Abstract
The impact of atrial fibrillation (AF) on patients with chronic total occlusions (CTOs) at the national level remains unclear. In this study, we conducted a retrospective analysis of data from the National Inpatient Sample to assess the characteristics and in-hospital outcomes of patients with CTO based on the presence or absence of AF. Multiple logistic and linear regressions examined factors associated with AF and evaluated its impact on length of stay (LoS), cost, and mortality. The analysis included 480,180 patients diagnosed with CTO, with AF present in 28.0% of cases. Patients with CTOs and AF were older (median age 73 vs. 66 years, p < 0.001) and exhibited lower female representation (25.0% vs. 27.9%, p < 0.001). Factors most strongly associated with AF included previous heart failure (OR 1.98, 95% CI 1.92–2.05, p < 0.001), liver disease (OR 1.37, 95% CI 1.27–1.48, p < 0.001), and obesity (OR 1.25, 95% CI 1.20–1.30, p < 0.001). AF correlated with increased in-hospital mortality (OR 1.29, 95% CI 1.18–1.40, p < 0.001), ischemic stroke (OR 1.27, 95% CI 1.13–1.42, p < 0.001), and major bleeding (OR 1.38, 95% CI 1.30–1.46). Moreover, AF was associated with a longer LoS (coef 1.58, 95% CI 1.50 to 1.67, p < 0.001) and higher in-hospital costs (coef 6.22, 95% CI 5.81 to 6.63, p < 0.001). Patients with CTOs and AF were older and had more underlying health problems compared to patients without AF. The patients with AF have worse outcomes in terms of mortality, ischemic stroke, major bleeding, length of stay, and costs.
1. Introduction
Atrial fibrillation (AF) is the most common arrhythmia worldwide and is known to exert a significant influence on cardiovascular morbidity and mortality [1]. Coronary artery disease (CAD) is the most common cardiovascular disease worldwide, and both AF and CAD have similar risk factors, which creates a bidirectional relationship between the two conditions that often occur together [2]. Additionally, CAD and AF have overlapping pathophysiological foundations [3].
A chronic total occlusion (CTO) is one of the most extreme manifestations of CAD and is common in patients with chronic coronary syndromes [4]. Several studies indicate that CTOs are associated with poor outcomes and higher mortality rates in different populations with coronary artery disease due to various underlying mechanisms [5,6]. Consequently, in some patients, particularly those who are symptomatic and experience angina despite medical therapy, there is evidence to support the use of revascularization techniques to open chronic total coronary occlusion if imaging methods demonstrate viability and ischemia in the territory supplied by the CTO vessel [7,8,9,10].
Recently, the negative impact of AF on mortality in patients undergoing CTO-PCI has been reported [11,12]. However, due to the complex nature of the intervention and lack of high-quality evidence regarding percutaneous coronary revascularization, many patients are treated conservatively [13]. The impact of AF on patients with CTOs, regardless of their treatment path has not been subject to much investigation. In this manuscript, we describe our retrospective analysis of data from the National Inpatient Sample to evaluate the population with a diagnosis of CTO and determine the factors associated with AF and the outcomes associated with AF compared to those without AF.
2. Methods
This manuscript was prepared in accordance with the recommendations of the STROBE criteria. Institutional review board approval for the study was not required for analysis of data from that National Inpatient Sample.
2.1. Study Design and Dataset
We conducted a retrospective cohort study by analyzing hospital admission data from the NIS between 2016 and 2020. The NIS is the largest all-payer inpatient care database in the United States, which is produced by the Healthcare Cost and Utilization Project (HCUP) at the Agency for Healthcare Research and Quality (AHRQ). The NIS hospital admission data were obtained from approximately 20% of the samples of hospitals in the United States, which translates to 5 to 8 million hospital admissions from approximately 1000 hospitals. It contains more than 100 clinical and non-clinical variables, including diagnostic codes, procedure codes, patient demographics, and patient admission and discharge status. The data from the NIS can be weighted to generate national estimates.
Hospital admissions with a diagnosis of CTO were included in the analysis based on the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) primary diagnosis codes to identify the hospital admissions where patients were diagnosed with coronary CTO (I25.82). Hospital admissions for patients with ages less than 18 years and those with missing values for age, sex, and in-hospital mortality were excluded.
