Abstract
(1) Background: As the burden of multimorbidity is increasing worldwide, little is known about its prevalence in Lithuania. We aimed to estimate the prevalence of chronic conditions and multimorbidity among Lithuanian adults and assess their impact on healthcare utilization. (2) Methods: A retrospective analysis of the Lithuanian National Health Insurance Fund database was performed in 2019. Multimorbidity was defined as having two or more chronic conditions. (3) Results: Of the Lithuanian population, 1,193,668 (51.5%) had at least one chronic condition, and 717,386 (31.0%) had multimorbidity. Complex multimorbidity (CM) was present in 670,312 (28.9%) patients, with 85.0% having complex cardiac multimorbidity (CCM) and 15.0% having complex non-cardiac multimorbidity (CNM). Multimorbidity increased with age, from 2% at age 18–24 to 77.5% at age 80 and above, and was more prevalent among women (63.3% vs. 36.7%, p < 0.001). One-third of multimorbid patients were hospitalized at least once per year, with half staying for a week or longer. CCM patients were more likely to be hospitalized, rehospitalized, and have more primary care visits (OR: 2.23, 1.60, 4.24, respectively, all p < 0.001). (4) Conclusions: Multimorbidity in Lithuania increases with age and affects women more. Chronic cardiovascular diseases contribute to a higher prevalence of multimorbidity and a more significant burden on the healthcare system.
1. Introduction
The World Health Organization (WHO) defines multimorbidity as the presence of at least two chronic diseases in one patient [1]. As the population ages, the occurrence of more than one chronic condition continues to rise, making multimorbidity a common phenomenon [2,3,4]. The prevalence of multimorbidity varies in the literature, depending on its definition, study designs, and patient characteristics [2,3]. The estimated pooled prevalence in meta-analyses ranges from 33.1% to 42.4%, with reported rates showing very high heterogeneity (ranging from 2.7% to 95.6%) [2,3,5]. Multimorbidity affects patients’ quality of life and mental well-being, leads to disability, and increases mortality rates [2,3,6]. It also places a burden on the healthcare system by increasing the number of outpatient visits, hospitalizations, and overall healthcare costs [3,5].
In the context of multimorbidity, cardiovascular diseases become increasingly important, as they are age-related and often diagnosed along with other diseases [7]. Approximately two-thirds of patients with cardiovascular disease are diagnosed with another chronic condition from the age of 70 [8,9]. The risk of developing a second or third cardiovascular disease is significantly higher than the risk of developing the first one [7]. The European Society of Cardiology highlights that multimorbid cardiovascular patients have been underrepresented in most clinical trials from which the guidelines have been derived and encourages the analysis of multimorbidity using registries and big data [8].
As the prevalence of chronic diseases grows, the single-disease-focused healthcare model becomes ineffective. Estimating the prevalence of chronic non-communicable diseases is essential to identify target population groups for intervention, optimize management strategies, and enable clinicians to provide high-quality care. The global heterogeneity in multimorbidity prevalence limits the use of this information as a universal standard across countries. There is a lack of research on this topic in Lithuania, with only one article published so far evaluating the prevalence of chronic diseases in 2014 [10]. As multimorbidity has increased over the past few decades, analyzing more recently available data on multimorbidity in Lithuania is essential.
We aimed: (1) to estimate the prevalence of chronic conditions and multimorbidity among Lithuanian adults in 2019, (2) to assess the prevalence of complex multimorbidity (CM), including complex cardiac multimorbidity (CCM), and (3) to evaluate the impact of complex cardiac and non-cardiac multimorbidity (CNM) on the utilization of healthcare resources.
2. Materials and Methods
2.1. Study Database
We performed a retrospective cohort study that analyzed the Lithuanian National Health Insurance Fund (NHIF) database. Since Lithuania mandates compulsory health insurance, the NHIF database contains a substantial part of the Lithuanian electronic health records. In 2018, the database consisted of 98% of the healthcare information of Lithuania’s population [11]. The data under analysis covers 1 January 2019 to 31 December 2019. These records include patients’ demographic data and disease diagnosis, as well as information about outpatient (primary care and specialist) and inpatient (hospitalizations) healthcare visits. All visits are linked to diagnosis codes from the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, and Australian Modification (ICD-10-AM).
The anonymous use of the NHIF database for research purposes was approved by the Biomedical Research Ethics Committee of the Vilnius Region (approval number: 2020/3-1207-692).
2.2. Study Cohort
We included adults aged 18 and older covered by Lithuanian mandatory health insurance in 2019 with at least one chronic disease from the list (Table 1). The patients’ age was determined based on their age in 2019.

Table 1.
The list of chronic conditions with ICD-10-AM diagnostic codes.
We identified patients as multimorbid according to the WHO’s accepted definition, which defines multimorbidity as two or more chronic diseases [1].
Since there is no universally accepted list of chronic conditions, we selected diseases according to Barnett et al. [6]. Barnett et al. highlighted the increasing prevalence of multimorbidity and its strong association with age and socioeconomic deprivation. The outlined set of diseases included hypertension, diabetes, coronary heart disease, depression, chronic obstructive pulmonary disease, and other conditions that form the core for analyzing multimorbidity, covering various medical specialties and having been previously used in other studies [10].
