Sex Differences in Outcomes of Patients with an Implantable Cardioverter-Defibrillator for the Secondary Prevention of Sudden Cardiac Death
Abstract
1. Introduction
2. Materials and Methods
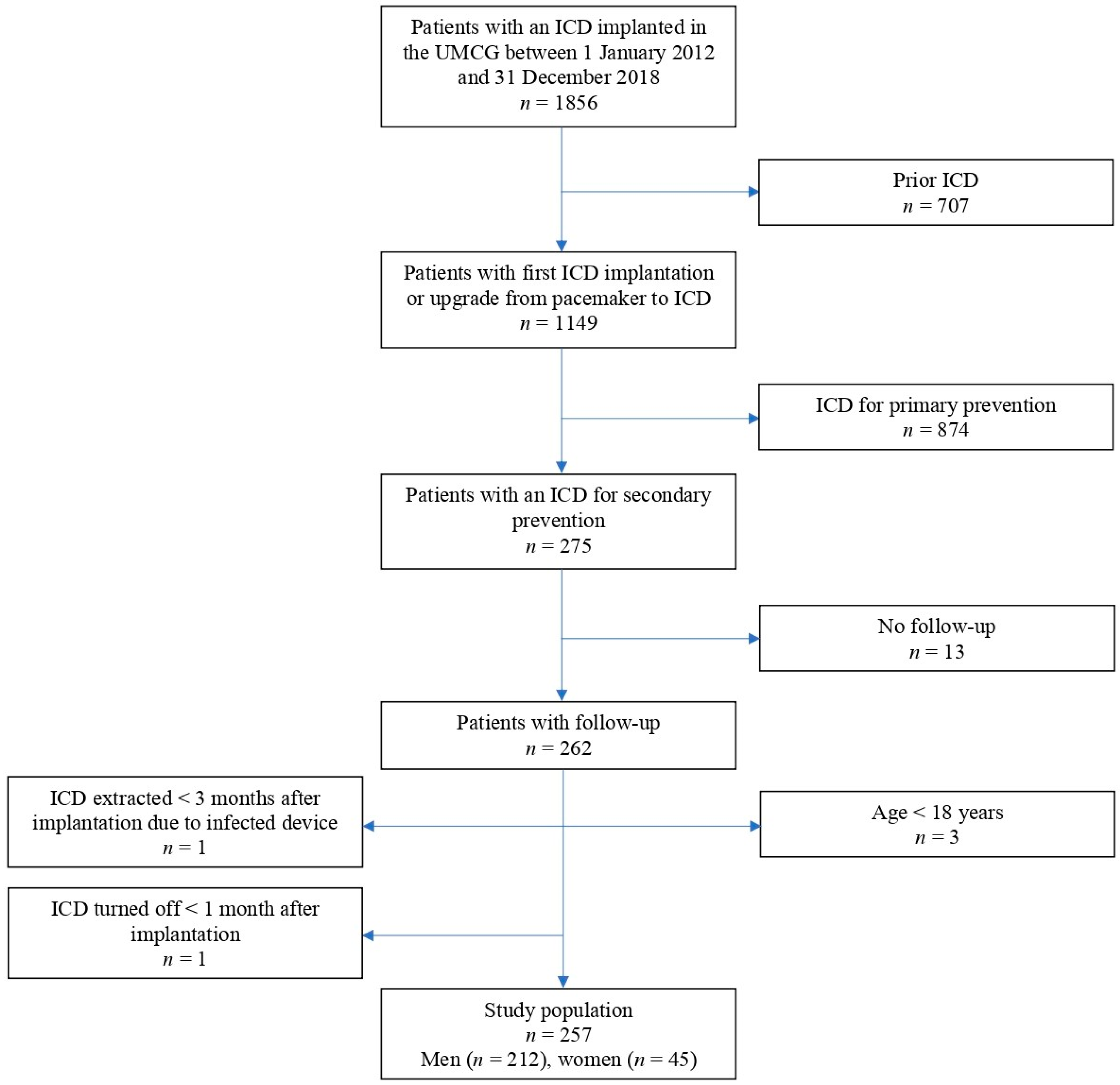
2.1. Study Population
2.2. Data Acquisition and Outcomes
2.3. ICD Programming
2.4. Statistical Analysis
3. Results
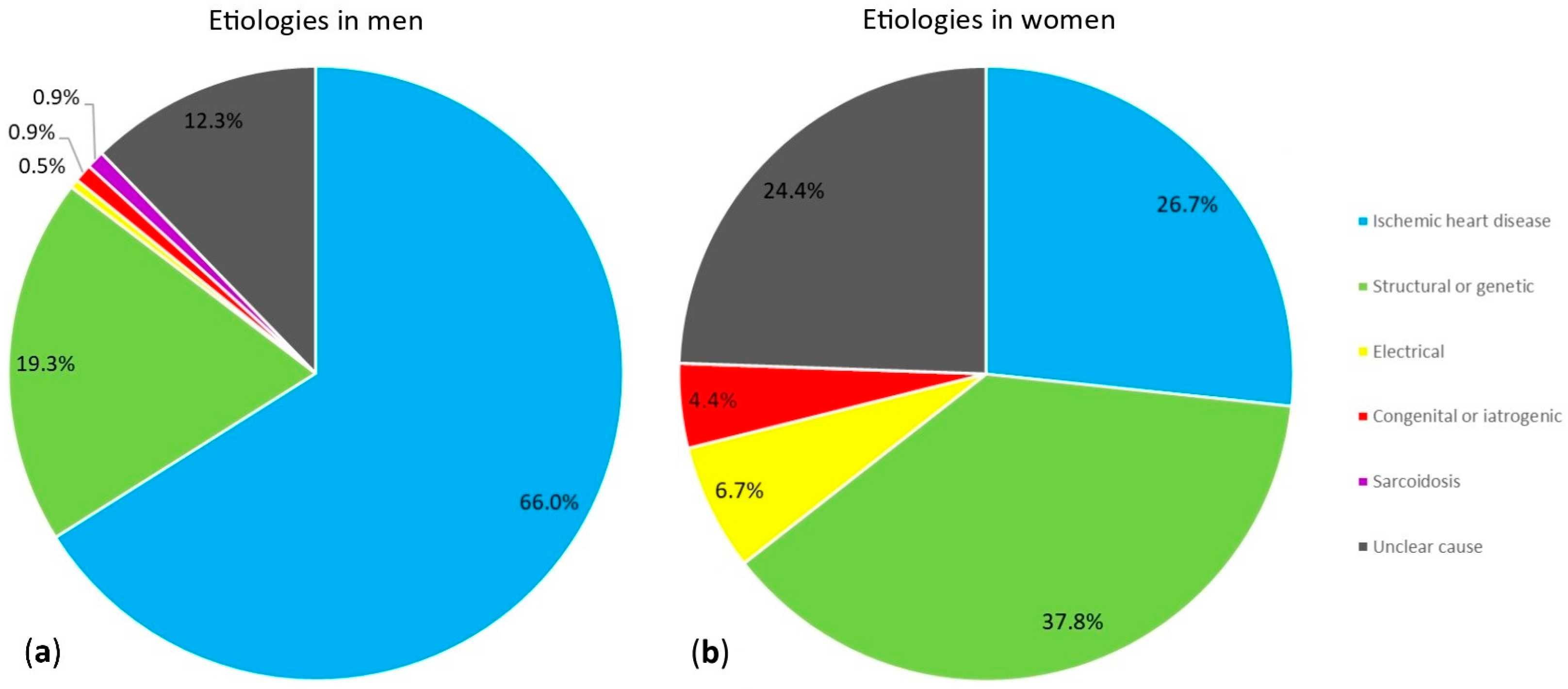
3.1. Characteristics of Patient Population
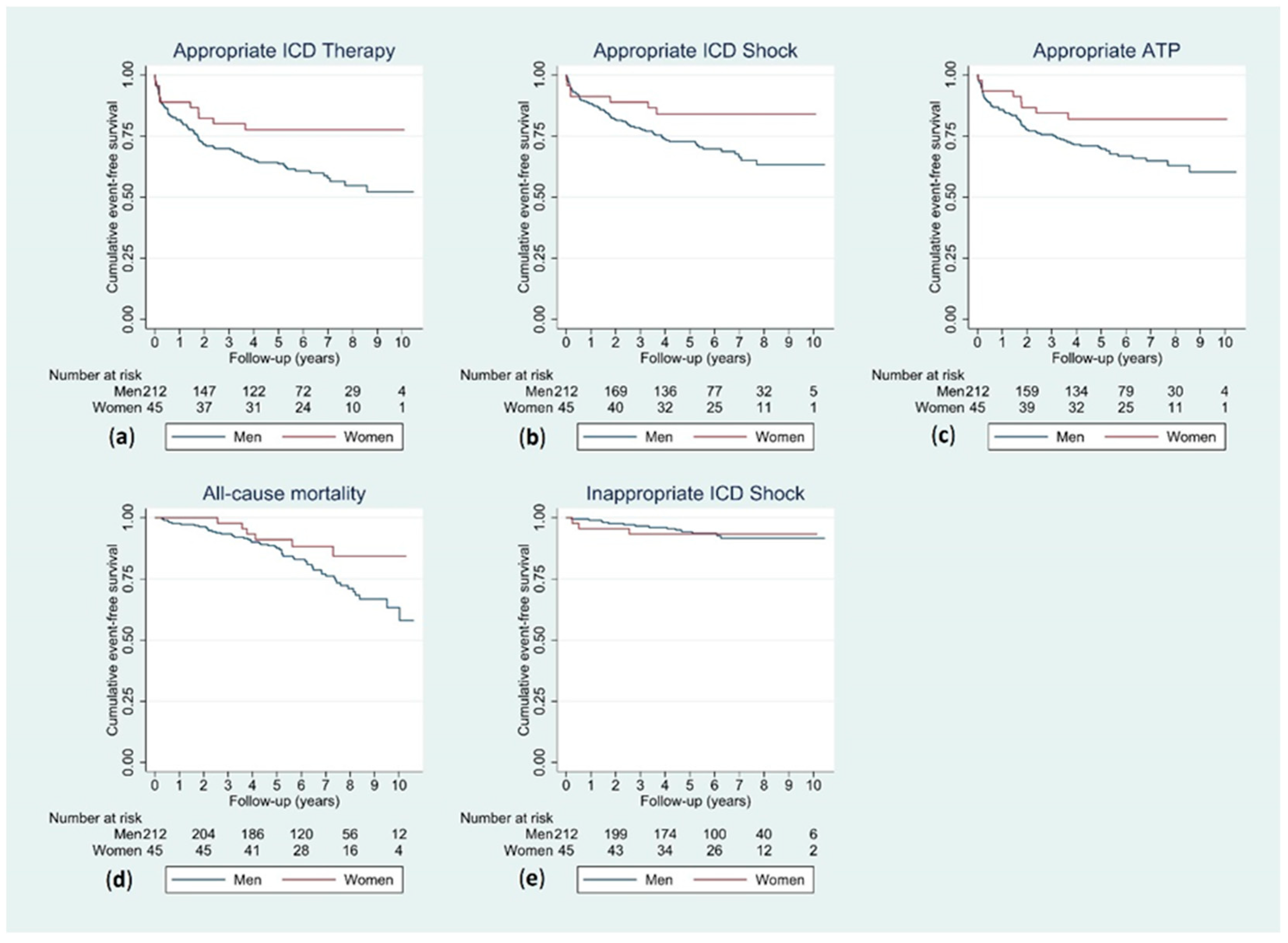
3.2. Outcomes during Follow-Up
3.3. Sex Differences in Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Srinivasan, N.T.; Schilling, R.J. Sudden Cardiac Death and Arrhythmias. Arrhythm. Electrophysiol. Rev. 2018, 7, 111–117. [Google Scholar] [CrossRef]
- Yousuf, O.; Chrispin, J.; Tomaselli, G.F.; Berger, R.D. Clinical management and prevention of sudden cardiac death. Circ. Res. 2015, 116, 2020–2040. [Google Scholar] [CrossRef]
- Zeppenfeld, K.; Tfelt-Hansen, J.; de Riva, M.; Winkel, B.G.; Behr, E.R.; Blom, N.A.; Charron, P.; Corrado, D.; Dagres, N.; de Chillou, C.; et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur. Heart J. 2022, 43, 3997–4126. [Google Scholar]
- Connolly, S.J.; Hallstrom, A.P.; Cappato, R.; Schron, E.B.; Kuck, K.H.; Zipes, D.P.; Greene, H.L.; Boczor, S.; Domanski, M.; Follmann, D.; et al. Meta-analysis of the implantable cardioverter defibrillator secondary prevention trials. AVID, CASH and CIDS studies. Antiarrhythmics vs Implantable Defibrillator study. Cardiac Arrest Study Hamburg. Canadian Implantable Defibrillator Study. Eur. Heart J. 2000, 21, 2071–2078. [Google Scholar] [CrossRef]
