Opening the Sacred Chamber: The Cultural and Ethical Odyssey of Cardiac Surgery
Abstract
1. Introduction
2. Materials and Methods
Source Selection and Search Strategy
- Peer-reviewed journal articles, academic books, and authoritative historical texts.
- Primary sources from antiquity to the modern period (e.g., Aristotle, Galen, Vesalius, Harvey, sacred scriptures).
- Scholarly interpretations from reputable disciplines such as medical history, ethics, theology, and cultural anthropology.
- Contemporary studies exploring the symbolic, emotional, or ethical dimensions of the heart or cardiac surgery.
- Non-scholarly or non-peer-reviewed publications, such as popular media articles or unverified web sources.
- Texts lacking relevance to the symbolic, ethical, or historical framing of the heart or cardiac surgery.
- Clinical case reports or technical studies unrelated to the broader conceptual or cultural analysis.
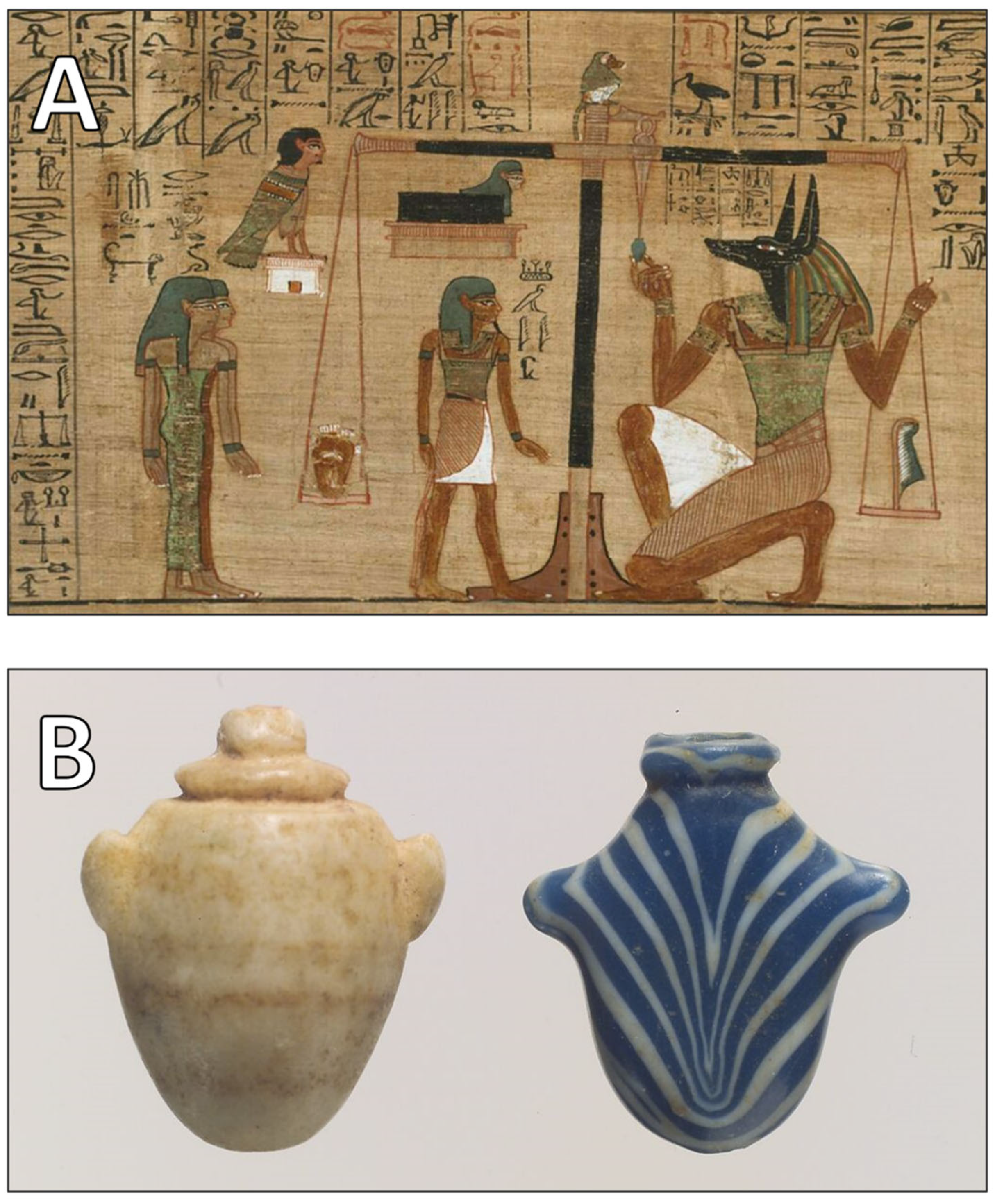
3. Ancient and Classical Views: The Heart as the Sacred Center of Being
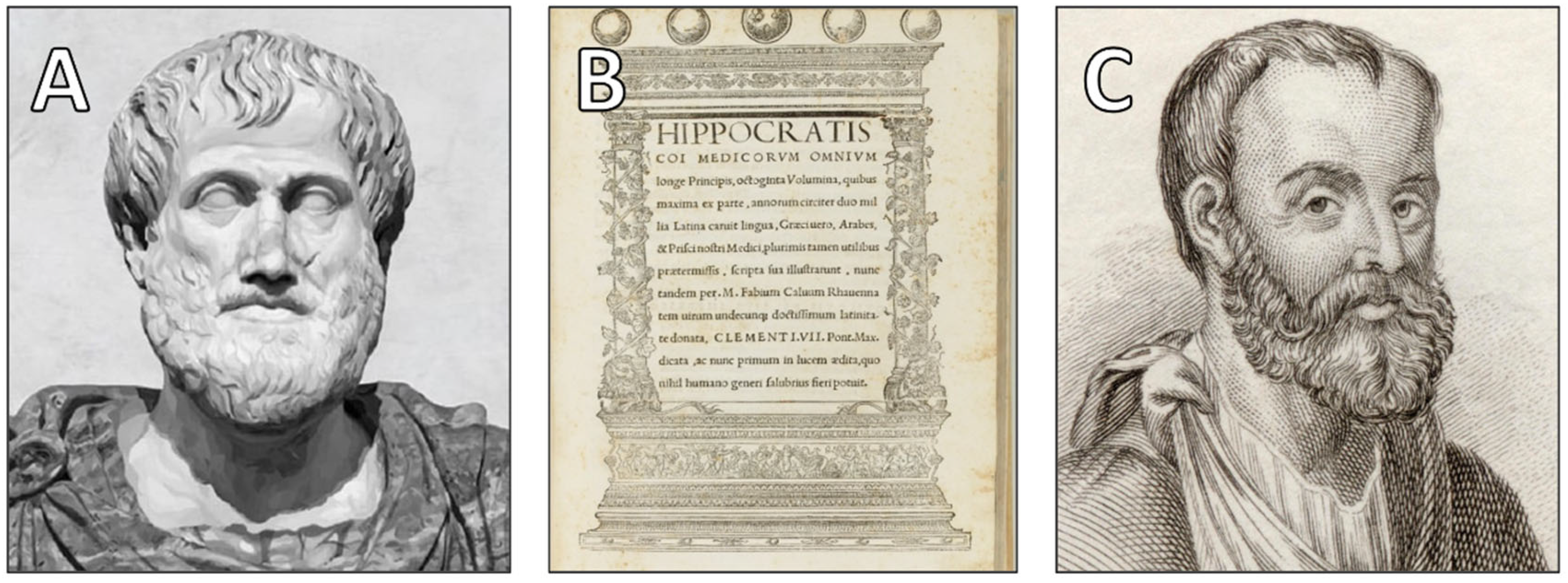
3.1. The Heart in Greek Philosophy and Medicine
3.2. The Heart in Religious Thought
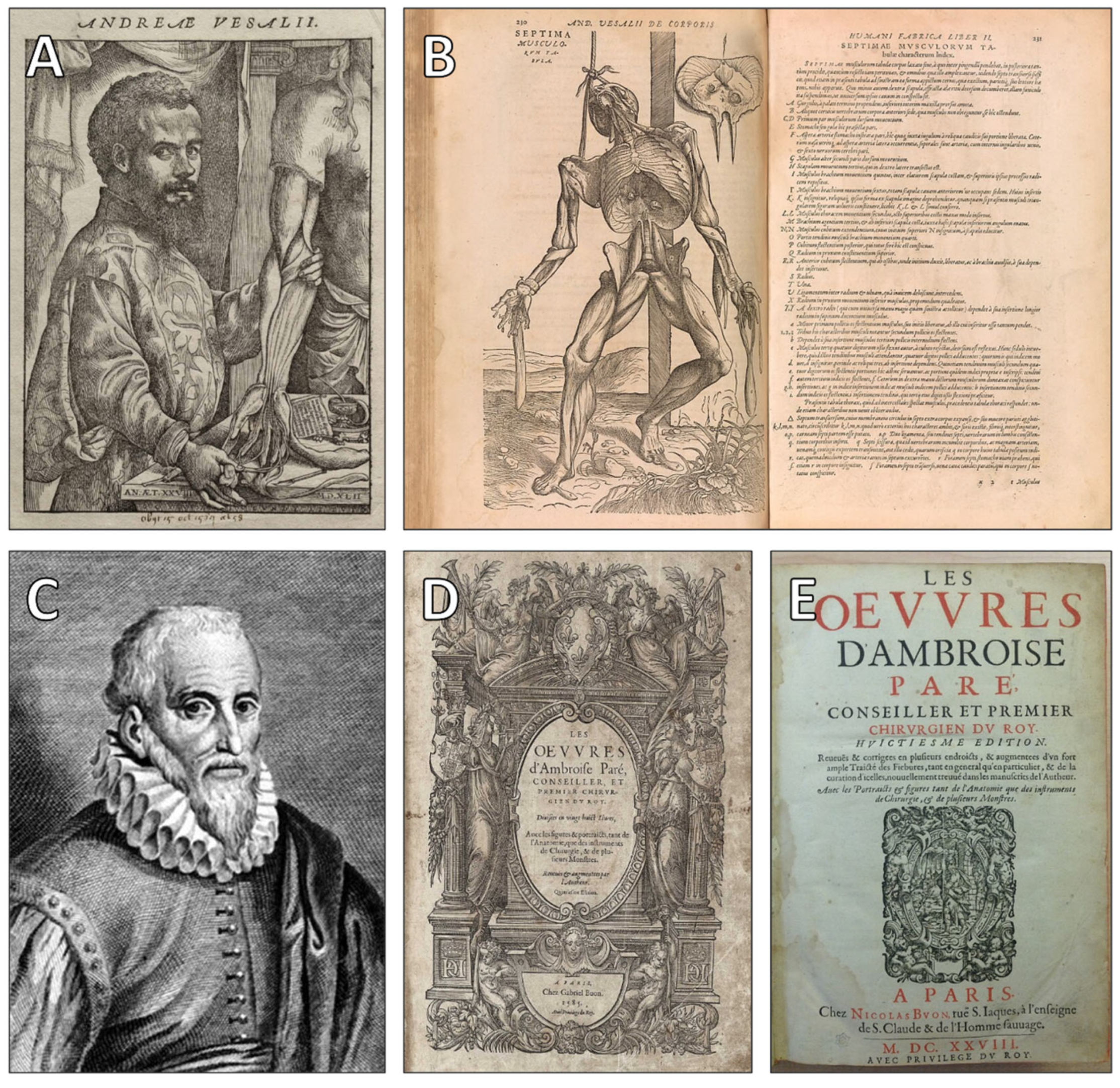
4. Early Surgical Practices: Approaching but Avoiding the Heart
5. Scientific Challenges Reinforcing Ethical Hesitations
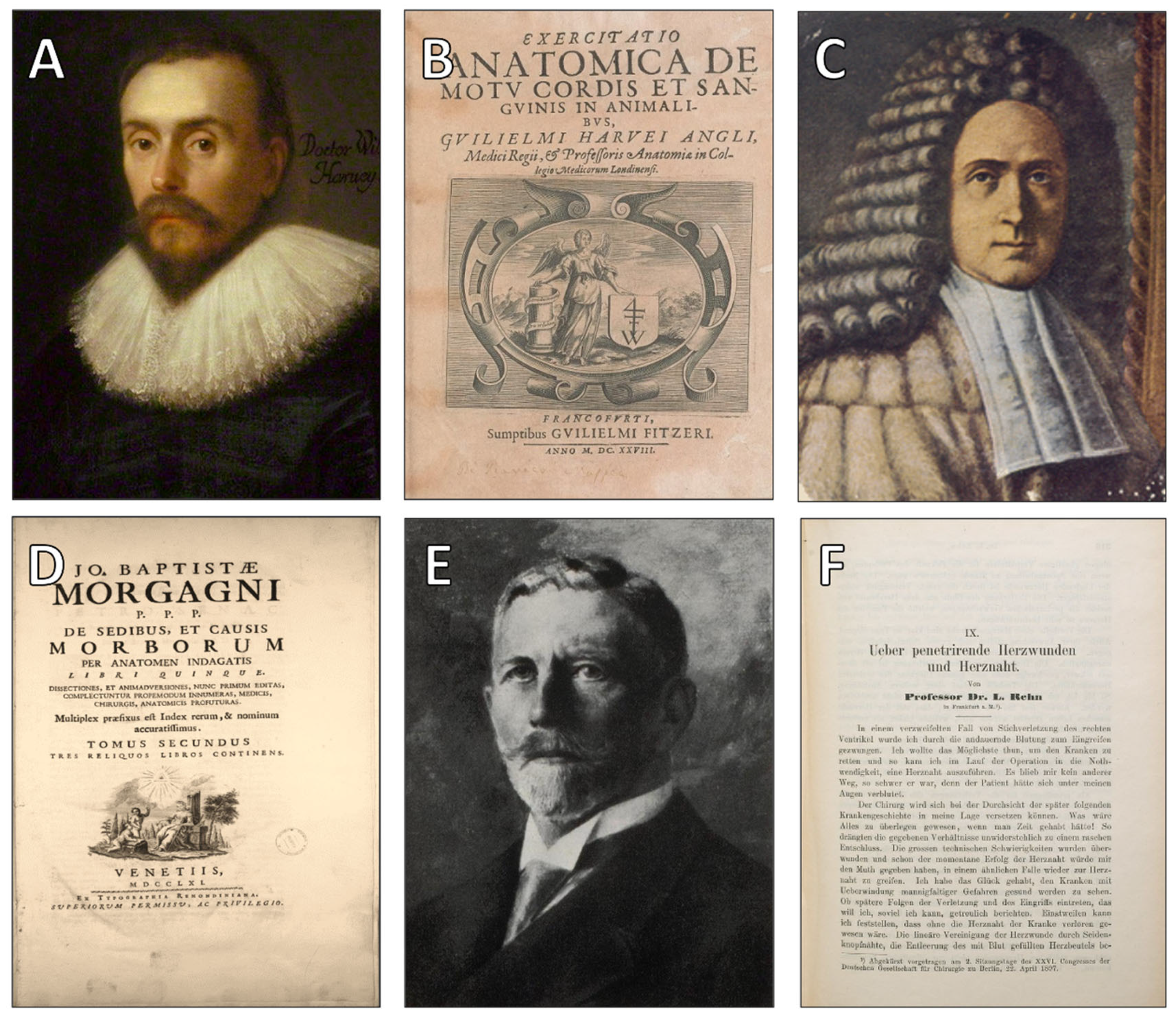
6. Shifts in Medical Thinking: Toward the Possibility of Heart Surgery
7. Modern Era: Redefining Ethics in Cardiothoracic Surgery
8. Discussion: Between Tissue and Meaning, Between Surgery and Soul
9. Limitations
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Riva, M.A.; Valnegri, C.; Invernizzi, P. The liver in Christian thought: Symbolism, morality, and spirituality. Clin. Liver Dis. 2024, 23, e0236. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zampieri, F.; Thiene, G.; Zanatta, A. Cardiocentrism in ancient medicines. Int. J. Cardiol. Heart Vasc. 2023, 48, 101261. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Butrous, G.; Maron, B.; Yacoub, M. The lamp of medicine of Ancient Egypt is still burning. Glob. Cardiol. Sci. Pract. 2020, 2020, e202016. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Woell, E.J. France and the Cult of the Sacred Heart: An Epic Tale for Modern Times. J. Soc. Hist. 2002, 35, 739–741. [Google Scholar] [CrossRef]