To evaluate the impact of cardiovascular diseases on the prevalence of multimorbidity, we categorized patients according to the complexity of multimorbidity: complex multimorbidity, complex cardiac multimorbidity, and complex non-cardiac multimorbidity. CM was defined as having two or more chronic diseases from at least two different medical specialties from the list (Table 1). CCM was defined as having two or more chronic diseases from at least two specialties, with cardiology as one of them. CNM included patients with two or more chronic diseases from at least two specialties, excluding cardiology.
The hospitalizations, length of stay, rehospitalizations (defined as hospital readmission within a period of up to 30 days), and outpatient visits (primary and specialists) were chosen to evaluate healthcare system utilization.
2.3. Statistical Analysis
Quantitative variables were reported as either the median with interquartile ranges or the mean with standard deviation (SD), depending on which better reflected the data’s variability. Categorical variables were presented as frequencies and percentages. The Pearson’s chi-square, Mann–Whitney U, and Kruskal–Wallis tests were used for group comparisons.
Given that the healthcare utilization outcomes were non-normally distributed variables with excessive zeros (indicating a large number of persons not using healthcare resources), two-part hurdle models were used to assess the association between multimorbidity or the number of chronic conditions and healthcare service utilization (e.g., the annual frequency of hospitalizations per person or the number of specialist visits per person per year). Hurdle models consist of two regression equations: the probability of observing non-zero outcomes (logit model) and the count of non-zero outcomes (negative binomial regression). The truncated negative binomial models were used where zero values were impossible—such as the total annual length of stay for hospitalized individuals.
The results of the hurdle models were presented as odds ratios (OR), which indicate the relationship between multimorbidity or the number of chronic conditions and the likelihood of having healthcare utilization, as well as incidence rate ratios (IRR), which reflect the change in the rate of healthcare utilization associated with multimorbidity or with the number of chronic conditions. IRRs were reported for truncated models, as these models do not include zero counts.
The population prevalence of chronic diseases was calculated using variables from official demographic data provided by the State Data Agency (Statistics Lithuania) at the Lithuanian Open Data Portal [12]. Statistical analysis was performed using R (version 4.4.1) [13], packages pscl [14,15].
The results were considered statistically significant if the p-value was less than 0.05.
3. Results
3.1. Study Cohort Characteristics
In 2019, the study database included 1,193,668 patients with at least one chronic condition, representing 51.5% of all individuals registered in Lithuania at that time, according to data from the State Data Agency (Table 2). The average patient’s age was 60 ± 16 years. The majority of the Lithuanian population were women, who also had a higher prevalence of at least one chronic condition (723,784 (60.6%) women vs. 469,884 (39.4%) men, p < 0.001).

Table 2.
The prevalence of at least one chronic disease by gender and age groups in the general population.
3.2. The Prevalence of Chronic Conditions and Their Impact on Healthcare Utilization
The number of patients with one chronic disease increased with age, varying from 13.3% in the 18–24 age group to 95.2% among individuals 80 years old and older (p < 0.001). The prevalence and number of chronic conditions based on gender and different age groups are shown in Figure 1.
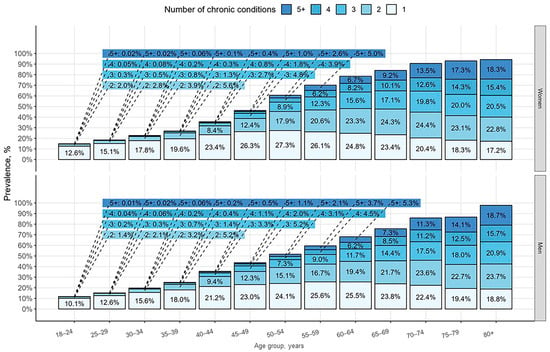
Figure 1.
The prevalence and number of chronic conditions by age and gender groups in the general population.
When patients were grouped based on the number of chronic conditions, 39.9% had one chronic condition, while only 8.8% were diagnosed with five or more chronic conditions (p < 0.001) (Table 3). The proportion of women increases from 56.7% to 67.4%, while men decrease from 43.3% to 32.6% as the number of diseases rises (from one to five and more) (p < 0.001). Patients with more chronic diseases were older, with an average age of 71 ± 11 years among those with five or more chronic conditions (p < 0.001).

Table 3.
Characteristics and healthcare resource utilization based on the number of chronic conditions.
Healthcare resource utilization analysis showed that a quarter of the study population (296,237 (24.8%)) was hospitalized at least once during the year, and 50.7% of these hospitalizations lasted longer than a week (Table 3). Comparing patients with different numbers of diseases, patients with five or more conditions had the most prolonged hospital stays (14.62 ± 15.34, p < 0.001), and a greater proportion of these patients required more than seven bed days (39,408 (70.4%), p < 0.001). An increase in the number of conditions was associated with more patients requiring rehospitalizations (13,001 (23.2%) patients with five or more diseases vs. 7809 (10.4%) patients with one disease, p < 0.001). The numbers of specialist visits were also more frequent in five and more chronic diseases group compared to one (15.30 ± 9.80 vs. 6.74 ± 5.62; 12.23 ± 9.81 vs. 4.32 ± 5.25, respectively, all p < 0.001).
