Minimally Invasive Repair of Sinus Venosus Atrial Septal Defects and Anomalous Pulmonary Venous Connections via Vertical Right Axillary Thoracotomy
Abstract
1. Introduction
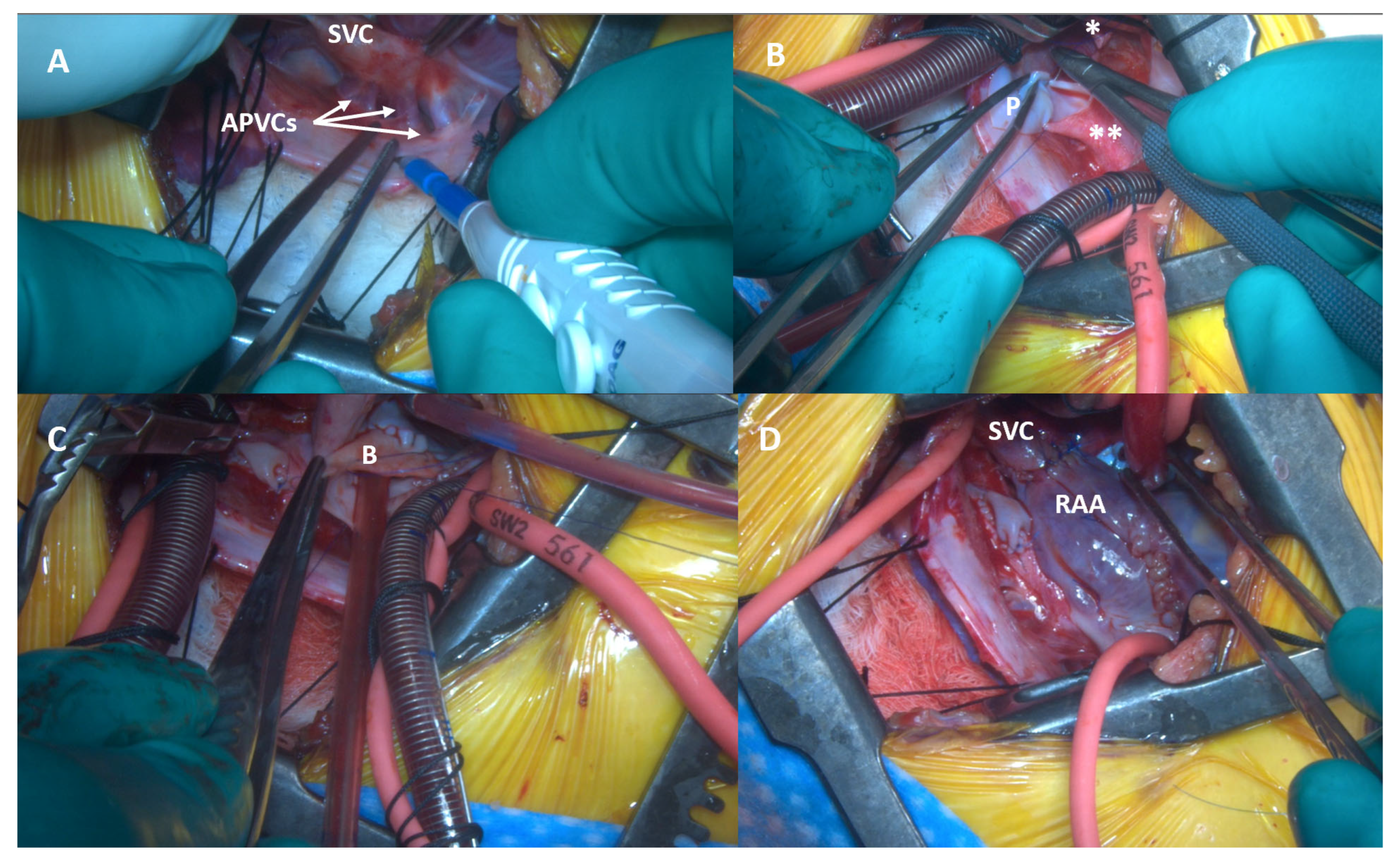
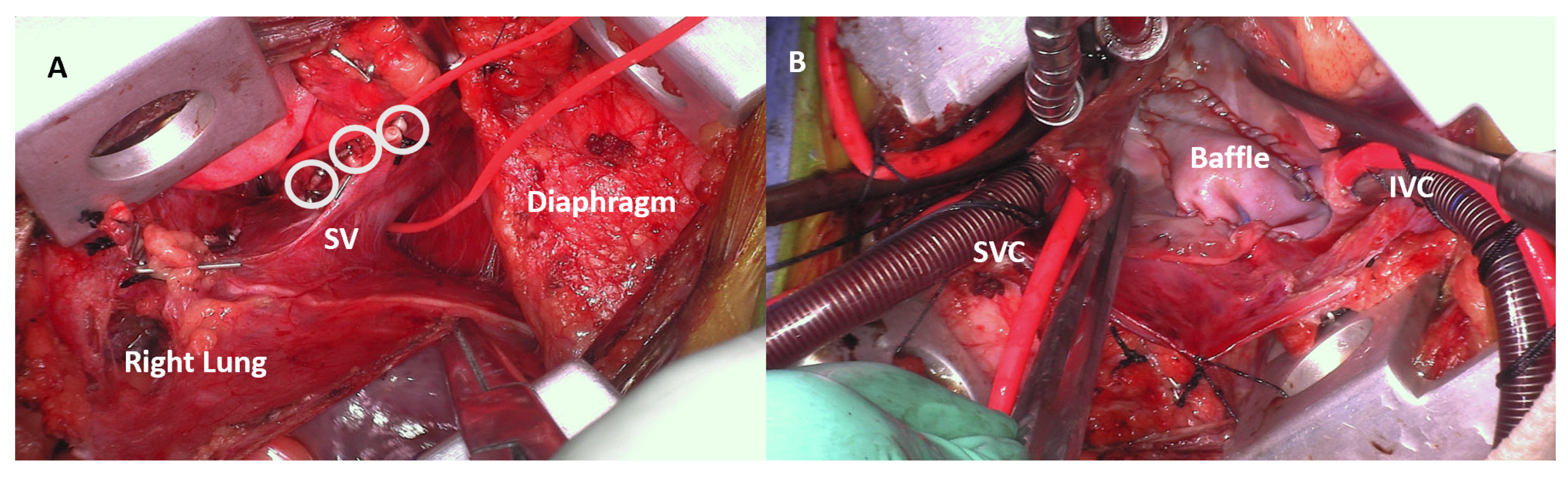
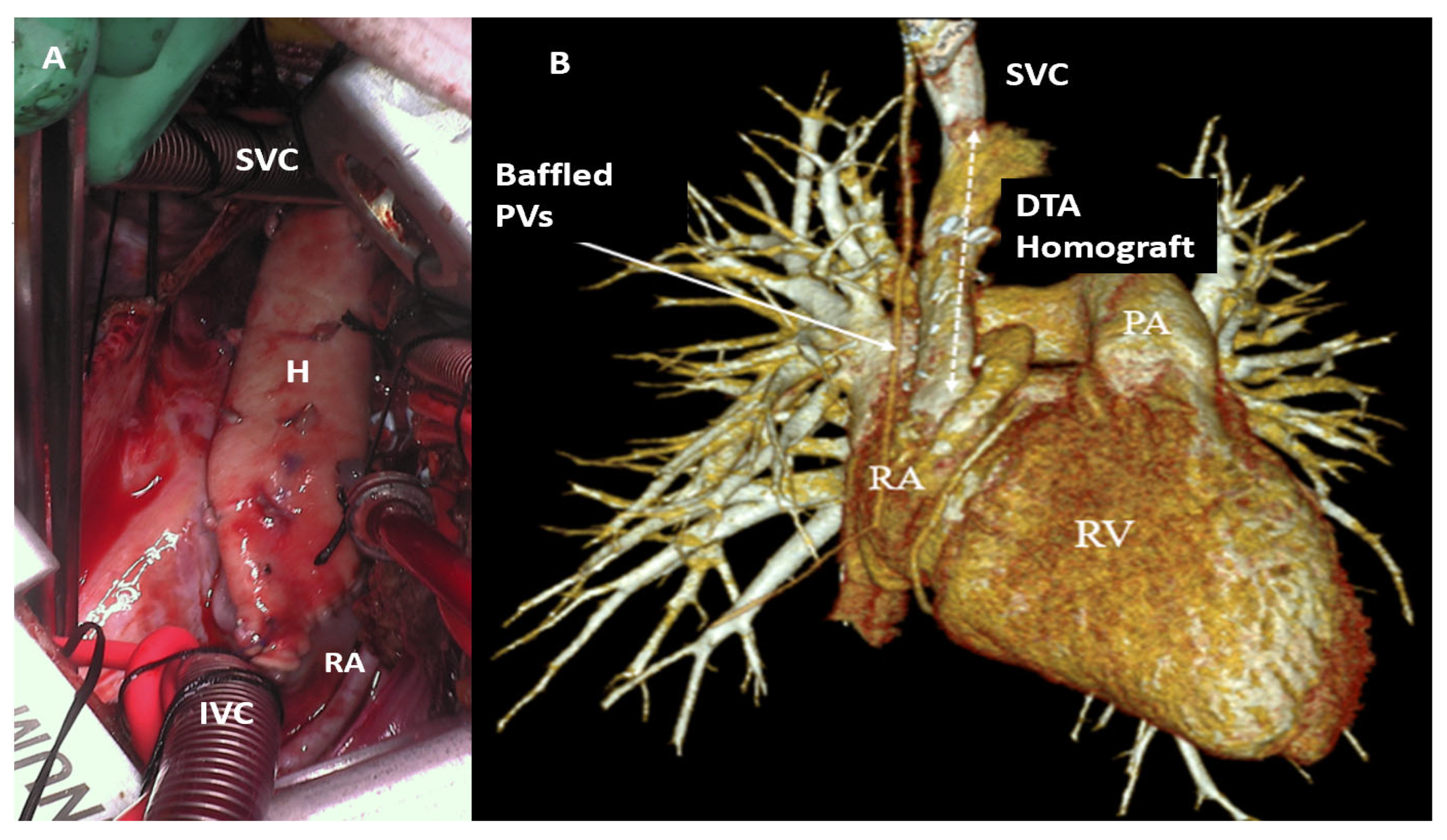
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
6. Study Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| APVCs | anomalous pulmonary venous connections |
| ASD(s) | atrial septal defect(s) |
| AXC | aortic cross-clamp |
| CPB | cardiopulmonary bypass |
| CS | coronary sinus |
| CT | computed tomography |
| IRB | institutional review board |
| MRI | magnetic resonance imaging |
| PAPVCs | partial anomalous pulmonary venous connections |
| PAPVR | partial anomalous pulmonary venous return |
| SD | standard deviation |
| SV | sinus venosus |
| SVC | superior vena cava |
| TAPVCs | total anomalous pulmonary venous connections |
| TEE | transesophageal echocardiography |
| TTE | transthoracic echocardiography |
| VRAT | vertical right axillary thoracotomy |
References
- Julian, O.C.; Lopez-Belio, M.; Dye, W.S.; Javid, H.; Grove, W.J. The median sternal incision in intracardiac surgery with extracorporeal circulation; a general evaluation of its use in heart surgery. Surgery 1957, 42, 753–761. [Google Scholar] [PubMed]