- Butters, A.; Arnott, C.; Sweeting, J.; Winkel, B.G.; Semsarian, C.; Ingles, J. Sex Disparities in Sudden Cardiac Death. Circ. Arrhythm. Electrophysiol. 2021, 14, e009834. [Google Scholar] [CrossRef]
- MacFadden, D.R.; Tu, J.V.; Chong, A.; Austin, P.C.; Lee, D.S. Evaluating sex differences in population-based utilization of implantable cardioverter-defibrillators: Role of cardiac conditions and noncardiac comorbidities. Heart Rhythm. 2009, 6, 1289–1296. [Google Scholar] [CrossRef]
- Ingelaere, S.; Hoffmann, R.; Guler, I.; Vijgen, J.; Mairesse, G.H.; Blankoff, I.; Vandekerckhove, Y.; le Polain de Waroux, J.B.; Vandenberk, B.; Willems, R. Inequality between women and men in ICD implantation. Int. J. Cardiol. Heart Vasc. 2022, 41, 101075. [Google Scholar] [CrossRef]
- Curtis, L.H.; Al-Khatib, S.M.; Shea, A.M.; Hammill, B.G.; Hernandez, A.F.; Schulman, K.A. Sex differences in the use of implantable cardioverter-defibrillators for primary and secondary prevention of sudden cardiac death. JAMA 2007, 298, 1517–1524. [Google Scholar] [CrossRef]
- MacFadden, D.R.; Crystal, E.; Krahn, A.D.; Mangat, I.; Healey, J.S.; Dorian, P.; Birnie, D.; Simpson, C.S.; Khaykin, Y.; Pinter, A.; et al. Sex differences in implantable cardioverter-defibrillator outcomes: Findings from a prospective defibrillator database. Ann. Intern. Med. 2012, 156, 195–203. [Google Scholar] [CrossRef]