Regression models were used to comprehensively analyze healthcare utilization across groups with different numbers of chronic diseases (Table S1). The odds of having any hospitalization, rehospitalization, or specialist visits increased with the number of chronic conditions. Patients with five or more diseases were 5.84 times more likely (95% CI: 5.75, 5.93, p < 0.001) to be hospitalized and had 2.89 (95% CI: 2.82, 2.97, p < 0.001) times higher hospitalization rate compared with the reference group (patients having one chronic disease). Patients with five or more diseases also had 2.04 times longer (95% CI: 2.00, 2.08, p < 0.001) hospitalizations. Compared to patients with one chronic condition, those with two, three, four, and five or more conditions were from 1.15 to 2.58 times more likely to be rehospitalized (p < 0.001). Furthermore, patients with five or more diseases were 7 times more likely (95% CI: 6.42, 7.64, p < 0.001) to have primary healthcare visits and 9.79 times more likely (95% CI: 9.52, 10.1, p < 0.001) to have specialist visits.
3.3. The Prevalence of Multimorbidity and Its Impact on Healthcare Utilization
In the Lithuanian population, 717,386 patients (31.0%) had multimorbidity, and 670,312 (28.9%) were classified as having CM (Table 4). Among patients with CM, 85.0% had CCM, while 15.0% presented with CNM. The mean age of patients with two or more chronic conditions was 65 ± 14 years. Multimorbidity was more prevalent among women than men (453,785 (63.3%) vs. 263,601 (36.7%). A higher proportion of women than men were diagnosed with both CCM and CNM (362,274 (63.6%) vs. 207,458 (36.4%) and 66,219 (65.8%) vs. 34,361 (34.2%), respectively, p < 0.001). A significantly higher age was observed among multimorbid patients with cardiovascular diseases (67 ± 13 years in CCM vs. 55 ± 15 in CNM, p < 0.001).

Table 4.
Characteristics and healthcare resource utilization based on the complexity of multimorbidity.
The prevalence of multimorbidity in the Lithuanian population by age group and gender is shown in Figure 2. As illustrated, women consistently demonstrate higher prevalence rates of chronic conditions compared to men across all age groups and multimorbidity types. The disparity between women and men was particularly pronounced between the ages of 55 and 79 across all multimorbidity groups, except CNM. The prevalence of CNM was less age-dependent than that of CCM.

Figure 2.
Prevalence of multimorbidity in the Lithuanian population by age groups and gender.
The prevalence of multimorbidity increased significantly with age, starting from 2.0% in the youngest age group (18–24 years) and peaking at 77.5% in individuals aged 80 years and older. In contrast, the prevalence of individuals with only one chronic condition peaked in middle-aged adults (55–59 years at 25.9%) and declined in the older population. A shift between one chronic condition and multimorbidity occurred around the age of 50–54, where multimorbidity surpassed one chronic condition, becoming the dominant pattern in older populations.
The utilization of healthcare resources was also assessed among multimorbidity groups (Table 4 and Table 5). It was revealed that one-third of multimorbid patients (221,017 (30.8%)) experienced at least one hospitalization per year, while half of them (123,729 (56.0%)) were hospitalized for a week or longer. When comparing CCM and CNM, the number of patients hospitalized per year was significantly higher in the CCM group (180,881 (31.7%) vs. 27,199 (27.0%), p < 0.001).

Table 5.
The hurdle negative binomial regression and truncated negative binomial models for healthcare utilization with multimorbidity group as a covariate.
Interestingly, within the CCM group, more patients were hospitalized for a week or longer (104,205 (57.6%) vs. 12,825 (47.2%), p < 0.001), whereas in the CNM group, more patients had 1–3 bed days per year (48,205 (26.7%) vs. 10,143 (37.3%), p < 0.001). Applying hurdle models to five outcomes revealed that both cardiac and non-cardiac multimorbidity groups showed significantly increased healthcare utilization compared to individuals with a single disease. The CCM patients demonstrated slightly higher hospitalization odds (OR 2.23 vs. 1.96) and frequency rates (IRR 1.75 vs. 1.67) compared to CNM. The CCM patients were 1.6 times more likely to be rehospitalized, with a 12% higher rehospitalization rate compared with CNM patients. In contrast, although CNM patients had slightly lower odds of rehospitalization (1.47 times more likely), their rehospitalization rates were significantly higher, increasing by 56.0%. In addition, the CCM group had higher odds (OR 4.24, 95% CI: 4.09, 4.39) of having primary healthcare visits and a higher number of visits rate (IRR 1.75, 95% CI: 1.75, 1.76). Specialist visits were 5.89 times more likely (95% CI: 5.73, 6.05) and 1.94 times more frequent (95% CI: 1.92, 1.95) among non-cardio patients.
4. Discussion
We conducted a retrospective Lithuanian population cohort study to evaluate the prevalence of chronic conditions and multimorbidity and to assess their burden on the healthcare system using data from the Lithuanian NHIF database. The study concluded that: (1) in Lithuania, 51.5% of patients have at least one chronic disease, and 31.0% suffer from multimorbidity; (2) multimorbidity increases with age, is more prevalent among women and is associated with increased likelihood of hospitalizations, rehospitalizations and higher amount of primary care visits than a reference group with single chronic disease.