2.2. Variable Definition
Clinical comorbidity variables for each admission were determined based on the ICD-10 codes or data available in the NIS, as defined in Supplementary Table S1. The primary exposure variable of interest was atrial fibrillation or flutter (I48*). Additional demographic variables, including age, sex, race, primary expected payer, and income based on ZIP code, were collected. Also, comorbidities such as smoking, alcohol misuse, obesity, hypertension, hyperlipidemia, diabetes mellitus, previous myocardial infarction, previous stroke, previous heart failure, previous venous thrombosis/embolism, chronic lung disease, chronic kidney disease, liver disease, anemia, any cancer, and dementia were determined. Hospital variables, including elective admission, weekend admission, season of admission, rural or urban designation of hospital, and hospital bed size, were extracted. The main outcome was in-hospital mortality, and the secondary outcomes were in-hospital acute ischemic stroke, major bleeding, length of stay, and in-hospital cost. In order to explore the impact of the primary diagnosis, we used the first digit of the primary or first ICD-10 code to define the category for the reason for admission. We compared the unadjusted, adjusted for all variables except the category of the primary diagnostic code, and adjusted for all variables including the category of the primary diagnostic code. As the majority of admissions were for diseases of the circulatory system, we further divided this category into the most common 3-digit diagnoses. As a sensitivity analysis, the cohort was divided according to the cause for hospitalization, and the proportion of patients with and without AF, as well as the mortality in each group, was determined. A further analysis was performed to identify the impact of AF on mortality for patients with a primary diagnosis of NSTEMI (ICD-10 code I21.4), NSTEMI (ICD-10 codes I21.0, I21.1, I21.2, I21.3), heart failure (I50), and for patients with heart failure who received intra-aortic balloon pump (ICD-10 code 5A02210) and left ventricular assist device (ICD-10 codes 5A02116, 5A0211D, 5A02216, 5A0221D).
2.3. Statistical Analysis
Statistical analysis was performed on STATA 13.0 (College Station, TX, USA). Descriptive statistics were presented for the patient characteristics, hospital characteristics and outcomes stratified by the presence or absence of AF. For continuous variables, the median and interquartile range were presented, and the median test on Stata was used to determine if there were statistical differences between the group with and without AF. Categorical variables were described with percentages, and a Chi2 test was used for determining if there were differences for the group with AF. Multiple logistic regression was performed to identify the independent predictors of AF in CTOs, with patient demographics, hospital, comorbidities, and severity markers as candidate variables in the adjusted model. Multiple logistic regressions were used to determine the impact of AF on in-hospital mortality, ischemic stroke, and major bleeding after adjustments for baseline variables. Multiple linear regression was used to estimate the impact of AF on length of stay and cost with adjustments for baseline variables. A sensitivity analysis was performed, evaluating the impact of AF on outcomes for the subgroup of patients with CTO who underwent PCI.
3. Results
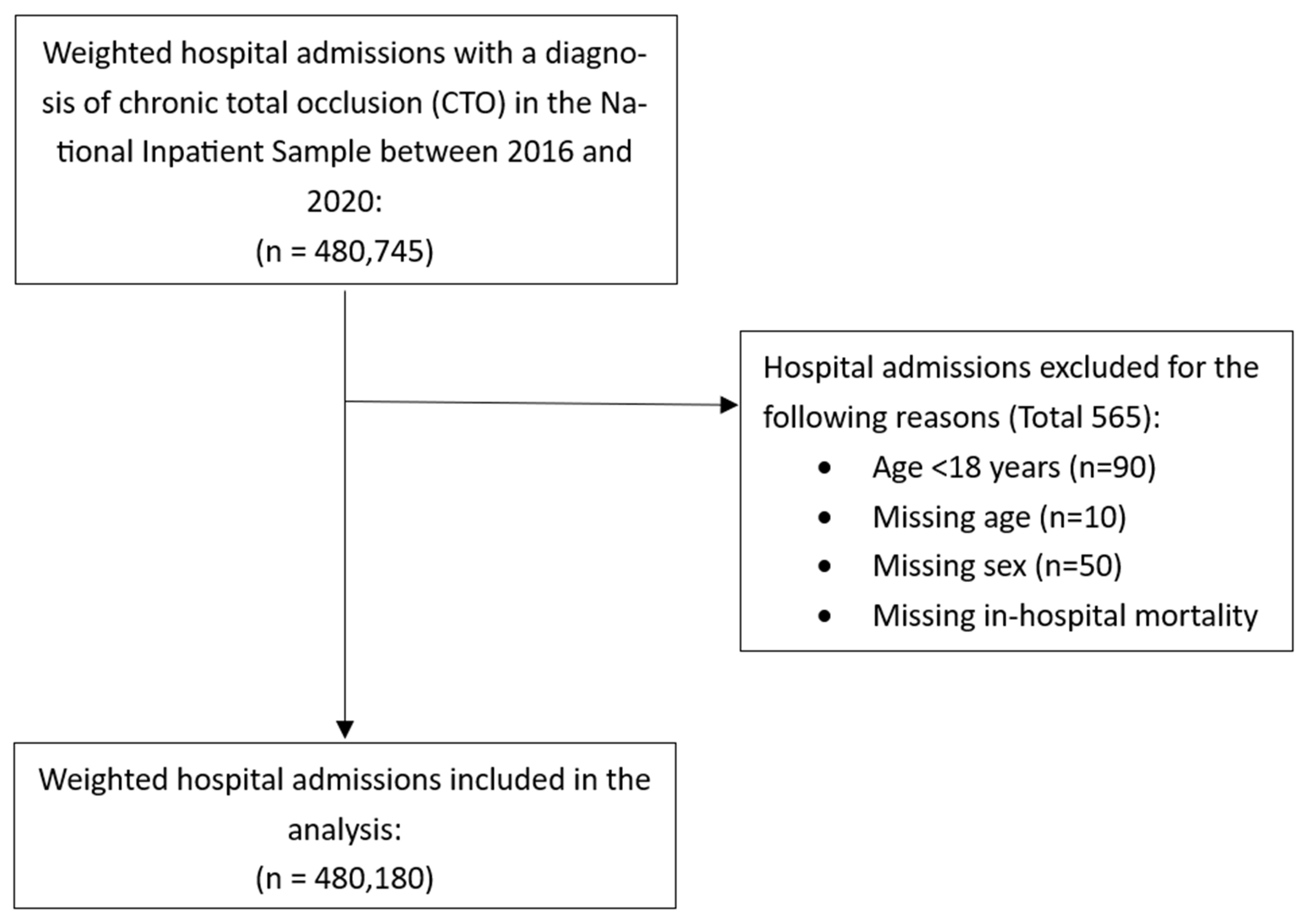
The process of identification of hospital admissions for patients with CTO is shown in Figure 1. There were a total of 480,180 hospital admissions included in the analysis with CTO.