- Saxena, S.; Goldenberg, I.; McNitt, S.; Hsich, E.; Kutyifa, V.; Bragazzi, N.L.; Polonsky, B.; Aktas, M.K.; Huang, D.T.; Rosero, S.; et al. Sex Differences in the Risk of First and Recurrent Ventricular Tachyarrhythmias Among Patients Receiving an Implantable Cardioverter-Defibrillator for Primary Prevention. JAMA Netw. Open 2022, 5, e2217153. [Google Scholar] [CrossRef]
- Wijers, S.C.; van der Kolk, B.Y.; Tuinenburg, A.E.; Doevendans, P.A.; Vos, M.A.; Meine, M. Implementation of guidelines for implantable cardioverter-defibrillator therapy in clinical practice: Which patients do benefit? Neth. Heart J. 2013, 21, 274–283. [Google Scholar] [CrossRef]
- Wilson, D.; Shi, B.; Harding, S.; Lever, N.; Larsen, P. Implantable cardioverter-defibrillators: A long-term view. Intern. Med. J. 2012, 42, 554–561. [Google Scholar] [CrossRef]
- Styles, K.; Sapp, J., Jr.; Gardner, M.; Gray, C.; Abdelwahab, A.; MacIntyre, C.; Gao, D.; Al-Harbi, M.; Doucette, S.; Theriault, C.; et al. The influence of sex and age on ventricular arrhythmia in a population-based registry. Int. J. Cardiol. 2017, 244, 169–174. [Google Scholar] [CrossRef]
- Noordman, A.B.P.; Rienstra, M.; Blaauw, Y.; Mulder, B.A.; Maass, A.H. Appropriate Implantable Cardioverter-Defibrillator Therapy in Patients with Ventricular Arrhythmia of Unclear Cause in Secondary Prevention of Sudden Cardiac Death. J. Clin. Med. 2023, 12, 4479. [Google Scholar] [CrossRef]
- Bergau, L.; Seegers, J.; Zabel, M. Sex differences in ICD benefit. J. Electrocardiol. 2014, 47, 869–873. [Google Scholar] [CrossRef]