4.1. The Rising Prevalence of Multiple Chronic Conditions
Evaluating the prevalence of chronic conditions is essential for a greater understanding of patients with long-term illnesses in the ageing world. This knowledge enhances patient management, reduces mortality, optimizes healthcare organization, and lowers healthcare costs [2,3]. Until now, in Lithuania, only one study has assessed the prevalence of chronic diseases, covering the period from January 2012 to June 2014 [10]. In that study, the overall multimorbidity prevalence was 16.3%; in contrast, our study found a significantly higher prevalence of 31.0%. This difference may indicate rising rates of chronic diseases in Lithuania, aligning with global trends. Due to advances in medical care and better survival rates, the global rise in multimorbidity has been observed since 2000 and stabilized between 2011 and 2021 [3]. Despite the increasing prevalence of multimorbidity, higher levels of disease accumulation remain relatively uncommon. We found that the proportion of affected patients decreases as the number of diseases rises. In our study, 26.1% of patients had two chronic diseases, while only a small proportion had five or more (8.8%). Similar results were reported by Pefoyo et al., where 12.3% of patients were diagnosed with two chronic diseases vs. 2.7% of patients with five or more [16].
Comparing multimorbidity prevalence with other studies is challenging due to methodological differences. However, comparisons can be made with global research that summarizes the literature. A recent systematic review and meta-analysis by Chowdhury et al. found an overall prevalence of multimorbidity of 37.2% [3]. Our study identified a slightly lower prevalence rate. We found that 31.0% of Lithuanians in 2019 had at least two conditions of 31 chronic diseases listed for the study. This difference may result from coding practices in our healthcare system, which prioritizes recording only those conditions that require active treatment, further testing, or specialist care. A higher prevalence of chronic diseases is observed in regions with private health insurance and payment systems depending on the diagnosis code [5]. Furthermore, our multimorbidity cohort was older than in Chowdhury’s study, with an average age of 56.95 ± 10.85 years compared to 65 ± 14 years in our cohort. As age is a well-established risk factor for multimorbidity, the lower prevalence of chronic diseases in the older age cohort may be attributed to unrecording. Nguyen et al. conducted a systematic review and meta-analysis and reported a pooled prevalence of multimorbidity at 33.1% [2]. In this study, the prevalence of multimorbidity was more similar to our findings. However, they included a more significant proportion of studies from low- and middle-income countries, associated with lower prevalence rates. For the high-income countries, the overall prevalence of 37.9% was slightly higher than what we observed. While, in comparison with regional studies, a similar prevalence of multimorbidity has also been reported in Estonia, where rates of at least one chronic condition were 49.1%, and two and more were 30.1% [17].
It is well known that the prevalence of multimorbidity varies by age and gender [2,3,4,5,6,10,18,19,20]. In line with the literature, we found that chronic diseases increased with age [21]. Middle-aged adults tend to visit hospitals more frequently, while older adults are challenged to access healthcare facilities regularly due to cognitive decline and physical limitations [22]. They also often present with overlapping or atypical symptoms. These barriers complicate the diagnostic process and delay timely treatment in older age groups [23,24]. Similar to findings in the literature, we observed that by age 65, more than half of our study population had at least two chronic conditions [2,17], while 80% of patients had at least one chronic condition [16]. Considering that individuals aged 65 and older account for about one-fifth of the population in Europe, this highlights the substantial healthcare burden posed by chronic diseases [25].
According to the literature, chronic conditions are noticeably more common among women [3,18,19,23,26]. This trend was observed in our study, as women showed a higher prevalence of at least one chronic condition (60.6% vs. 39.4%, p < 0.001), as well as multimorbidity (63.3% vs. 36.7% p < 0.001). It is suggested that the prevalence of chronic diseases among women is influenced by risk factors such as low physical activity and being overweight [27]. However, it is well known that women are more likely to seek medical help and report health issues [21,28,29]. We found that as the number of diseases increases (from one to five and more) the proportion of women grows from 56.7% to 67.4%. Since the life expectancy among Lithuanian women is higher (in 2019, 81 years vs. 71.5 years in men) [30], this may also reflect a more active role of women in using healthcare resources, leading to a higher number of chronic diseases.
4.2. Cardiovascular Diseases Impact on Prevalence of Multimorbidity
Our study showed that the prevalence of CCM is higher than CNM. We found that 85.0% of patients had multimorbidity involving at least one cardiovascular condition. Heart diseases have been identified as one of the most common initial diagnoses among patients who subsequently develop multimorbidity [29,31]. Moreover, studies investigating the structure of multimorbidity define hypertension as a predominant condition [4,16,32,33,34]. Since cardiovascular diseases often develop at an early age, and cardiology patients are more likely to seek active treatment by visiting healthcare specialists and participating in preventive programs, this results in a higher number of additional diagnoses [18]. Cardiovascular diseases remain the leading cause of morbidity and mortality worldwide [35]. It is evidenced that the development of cardiovascular disease in multimorbid patients leads to poorer prognosis [36,37]. Lawson et al., using data from 10,575 patients in the Swedish Heart Failure Registry, found that non-cardiovascular comorbidities were associated with much higher overall symptom burdens and more severe symptoms than cardiovascular comorbidities [38]. The literature analyses cardiovascular multimorbidity (with at least two cardiovascular diseases) [36], whereas we analyzed CCM (with one cardiovascular and another non-cardiac condition), demonstrating that even a single cardiovascular disease can contribute to a higher prevalence of multimorbidity. While two or more cardiovascular diseases facilitate disease management due to similar pathophysiological mechanisms, clinical decisions become more complicated with complex multimorbidity [16].