- Dodge-Khatami, J.; Dodge-Khatami, A. Advantages of a mini right axillary thoracotomy for congenital heart defect repair in children. Cardiol. Young 2022, 32, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Prêtre, R.; Kadner, A.; Dave, H.; Dodge-Khatami, A.; Bettex, D.; Berger, F. Right axillary incision: A cosmetically superior approach to repair a wide range of congenital cardiac defects. J. Thorac. Cardiovasc. Surg. 2005, 130, 277–281. [Google Scholar] [CrossRef] [PubMed]
- Lo Rito, M.; Brindicci, Y.C.M.; Moscatiello, M.; Varrica, A.; Reali, M.; Saracino, A.; Chessa, M.; Aloisio, T.; Isgrò, G.; Giamberti, A. Minimally Invasive Surgery for Simple Congenital Heart Defects: Preserving Aesthetics without Jeopardizing Patient Safety. J. Cardiovasc. Dev. Dis. 2023, 10, 452. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.X.; Tan, J.; Chen, S.; Ding, H.; Xu, Z.W. Comparison of clinical outcomes and postoperative recovery between two open heart surgeries: Minimally invasive right subaxillary vertical thoracotomy and traditional median sternotomy. Asian Pac. J. Trop. Med. 2014, 7, 625–629. [Google Scholar] [CrossRef] [PubMed]
- Tran, D.M.; Tran, V.Q.; Nguyen, M.T.; Mai, D.D.; Doan, A.V.; Hoang, S.T.; Kotani, Y.; Nguyen, T.L.T. Minimally Invasive Surgical Repair of Simple Congenital Heart Defects Using the Right Vertical Infra-Axillary Thoracotomy Approach. Innovations 2024, 19, 520–525. [Google Scholar] [CrossRef] [PubMed]