- Santangeli, P.; Pelargonio, G.; Dello Russo, A.; Casella, M.; Bisceglia, C.; Bartoletti, S.; Santarelli, P.; Di Biase, L.; Natale, A. Gender differences in clinical outcome and primary prevention defibrillator benefit in patients with severe left ventricular dysfunction: A systematic review and meta-analysis. Heart Rhythm. 2010, 7, 876–882. [Google Scholar] [CrossRef]
- van der Lingen, A.C.J.; Theuns, D.; Rijnierse, M.T.; Becker, M.A.J.; van de Ven, P.M.; van Rossum, A.C.; van Halm, V.P.; Kemme, M.J.B.; Yap, S.C.; Allaart, C.P. Sex-specific differences in outcome and risk stratification of ventricular arrhythmias in implantable cardioverter defibrillator patients. ESC Heart Fail. 2021, 8, 3726–3736. [Google Scholar] [CrossRef] [PubMed]
- Skjelbred, T.; Rajan, D.; Svane, J.; Lynge, T.H.; Tfelt-Hansen, J. Sex differences in sudden cardiac death in a nationwide study of 54 028 deaths. Heart 2022, 108, 1012–1018. [Google Scholar] [CrossRef]
- Ghanbari, H.; Dalloul, G.; Hasan, R.; Daccarett, M.; Saba, S.; David, S.; Machado, C. Effectiveness of implantable cardioverter-defibrillators for the primary prevention of sudden cardiac death in women with advanced heart failure: A meta-analysis of randomized controlled trials. Arch. Intern. Med. 2009, 169, 1500–1506. [Google Scholar] [CrossRef] [PubMed]
- Barra, S.; Narayanan, K.; Garcia, R.; Marijon, E. Time to revisit implantable cardioverter-defibrillator implantation criteria in women. Eur. Heart J. 2021, 42, 1110–1112. [Google Scholar] [CrossRef] [PubMed]
- Bardy, G.H.; Lee, K.L.; Mark, D.B.; Poole, J.E.; Packer, D.L.; Boineau, R.; Domanski, M.; Troutman, C.; Anderson, J.; Johnson, G.; et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N. Engl. J. Med. 2005, 352, 225–237. [Google Scholar] [CrossRef] [PubMed]
