Readmissions for Cardiac Disease Within 30 Days of Hospitalization for Cerebral Infarction: An Evaluation of the Stroke–Heart Syndrome Using the Nationwide Readmission Database
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting and Participants
2.3. Variables and Data Source
2.4. Statistical Methods
3. Results
3.1. Description of the Hospital Admissions with Cerebral Infarction According to Readmissions for Cardiac Disease
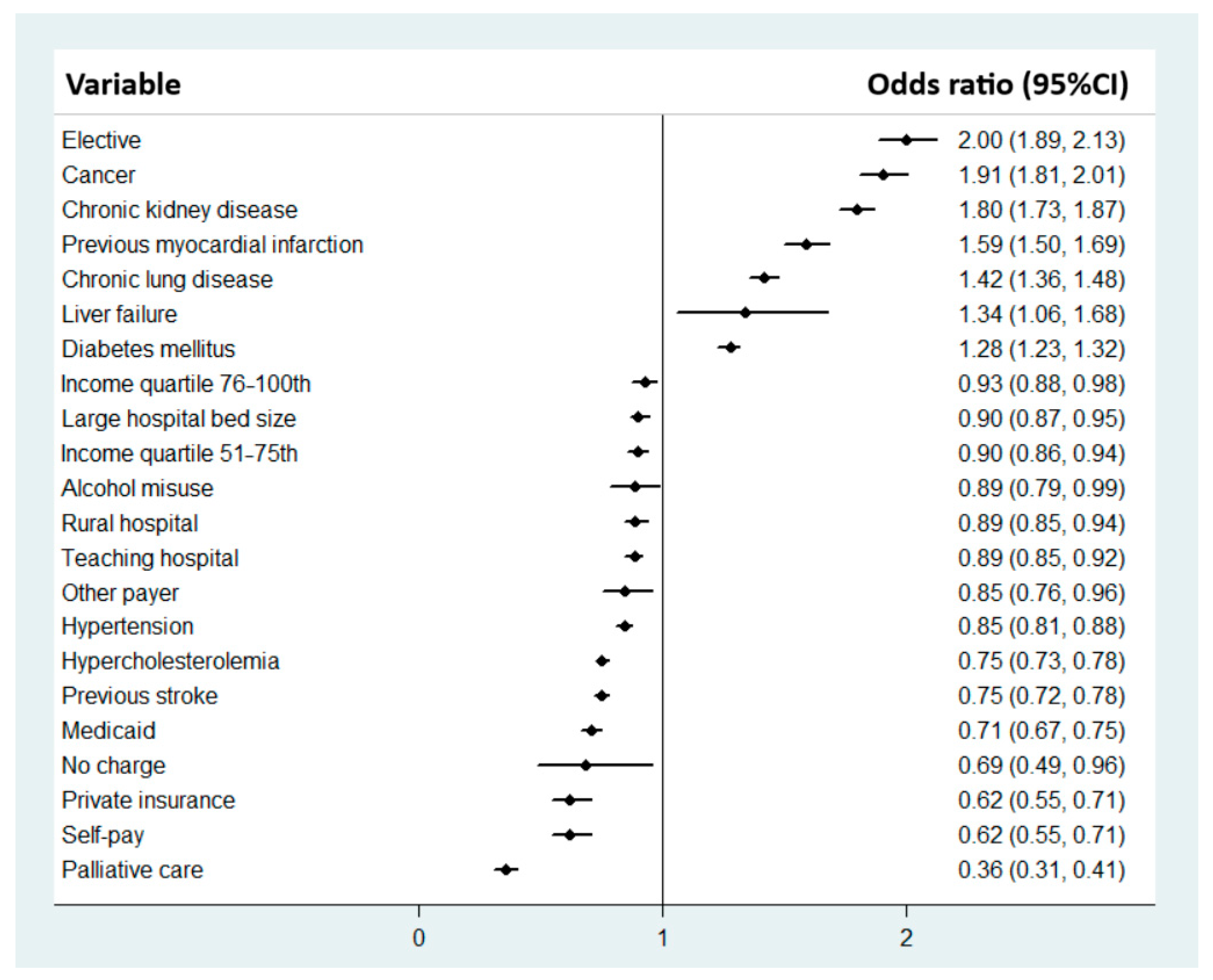
3.2. Factors Associated with 30-Day Readmissions for Cardiac Disease
3.3. Sensitivity Analysis
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Scheitz, J.F.; Nolte, C.H.; Doehner, W.; Hachinski, V.; Endres, M. Stroke-heart syndrome: Clinical presentation and underlying mechanism. Lancet Neurol. 2018, 17, 1109–1120. [Google Scholar] [CrossRef] [PubMed]
- Scheitz, J.F.; Sposato, L.A.; Schulz-Menger, J.; Nolte, C.H.; Backs, J.; Endres, M. Stroke-heart syndrome: Recent advances and challenges. J. Am. Heart Assoc. 2022, 11, e026528. [Google Scholar]
- Doehner, W.; Böhm, M.; Boriani, G.; Christersson, C.; Coats, A.J.S.; Haeusler, K.G.; Jones, I.D.; Lip, G.Y.H.; Metra, M.; Ntaios, G.; et al. Interaction of heart failure and stroke: A clinical consensus statement of the ESC Council on Stroke, the Heart Failure Association (HFA) and the ESC Working Group on Thrombosis. Eur. J. Heart Fail. 2023, 25, 2107–2129. [Google Scholar]
- Wang, M.; Peng, Y. Advances in brain-heart syndrome: Attention to cardiac complications after ischemic stroke. Front. Mol. Neurosci. 2022, 15, 1053478. [Google Scholar]
- Wang, L.; Ma, L.; Ren, C.; Zhao, W.; Ji, X.; Liu, Z.; Li, S. Stroke-heart syndrome: Current progress and future outlook. J. Neurol. 2024, 271, 4813–4815. [Google Scholar]
