | 78.2 | 78.4 | 78.1 | 0.941 | 0.6 |
| Beta blocker | 79.9 | 85.8 | 77.5 | <0.001 | 22.7 * | 86.1 | 86.1 | 86.1 | 0.99 | 0.1 |
| Statin | 93.0 | 98.1 | 90.9 | <0.001 | 30.6 * | 98.6 | 98.6 | 98.6 | 0.969 | 0.2 |
| Outcome Characteristics | Original Unmatched Cohort (n = 1820) | EB Matched Cohort (n = 1050) | ||||
|---|---|---|---|---|---|---|
| PCI/CABG | PCI/CABG | |||||
| Without (n = 1291) | With (n = 529) | p-Value | Without (n = 762) | With (n = 288) | p-Value | |
| MACE | 563 (44%) | 140 (26%) | <0.001 | 326 (43%) | 71 (25%) | <0.001 |
| Stroke/TIA | 73 (5.7%) | 15 (2.8%) | 0.011 | 53 (7.0%) | 7 (2.4%) | 0.005 |
| Reinfarction | 17 (1.3%) | 10 (1.9%) | 0.358 | 11 (1.4%) | 5 (1.7%) | 0.73 |
| All-cause mortality | 184 (14%) | 27 (5.1%) | <0.001 | 100 (13%) | 13 (4.5%) | <0.001 |
| Cardiac-related readmission | 399 (31%) | 112 (21%) | <0.001 | 235 (31%) | 58 (20%) | 0.001 |
| Characteristic | LTF (n = 68) 3.7% | Remaining (n = 1752) 96.3% | p-Value |
|---|---|---|---|
| Demographic, mean ± SD unless stated otherwise | |||
| Age, years | 62.1 ± 12.8 | 61.7 ± 12.2 | 0.788 |
| Male gender, n (%) | 48 (70.6%) | 1142 (65.2%) | 0.358 |
| BMI, kg/m2 | 28.5 ± 5.1 | 28.5 ± 5.8 | 0.946 |
| Smoker, n (%) | 22 (32.4%) | 355 (20.3%) | 0.011 |
| Clinical, mean ± SD or median (IQR) unless stated otherwise | |||
| GRACE risk score | 135.3 ± 44.1 | 132.0 ± 38.2 | 0.491 |
| Atrial fibrillation, n (%) | 3 (4.4%) | 81 (4.6%) | 0.935 |
| Troponin, ng/ml | 0.2 (0.1–1.8) | 0.3 (0.1–2.9) | 0.552 |
| Diabetes mellitus, n (%) | 39 (57.4%) | 1009 (57.6%) | 0.969 |
| Hypertension, n (%) | 41 (60.3%) | 1242 (70.9%) | 0.06 |
| Dyslipidemia, n (%) | 35 (51.5%) | 1052 (60.1%) | 0.157 |
| Killip class II/III/IV, n (%) | 15 (22.1%) | 444 (25.3%) | 0.541 |
| LVEF <40%, n (%) | 6 (12.2%) | 269 (23.8%) | 0.061 |
| CVD, n (%) | 27 (39.7%) | 679 (38.8%) | 0.875 |
| Cardiogenic shock, n (%) | 3 (4.4%) | 47 (2.7%) | 0.392 |
| Renal failure, n (%) | 8 (11.8%) | 170 (9.7%) | 0.574 |
| Prior PCI/CABG, n (%) | 24 (35.3%) | 494 (28.2%) | 0.203 |
| In-hospital medications, n (%) | |||
| UFH/LMWH | 62 (91.2%) | 1502 (85.7%) | 0.205 |
| GP IIb/IIIa inhibitor | 2 (2.9%) | 99 (5.7%) | 0.338 |
| Thrombolytic | 0 | 3 (0.2%) | 0.733 |
| Inotropes | 5 (7.4%) | 93 (5.3%) | 0.464 |
| Medications at discharge, n (%) | |||
| Aspirin | 55 (80.9%) | 1621 (92.5%) | <0.001 |
| Platelet inhibitor | 43 (63.2%) | 1247 (71.2%) | 0.157 |
| RAS blocker | 45 (66.2%) | 1315 (75.1%) | 0.098 |
| Beta blocker | 54 (79.4%) | 1400 (79.9%) | 0.92 |
| Statin, n (%) | 60 (88.2%) | 1632 (93.2%) | 0.12 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Zakwani, I.; AlKindi, F.; Almahmeed, W.; Zubaid, M. Impact of Revascularization on Major Adverse Cardiovascular Events in Patients Without ST-Elevation Myocardial Infarction in the Arabian Gulf. J. Cardiovasc. Dev. Dis. 2025, 12, 117. https://doi.org/10.3390/jcdd12040117
Al-Zakwani I, AlKindi F, Almahmeed W, Zubaid M. Impact of Revascularization on Major Adverse Cardiovascular Events in Patients Without ST-Elevation Myocardial Infarction in the Arabian Gulf. Journal of Cardiovascular Development and Disease. 2025; 12(4):117. https://doi.org/10.3390/jcdd12040117
Chicago/Turabian StyleAl-Zakwani, Ibrahim, Fahad AlKindi, Wael Almahmeed, and Mohammad Zubaid. 2025. "Impact of Revascularization on Major Adverse Cardiovascular Events in Patients Without ST-Elevation Myocardial Infarction in the Arabian Gulf" Journal of Cardiovascular Development and Disease 12, no. 4: 117. https://doi.org/10.3390/jcdd12040117
APA StyleAl-Zakwani, I., AlKindi, F., Almahmeed, W., & Zubaid, M. (2025). Impact of Revascularization on Major Adverse Cardiovascular Events in Patients Without ST-Elevation Myocardial Infarction in the Arabian Gulf. Journal of Cardiovascular Development and Disease, 12(4), 117. https://doi.org/10.3390/jcdd12040117