- Russo, A.M.; Poole, J.E.; Mark, D.B.; Anderson, J.; Hellkamp, A.S.; Lee, K.L.; Johnson, G.W.; Domanski, M.; Bardy, G.H. Primary prevention with defibrillator therapy in women: Results from the Sudden Cardiac Death in Heart Failure Trial. J. Cardiovasc. Electrophysiol. 2008, 19, 720–724. [Google Scholar] [CrossRef] [PubMed]
- Wathen, M.S.; Sweeney, M.O.; DeGroot, P.J.; Stark, A.J.; Koehler, J.L.; Chisner, M.B.; Machado, C.; Adkisson, W.O. Shock reduction using antitachycardia pacing for spontaneous rapid ventricular tachycardia in patients with coronary artery disease. Circulation 2001, 104, 796–801. [Google Scholar] [CrossRef] [PubMed]
| Variable | Men (n = 212) | Women (n = 45) | p-Value |
|---|---|---|---|
| Age (years) | 64.9 (54.8–72.1) | 57.7 (47.3–66.9) | 0.003 |
| Ischemic heart disease | 140 (66.0%) | 12 (26.7%) | <0.001 |
| Non-ischemic heart disease | 46 (21.7%) | 22 (48.9%) | <0.001 |
| Ventricular arrhythmia of unclear cause | 26 (12.3%) | 11 (24.4%) | 0.035 |
| Presenting ventricular arrhythmia | 0.651 | ||
| VF | 144 (67.9%) | 29 (64.4%) | |
| Sustained VT | 68 (32.1%) | 16 (35.6%) | |
| BMI (kg/m2) | 26.5 (24.5–29.2) | 27.0 (23.9–34.8) | 0.423 |
| NYHA class | 1.000 | ||
| I or II | 147 (69.3%) | 28 (62.2%) | |
| III or IV | 25 (11.8%) | 5 (11.1%) | |
| Medical history | |||
| Myocardial infarction | 126 (59.4%) | 11 (24.4%) | <0.001 |
| DM | 40 (18.9%) | 8 (17.8%) | 0.865 |
| Syncope | 18 (8.5%) | 6 (13.3%) | 0.394 |
