Coronary Artery Disease in Very Young Women: Risk Factors and Prognostic Insights from Extended Follow-Up †
Abstract
1. Introduction
2. Methods
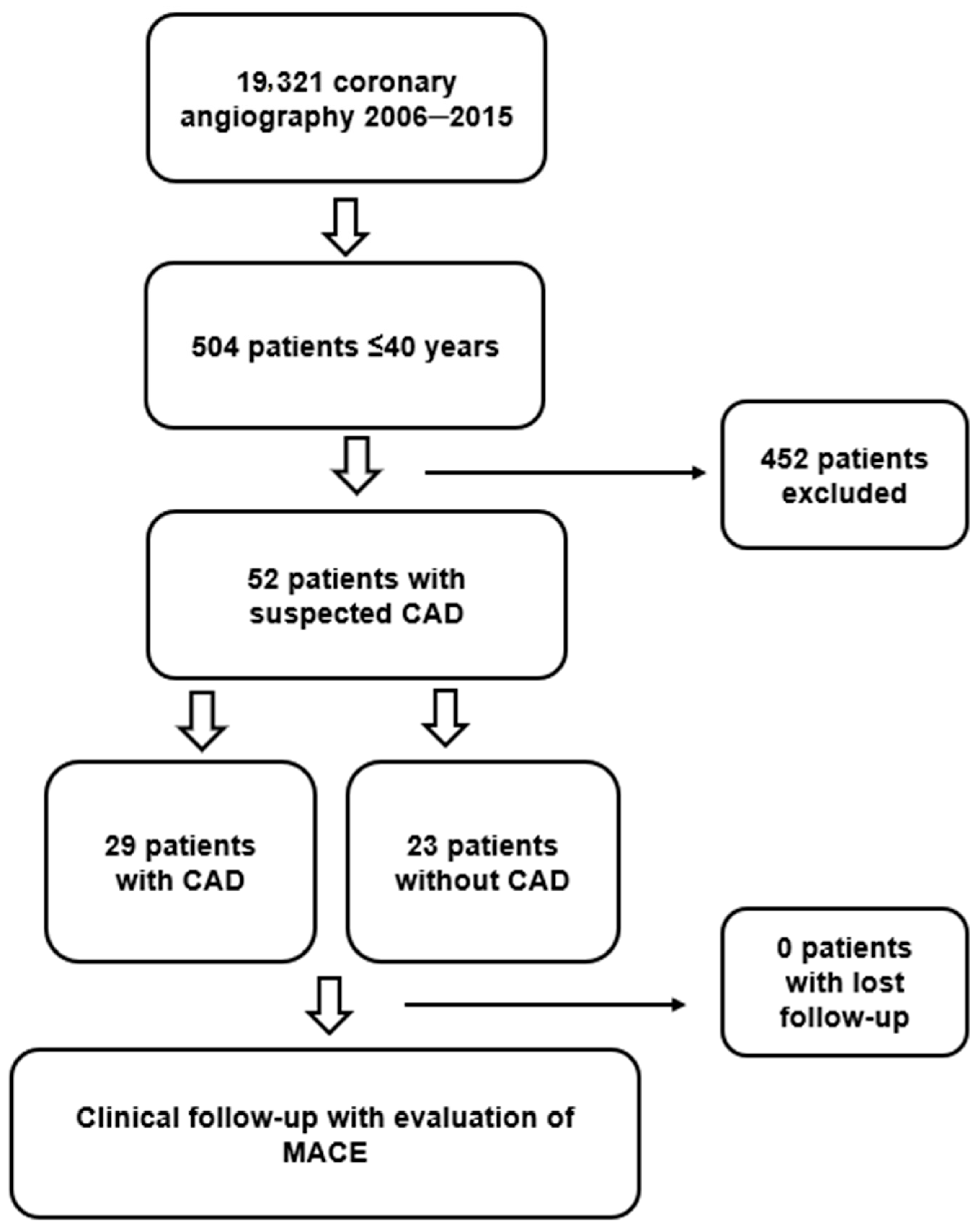
2.1. Design and Study Population
- Cases: Women aged between 18 and 40 years referred for coronary angiography due to suspicion of CAD based on signs or symptoms or a positive ischemia stress test. They must present at least one angiographically significant coronary stenosis (≥75% of the luminal diameter determined visually or ≥50% by quantitative coronary analysis; in the left main, stenosis ≥ 50% was considered a significant disease) or any positive invasive fractional flow reserve test in one or more epicardial vessels.