- Buckley, B.J.R.; Harrison, S.L.; Hill, A.; Underhill, P.; Lane, D.A.; Lip, G.Y.H. Stroke-Heart Syndrome: Incidence and clinical outcomes of cardiac complications following stroke. Stroke 2022, 53, 1759–1863. [Google Scholar] [CrossRef]
- Bucci, T.; Pastori, D.; Pignatelli, P.; Ntaios, G.; Abdul-Rahim, A.H.; Violi, F.; Lip, G.Y.H. Albumin levels and risk of early cardiovascular complications after ischemic stroke: A propensity-matched analysis of the a Global Federated Health Network. Stroke 2024, 55, 605–612. [Google Scholar]
- Bucci, T.; Sagris, D.; Harrison, S.L.; Underhill, P.; Pastori, D.; Ntaios, G.; McDowell, G.; Buckley, B.J.R.; Lip, G.Y.H. C-reactive protein levels are associated with early complications or death in patients with acute ischemic stroke: A propensity-match analysis of a global federated health from the TriNetX network. Intern. Emerg. Med. 2023, 18, 1329–1336. [Google Scholar] [CrossRef]
- Gruezo-Realpe, P.; Lainez, J.L.; Rodriguez-Alarcon, C.; Acosta, A. Stroke-heart syndrome: Clinical features, electrocardiographic, and imaging findings in the adult population. Neurology 2024, 102 (Suppl. S1), 17. [Google Scholar] [CrossRef]
- Kwok, C.S.; Abbas, K.S.; Iqbal, A.I.; Lip, G.Y.H. Outcomes for patients hospitalized with acute myocardial infarction and cerebral infarction in the United States: Insights from the National Inpatient Sample. Intern. Emerg. Med. 2023, 18, 375–383. [Google Scholar] [CrossRef]
- National Bureau of Economic Research. Guidance: Data Sets not Requiring IRB Review. Available online: https://www.nber.org/programs-projects/projects-and-centers/human-subjects-protection-and-institutional-review-board-irb/guidance-data-sets-not-requiring-irb-review (accessed on 1 October 2024).
- Agency for Healthcare Research and Quality. NRD Overview. Available online: https://hcup-us.ahrq.gov/nrdoverview.jsp (accessed on 1 October 2024).