- Said, S.M.; Greathouse, K.C.; McCarthy, C.M.; Brown, N.; Kumar, S.; Salem, M.I.; Kloesel, B.; Sainathan, S. Safety and Efficacy of Right Axillary Thoracotomy for Repair of Congenital Heart Defects in Children. World J. Pediatr. Congenit. Heart Surg. 2023, 14, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Rao, R.K.; Varadaraju, R.; Basappa, G.; Nagaraja, P.S. Repair of Sinus Venosus Defects with Partial Anomalous Pulmonary Venous Connection in Children by Modified Right Vertical Infra Axillary Thoracotomy. Innovations 2019, 14, 553–557. [Google Scholar] [CrossRef] [PubMed]
- Amirghofran, A.A.; Nirooei, E.; Edraki, M.; Ramsheh, A.R.; Ajami, G.; Amoozgar, H.; Arabi, H.; Hemmati, R. Minimally invasive versus sternotomy approach for double-patch repair of partial anomalous pulmonary venous connection and sinus venosus defect in pediatric and adult patients: Mid to long-term outcomes. J. Card. Surg. 2022, 37, 4808–4815. [Google Scholar] [CrossRef] [PubMed]
- Said, S.M. Vertical right axillary thoracotomy for a modified Warden procedure with a descending thoracic aortic homograft: Tips and pitfalls. Multimed. Man. Cardiothorac. Surg. 2021. [Google Scholar] [CrossRef]