We also observed gender differences in CCM. In our cohort, more women than men were attributed to this multimorbidity subgroup (63.6% women vs. 36.4% men). Similarly, Tisminetzky et al. found that women were more prevalent in mixed multimorbidity groups (≥2 cardiovascular and ≥1 non-cardiovascular comorbidities) compared to men [39]. Increasing evidence highlights gender disparities in cardiovascular diseases. Studies show that cardiovascular diseases tend to develop 7–10 years later in women than in men, making women more vulnerable [40]. The first diagnosis of cardiovascular multimorbidity for women occurs at an average age of 73 [41]. In our study, patients with CCM were older than those in other multimorbidity groups, with a higher proportion of women in this group (multimorbidity 65 ± 14 years; CCM 67 ± 13 years; CNM 55 ± 15 years). This shows that older women not only face a growing prevalence of chronic conditions but also an increasing burden of cardiovascular diseases [42,43]. Identifying and targeting this multimorbidity subgroup’s prevention strategies could significantly improve patient care. A more detailed analysis of the structure of complex cardiac multimorbidity should be a focus of future research.
4.3. Healthcare Utilization
Reducing the burden associated with multiple chronic conditions remains a healthcare priority. It is well known that having more than one chronic disease increases the use of healthcare resources [18,21,39,44,45]. Our study revealed that more chronic conditions were associated with more frequent hospitalizations and rehospitalizations, extended hospital stays, and more primary and specialist visits. Furthermore, the odds of having any healthcare services increased with the number of chronic conditions. Buja et al. found that having more chronic diseases leads to a greater number of hospital admissions and a higher likelihood of spending more days in hospital per year [44]. In the study by Jankovic et al., more non-communicable chronic conditions were associated with a higher use of healthcare resources [19]. In contrast, in the study by Zhong et al., multimorbidity was the influencing factor [21].
It is suggested that not only the number of diseases but also the pattern may influence healthcare utilization [46]. Our study highlighted that multimorbidity with cardiovascular diseases is associated with a higher burden on the healthcare system. We found that the CCM group used more healthcare services such as hospitalizations and rehospitalizations and had longer hospital stays and more primary care visits. The specialist visits were more frequent among CNM patients. As patients with cardiovascular conditions experience more frequent disease exacerbations, accompanied by more prolonged and complicated hospitalizations, this may result in a lower number of specialist visits. This supports a study comparing multimorbidity phenotypes among patients with heart failure [47]. The study demonstrated that different multimorbidity patterns influence healthcare facility use, with the ‘malignant’ type of multimorbidity being linked to more prolonged hospitalizations and unplanned readmissions compared to less ‘malignant’ multimorbidity. Furthermore, it has already been shown that patients with myocardial infarction and non-cardiac comorbidities were more likely to have prolonged hospital stays compared to those without any non-cardiac comorbidities [37]. In addition, Canivell et al. revealed that multimorbid patients with myocardial infarction and non-cardiac conditions have a higher risk of experiencing recurrent cardiovascular events, with a rate of 12.78 per 100 person-years, compared to patients with only cardiovascular conditions, who have a rate of 7.79 per 100 person-years [36]. However, in that study, the highest risk was observed in patients with myocardial infarction and both cardiac and non-cardiac conditions with a rate of 20.45 per 100 person-years, indicating that multiple cardiovascular diseases along with non-cardiac conditions lead to poorer outcomes. As we see, the cardiovascular multimorbidity pattern leads to increasing healthcare needs. Therefore, in an ageing population with multimorbidity, disease management strategies should focus not only on single conditions but also on addressing coexisting comorbidities to optimize healthcare utilization.
4.4. Study Limitations
This study has some limitations. Our research used health administrative data, which covers a large part of the Lithuanian population and enables population-based analysis. However, the use of administrative data presents certain challenges. Firstly, coding practices may affect the data quality, resulting in overestimated or unreported conditions. Secondly, administrative data lack subjective information, such as patient status, type, and severity of symptoms. Lastly, the one-year study period limits the ability to observe long-term disease prevalence trends.
Additionally, multimorbidity research lacks a standardized methodology, a uniform multimorbidity definition, and a standard list of chronic conditions, which limits the ability to compare findings with other studies. Furthermore, we did not analyze the structure of multimorbidity to identify the high-burden conditions, which could be a focus of future research.
5. Conclusions
The prevalence of chronic conditions and multimorbidity in Lithuania is relatively high compared to global rates. It increases with age and is higher among women. As the population ages, the increase in multimorbidity leads to greater utilization of healthcare services. Cardiovascular diseases contribute to a higher prevalence of multimorbidity as well as a more significant burden on the healthcare system. Understanding the risks posed by rising rates of multiple chronic conditions is the crucial first step toward reducing their impact on the healthcare system and related expenditures.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcdd12020047/s1, Table S1: The hurdle negative binomial regression and truncated negative binomial models for healthcare utilization with number of diseases as covariate.