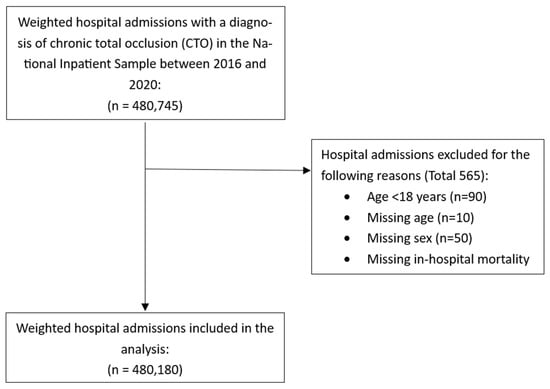
Figure 1.
Flow diagram of identification of hospital admission with atrial fibrillation and chronic total occlusions.
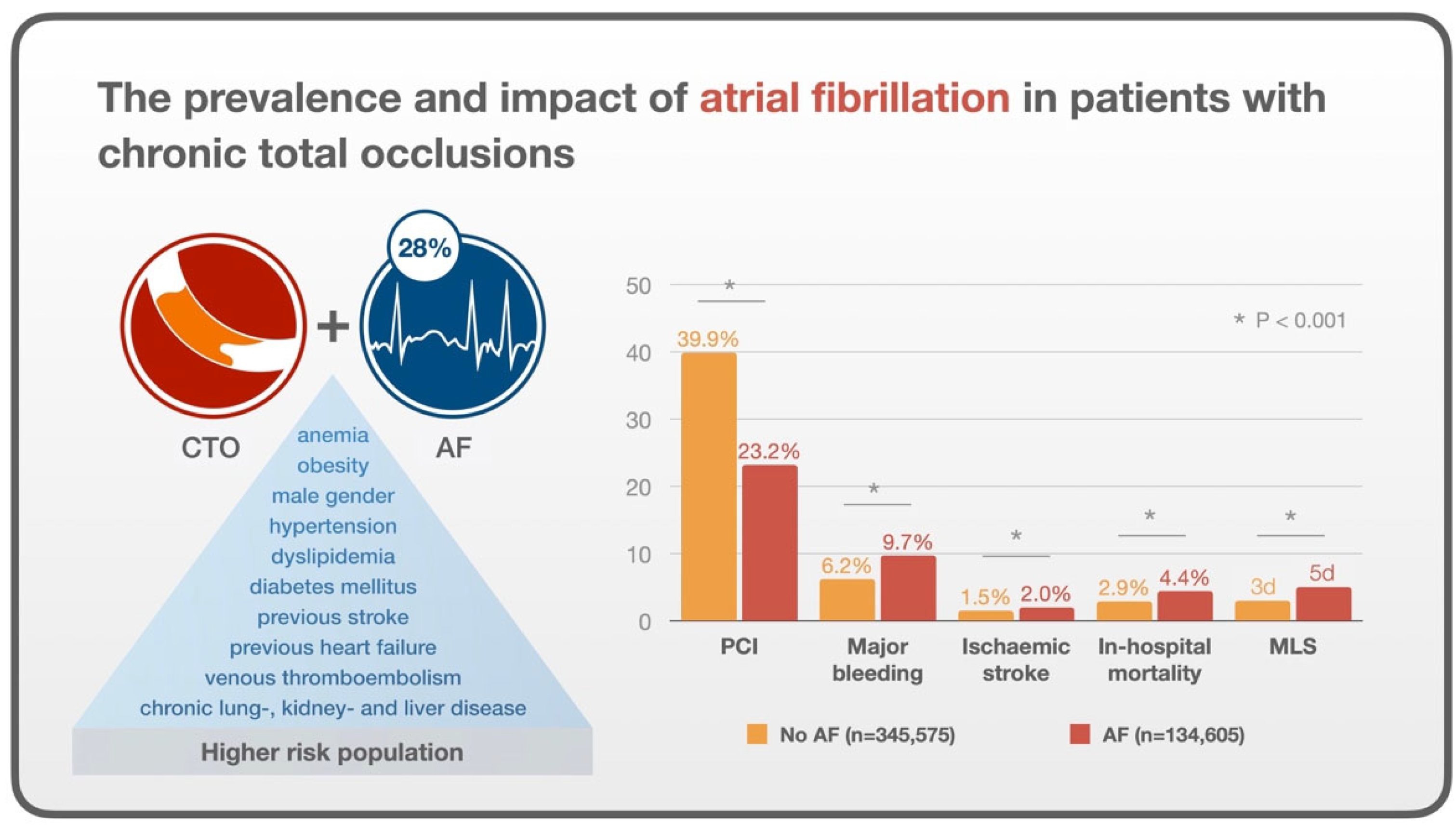
The characteristics of patients with CTOs were analyzed based on the presence or absence of atrial fibrillation. The results are presented in Table 1. There were 134,604 hospital admissions with AF (28.0%). The median age of patients with AF was significantly higher than those without AF (73 vs. 66 years, p < 0.001). Female representation was slightly lower in the AF group (25.0% vs. 27.9%, p < 0.001). Smoking and alcohol misuse was more prevalent in the group without AF compared to patients with AF (1.4% vs. 0.9%, p < 0.001 and 1.8% vs. 1.5%, p = 0.014, respectively). The prevalence of hypertension (90.7% vs. 86.9%, p < 0.001), previous myocardial infarction (31.5% vs. 29.6%, p < 0.001), previous stroke (14.1% vs. 11.5%, p < 0.001), previous heart failure (48.4% vs. 28.8%, p < 0.001), previous venous thromboembolism (5.0% vs. 3.9%, p < 0.001), chronic lung disease (31.4% vs. 24.7%, p < 0.001), chronic kidney disease (37.5% vs. 26.0%, p < 0.001), liver disease (5.1% vs. 3.9%, p < 0.001), anemia (10.2% vs. 7.8%, p < 0.001), and cancer (5.0% vs. 3.6%, p < 0.001) was higher in the AF group. Fewer patients had PCI (23.2% vs. 39.9%, p < 0.001).

Table 1.
Characteristics of patients with atrial fibrillation according to presence of chronic total occlusion.
In terms of crude outcomes, patients with AF had more major bleeding (9.7% vs. 6.2%, p < 0.001), ischemic stroke (2.0% vs. 1.5%, p < 0.001) and in-hospital mortality (4.4% vs. 2.9%, p < 0.001) compared to patients with CTO and no AF. The median hospital length of stay and in-hospital cost was also greater in the group with AF (5 vs. 3, p < 0.001 and USD 21,671 vs. USD 18,747, p < 0.001, respectively).