- Lafrance, J. In Prayer with Mary the Mother of Jesus; Médiaspaul: Paris, France, 1988; p. 310. ISBN 2-89039-183-3. [Google Scholar]
- Feiler, T.; Hordern, J. The heart in medicine, history and culture. Med. Humanit. 2020, 46, 350–351. [Google Scholar] [CrossRef] [PubMed]
- Figueredo, V.M. The Ancient Heart: What the Heart Meant to Our Ancestors. J. Am. Coll. Cardiol. 2021, 78, 957–959. [Google Scholar] [CrossRef] [PubMed]
- López Sánchez, O.; Nance, D.C. “Something Born of the Heart”: Culturally Affiliated Illnesses of Older Adults in Oaxaca. Issues Ment. Health Nurs. 2020, 41, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Furst, B. The Heart and Circulation: An Integrative Model; Springer: London, UK, 2016. [Google Scholar]
- Tsagkaris, C.; Moysidis, D.V.; Storozhuk, S.; Mozgova, N.G.; Papazoglou, A.S.; Loudovikou, A.; Poperechna, G. Lessons from the heart: Revisiting the psychocardiological theories of Aristotle in the 21st century. Wiad Lek. 2021, 74, 2846–2849. [Google Scholar] [CrossRef] [PubMed]
- Fowler, R.C. On the Heart of the Hippocratic Corpus: Its meaning, context and purpose. Med. Hist. 2023, 67, 266–283. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Figueredo, V.M. The Heart Renaissance. Rev. Cardiovasc. Med. 2024, 25, 91. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aird, W.C. Discovery of the cardiovascular system: From Galen to William Harvey. J. Thromb. Haemost. 2011, 9 (Suppl. S1), 118–129. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, S.; Ghaffari, F.; Heydarirad, G.; Alizadeh, M. Galen’s place in Avicenna’s The Canon of Medicine: Respect, confirmation and criticism. J. Integr. Med. 2020, 18, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Reverón, R.R. Herophilus and Erasistratus, pioneers of human anatomical dissection. Vesalius 2014, 20, 55–58. [Google Scholar] [PubMed]
- Ghosh, S.K. Human cadaveric dissection: A historical account from ancient Greece to the modern era. Anat. Cell Biol. 2015, 48, 153–169. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Conti, A.A.; Paternostro, F. Anatomical study in the Western world before the Middle Ages: Historical evidence. Acta Biomed. 2019, 90, 523–525. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Loukas, M.; Youssef, P.; Gielecki, J.; Walocha, J.; Natsis, K.; Tubbs, R.S. History of cardiac anatomy: A comprehensive review from the Egyptians to today. Clin. Anat. 2016, 29, 270–284. [Google Scholar] [CrossRef] [PubMed]