- Sennfalt, S.; Petersson, J.; Ullberg, T.; Norrving, B. Patterns in hospital readmissions after ischaemic stroke—AN observational study from the Swedish stroke register. Eur. Stroke J. 2020, 5, 286–296. [Google Scholar] [PubMed]
- Vahidy, F.S.; Donnelly, J.P.; McCullogh, L.D.; Tyson, J.E.; Miller, C.C.; Boehme, A.K.; Savitz, S.I.; Albright, K.C. Nationwide estimates of 30-day readmissions in patients with ischemic stroke. Stroke 2017, 48, 1386–1388. [Google Scholar] [PubMed]
- Lee, K.J.; Kim, S.E.; Kim, J.Y.; Kang, J.; Kim, B.J.; Han, M.K.; Choi, K.H.; Kim, J.T.; Shin, D.I.; Cha, J.K.; et al. Five-year risk of acute myocardial infarction after acute ischemic stroke in Korea. J. Am. Heart Assoc. 2021, 10, e018807. [Google Scholar]
- Carlsson, A.; Irewall, A.L.; Graipe, A.; Ulvenstam, A.; Moore, T.; Ogren, J. Long-term risk of major adverse cardiovascular events following ischemic stroke and TIA. Sci. Rep. 2023, 13, 8333. [Google Scholar]
- Favilla, C.G.; Ingala, E.; Jara, J.; Fessler, E.; Cucchiara, B.; Messe, S.R.; Mullen, M.T.; Prasad, A.; Siegler, J.; Hutching, M.D.; et al. Predictors of finding occult atrial fibrillation after cryptogenic stroke. Stroke 2015, 46, 1205–1210. [Google Scholar]
- Wang, Y.; Qian, Y.; Smerin, D.; Zhang, S.; Zhao, Q.; Xiong, X. Newly detected atrial fibrillation after acute stroke: A narrative review of cause and implications. Cardiology 2019, 144, 112–121. [Google Scholar]
- Koppikar, S.; Baranchuk, A.; Guzman, J.C.; Morillo, C.A. Stroke and ventricular arrhythmias. Int. J. Cardiol. 2013, 168, 653–659. [Google Scholar]
- Chen, Z.; Venkat, P.; Seyfried, D.; Chopp, M.; Yan, T.; Chen, J. Brain-heart interaction: Cardiac complications after stroke. Circ. Res. 2017, 121, 451–468. [Google Scholar]
- Kato, Y.; Takeda, H.; Furuya, D.; Deguchi, I.; Tanahashi, N. Takotsubo cardiomyopathy and cerebral infarction. Rinsho Shinkeigaku 2009, 49, 158–166. [Google Scholar]
- Sander, D.; Winbeck, K.; Klingelhöfer, J.; Etgen, T.; Conrad, B. Prognostic relevance of pathological sympathetic activation after acute thromboembolic stroke. Neurology 2001, 57, 833–838. [Google Scholar]
- Santoro, F.; Núñez Gil, I.J.; Arcari, L.; Vitale, E.; Martino, T.; El-Battrawy, I.; Guerra, F.; Novo, G.; Mariano, E.; Musumeci, B.; et al. Neurological Disorders in Takotsubo Syndrome: Clinical Phenotypes and Outcomes. J. Am. Heart Assoc. 2024, 13, e032128. [Google Scholar] [CrossRef] [PubMed]
- Navi, B.B.; Reiner, A.S.; Kamel, H.; Iadecola, C.; Okin, P.M.; Elkind, M.S.V.; Panageas, K.S.; Deangelis, L.M. Risk of arterial thromboembolism in patients with cancer. J. Am. Coll. Cardiol. 2017, 70, 926–938. [Google Scholar] [CrossRef] [PubMed]
- Sener, U.; Keser, Z. Ischemic stroke in patients with malignancy. Mayo Clin. Proc. 2022, 97, 2139–2144. [Google Scholar]
- Bang, O.Y.; Chung, J.W.; Lee, M.J.; Seo, W.K.; Kim, G.M.; Ahn, M.J. Cancer-related stroke: An emerging subtype of ischemic stroke with unique pathomechanism. J. Stroke 2020, 22, 1–10. [Google Scholar]
- Wilcox, N.S.; Amit, U.; Reibel, J.B.; Berlin, E.; Howell, K.; Ky, B. Cardiovascular disease and cancer: Shared risk factors and mechanisms. Nat. Rev. Cardiol. 2024, 21, 617–631. [Google Scholar]
- Dardiotis, E.; Zloizou, A.M.; Markoula, S.; Siokas, V.; Tsarouhas, K.; Tzanakakis, G.; Libra, M.; Kritsis, A.P.; Brotis, A.G.; Aschner, M.; et al. Cancer-associated stroke: Pathophysiology, detection and management. Int. J. Oncol. 2019, 54, 779–796. [Google Scholar] [CrossRef]