The results of the multiple logistic regression to evaluate the predictors of AF is shown in Table 2. Previous heart failure was the strongest factor associated with AF (OR 1.98 95% CI 1.92–2.05, p < 0.001). Other factors associated with increased odds of AF were liver disease (OR 1.37 95% CI 1.27–1.48, p < 0.001), obesity (OR 1.25 95% CI 1.20–1.30, p < 0.001), chronic kidney disease (OR 1.20 95% CI 1.16–1.24, p < 0.001), and hypertension (OR 1.17 95% CI 1.11–1.23, p < 0.001). Older age was associated with increased odds of AF (OR 1.05 95% CI 1.04–1.5, p < 0.001), but female sex was associated with reduced odds of AF (OR 0.75 95% CI 0.73–0.78, p < 0.001). Compared to white patients, patients who were black (OR 0.59 95% CI 0.55–0.62, p < 0.001), Native American (OR 0.60 95% CI 0.48–0.75, p < 0.001), and Hispanic (OR 0.62 95% CI 0.58–0.66, p < 0.001) were less likely to have AF.

Table 2.
Predictors of atrial fibrillation in patients with chronic total occlusions (n = 454,110).
Table 3 evaluates the odds of adverse outcomes and regression coefficients for length of stay and cost for AF in patients with CTO. AF was associated with an increase in in-hospital mortality (OR 1.29 95% CI 1.18–1.40, p < 0.001), ischemic stroke (OR 1.27 95% CI 1.13–1.42, p < 0.001), and major bleeding (OR 1.38 95% CI 1.30–1.46). It was also associated with longer length of stay (coef 1.58 days 95% CI 1.50 to 1.67, p < 0.001) and greater in-hospital cost (coef USD 6219 95% CI 5811 to 6627, p < 0.001). Sensitivity analysis for the subgroup of patients who underwent PCI showed even greater odds of in-hospital mortality (OR 1.55 95% CI 1.35–1.78, p < 0.001), ischemic stroke (OR 1.53 95% CI 1.19–1.96, p = 0.001), and major bleeding (OR 1.44 95% CI 1.26–1.64, p < 0.001) but slightly lower regression coefficients for length of stay (coef 1.47 95% CI 1.34 to 1.60, p < 0.001) and cost (5342 95% CI 4684 to 6000, p < 0.001).

Table 3.
Multivariable outcomes for patients with chronic total occlusion and atrial fibrillation.