- Allen, T.G. The Book of the Dead: Becoming God in Ancient Egypt; University of Chicago Press: Chicago, IL, USA, 2010. [Google Scholar]
- Nunn, J.F. Ancient Egyptian Medicine; University of Oklahoma Press: Norman, OK, USA, 2011. [Google Scholar]
- Isidro, A.; Gonzálvez, L.M.; Huber, B. Mummified heart of an ancient Egyptian. Rev. Esp. Cardiol. (Engl Ed). 2014, 67, 407. [Google Scholar] [CrossRef] [PubMed]
- Mavrodi, A.; Paraskevas, G. Morphology of the heart associated with its function as conceived by ancient Greeks. Int. J. Cardiol. 2014, 172, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Snell, B. Scenes from Greek Drama; University of California Press: Berkeley, CA, USA, 2023; ISBN 978-0520319080. [Google Scholar]
- Snell, B. The Discovery of the Mind: The Greek Origins of European Thought; Harper & Row: New York, NY, USA, 2002. [Google Scholar]
- Harrison, N.A.; Critchley, H.D. Affective neuroscience and psychiatry. Br. J. Psychiatry 2007, 191, 192–194. [Google Scholar] [CrossRef] [PubMed]
- Lykouras, E.; Poulakou-Rebelakou, E.; Ploumpidis, D.N. Searching the seat of the soul in Ancient Greek and Byzantine medical literature. Acta Cardiol. 2010, 65, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Holweck, F. “The Five Sacred Wounds” The Catholic Encyclopedia; Robert Appleton Company: New York, NY, USA, 1912; Volume 15. [Google Scholar]
- Jonsen, A.R. Theological ethics, moral philosophy, and public moral discourse. Kennedy Inst. Ethics J. 1994, 4, 1–11. [Google Scholar] [CrossRef] [PubMed]
- King, U. ‘Consumed by Fire from Within’: Teilhard de Chardin’s Pan-christic Mysticism in Relation to the Catholic Tradition. Heythrop J. 2002, 40, 456–477. [Google Scholar] [CrossRef]
- Nasr, S.H. Science and Civilization in Islam; Harvard University Press: Cambridge, MA, USA, 1968. [Google Scholar]
- Sachedina, A. Islamic Biomedical Ethics: Principles and Application; Oxford University Press: Oxford, UK, 2009. [Google Scholar]
- Jakobovits, I. Jewish Medical Ethics: A Comparative and Historical Study of the Jewish Religious Attitude to Medicine and Its Practice; Bloch Publishing: New York, NY, USA, 1959. [Google Scholar]