- Controls: Women aged between 18 and 40 years referred for coronary angiography due to suspicion of CAD based on signs or symptoms or a positive ischemia stress test but with non-diagnostic of CAD.
2.2. Data Collection and Definition of Variables
2.3. Ethical and Legal Aspects
2.4. Statistical Analysis
3. Results
Study Characteristics
4. Discussion
4.1. Factors Associated with Early CAD
4.2. Follow Up
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Beaton, A.Z.; Boehme, A.K.; Buxton, A.E.; et al. Heart Disease and Stroke Statistics—2023 Update: A Report from the American Heart Association. AHA ASA J. 2023, 148. [Google Scholar] [CrossRef]
- Singh, B.; Singh, A.; Goyal, A.; Chhabra, S.; Tandon, R.; Aslam, N.; Mohan, B.; Wander, G.S. The Prevalence, Clinical Spectrum and the Long Term Outcome of ST-Segment Elevation Myocardial Infarction in Young—A Prospective Observational Study. Cardiovasc. Revasc.Med. 2019, 20, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Trzeciak, P.; Gierlotka, M.; Poloński, L.; Gąsior, M. Treatment and Outcomes of Patients under 40 Years of Age with Acute Myocardial Infarction in Poland in 2009–2013 (Analysis from PL-ACS Registry). Pol. Arch. Intern. Med. 2017, 127, 666–673. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Prajapati, J.; Jain, S.; Virpariya, K.; Rawal, J.; Joshi, H.; Sharma, K.; Roy, B.; Thakkar, A. Novel Atherosclerotic Risk Factors and Angiographic Profile of Young Gujarati Patients with Acute Coronary Syndrome. J. Assoc. Physicians India 2014, 62, 584–588. [Google Scholar] [PubMed]
- Morillas, P.; Bertomeu, V.; Pabón, P.; Ancillo, P.; Bermejo, J.; Fernández, C.; Arós, F. Characteristics and Outcome of Acute Myocardial Infarction in Young Patients: The PRIAMHO II Study. Cardiology 2006, 107, 217–225. [Google Scholar] [CrossRef]
- Andrés, E.; León, M.; Cordero, A.; Magallón Botaya, R.; Magán, P.; Luengo, E.; Alegría, E.; Casasnovas, J.A. Factores de riesgo cardiovascular y estilo de vida asociados a la aparición prematura de infarto agudo de miocardio. Rev. Española Cardiol. 2011, 64, 527–529. [Google Scholar] [CrossRef] [PubMed]
- Esteban, M.R.; Montero, S.M.; Sánchez, J.J.A.; Hernández, H.P.; Pérez, J.J.G.; Afonso, J.H.; Pérez, D.C.R.; Díaz, B.B.; De León, A.C. Acute Coronary Syndrome in the Young: Clinical Characteristics, Risk Factors and Prognosis. Open Cardiovasc. Med. J. 2014, 8, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Meirhaeghe, A.; Montaye, M.; Biasch, K.; Huo Yung Kai, S.; Moitry, M.; Amouyel, P.; Ferrières, J.; Dallongeville, J. Coronary Heart Disease Incidence Still Decreased between 2006 and 2014 in France, except in Young Age Groups: Results from the French MONICA Registries. Eur. J. Prev. Cardiol. 2020, 27, 1178–1186. [Google Scholar] [CrossRef] [PubMed]
- Andersson, C.; Vasan, R.S. Epidemiology of Cardiovascular Disease in Young Individuals. Nat. Rev. Cardiol. 2018, 15, 230–240. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.Y.; Berman, A.N.; Biery, D.W.; Blankstein, R. Recent Trends in Acute Myocardial Infarction among the Young. Curr. Opin. Cardiol. 2020, 35, 524. [Google Scholar] [CrossRef]
- Bucholz, E.M.; Strait, K.M.; Dreyer, R.P.; Lindau, S.T.; D’Onofrio, G.; Geda, M.; Spatz, E.S.; Beltrame, J.F.; Lichtman, J.H.; Lorenze, N.P.; et al. Editor’s Choice-Sex Differences in Young Patients with Acute Myocardial Infarction: A VIRGO Study Analysis. Eur. Heart J. Acute Cardiovasc. Care 2017, 6, 610–622. [Google Scholar] [CrossRef]