| Variable | No Readmission for Heart Disease (n = 3,115,850) | Readmission for Heart Disease (n = 75,440) | p-Value |
|---|---|---|---|
| Median age [IQR] (years) | 68 [58 to 78] | 73 [64 to 82] | <0.001 |
| Female | 49.0% | 51.1% | <0.001 |
| Weekend admission | 25.1% | 23.4% | <0.001 |
| Elective admission | 4.2% | 8.9% | <0.001 |
| ZIP income quartile | 0.075 | ||
| 0–25th | 29.7% | 30.1% | |
| 26–50th | 27.1% | 27.5% | |
| 51–75th | 24.1% | 23.2% | |
| 76–100th | 19.2% | 19.3% | |
| Primary expected payer | <0.001 | ||
| Medicare | 59.6% | 74.7% | |
| Medicaid | 11.6% | 8.5% | |
| Private insurance | 21.5% | 12.5% | |
| Self-pay | 4.2% | 1.9% | |
| No charge | 0.5% | 0.2% | |
| Other | 2.6% | 2.1% | |
| Nicotine dependence | 1.2% | 0.9% | <0.001 |
| Alcohol misuse | 3.2% | 2.1% | <0.001 |
| Obesity | 14.7% | 13.0% | <0.001 |
| Hypertension | 82.3% | 82.1% | 0.58 |
| Hypercholesterolemia | 58.0% | 53.4% | <0.001 |
| Diabetes mellitus | 38.2% | 43.6% | <0.001 |
| Previous myocardial infarction | 5.0% | 8.1% | <0.001 |
| Previous stroke | 29.4% | 24.2% | <0.001 |
| Peripheral vascular disease | 3.4% | 4.0% | <0.001 |
| Chronic kidney disease | 15.1% | 27.0% | <0.001 |
| Chronic lung disease | 14.8% | 21.1% | <0.001 |
| Liver failure | 0.4% | 0.5% | 0.008 |
| Cancer | 6.3% | 12.6% | <0.001 |
| Dementia | 10.6% | 13.3% | <0.001 |
| Rural hospital | 15.0% | 15.0% | 0.94 |
| Teaching hospital | 73.5% | 70.2% | <0.001 |
| Hospital bed size | <0.001 | ||
| Small | 16.2% | 17.9% | |
| Medium | 27.1% | 28.6% | |
| Large | 56.8% | 53.5% | |
| Palliative care | 2.7% | 1.4% | <0.001 |
| Length of stay | 3 [2 to 7] | 4 [2 to 6] | <0.001 |
| Cost | $11,319 [7045 to 21,309] | $10,687 [6563 to 18,712] | <0.001 |
| Variable | Odds Ratio (95% CI) | p-Value |
|---|---|---|
| Age (years) | 1.01 (1.01–1.02) | <0.001 |
| Elective | 1.94 (1.72–2.18) | <0.001 |
| Primary expected payer vs. Medicare | ||
| Private insurance | 0.76 (0.68–0.86) | <0.001 |
| Self-pay | 0.65 (0.51–0.82) | <0.001 |
| Other | 0.77 (0.60–0.98) | 0.035 |
| Obesity | 0.85 (0.76–0.94) | 0.003 |
| Hypertension | 0.83 (0.76–0.94) | <0.001 |
| Hypercholesterolemia | 0.74 (0.69–0.80) | <0.001 |
| Diabetes mellitus | 1.31 (1.22–1.41) | <0.001 |
| Previous myocardial infarction | 1.65 (1.46–1.87) | <0.001 |
| Previous stroke | 0.71 (0.65–0.77) | <0.001 |
| Chronic kidney disease | 1.70 (1.57–1.84) | <0.001 |
| Chronic lung disease | 1.33 (1.22–1.45) | <0.001 |
| Cancer | 2.90 (2.65–3.17) | <0.001 |
| Teaching hospital | 0.92 (0.86–1.00) | 0.046 |
| Hospital bed size vs. small | ||
| Large | 0.88 (0.80–0.96) | 0.006 |
| Palliative care | 0.41 (0.32–0.54) | <0.001 |
| Variable | Odds Ratio (95% CI) | p-Value |
|---|---|---|
| Age (years) | 1.04 (1.04–1.05) | <0.001 |
| Female | 0.93 (0.89–0.98) | 0.004 |
| Elective | 2.22 (2.05–2.41) | <0.001 |
| Primary expected payer vs. Medicare | ||
| Medicaid | 0.87 (0.77–0.97) | 0.012 |
| Private insurance | 0.77 (0.70–0.84) | <0.001 |
| Self-pay | 0.53 (0.42–0.66) | <0.001 |
| Smoking | 0.73 (0.54–0.97) | 0.033 |
| Hypertension | 0.83 (0.78–0.88) | <0.001 |
| Hypercholesterolemia | 0.79 (0.75–0.83) | <0.001 |
| Diabetes mellitus | 1.07 (1.02–1.13) | 0.008 |
| Previous myocardial infarction | 1.34 (1.22–1.48) | <0.001 |
| Previous stroke | 0.74 (0.70–0.79) | <0.001 |