The evaluation of the impact of AF on outcomes according to use of adjustments and consideration of the category of the first diagnostic code is shown in Supplementary Table S2. The effects of adjustments reduced the magnitude of the association between AF and outcome, but all associations showed increased in adverse events, length of stay, and cost with AF. To provide further clarity on the reasons for hospitalization, we conducted additional sensitivity analyses, categorizing patients based on the primary diagnosis. These findings are illustrated in Supplementary Tables S3–S5.
4. Discussion
Our study reports several key findings that are summarized in Figure 2. Firstly, patients who are hospitalized and found to have a diagnosis of CTO and concomitant AF were older and had more comorbidities as well as a greater rate of in-hospital ischemic stroke, major bleeding, and in-hospital mortality. Second, the greater comorbidity and poor outcomes are likely to have contributed to a greater length of stay and cost for the group with AF.
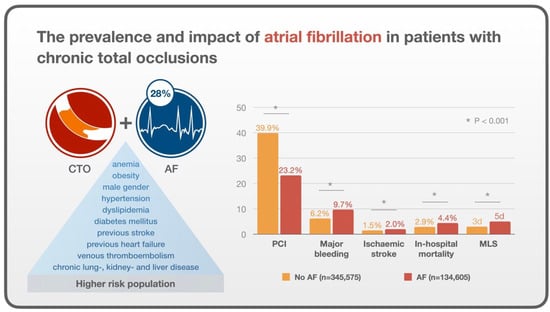
Figure 2.
Central illustration: The prevalence and impact of atrial fibrillation in patients with chronic total occlusions.
These findings suggest that patients with AF are a higher-risk group compared to patients without AF, and more studies are needed to know if AF itself a marker of risk or if it is the profile of the patient with AF that contributes to poor outcome. In addition, studies are needed to better understand the ideal management for patients with AF and CTO in order to minimize their risk, as these patients are at risk of ischemic stroke and bleeding, which may be related to antithrombotic use.
To the best of our knowledge, this is the first study to report the prevalence of AF in ‘all comer’ nationwide pool of patients with CTO, regardless of their further treatment path. Whereas two important RCTs [9,14] comparing revascularization versus optimal medical therapy in CTO are lacking information on the presence of AF, there are sparse registry data on the prevalence of AF in patients who underwent CTO PCI [11,12]. Alexandru et al. [11] report that 12% of patients with CTO PCI have AF too, which is comparable with a prior study of Staehli et al., who report a prevalence of 8.4% and with studies of patients undergoing non-CTO PCI [15,16]. A key finding in the current study is that it is more common than the rate reported in other studies, as more than 1 in 4 patients have AF.
The presence of AF in patients with CTOs in our cohort was associated with older age; male gender; obesity; hypertension; dyslipidemia; diabetes mellitus; previous stroke; previous heart failure and venous thromboembolism; chronic lung, kidney, and liver disease; and anemia. These common comorbidities associated with AF are widely recognized in the literature as contributors to the development of AF [17]. An important consideration is whether the AF directly contributes to poor outcomes in patients with CTO or if it is mediated by a more comorbid cohort, and it remains unclear the mechanisms for these poor outcomes. Evidently, our analysis revealed statistically significant differences across several variables. However, the clinical relevance of these differences requires careful consideration. For instance, the 0.8% difference in diabetes mellitus, while statistically significant, may have a negligible impact on clinical decision-making and patient outcomes in this setting. Similarly, the observed differences in the other variables, though notable, may not necessarily translate into meaningful changes in risk assessment or treatment interventions.
This cohort highlights the clinical complexity associated with AF, including frailty, multimorbidity, and polypharmacy [18,19,20]. Apart from stroke prevention and rhythm management, additional multidisciplinary preventive strategies, such as lifestyle modifications, might alleviate the burden of AF. This is aligned with current recommendations, for a holistic or integrated care approach to AF management [21], where improved clinical outcomes are seen by adherence to the Atrial fibrillation Better Care (ABC) pathway, including reductions in mortality, stroke, bleeding, and hospitalizations [22,23].
The treatment of AF with anticoagulation will shift the thrombotic-bleeding profile to that of increased risk of bleeding [24]. It is likely that the treatment of patients with CTO and AF needs to be individualized, with some having greater underlying bleeding risk where it may be acceptable to not have antithrombotic, while other patients have a greater thrombotic risk, thus supporting this use of anticoagulation [25,26].
The impact of AF on in-hospital outcomes following CTO PCI has been previously assessed by two studies, which found similar results. The first analyzed 2002 CTO PCIs performed in Germany between 2005 and 2013 and found higher periprocedural MACE with present AF (3.6% vs. 1.4%, p = 0.04) [12]. This finding was mainly driven by more frequently observed vascular access site complications and cardiac tamponade in patients with AF. The second study, by Alexandru et al. [11], showed no significant difference in procedural complications related to the presence of AF. One potential reason for the observed difference between both studies could be the growing utilization of radial access over time [26], given a decade gap between the analyzed time frames of the studies. Of note, the incidence of follow-up MACE and all-cause mortality was significantly higher in patients with AF in both studies. Our study supports these findings from a national American perspective but we were able to explore additional outcomes, such as ischemic stroke, bleeding, length of stay, and cost. How to minimize these adverse outcomes requires further studies.