- Manzo-Silberman, S.; Couturaud, F.; Bellemain-Appaix, A.; Vautrin, E.; Gompel, A.; Drouet, L.; Marliere, S.; Sollier, C.B.D.; Uhry, S.; Eltchaninoff, H.; et al. Characteristics of Young Women Presenting with Acute Myocardial Infarction: The Prospective, Multicenter, Observational Young Women Presenting Acute Myocardial Infarction in France Study. J. Am. Heart Assoc. 2024, 13, e034456. [Google Scholar] [CrossRef]
- Siagian, S.N.; Christianto, C.; Angellia, P.; Holiyono, H.I. The Risk Factors of Acute Coronary Syndrome in Young Women:A Systematic Review and Meta-Analysis. Clin. Cancer Res. 2023, 19, e161122210969. [Google Scholar] [CrossRef]
- Page, R.L.I.; Ghushchyan, V.; Gifford, B.; Read, R.A.; Raut, M.; Crivera, C.; Naim, A.B.; Damaraju, C.V.; Nair, K.V. The Economic Burden of Acute Coronary Syndromes for Employees and Their Dependents: Medical and Productivity Costs. J. Occup. Environ. Med. 2013, 55, 761. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Li, S.-X.; Liu, Y.; Rodriguez, F.; Watson, K.E.; Dreyer, R.P.; Khera, R.; Murugiah, K.; D’Onofrio, G.; Spatz, E.S.; et al. Sex-Specific Risk Factors Associated with First Acute Myocardial Infarction in Young Adults. JAMA Netw. Open 2022, 5, e229953. [Google Scholar] [CrossRef]
- Flores-Umanzor, E.; Cepas-Guillén, P.; Freixa, X.; Regueiro, A.; Tizón-Marcos, H.; Brugaletta, S.; Ariza-Solé, A.; Calvo, M.; Forado, I.; Carrillo, X.; et al. Perfil clínico y pronóstico de pacientes jóvenes con infarto agudo de miocardio con elevación del segmento ST tratados en la red Codi IAM. Rev. Española Cardiol. 2023, 76, 881–890. [Google Scholar] [CrossRef]
- Papathanasiou, K.A.; Rallidis, S.L.; Armylagos, S.; Kotrotsios, G.; Rallidis, L.S. Gender Differences Among Very Young Patients with Acute Coronary Syndrome: Long-Term Follow-Up of the STAMINA Study. Angiology 2024, Epub ahead of printing. [Google Scholar] [CrossRef]
- Maroszyńska-Dmoch, E.M.; Wożakowska-Kapłon, B. Clinical and Angiographic Characteristics of Coronary Artery Disease in Young Adults: A Single Centre Study. Pol. Heart J. 2016, 74, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Fournier, J.A.; Cabezón, S.; Cayuela, A.; Ballesteros, S.M.; Cortacero, J.A.P.; Díaz De La Llera, L.S. Long-Term Prognosis of Patients Having Acute Myocardial Infarction When ≤40 Years of Age. Am. J. Cardiol. 2004, 94, 989–992. [Google Scholar] [CrossRef]
- Leifheit-Limson, E.C.; D’Onofrio, G.; Daneshvar, M.; Geda, M.; Bueno, H.; Spertus, J.A.; Krumholz, H.M.; Lichtman, J.H. Sex Differences in Cardiac Risk Factors, Perceived Risk, and Health Care Provider Discussion of Risk and Risk Modification Among Young Patients with Acute Myocardial Infarction. J. Am. Coll. Cardiol. 2015, 66, 1949–1957. [Google Scholar] [CrossRef]
- Desai, R.; Mishra, V.; Chhina, A.K.; Jain, A.; Vyas, A.; Allamneni, R.; Lavie, C.J.; Sachdeva, R.; Kumar, G. Cardiovascular Disease Risk Factors and Outcomes of Acute Myocardial Infarction in Young Adults: Evidence From 2 Nationwide Cohorts in the United States a Decade Apart. Curr. Probl. Cardiol. 2023, 48, 101747. [Google Scholar] [CrossRef] [PubMed]
- Presentation, Clinical Profile, and Prognosis of Young Patients with Myocardial Infarction with Nonobstructive Coronary Arteries (MINOCA): Results from the VIRGO Study. Available online: https://www.ahajournals.org/doi/epub/10.1161/JAHA.118.009174 (accessed on 17 October 2024).