| Chronic kidney disease | 1.35 (1.27–1.43) | <0.001 |
| Chronic lung disease | 1.27 (1.19–1.35) | <0.001 |
| Cancer | 1.75 (1.63–1.88) | <0.001 |
| Dementia | 0.91 (0.85–0.98) | 0.012 |
| Rural hospital | 0.88 (0.81–0.94) | <0.001 |
| Teaching hospital | 0.89 (0.85–0.94) | <0.001 |
| Hospital bed size vs. small | ||
| Large | 0.92 (0.86–0.98) | 0.013 |
| Palliative care | 0.32 (0.27–0.40) | <0.001 |
| Variable | Odds Ratio (95% CI) | p-Value |
|---|---|---|
| Age (years) | 1.01 (1.01–1.02) | <0.001 |
| Female | 1.08 (1.03–1.13) | 0.003 |
| Elective | 2.01 (1.85–2.19) | <0.001 |
| Income quartile vs. 0–25th | ||
| 26–50th | 0.93 (0.87–0.99) | 0.015 |
| 51–75th | 0.86 (0.80–0.91) | <0.001 |
| 76–100th | 0.83 (0.77–0.89) | <0.001 |
| Primary expected payer vs. Medicare | ||
| Private insurance | 0.65 (0.60–0.71) | <0.001 |
| Self-pay | 0.64 (0.54–0.76) | <0.001 |
| No charge | 0.58 (0.35–0.95) | 0.029 |
| Other | 0.74 (0.63–0.88) | 0.001 |
| Alcohol misuse | 0.79 (0.67–0.94) | 0.008 |
| Hypertension | 0.87 (0.80–0.93) | <0.001 |
| Hypercholesterolemia | 0.71 (0.67–0.74) | <0.001 |
| Diabetes mellitus | 1.53 (1.45–1.60) | <0.001 |
| Previous myocardial infarction | 1.86 (1.72–2.02) | <0.001 |
| Previous stroke | 0.76 (0.72–0.80) | <0.001 |
| Peripheral vascular disease | 1.25 (1.11–1.40) | <0.001 |
| Chronic kidney disease | 2.40 (2.28–2.53) | <0.001 |
| Chronic lung disease | 1.59 (1.50–1.68) | <0.001 |
| Liver failure | 1.56 (1.16–2.10) | 0.003 |
| Cancer | 1.44 (1.33–1.56) | <0.001 |
| Rural hospital | 0.90 (0.84–0.96) | 0.003 |
| Teaching hospital | 0.87 (0.82–0.91) | <0.001 |
| Hospital bed size vs. small | ||
| Medium | 0.91 (0.85–0.98) | 0.013 |
| Large | 0.87 (0.81–0.93) | <0.001 |
| Palliative care | 0.33 (0.26–0.41) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwok, C.S.; Qureshi, A.I.; Borovac, J.A.; Will, M.; Schwarz, K.; Hall, M.; Mann, P.; Holroyd, E.; Lip, G.Y.H. Readmissions for Cardiac Disease Within 30 Days of Hospitalization for Cerebral Infarction: An Evaluation of the Stroke–Heart Syndrome Using the Nationwide Readmission Database. J. Cardiovasc. Dev. Dis. 2025, 12, 116. https://doi.org/10.3390/jcdd12040116
Kwok CS, Qureshi AI, Borovac JA, Will M, Schwarz K, Hall M, Mann P, Holroyd E, Lip GYH. Readmissions for Cardiac Disease Within 30 Days of Hospitalization for Cerebral Infarction: An Evaluation of the Stroke–Heart Syndrome Using the Nationwide Readmission Database. Journal of Cardiovascular Development and Disease. 2025; 12(4):116. https://doi.org/10.3390/jcdd12040116
Chicago/Turabian StyleKwok, Chun Shing, Adnan I. Qureshi, Josip Andelo Borovac, Maximilian Will, Konstantin Schwarz, Mark Hall, Paul Mann, Eric Holroyd, and Gregory Y. H. Lip. 2025. "Readmissions for Cardiac Disease Within 30 Days of Hospitalization for Cerebral Infarction: An Evaluation of the Stroke–Heart Syndrome Using the Nationwide Readmission Database" Journal of Cardiovascular Development and Disease 12, no. 4: 116. https://doi.org/10.3390/jcdd12040116
APA StyleKwok, C. S., Qureshi, A. I., Borovac, J. A., Will, M., Schwarz, K., Hall, M., Mann, P., Holroyd, E., & Lip, G. Y. H. (2025). Readmissions for Cardiac Disease Within 30 Days of Hospitalization for Cerebral Infarction: An Evaluation of the Stroke–Heart Syndrome Using the Nationwide Readmission Database. Journal of Cardiovascular Development and Disease, 12(4), 116. https://doi.org/10.3390/jcdd12040116