- Miles, S.H. The Hippocratic Oath and the Ethics of Medicine; Oxford University Press: Oxford, UK, 2005. [Google Scholar]
- Calhoun, A.W. Primum Non Nocere. Simul. Healthc. 2020, 15, 301–302. [Google Scholar] [CrossRef] [PubMed]
- Park, K. Secrets of Women: Gender, Generation, and the Origins of Human Dissection; Zone Books: New York, NY, USA, 2006. [Google Scholar]
- Bynum, C.W. The Resurrection of the Body in Western Christianity, 200–1336 (American Lectures on the History of Religions); Columbia University Press: New York, NY, USA, 2017; ISBN 9780231185295. [Google Scholar]
- Rosner, F. Biomedical Ethics and Jewish Law; Ktav Pub & Distributors Inc.: New York, NY, USA, 2001; ISBN 978-0881257014. [Google Scholar]
- Haddad, F.S. Perspectives of the history of anesthesia. Middle East. J. Anaesthesiol. 1997, 14, 3–6. [Google Scholar] [PubMed]
- Shamji, F.M.; Waddell, K.; Beauchamp, G. The History and Evolution of Surgical Instruments in Thoracic Surgery. Thorac. Surg. Clin. 2021, 31, 449–461. [Google Scholar] [CrossRef] [PubMed]
- Best, M.; Neuhauser, D. Ignaz Semmelweis and the birth of infection control. BMJ Qual. Saf. 2004, 13, 233–234. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vesalius, A. De Humani Corporis Fabrica; Oporinus: Basel, Switzerland, 1543. [Google Scholar]
- Carlino, A. Books of the Body: Anatomical Ritual and Renaissance Learning; University of Chicago Press: Chicago, IL, USA, 1999. [Google Scholar]
- Paré, A. The Collected Works of Ambroise Paré; Johnson, T., Translator; Dover Publications: New York, NY, USA, 1968. [Google Scholar]
- Bhadriraju, K.B.; Goodwin, R. “I Dressed Him, God Cured Him”: Ambroise Paré, the Father of Surgery. Cureus 2024, 16, e72717. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lorkowski, J.; Pokorski, M. Medical Records: A Historical Narrative. Biomedicines 2022, 10, 2594. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Harvey, W. Exercitatio Anatomica de Motu Cordis et Sanguinis in Animalibus; William Fitzer: Frankfurt, Germany, 1628. [Google Scholar]
- Ritz, K.; van Buchem, M.A.; Daemen, M.J. The heart-brain connection: Mechanistic insights and models. Neth. Heart J. 2013, 21, 55–57. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Porter, R. The Enlightenment: Britain and the Creation of the Modern World; Penguin Books: London, UK, 1997. [Google Scholar]