- Zasada, W.; Bobrowska, B.; Plens, K.; Dziewierz, A.; Siudak, Z.; Surdacki, A.; Dudek, D.; Bartuś, S. Acute Myocardial Infarction in Young Patients. Pol. Heart J. 2021, 79, 1093–1098. [Google Scholar] [CrossRef]
- Rallidis, L.S.; Gialeraki, A.; Triantafyllis, A.S.; Tsirebolos, G.; Liakos, G.; Moutsatsou, P.; Iliodromitis, E. Characteristics and Long-Term Prognosis of Patients ≤35 Years of Age with ST Segment Elevation Myocardial Infarction and “Normal or Near Normal” Coronary Arteries. Am. J. Cardiol. 2017, 120, 740–746. [Google Scholar] [CrossRef]
- Rodriguez, S.P.; Salvadores, P.J.; Garcia, C.V.; González-Novoa, J.A.; Romo, A.I.; Díaz, V.A.J. TCT-775 Behind the Heart of Women: Coronary Artery Disease in Very Young Women. In Proceedings of the TCT® 2024: Transcatheter Cardiovascular Therapeutics, Washington, DC, USA, 27–30 November 2024. [Google Scholar]
- Loria, C.M.; Liu, K.; Lewis, C.E.; Hulley, S.B.; Sidney, S.; Schreiner, P.J.; Williams, O.D.; Bild, D.E.; Detrano, R. Early Adult Risk Factor Levels and Subsequent Coronary Artery Calcification. J. Am. Coll. Cardiol. 2007, 49, 2013–2020. [Google Scholar] [CrossRef] [PubMed]
- Rallidis, L.S.; Lekakis, J.; Panagiotakos, D.; Fountoulaki, K.; Komporozos, C.; Apostolou, T.; Rizos, L.; Kremastinos, D.T. Long-Term Prognostic Factors of Young Patients (≤35 Years) Having Acute Myocardial Infarction: The Detrimental Role of Continuation of Smoking. Eur. J. Cardiovasc. Prev. Rehabil. 2008, 15, 567–571. [Google Scholar] [CrossRef] [PubMed]
- Alkhawam, H.; Sogomonian, R.; El-Hunjul, M.; Kabach, M.; Syed, U.; Vyas, N.; Ahmad, S.; Vittorio, T.J. Risk Factors for Coronary Artery Disease and Acute Coronary Syndrome in Patients ≤40 Years Old. Future Cardiol. 2016, 12, 545–552. [Google Scholar] [CrossRef]
- Sawano, M.; Lu, Y.; Caraballo, C.; Mahajan, S.; Dreyer, R.; Lichtman, J.H.; D’Onofrio, G.; Spatz, E.; Khera, R.; Onuma, O.; et al. Sex Difference in Outcomes of Acute Myocardial Infarction in Young Patients. J. Am. Coll. Cardiol. 2023, 81, 1797–1806. [Google Scholar] [CrossRef] [PubMed]
- Medication Adherence Influencing Factors—An (Updated) Overview of Systematic Reviews Full Text. Available online: https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-019-1014-8 (accessed on 17 October 2024).