Author Contributions
Conceptualization, S.G.; methodology, D.R., R.P. and S.G.; formal analysis, R.P.; writing—original draft preparation, D.R.; writing—review and editing, D.R. and S.G.; visualization, R.P.; supervision, A.J. and S.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the Biomedical Research Ethics Committee of the Vilnius Region (approval number: 2020/3-1207-692).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data from this study are available from the Lithuania National Health Insurance Fund, but restrictions apply to the availability of these data, which were used under license for the current study and are not publicly available. The data are however available from the authors upon reasonable request and with the permission of the Lithuania National Health Insurance Fund.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. Multimorbidity. Available online: https://www.who.int/publications/i/item/9789241511650 (accessed on 13 December 2016).
- Nguyen, H.; Manolova, G.; Daskalopoulou, C.; Vitoratou, S.; Prince, M.; Prina, A.M. Prevalence of Multimorbidity in Community Settings: A Systematic Review and Meta-Analysis of Observational Studies. J. Comorbidity 2019, 9, 2235042X19870934. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, S.R.; Chandra Das, D.; Sunna, T.C.; Beyene, J.; Hossain, A. Global and Regional Prevalence of Multimorbidity in the Adult Population in Community Settings: A Systematic Review and Meta-Analysis. eClinicalMedicine 2023, 57, 101860. [Google Scholar] [CrossRef] [PubMed]
- Kone, A.P.; Mondor, L.; Maxwell, C.; Kabir, U.S.; Rosella, L.C.; Wodchis, W.P. Rising Burden of Multimorbidity and Related Socio-Demographic Factors: A Repeated Cross-Sectional Study of Ontarians. Can. J. Public Health 2021, 112, 737–747. [Google Scholar] [CrossRef] [PubMed]
- Ho, I.S.-S.; Azcoaga-Lorenzo, A.; Akbari, A.; Davies, J.; Hodgins, P.; Khunti, K.; Kadam, U.; Lyons, R.; McCowan, C.; Mercer, S.W.; et al. Variation in the Estimated Prevalence of Multimorbidity: Systematic Review and Meta-Analysis of 193 International Studies. BMJ Open 2022, 12, e057017. [Google Scholar] [CrossRef]
- Barnett, K.; Mercer, S.W.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of Multimorbidity and Implications for Health Care, Research, and Medical Education: A Cross-Sectional Study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef]
- Forman, D.E.; Maurer, M.S.; Boyd, C.; Brindis, R.; Salive, M.E.; Horne, F.M.; Bell, S.P.; Fulmer, T.; Reuben, D.B.; Zieman, S.; et al. Multimorbidity in Older Adults with Cardiovascular Disease. J. Am. Coll. Cardiol. 2018, 71, 2149–2161. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on Cardiovascular Disease Prevention in Clinical Practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Liu, J.; Ma, J.; Wang, J.; Zeng, D.D.; Song, H.; Wang, L.; Cao, Z. Comorbidity Analysis According to Sex and Age in Hypertension Patients in China. Int. J. Med. Sci. 2016, 13, 99–107. [Google Scholar] [CrossRef]
- Navickas, R.; Visockienė, Ž.; Puronaitė, R.; Rukšėnienė, M.; Kasiulevičius, V.; Jurevičienė, E. Prevalence and Structure of Multiple Chronic Conditions in Lithuanian Population and the Distribution of the Associated Healthcare Resources. Eur. J. Intern. Med. 2015, 26, 160–168. [Google Scholar] [CrossRef]
- Lithuania Country Health Profile 2019. The State of Health in the EU. Available online: https://Eurohealthobservatory.Who.Int/Publications/m/Lithuania-Country-Health-Profile-2019 (accessed on 14 November 2019).
- Lithuanian Open Data Portal. Number of Permanent Residents at the Beginning of the Year. Available online: https://data.gov.lt/datasets/2689/ (accessed on 18 June 2024).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2024; Available online: https://www.r-project.org/ (accessed on 29 December 2024).
- Jackman, S. Pscl: Classes and Methods for R Developed in the Political Science Computational Laboratory. R Package, version 1.5.9; University of Sydney: Sydney, Australia, 2024. Available online: https://github.com/atahk/pscl/ (accessed on 29 December 2024).