In our cohort, AF among patients with CTOs was strongly associated with previous heart failure. This finding is aligned with Staehli et al. [12], reporting that AF was associated with reduced left ventricular systolic function in patients with CTOs. Mechanistically, AF can result in tachycardic or bradycardic left heart failure in patients with chronic total occlusions. However, patients with CTOs may also be more prone to develop heart failure as a consequence of increased left atrial pressure due to ischemia-related impairment of diastolic relaxation [3,26] or proarrhythmogenic scar tissue, raising a complex cause or effect question.
Our study suggests that major bleeding may play an important role in the high death rate among people with AF and CTOs. Naturally, when anticoagulation is required, bleeding complications are a logical concern. This risk is further heightened during PCI due to the potential for vascular access site complications, particularly with CTO-PCI [12].
Limitations
Our study has several limitations. The NIS is an observational dataset with inherent biases, such as risk of bias from confounding. There was no independent adjudication of the diagnosis of AF and clinical events, and there was no core laboratory assessment of the study angiograms. Data on anticoagulant use and long-term bleeding data were not available, as well as information regarding detailed coronary anatomy, viability, and follow-up mortality or MACE.
The study population comprises 345,575 individuals without AF and 134,605 with AF. While numerous variables demonstrate statistical significance, the associated percentage differences are negligible. This phenomenon likely stems from the substantial sample size, which enables the detection of minor discrepancies as statistically meaningful. This represents an important limitation of the present investigation, necessitating cautious interpretation of the results.
5. Conclusions
Patients with coronary CTOs and concomitant AF were older and had more comorbidities in comparison to patients without AF in the observed cohort. Moreover, AF was associated with a higher risk of periprocedural complications, in-hospital mortality, longer median length of stay, and increased costs. Even though the study found statistically significant differences in several clinical factors, the broader clinical significance of these findings remains unclear. Further research is warranted to determine whether CTO lesions have wider clinical relevance in patients with AF.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcdd12030100/s1, Table S1: Description of codes to the data analysis; Table S2: Impact of atrial fibrillation on outcomes for patients with chronic total occlusion according to level of adjustments, Table S3: Cause of admission according to primary diagnostic code, Table S4: Cause of admission sensitivity analysis, Table S5: Primary diagnosis of acute myocardial infarction sensitivity analysis.
Author Contributions
Conceptualization, M.W. and C.S.K.; methodology, C.S.K.; formal analysis, C.S.K.; data curation, C.S.K.; writing—original draft preparation, M.W.; writing—review and editing, K.S., E.H., T.W.W., J.M., J.A.B., G.Y.H.L., G.L. and A.I.Q.; visualization, G.L.; supervision, C.S.K.; project administration, M.W.; funding acquisition, M.W. All authors have read and agreed to the published version of the manuscript.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article. This research received funding for open access publication by the Karl Landsteiner University of Health Sciences, Dr. Karl-Dorrek-Straße 30, 3500 Krems, Austria.
Institutional Review Board Statement
This study utilized data from the National Inpatient Sample (NIS), which is a publicly available, de-identified dataset maintained by the Healthcare Cost and Utilization Project (HCUP) and the Agency for Healthcare Research and Quality (AHRQ). According to the guidelines set forth by the Department of Health and Human Services (HHS) and the Office for Human Research Protections (OHRP), research involving publicly available, de-identified data does not constitute human subjects research and is therefore exempt from Institutional Review Board (IRB) review.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data used in this study were obtained from the National Inpatient Sample (NIS), which is part of the Healthcare Cost and Utilization Project (HCUP) maintained by the Agency for Healthcare Research and Quality (AHRQ). The NIS dataset is available for purchase and access through HCUP’s online database.