- Chowdhury, R.; Khan, H.; Heydon, E.; Shroufi, A.; Fahimi, S.; Moore, C.; Stricker, B.; Mendis, S.; Hofman, A.; Mant, J.; et al. Adherence to Cardiovascular Therapy: A Meta-Analysis of Prevalence and Clinical Consequences. Eur. Heart J. 2013, 34, 2940–2948. [Google Scholar] [CrossRef] [PubMed]
- Cole, J.H.; Miller, J.I.; Sperling, L.S.; Weintraub, W.S. Long-Term Follow-up of Coronary Artery Disease Presenting in Young Adults. J. Am. Coll. Cardiol. 2003, 41, 521–528. [Google Scholar] [CrossRef]
- Juan-Salvadores, P.; Castro-Rodríguez, M.; Jiménez-Díaz, V.A.; Veiga, C.; Busto, L.; Fernández-Barbeira, S.; Iñiguez-Romo, A. Sex Differences in Delay Times in ST-Segment Elevation Myocardial Infarction: A Cohort Study. Med. Clin. 2024, 163, 115–120. [Google Scholar] [CrossRef]
- Smolderen, K.G.; Strait, K.M.; Dreyer, R.P.; D’Onofrio, G.; Zhou, S.; Lichtman, J.H.; Geda, M.; Bueno, H.; Beltrame, J.; Safdar, B.; et al. Depressive Symptoms in Younger Women and Men with Acute Myocardial Infarction: Insights from the VIRGO Study. J. Am. Heart Assoc. 2015, 4, e001424. [Google Scholar] [CrossRef] [PubMed]
- Bucholz, E.M.; Strait, K.M.; Dreyer, R.P.; Geda, M.; Spatz, E.S.; Bueno, H.; Lichtman, J.H.; D’Onofrio, G.; Spertus, J.A.; Krumholz, H.M. Effect of Low Perceived Social Support on Health Outcomes in Young Patients with Acute Myocardial Infarction: Results from the Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients (VIRGO) Study. J. Am. Heart Assoc. 2014, 3, e001252. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Overall (n = 52) | Non-CAD Women (n = 23) | Women with CAD (n = 29) | p-Value |
|---|---|---|---|---|
| Age, median (IQR) | 35 (26–40) | 35 (26–40) | 35 (26–40) | 0.879 |
| Family History of CAD; n (%) | 14 (26.9) | 2 (8.7) | 12 (41.4) | 0.008 * |
| Follow-up time (years) | 4.9 ± 2.3 | 5.4 ± 2.4 | 4.5 ± 2.2 | 0.144 |
| Hospitalization days | 6.9 ± 7.4 | 7.8 ± 11.0 | 6.2 ± 3.1 | 0.522 |
| Comorbidities; n (%) | ||||
| Hypertension | 9 (17.3) | 4 (17.4) | 5 (17.2) | 0.989 |
| Diabetes | 1 (1.9) | 0 (0) | 1 (3.4) | 0.369 |
| Current smoker | 40 (76.9) | 14 (60.9) | 26 (89.7) | 0.014 * |
| BMI ≥ 30 kg/m2 | 14 (26.9) | 7 (30.4) | 7 (24.1) | 0.611 |
| Dyslipidaemia | 16 (30.8) | 7 (30.4) | 9 (31.0) | 0.963 |
| Drug consumption | 5 (9.6) | 2 (8.7) | 3 (10.3) | 0.841 |
| Depression | 9 (17.3) | 5 (21.7) | 4 (13.8) | 0.452 |
| Lipid levels and Atherogenic Indexes; n (%) | ||||
| Total cholesterol | 190.8 ± 50.6 | 188.7 ± 40.8 | 192.4 ± 57.8 | 0.274 |
| HDL-C | 45.8 ± 14.8 | 47.4 ± 14.5 | 44.9 ± 15.2 | 0.807 |
| LDL-C | 120.6 ± 46.2 | 125.8 ± 34.7 | 117.5 ± 52.1 | 0.457 |
| Triglycerides | 144.0 ± 117.6 | 142.2 ± 78.4 | 145.4 ± 143.2 | 0.515 |
| Creatinine | 0.75 ± 0.17 | 0.79 ± 0.17 | 0.72 ± 0.16 | 0.508 |
| Glucose | 105.2 ± 30.5 | 101.9 ± 29.3 | 107.7 ± 31.7 | 0.503 |