- Dodge-Khatami, A.; Gil-Jaurena, J.M.; Horer, J.; Heinisch, P.P.; Cleuziou, J.; Arrigoni, S.C.; Cesnjevar, R.A.; Dave, H.H.; Giamberti, A.; Rito, M.L.; et al. Over 3,000 minimally invasive thoracotomies from the European Congenital Heart Surgeons Association for quality repairs of the most common congenital heart defects: Safe and routine for selected repairs. World J. Pediatr. Congenit. Heart Surg. 2025, 16, 578–584. [Google Scholar] [CrossRef] [PubMed]
- Dodge-Khatami, J.; Dodge-Khatami, A.; Nguyen, T.D.; Rüffer, A. Minimally invasive approaches for pediatric & congenital heart surgery: Safe, reproducible, more cosmetic than through sternotomy, and here to stay. Transl. Pediatr. 2023, 12, 1744–1752. [Google Scholar] [CrossRef] [PubMed]
| Age: Median (range) | 36 months (1–277 months) |
| Weight: Median (range) | 14.4 kg (3.6–79.4 kg) |
| Female: (%) | 13 (56.5%) |
| Primary Diagnosis | |
| Partial APVCs (%) | 14 (60.9%) |
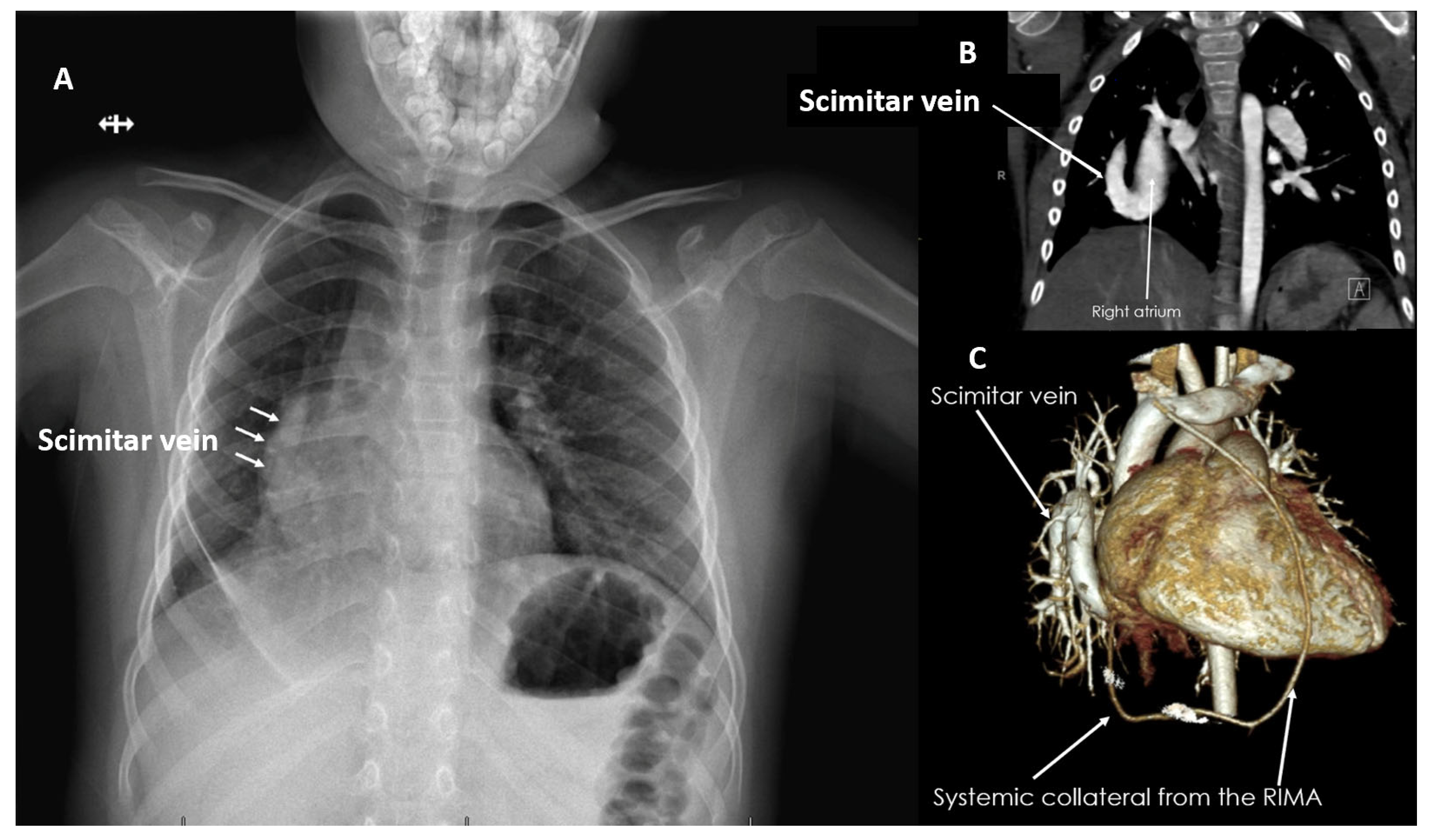
| Scimitar Syndrome (%) | 3 (13%) |
| Total APVCs to Coronary Sinus (%) | 2 (8.7%) |
| Conversion from VRAT to Sternotomy | 0 |
| Repair Technique | |
| Single Patch (%) | 10 (43.5%) |
| Warden (%) | 6 (26.1%) |
| Two-Patch (%) | 4 (17.4%) |
| Scimitar Repair (%) | 3 (13%) |
| Intraoperative | |
| CPB Median (range) | 91 min (48–257 min) |
| AXC Median (range) | 62 min (31–196 min) |
| Mortality | |
| Early/Late Mortality | 0 |
| Late Follow-Up | |
| Pulmonary/Systemic Venous Pathway Obstruction | 0 |