- Zeileis, A.; Kleiber, C.; Jackman, S. Regression Models for Count Data in R. J. Stat. Softw. 2008, 27, 1–25. Available online: http://www.jstatsoft.org/article/view/v027i08 (accessed on 29 December 2024). [CrossRef]
- Koné Pefoyo, A.J.; Bronskill, S.E.; Gruneir, A.; Calzavara, A.; Thavorn, K.; Petrosyan, Y.; Maxwell, C.J.; Bai, Y.; Wodchis, W.P. The Increasing Burden and Complexity of Multimorbidity. BMC Public Health 2015, 15, 415. [Google Scholar] [CrossRef] [PubMed]
- Jürisson, M.; Pisarev, H.; Uusküla, A.; Lang, K.; Oona, M.; Kalda, R. Prevalence of Chronic Conditions and Multimorbidity in Estonia: A Population-Based Cross-Sectional Study. BMJ Open 2021, 11, e049045. [Google Scholar] [CrossRef] [PubMed]
- Ji, E.; Ahn, S.; Choi, J.-Y.; Kim, C.-H.; Kim, K. Effect of Multimorbidity on Hypertension Management. Sci. Rep. 2023, 13, 18764. [Google Scholar] [CrossRef] [PubMed]
- Jankovic, J.; Mirkovic, M.; Jovic-Vranes, A.; Santric-Milicevic, M.; Terzic-Supic, Z. Association between Non-Communicable Disease Multimorbidity and Health Care Utilization in a Middle-Income Country: Population-Based Study. Public Health 2018, 155, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Kiliari, N.; Theodosopoulou, E.; Papanastasiou, E. Multimorbidity and Unmet Citizens’ Needs and Expectations Urge for Reforms in the Health System of Cyprus: A Questionnaire Survey. JRSM Open 2014, 5, 2042533313515860. [Google Scholar] [CrossRef]
- Zhong, Y.; Qin, G.; Xi, H.; Cai, D.; Wang, Y.; Wang, T.; Gao, Y. Prevalence, Patterns of Multimorbidity and Associations with Health Care Utilization among Middle-Aged and Older People in China. BMC Public Health 2023, 23, 537. [Google Scholar] [CrossRef]
- Lai, F.T.T.; Wong, S.Y.S.; Yip, B.H.K.; Guthrie, B.; Mercer, S.W.; Chung, R.Y.; Chung, G.K.K.; Chau, P.Y.K.; Wong, E.L.Y.; Woo, J.; et al. Multimorbidity in Middle Age Predicts More Subsequent Hospital Admissions than in Older Age: A Nine-Year Retrospective Cohort Study of 121,188 Discharged In-Patients. Eur. J. Intern. Med. 2019, 61, 103–111. [Google Scholar] [CrossRef]
- Zhang, X.; Padhi, A.; Wei, T.; Xiong, S.; Yu, J.; Ye, P.; Tian, W.; Sun, H.; Peiris, D.; Praveen, D.; et al. Community Prevalence and Dyad Disease Pattern of Multimorbidity in China and India: A Systematic Review. BMJ Glob. Health 2022, 7, e008880. [Google Scholar] [CrossRef]
- Jin, Y.; Liang, J.; Hong, C.; Liang, R.; Luo, Y. Cardiometabolic Multimorbidity, Lifestyle Behaviours, and Cognitive Function: A Multicohort Study. Lancet Healthy Longev. 2023, 4, e265–e273. [Google Scholar] [CrossRef]
- Global Age Distribution by Region 2023. Statista. Available online: https://www.statista.com/statistics/932555/Global-Population-by-Age-by-Continent/ (accessed on 11 July 2024).
- Saavedra-Moreno, C.; Hurtado, R.; Velasco, N.; Ramírez, A. Identification of Population Multimorbidity Patterns in 3.9 Million Patients from Bogota in 2018. Glob. Epidemiol. 2024, 8, 100171. [Google Scholar] [CrossRef]
- Keetile, M.; Navaneetham, K.; Letamo, G. Prevalence and Correlates of Multimorbidity among Adults in Botswana: A Cross-Sectional Study. PLoS ONE 2020, 15, e0239334. [Google Scholar] [CrossRef] [PubMed]
- López Ferreruela, I.; Obón Azuara, B.; Malo Fumanal, S.; Rabanaque Hernández, M.J.; Aguilar-Palacio, I. Gender Inequalities in Secondary Prevention of Cardiovascular Disease: A Scoping Review. Int. J. Equity Health 2024, 23, 146. [Google Scholar] [CrossRef] [PubMed]
- Kudesia, P.; Salimarouny, B.; Stanley, M.; Fortin, M.; Stewart, M.; Terry, A.; Ryan, B.L. The Incidence of Multimorbidity and Patterns in Accumulation of Chronic Conditions: A Systematic Review. J. Multimorb. Comorbidity 2021, 11, 26335565211032880. [Google Scholar] [CrossRef] [PubMed]
- WHO Mortality Database. Available online: https://Platform.Who.Int/Mortality/Countries/Country-Details/MDB/Lithuania?countryProfileId=b6fab8f3-9f75-4dd3-9cd0-B6aee45781fd (accessed on 22 January 2025).