- Morgagni, G.B. The Seats and Causes of Diseases Investigated by Anatomy; Remondini: Venice, Italy, 1761. [Google Scholar]
- Ghosh, S.K. Giovanni Battista Morgagni (1682–1771): Father of pathologic anatomy and pioneer of modern medicine. Anat. Sci. Int. 2017, 92, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Atalić, B. 200th Anniversary of the Beginning of Clinical Application of the Laennec’s Stethoscope in 1819. Acta Med.-Hist. Adriat. 2019, 17, 9–18. [Google Scholar] [PubMed]
- Rehn, L. Ueber Penetrirende Herzwunden und Herznaht; The Royal College of Surgeons of England: London, UK, 1897. [Google Scholar]
- Blatchford, J.W. 3rd. Ludwig Rehn: The first successful cardiorrhaphy. Ann. Thorac. Surg. 1985, 39, 492–495. [Google Scholar] [CrossRef] [PubMed]
- Livesay, J.J. A History of Cardiac Surgery: An Adventurous Voyage from Antiquity to the Artificial Heart. Tex. Heart Inst. J. 2020, 47, 339–341. [Google Scholar] [CrossRef] [PubMed Central]
- Schlich, T. The Origins of Modern Surgery: An Introduction; Routledge: New York, NY, USA, 2010. [Google Scholar]
- Jonsen, A.R. A Short History of Medical Ethics; Oxford University Press: Oxford, UK, 2000. [Google Scholar]
- Angelos, P.; Taylor, L.J.; Roggin, K.; Schwarze, M.L.; Vaughan, L.M.; Wightman, S.C.; Sade, R.M. Decision-Making in Surgery. Ann. Thorac. Surg. 2024, 117, 1087–1094. [Google Scholar] [CrossRef] [PubMed]
- Beecher, H.K. Ethics and clinical research. N. Engl. J. Med. 1966, 274, 1354–1360. [Google Scholar] [CrossRef] [PubMed]
- Moreno, J.D.; Schmidt, U.; Joffe, S. The Nuremberg Code 70 Years Later. JAMA 2017, 318, 795–796. [Google Scholar] [CrossRef] [PubMed]
- Goodyear, M.D.; Krleza-Jeric, K.; Lemmens, T. The Declaration of Helsinki. BMJ 2007, 335, 624–625. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Faden, R.R.; Beauchamp, T.L. A History and Theory of Informed Consent; Oxford University Press: New York, NY, USA, 1986. [Google Scholar]
- Byrom, A. Heart matters--a history. Pract. Midwife 2016, 19, 5. [Google Scholar] [PubMed]