Acknowledgments
The authors want to appreciate the contribution of NÖ Landesgesundheitsagentur, legal entity of University Hospitals in Lower Austria, for providing the organizational framework to conduct this research. The authors also would like to acknowledge support by Open Access Publishing Fund of Karl Landsteiner University of Health Sciences, Krems, Austria.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Go, A.S.; Hylek, E.M.; Phillips, K.A.; Chang, Y.C.; Henault, L.E.; Selby, J.V.; Singer, D.E. Prevalence of diagnosed atrial fibrillation in adults: National implications for rhythm management and stroke prevention: The AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001, 285, 2370–2375. [Google Scholar] [CrossRef] [PubMed]
- Michniewicz, E.; Mlodawska, E.; Lopatowska, P.; Tomaszuk-Kazberuk, A.; Malyszko, J. Patients with atrial fibrillation and coronary artery disease—Double trouble. Adv. Med. Sci. 2018, 63, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Mekhael, M.; Marrouche, N.; Hajjar AHEl Donnellan, E. The relationship between atrial fibrillation and coronary artery disease: Understanding common denominators. Trends Cardiovasc. Med. 2022, 34, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Fefer, P.; Knudtson, M.L.; Cheema, A.N.; Galbraith, P.D.; Osherov, A.B.; Yalonetsky, S.; Gannot, S.; Samuel, M.; Weisbrod, M.; Bierstone, D.; et al. Current Perspectives on Coronary Chronic Total Occlusions: The Canadian Multicenter Chronic Total Occlusions Registry. J. Am. Coll. Cardiol. 2012, 59, 991–997. [Google Scholar] [CrossRef]
- Godino, C.; Giannattasio, A.; Scotti, A.; Baldetti, L.; Pivato, C.A.; Munafò, A.; Cappelletti, A.; Beneduce, A.; Melillo, F.; Chiarito, M.; et al. Risk of cardiac and sudden death with and without revascularisation of a coronary chronic total occlusion. Heart 2019, 105, 1096–1102. [Google Scholar] [CrossRef]
- van der Schaaf, R.J.; Vis, M.M.; Sjauw, K.D.; Koch, K.T.; Baan, J., Jr.; Tijssen, J.G.; de Winter, R.J.; Piek, J.J.; Henriques, J.P. Impact of multivessel coronary disease on long-term mortality in patients with ST-elevation myocardial infarction is due to the presence of a chronic total occlusion. Am. J. Cardiol. 2006, 98, 1165–1169. [Google Scholar] [CrossRef]
- Park, T.K.; Lee, S.H.; Choi, K.H.; Lee, J.M.; Yang, J.H.; Song, Y.B.; Hahn, J.Y.; Choi, J.H.; Gwon, H.C.; Lee, S.H.; et al. Late Survival Benefit of Percutaneous Coronary Intervention Compared With Medical Therapy in Patients with Coronary Chronic Total Occlusion: A 10-Year Follow-Up Study. J. Am. Heart Assoc. 2021, 10, e019022. [Google Scholar] [CrossRef]
- Galassi, A.R.; Brilakis, E.S.; Boukhris, M.; Tomasello, S.D.; Sianos, G.; Karmpaliotis, D.; Di Mario, C.; Strauss, B.H.; Rinfret, S.; Yamane, M.; et al. Appropriateness of percutaneous revascularization of coronary chronic total occlusions: An overview. Eur. Heart J. 2016, 37, 2692–2700. [Google Scholar] [CrossRef]
- Werner, G.S.; Martin-Yuste, V.; Hildick-Smith, D.; Boudou, N.; Sianos, G.; Gelev, V.; Rumoroso, J.R.; Erglis, A.; Christiansen, E.H.; Escaned, J.; et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions cardiology. Eur. Heart J. 2018, 39, 2484–2493. [Google Scholar] [CrossRef]
- Brilakis, E.S.; Mashayekhi, K.; Tsuchikane, E.; Abi Rafeh, N.; Alaswad, K.; Araya, M.; Avran, A.; Azzalini, L.; Babunashvili, A.M.; Bayani, B.; et al. Guiding Principles for Chronic Total Occlusion Percutaneous Coronary Intervention: A Global Expert Consensus Document. Circulation 2019, 140, 420–433. [Google Scholar] [CrossRef]
- Alexandrou, M.; Rempakos, A.; Kostantinis, S.; Simsek, B.; Karacsonyi, J.; Choi, J.W.; Poommipanit, P.; Khatri, J.J.; Young, L.; Davies, R.; et al. Atrial fibrillation and chronic total occlusion percutaneous coronary intervention outcomes: Insights from the Progress-CTO registry. J. Invasive Cardiol. 2023, 35, 20–26. [Google Scholar] [CrossRef]
- Stähli, B.E.; Gebhard, C.; Gick, M.; Mashayekhi, K.; Ferenc, M.; Buettner, H.J.; Neumann, F.J.; Toma, A. Outcomes of patients with periprocedural atrial fibrillation undergoing percutaneous coronary intervention for chronic total occlusion. Clin. Res. Cardiol. 2017, 106, 986–994. [Google Scholar] [CrossRef] [PubMed]