- Sison, S.D.M.; Lin, K.J.; Najafzadeh, M.; Ko, D.; Patorno, E.; Bessette, L.G.; Zakoul, H.; Kim, D.H. Common Non-cardiovascular Multimorbidity Groupings and Clinical Outcomes in Older Adults with Major Cardiovascular Disease. J. Am. Geriatr. Soc. 2023, 71, 3179–3188. [Google Scholar] [CrossRef] [PubMed]
- Li, F.-R.; Wang, S.; Li, X.; Cheng, Z.-Y.; Jin, C.; Mo, C.-B.; Zheng, J.; Liang, F.-C.; Gu, D.-F. Multimorbidity and Mortality among Older Patients with Coronary Heart Disease in Shenzhen, China. J. Geriatr. Cardiol. 2024, 21, 81–89. [Google Scholar] [CrossRef]
- Ho, C.L.B.; Si, S.; Brennan, A.; Briffa, T.; Stub, D.; Ajani, A.; Reid, C.M. Multimorbidity Impacts Cardiovascular Disease Risk Following Percutaneous Coronary Intervention: Latent Class Analysis of the Melbourne Interventional Group (MIG) Registry. BMC Cardiovasc. Disord. 2024, 24, 66. [Google Scholar] [CrossRef]
- Tian, Y.; Li, D.; Cui, H.; Zhang, X.; Fan, X.; Lu, F. Epidemiology of Multimorbidity Associated with Atherosclerotic Cardiovascular Disease in the United States, 1999–2018. BMC Public Health 2024, 24, 267. [Google Scholar] [CrossRef]
- Mensah, G.A.; Fuster, V.; Murray, C.J.L.; Roth, G.A.; Mensah, G.A.; Abate, Y.H.; Abbasian, M.; Abd-Allah, F.; Abdollahi, A.; Abdollahi, M.; et al. Global Burden of Cardiovascular Diseases and Risks, 1990-2022. J. Am. Coll. Cardiol. 2023, 82, 2350–2473. [Google Scholar] [CrossRef]
- Canivell, S.; Muller, O.; Gencer, B.; Heg, D.; Klingenberg, R.; Räber, L.; Carballo, D.; Matter, C.; Lüscher, T.; Windecker, S.; et al. Prognosis of Cardiovascular and Non-Cardiovascular Multimorbidity after Acute Coronary Syndrome. PLoS ONE 2018, 13, e0195174. [Google Scholar] [CrossRef]
- Goldberg, R.; Chen, H.-Y.; Saczynski, J.; McManus, D.D.; Lessard, D.; Yarzebski, J.; Lapane, K. Gore the Impact of Cardiac and Noncardiac Comorbidities on the Short-Term Outcomes of Patients Hospitalized with Acute Myocardial Infarction: A Population-Based Perspective. Clin. Epidemiol. 2013, 5, 439–448. [Google Scholar] [CrossRef]
- Lawson, C.A.; Solis-Trapala, I.; Dahlstrom, U.; Mamas, M.; Jaarsma, T.; Kadam, U.T.; Stromberg, A. Comorbidity Health Pathways in Heart Failure Patients: A Sequences-of-Regressions Analysis Using Cross-Sectional Data from 10,575 Patients in the Swedish Heart Failure Registry. PLoS Med. 2018, 15, e1002540. [Google Scholar] [CrossRef] [PubMed]
- Tisminetzky, M.; Gurwitz, J.H.; Miozzo, R.; Gore, J.M.; Lessard, D.; Yarzebski, J.; Goldberg, R.J. Impact of Cardiac- and Noncardiac-Related Conditions on Adverse Outcomes in Patients Hospitalized with Acute Myocardial Infarction. J. Comorbidity 2019, 9, 2235042X19852499. [Google Scholar] [CrossRef] [PubMed]
- Suman, S.; Pravalika, J.; Manjula, P.; Farooq, U. Gender and CVD- Does It Really Matters? Curr. Probl. Cardiol. 2023, 48, 101604. [Google Scholar] [CrossRef] [PubMed]
- Suh, J.W.; Floud, S.; Reeves, G.K.; Cairns, B.J.; Wright, F.L. Multimorbidity of Cardiovascular Disease Subtypes in a Prospective Cohort of 1.2 Million UK Women. Open Heart 2023, 10, e002552. [Google Scholar] [CrossRef]
- Jin, L.; Guo, X.; Dou, J.; Liu, B.; Wang, J.; Li, J.; Sun, M.; Sun, C.; Yu, Y.; Yao, Y. Multimorbidity Analysis According to Sex and Age towards Cardiovascular Diseases of Adults in Northeast China. Sci. Rep. 2018, 8, 8607. [Google Scholar] [CrossRef]
- Tang, Z.; Wang, C.; Song, X.; Shi, J.; Mitnitski, A.; Fang, X.; Yu, P.; Rockwood, K. Co-Occurrence of Cardiometabolic Diseases and Frailty in Older Chinese Adults in the Beijing Longitudinal Study of Ageing. Age Ageing 2013, 42, 346–351. [Google Scholar] [CrossRef]
- Buja, A.; Rivera, M.; De Battisti, E.; Corti, M.C.; Avossa, F.; Schievano, E.; Rigon, S.; Baldo, V.; Boccuzzo, G.; Ebell, M.H. Multimorbidity and Hospital Admissions in High-Need, High-Cost Elderly Patients. J. Aging Health 2020, 32, 259–268. [Google Scholar] [CrossRef]
- Odland, M.L.; Ismail, S.; Sepanlou, S.G.; Poustchi, H.; Sadjadi, A.; Pourshams, A.; Marshall, T.; Witham, M.D.; Malekzadeh, R.; Davies, J.I. Multimorbidity and Associations with Clinical Outcomes in a Middle-Aged Population in Iran: A Longitudinal Cohort Study. BMJ Glob. Health 2022, 7, e007278. [Google Scholar] [CrossRef]
- Islam, M.M.; McRae, I.S.; Yen, L.; Jowsey, T.; Valderas, J.M. Time Spent on Health-related Activities by Senior Australians with Chronic Diseases: What Is the Role of Multimorbidity and Comorbidity? Aust. N. Z. J. Public Health 2015, 39, 277–283. [Google Scholar] [CrossRef]
- Chen, L.; Chan, Y.-K.; Busija, L.; Norekval, T.M.; Riegel, B.; Stewart, S. Malignant and Benign Phenotypes of Multimorbidity in Heart Failure: Implications for Clinical Practice. J. Cardiovasc. Nurs. 2019, 34, 258–266. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).