- Davies, M.K.; Hollman, A. History of cardiac surgery. Heart 2002, 87, 509. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Karl, T.R.; Martin, G.R.; Jacobs, J.P.; Wernovsky, G. Key events in the history of cardiac surgery and paediatric cardiology. Cardiol. Young 2017, 27, 2029–2062. [Google Scholar] [CrossRef] [PubMed]
- Mol, A. The Body Multiple: Ontology in Medical Practice; Duke University Press: Durham, UK, 2002. [Google Scholar]
- Morris, D.B. Illness and Culture in the Postmodern Age; University of California Press: Berkeley, CA, USA, 1998. [Google Scholar]
- Lena, T.; Amabile, A.; Morrison, A.; Torregrossa, G.; Geirsson, A.; Tesler, U.F.; John, H. Gibbon and the development of the heart-lung machine: The beginnings of open cardiac surgery. J. Card. Surg. 2022, 37, 4199–4201. [Google Scholar] [CrossRef] [PubMed]
- Fox, R.C.; Swazey, J.P. The Courage to Fail: A Social View of Organ Transplants and Dialysis; University of Chicago Press: Chicago, IL, USA, 1978. [Google Scholar]
- Parsons, T. The Social System; Free Press: New York, NY, USA, 2010. [Google Scholar]
- Holm, A.M.; Fedson, S.; Courtwright, A.; Olland, A.; Bryce, K.; Kanwar, M.; Sweet, S.; Egan, T.; Lavee, J. International society for heart and lung transplantation statement on transplant ethics. J. Heart Lung Transplant. 2022, 41, 1307–1308. [Google Scholar] [CrossRef] [PubMed]
- Potts, M. Morals, metaphysics, and heart transplantation: Reflections on Richard Selzer’s “Whither Thou Goest”. Perspect. Biol. Med. 1998, 41, 212–223. [Google Scholar] [CrossRef] [PubMed]
- DeMartino, E.S.; Wordingham, S.E.; Stulak, J.M.; Boilson, B.A.; Fuechtmann, K.R.; Singh, N.; Sulmasy, D.P.; Pajaro, O.E.; Mueller, P.S. Ethical Analysis of Withdrawing Total Artificial Heart Support. Mayo Clin. Proc. 2017, 92, 719–725. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Roggi, S.; Picozzi, M. Is Left Ventricular Assist Device Deactivation Ethically Acceptable? A Study on the Euthanasia Debate. HEC Forum 2021, 33, 325–343. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hansen, C.; Stevens, M.C. Be still, my beating heart: Reading pulselessness from Shakespeare to the artificial heart. Med. Humanit. 2021, 47, 344–353. [Google Scholar] [CrossRef] [PubMed]
- Miles, S.H.; Siegler, M.; Schiedermayer, D.L.; Lantos, J.D.; La Puma, J. The total artificial heart: An ethics perspective on current clinical research and deployment. Chest 1988, 94, 409–413. [Google Scholar] [CrossRef] [PubMed]