| Warden Mild SVC Gradient (%) | 2 (8.7%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Said, S.M.; Mashadi, A.H.; Essa, Y.; Greathouse, K.; Brown, N.; Salem, M.I.; Giamelli, J. Minimally Invasive Repair of Sinus Venosus Atrial Septal Defects and Anomalous Pulmonary Venous Connections via Vertical Right Axillary Thoracotomy. J. Cardiovasc. Dev. Dis. 2025, 12, 404. https://doi.org/10.3390/jcdd12100404
Said SM, Mashadi AH, Essa Y, Greathouse K, Brown N, Salem MI, Giamelli J. Minimally Invasive Repair of Sinus Venosus Atrial Septal Defects and Anomalous Pulmonary Venous Connections via Vertical Right Axillary Thoracotomy. Journal of Cardiovascular Development and Disease. 2025; 12(10):404. https://doi.org/10.3390/jcdd12100404
Chicago/Turabian StyleSaid, Sameh M., Ali H. Mashadi, Yasin Essa, Kristin Greathouse, Nicholas Brown, Mahmoud I. Salem, and Joseph Giamelli. 2025. "Minimally Invasive Repair of Sinus Venosus Atrial Septal Defects and Anomalous Pulmonary Venous Connections via Vertical Right Axillary Thoracotomy" Journal of Cardiovascular Development and Disease 12, no. 10: 404. https://doi.org/10.3390/jcdd12100404
APA StyleSaid, S. M., Mashadi, A. H., Essa, Y., Greathouse, K., Brown, N., Salem, M. I., & Giamelli, J. (2025). Minimally Invasive Repair of Sinus Venosus Atrial Septal Defects and Anomalous Pulmonary Venous Connections via Vertical Right Axillary Thoracotomy. Journal of Cardiovascular Development and Disease, 12(10), 404. https://doi.org/10.3390/jcdd12100404