| Castelli Index | 4.6 ± 1.8 | 4.6 ± 1.71 | 4.7 ± 1.87 | 0.873 |
| Kannel Index | 2.9 ± 1.4 | 3.0 ± 1.4 | 2.9 ± 1.5 | 0.843 |
| TGL/HDL Index | 3.8 ± 4.0 | 3.5 ± 2.3 | 4.02 ± 4.77 | 0.325 |
| Residual Cholesterol | 26.8 ± 14.1 | 28.3 ± 15.0 | 25.9 ± 13.7 | 0.582 |
| TGL/Glucose Index | 8.71 ± 0.68 | 8.68 ± 0.60 | 8.73 ± 0.75 | 0.673 |
| Admission Symptoms | ||||
| Chest pain | 46 (88.5) | 19 (82.7) | 27 (93.1) | 0.239 |
| Dyspnoea | 5 (9.6) | 1 (4.3) | 4 (13.8) | 0.251 |
| Shock | 5 (9.6) | 3 (13.0) | 2 (6.9) | 0.455 |
| LVEF (%) | 54.7 ± 11.7 | 52.5 ± 15.3 | 56.3 ± 7.9 | 0.313 |
| Coronary angiography indication | ||||
| ACS | 41 (78.8) | 14 (60.9) | 27 (93.1) | 0.005 * |
| STEMI | 18 (34.6) | 4 (17.4) | 14 (48.3) | |
| NSTEMI | 23 (44.2) | 10 (43.5) | 13 (44.8) | |
| Stable angina | 11 (21.2) | 9 (39.1) | 2 (6.9) | |
| Characteristic | Overall (n = 52) | Non-CAD Women (n = 23) | Women with CAD (n = 29) | p-Value |
|---|---|---|---|---|
| Pharmacological treatment at hospital admission. | ||||
| Statins | 1 (1.9) | 1 (4.5) | 0 (0) | 0.246 |
| CCB | 2 (3.8) | 1 (4.5) | 1 (3.4) | 0.842 |
| ARBs | 1 (1.9) | 0 (0) | 1 (3.4) | 0.379 |
| ACE inhibitors | 3 (5.8) | 1 (4.5) | 2 (6.9) | 0.724 |
| Beta Blockers | 2 (3.8) | 2 (9.1) | 0 (0) | 0.098 |
| Anticoagulants | 1 (1.9) | 0 (0) | 1 (3.4) | 0.379 |
| ASA | 3 (5.8) | 3 (13.6) | 0 (0) | 0.040 * |
| P2Y12 Inhibitors | 1 (1.9) | 1 (4.5) | 0 (0) | 0.246 |
| Pharmacological treatment at discharge. | ||||
| Statins | 27 (54.0) | 4 (18.2) | 23 (82.1) | <0.001 * |
| CCB | 4 (8.0) | 2 (9.1) | 2 (7.1) | 0.801 |
| ARBs | 1 (2.0) | 0 (0) | 1 (3.6) | 0.371 |
| ACE-I | 12 (24.0) | 1 (4.5) | 11 (39.3) | 0.004 * |
| Beta Blockers | 31 (62.0) | 6 (27.3) | 25 (89.3) | <0.001 * |
| Anticoagulants | 0 (0) | 0 (0) | 0 (0) | - |
| ASA | 38 (76.0) | 10 (45.5) | 28 (100.0) | <0.001 * |
| P2Y12 Inhibitors | 26 (52.0) | 2 (91.1) | 24 (85.7) | <0.001 * |
| Oral contraceptives | 4 (8.0) | 2 (9.1) | 2 (9.1) | 0.801 |
| Adverse Events | Overall (n = 52) | Non-CAD Women (n = 23) | Women with CAD (n = 29) | p-Value |
|---|---|---|---|---|
| New coronary revascularization | 4 (7.7) | 1 (4.3) | 3 (10.3) | 0.420 |
| Death | 1 (1.9) | 0 (0) | 1 (3.4) | 0.369 |
| AMI | 1 (1.9) | 0 (0) | 1 (3.4) | 0.369 |
| Stroke | 1 (1.9) | 0 (0) | 1 (3.4) | 0.369 |
| MACE | 7 (13.5) | 1 (4.3) | 6 (20.7) | 0.086 |
| Characteristic | Overall (n = 52) | Non-MACE Women (n = 45) | Women with MACE (n = 7) | p-Value |
|---|---|---|---|---|
| Age, median (IQR) | 35 (26–40) | 35 (26–40) | 35 (28–40) | 0.213 |
| Family History of CAD; n (%) | 14 (26.9) | 12 (26.7) | 2 (28.6) | 0.916 |
| Previous EAC; n (%) | 7 (13.5) | 1 (2.2) | 6 (85.7) | 0.086 |
| Follow-up time (years) | 4.9 ± 2.3 | 5.0 ± 2.2 | 3.7 ± 2.6 | 0.157 |
| Hospitalization days | 6.9 ± 7.4 | 6.8 ± 7.9 | 7.3 ± 4.3 | 0.878 |