- Barić, D. Why pulsatility still matters: A review of current knowledge. Croat. Med. J. 2014, 55, 609–620. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Santoro, G.; Wood, M.D.; Merlo, L.; Anastasi, G.P.; Tomasello, F.; Germanò, A. The anatomic location of the soul from the heart, through the brain, to the whole body, and beyond: A journey through Western history, science, and philosophy. Neurosurgery 2009, 65, 633–643, discussion 643. [Google Scholar] [CrossRef] [PubMed]
- Biglino, G.; Layton, S.; Wray, J. Beyond Heart Symbolism: Artistic Representation of Narratives of Congenital Heart Disease. JAMA 2017, 318, 1740–1742. [Google Scholar] [CrossRef] [PubMed]
- Merleau-Ponty, M. Phenomenology of Perception; Routledge: London, UK, 1962. [Google Scholar]
- Damasio, A.R. Descartes’ Error: Emotion, Reason, and the Human Brain; Putnam: New York, NY, USA, 1994. [Google Scholar]
- Armour, J.A. Neurocardiology: Anatomical and Functional Principles; Oxford University Press: New York, NY, USA, 2003; ISBN 0195073045. [Google Scholar]
- Critchley, H.D.; Harrison, N.A. Visceral influences on brain and behavior. Neuron 2013, 77, 624–638. [Google Scholar] [CrossRef] [PubMed]
- Pearsall, P.; Schwartz, G.E.; Russek, L.G. Changes in heart transplant recipients that parallel the personalities of their donors. Integr. Med. 2000, 2, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Al-Juhani, A.; Imran, M.; Aljaili, Z.K.; Alzhrani, M.M.; Alsalman, R.A.; Ahmed, M.; Ali, D.K.; Fallatah, M.I.; Yousuf, H.M.; Dajani, L.M. Beyond the Pump: A Narrative Study Exploring Heart Memory. Cureus 2024, 16, e59385. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Svenaeus, F. Organ transplantation and personal identity: How does loss and change of organs affect the self? J. Med. Philos. 2012, 37, 139–158. [Google Scholar] [CrossRef] [PubMed]
- Charon, R. Narrative Medicine: Honoring the Stories of Illness; Oxford University Press: New York, NY, USA, 2001. [Google Scholar]
- Goli, F. Biosemiotic medicines: Symbolic formulations for placebo enhancements. J. Educ. Health Promot. 2024, 13, 156. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- MacIntyre, A. After Virtue: A Study in Moral Theory; University of Notre Dame Press: Notre Dame, IN, USA, 2013. [Google Scholar]