- Råmunddal, T.; Hoebers, L.; Henriques, J.P.; Dworeck, C.; Angerås, O.; Odenstedt, J.; Ioanes, D.; Olivecrona, G.; Harnek, J.; Jensen, U.; et al. Chronic total occlusions in Sweden–a report from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR). PLoS ONE 2014, 9, e103850. [Google Scholar] [CrossRef]
- Lee, S.W.; Lee, P.H.; Ahn, J.M.; Park, D.W.; Yun, S.C.; Han, S.; Kang, H.; Kang, S.J.; Kim, Y.H.; Lee, C.W.; et al. Randomized Trial Evaluating Percutaneous Coronary Intervention for the Treatment of Chronic Total Occlusion: The DECISION-CTO Trial. Circulation 2019, 139, 1674–1683. [Google Scholar] [CrossRef]
- Shanmugasundaram, M.; Dhakal, B.P.; Murugapandian, S.; Hashemzadeh, M.; Paul, T.; Movahed, M.R. Outcomes of Patients with Atrial Fibrillation Undergoing Percutaneous Coronary Intervention Analysis of National Inpatient Sample. Cardiovasc. Revasc. Med. 2020, 21, 14–19. [Google Scholar] [CrossRef]
- Garg, L.; Agrawal, S.; Agarwal, M.; Shah, M.; Garg, A.; Patel, B.; Agarwal, N.; Nanda, S.; Sharma, A.; Cox, D. Influence of Atrial Fibrillation on Outcomes in Patients Who Underwent Primary Percutaneous Coronary Intervention for ST-Segment Elevation Myocardial Infarction. Am. J. Cardiol. 2018, 121, 684–689. [Google Scholar] [CrossRef]
- Chung, M.K.; Eckhardt, L.L.; Chen, L.Y.; Ahmed, H.M.; Gopinathannair, R.; Joglar, J.A.; Noseworthy, P.A.; Pack, Q.R.; Sanders, P.; Trulock, K.M. Lifestyle and Risk Factor Modification for Reduction of Atrial Fibrillation: A Scientific Statement From the American Heart Association. Circulation 2020, 141, e750–e772. [Google Scholar] [CrossRef]
- Grymonprez, M.; Petrovic, M.; De Backer, T.L.; Steurbaut, S.; Lahousse, L. The Impact of Polypharmacy on the Effectiveness and Safety of Non-vitamin K Antagonist Oral Anticoagulants in Patients with Atrial Fibrillation. Thromb. Haemost. 2024, 124, 135–148. [Google Scholar] [CrossRef]
- Zheng, Y.; Li, S.; Liu, X.; Lip, G.Y.H.; Guo, L.; Zhu, W. Effect of Oral Anticoagulants in Atrial Fibrillation Patients with Polypharmacy: A Meta-analysis. Thromb. Haemost. 2023, 122, 166–177. [Google Scholar] [CrossRef]
- Romiti, G.F.; Proietti, M.; Bonini, N.; Ding, W.Y.; Boriani, G.; Huisman, M.V.; Lip, G.Y.; GLORIA-AF Investigators. Clinical Complexity Domains, Anticoagulation, and Outcomes in Patients with Atrial Fibrillation: A Report from the GLORIA-AF Registry Phase II and III. Thromb. Haemost. 2022, 122, 2030–2041. [Google Scholar] [CrossRef]
- Chao, T.F.; Joung, B.; Takahashi, Y.; Lim, T.W.; Choi, E.K.; Chan, Y.H.; Guo, Y.; Sriratanasathavorn, C.; Oh, S.; Okumura, K.; et al. 2021 Focused Update Consensus Guidelines of the Asia Pacific Heart Rhythm Society on Stroke Prevention in Atrial Fibrillation: Executive Summary. Thromb. Haemost. 2022, 122, 20–47. [Google Scholar] [CrossRef] [PubMed]
- Romiti, G.F.; Pastori, D.; Rivera-Caravaca, J.M.; Ding, W.Y.; Gue, Y.X.; Menichelli, D.; Gumprecht, J.; Kozieł, M.; Yang, P.S.; Guo, Y.; et al. Adherence to the “Atrial Fibrillation Better Care” Pathway in Patients with Atrial Fibrillation: Impact on Clinical Outcomes—A Systematic Review and Meta-Analysis of 285,000 Patients. Thromb. Haemost. 2022, 122, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Romiti, G.F.; Guo, Y.; Corica, B.; Proietti, M.; Zhang, H.; Lip, G.Y.H. Mobile Health-Technology-Integrated Care for Atrial Fibrillation: A Win Ratio Analysis from the mAFA-II Randomized Clinical Trial. Thromb. Haemost. 2023, 123, 1042–1048. [Google Scholar] [CrossRef]
- Gorog, D.A.; Gue, Y.X.; Chao, T.F.; Fauchier, L.; Ferreiro, J.L.; Huber, K.; Konstantinidis, S.V.; Lane, D.A.; Marin, F.; Oldgren, J.; et al. Assessment and Mitigation of Bleeding Risk in Atrial Fibrillation and Venous Thromboembolism: Executive Summary of a European and Asia-Pacific Expert Consensus Paper. Thromb. Haemost. 2022, 122, 1625–1652. [Google Scholar] [CrossRef]
- Simsek, B.; Gorgulu, S.; Kostantinis, S.; Karacsonyi, J.; Alaswad, K.; Jaffer, F.A.; Doshi, D.; Goktekin, O.; Kerrigan, J.; Haddad, E.; et al. Radial access for chronic total occlusion percutaneous coronary intervention: Insights from the PROGRESS-CTO registry. Catheter. Cardiovasc. Interv. 2022, 100, 730–736. [Google Scholar] [CrossRef]
- Packer, M.; Lam, C.S.P.; Lund, L.H.; Redfield, M.M. Interdependence of Atrial Fibrillation and Heart Failure with a Preserved Ejection Fraction Reflects a Common Underlying Atrial and Ventricular Myopathy. Circulation 2020, 141, 4–6. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).