| Comorbidities; n (%) | ||||
| Hypertension | 9 (17.3) | 8 (17.8) | 1 (14.3) | 0.820 |
| Diabetes | 1 (1.9) | 0 (0) | 1 (14.3) | 0.010 ** |
| Current smoker | 40 (76.9) | 34 (75.6) | 6 (85.7) | 0.553 |
| BMI ≥ 30 kg/m2 | 14 (26.9) | 12 (26.7) | 2 (28.6) | 0.916 |
| Dyslipidaemia | 16 (30.8) | 12 (26.7) | 4 (57.1) | 0.104 |
| Drug consumption | 5 (9.6) | 5 (11.1) | 0 (0) | 0.354 |
| Depression | 9 (17.3) | 5 (11.1) | 4 (57.1) | 0.003 * |
| Lipid levels and Atherogenic Indexes; n (%) | ||||
| Total cholesterol | 190.8 ± 50.6 | 190.6 ± 48.3 | 191.6 ± 67.3 | 0.064 |
| HDL-C | 45.8 ± 14.8 | 48.4 ± 14.5 | 32.6 ± 8.2 | 0.058 |
| LDL-C | 120.6 ± 46.2 | 122.2 ± 44.0 | 111.2 ± 61.6 | 0.141 |
| Triglycerides | 144.0 ± 117.6 | 125.9 ± 70.6 | 247.6 ± 242.5 | 0.001 * |
| Creatinine | 0.75 ± 0.17 | 0.76 ± 0.16 | 0.72 ± 0.20 | 0.222 |
| Glucose | 105.2 ± 30.5 | 101.9 ± 24.9 | 124.6 ± 51.5 | <0.001 * |
| Castelli Index | 4.6 ± 1.8 | 4.3 ± 1.5 | 6.3 ± 2.5 | 0.007 * |
| Kannel Index | 2.9 ± 1.4 | 2.7 ± 1.3 | 3.7 ± 2.2 | 0.006 * |
| TGL/HDL Index | 3.8 ± 4.0 | 2.9 ± 2.0 | 8.1 ± 7.7 | <0.001 * |
| Residual Cholesterol | 26.8 ± 14.1 | 25.9 ± 13.7 | 32.0 ± 16.4 | 0.580 |
| TGL/Glucose Index | 8.71 ± 0.68 | 8.61 ± 0.56 | 9.26 ± 1.00 | 0.171 |
| LVEF (%) | 54.7 ± 11.7 | 54.9 ± 11.8 | 53.3 ± 11.6 | 0.738 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pintos-Rodríguez, S.; Jiménez Díaz, V.A.; Veiga, C.; Martínez García, C.; Caamaño Isorna, F.; Íñiguez Romo, A.; Juan-Salvadores, P. Coronary Artery Disease in Very Young Women: Risk Factors and Prognostic Insights from Extended Follow-Up. J. Cardiovasc. Dev. Dis. 2025, 12, 34. https://doi.org/10.3390/jcdd12020034
Pintos-Rodríguez S, Jiménez Díaz VA, Veiga C, Martínez García C, Caamaño Isorna F, Íñiguez Romo A, Juan-Salvadores P. Coronary Artery Disease in Very Young Women: Risk Factors and Prognostic Insights from Extended Follow-Up. Journal of Cardiovascular Development and Disease. 2025; 12(2):34. https://doi.org/10.3390/jcdd12020034
Chicago/Turabian StylePintos-Rodríguez, Samuel, Víctor Alfonso Jiménez Díaz, César Veiga, Carlos Martínez García, Francisco Caamaño Isorna, Andrés Íñiguez Romo, and Pablo Juan-Salvadores. 2025. "Coronary Artery Disease in Very Young Women: Risk Factors and Prognostic Insights from Extended Follow-Up" Journal of Cardiovascular Development and Disease 12, no. 2: 34. https://doi.org/10.3390/jcdd12020034
APA StylePintos-Rodríguez, S., Jiménez Díaz, V. A., Veiga, C., Martínez García, C., Caamaño Isorna, F., Íñiguez Romo, A., & Juan-Salvadores, P. (2025). Coronary Artery Disease in Very Young Women: Risk Factors and Prognostic Insights from Extended Follow-Up. Journal of Cardiovascular Development and Disease, 12(2), 34. https://doi.org/10.3390/jcdd12020034