- Zhou, P.; Critchley, H.; Nagai, Y.; Wang, C. Divergent Conceptualization of Embodied Emotions in the English and Chinese Languages. Brain Sci. 2022, 12, 911. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Murthy, A.R.; Singh, R.H. Ayurvedic concept of hridroga its present relevance. Anc. Sci. Life 1993, 12, 403–413. [Google Scholar] [PubMed] [PubMed Central]
- Vedam, R.; Pansare, T.A.; Narula, J. Contributions of ancient Indian knowledge to modern medicine and cardiology. Indian Heart J. 2021, 73, 531–534. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Menon, M.; Shukla, A. Understanding hypertension in the light of Ayurveda. J. Ayurveda Integr. Med. 2018, 9, 302–307. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leivaditis, V.; Mavroudes, G.; Mulita, F.; Baikoussis, N.G.; Papatriantafyllou, A.; Garantzioti, V.; Tasios, K.; Tchabashvili, L.; Litsas, D.; Katsakiori, P.; et al. Opening the Sacred Chamber: The Cultural and Ethical Odyssey of Cardiac Surgery. J. Cardiovasc. Dev. Dis. 2025, 12, 378. https://doi.org/10.3390/jcdd12100378
Leivaditis V, Mavroudes G, Mulita F, Baikoussis NG, Papatriantafyllou A, Garantzioti V, Tasios K, Tchabashvili L, Litsas D, Katsakiori P, et al. Opening the Sacred Chamber: The Cultural and Ethical Odyssey of Cardiac Surgery. Journal of Cardiovascular Development and Disease. 2025; 12(10):378. https://doi.org/10.3390/jcdd12100378
Chicago/Turabian StyleLeivaditis, Vasileios, Georgios Mavroudes, Francesk Mulita, Nikolaos G. Baikoussis, Athanasios Papatriantafyllou, Vasiliki Garantzioti, Konstantinos Tasios, Levan Tchabashvili, Dimitrios Litsas, Paraskevi Katsakiori, and et al. 2025. "Opening the Sacred Chamber: The Cultural and Ethical Odyssey of Cardiac Surgery" Journal of Cardiovascular Development and Disease 12, no. 10: 378. https://doi.org/10.3390/jcdd12100378
APA StyleLeivaditis, V., Mavroudes, G., Mulita, F., Baikoussis, N. G., Papatriantafyllou, A., Garantzioti, V., Tasios, K., Tchabashvili, L., Litsas, D., Katsakiori, P., Assimakopoulos, S. F., Nikolakopoulos, K., Antzoulas, A., Liolis, E., Papadoulas, S., Koletsis, E., & Dahm, M. (2025). Opening the Sacred Chamber: The Cultural and Ethical Odyssey of Cardiac Surgery. Journal of Cardiovascular Development and Disease, 12(10), 378. https://doi.org/10.3390/jcdd12100378