| Prior heart surgery | 65 (30.7%) | 1 (2.2%) | <0.001 |
| Atrial fibrillation | 74 (34.9%) | 12 (26.7%) | 0.287 |
| Non-sustained VT | 40 (18.9%) | 7 (15.6%) | 0.602 |
| CAD | 145 (68.4%) | 12 (26.7%) | <0.001 |
| Echocardiography | |||
| LVEF (%) | 43 (34–53) | 47 (35–58) | 0.129 |
| Electrocardiography | |||
| Rhythm | 0.024 | ||
| Sinus rhythm | 179 (84.4%) | 42 (93.3%) | |
| Atrial fibrillation | 27 (12.7%) | 1 (2.2%) | |
| Atrial flutter | 2 (0.9%) | 0 (0.0%) | |
| Pacemaker | 1 (0.5%) | 2 (4.4%) | |
| QRS fragmentation † | 79 (37.3%) | 11 (24.4%) | 0.214 |
| Laboratory values | |||
| eGFR (mL/min/1.73 m2) | 76 ± 23 | 83 ± 24 | 0.101 |
| Medication at baseline | |||
| ACE-I/ARB | 99 (46.7%) | 14 (31.1%) | 0.117 |
| β-blocker | 106 (50.0%) | 19 (42.2%) | 0.606 |
| Calcium antagonist | 39 (18.4%) | 4 (8.9%) | 0.166 |
| Diuretic | 50 (23.6%) | 6 (13.3%) | 0.191 |
| Statin | 100 (47.2%) | 11 (24.4%) | 0.012 |
| MRA | 19 (9.0%) | 3 (6.7%) | 1.000 |
| Class 3 antiarrhythmic drugs | 13 (6.1%) | 2 (4.4%) | 1.000 |
| Digoxin | 8 (3.8%) | 1 (2.2%) | 1.000 |
| Outcomes | Men (n = 212) | Women (n = 45) |
|---|---|---|
| Appropriate ICD therapy | 85 (40.1%) | 10 (22.2%) |
| Appropriate shock | 65 (30.7%) | 7 (15.6%) |
| Appropriate ATP | 70 (33.0%) | 8 (17.8%) |
| All-cause mortality | 53 (25.0%) | 6 (13.3%) |
| Cardiac cause of death | 13 (6.1%) | 1 (2.2%) |
| Non-cardiac cause of death | 11 (5.2%) | 3 (6.7%) |
| Unknown cause of death | 29 (13.7%) | 2 (4.4%) |
| Inappropriate ICD therapy | 21 (9.9%) | 5 (11.1%) |
| Inappropriate shocks | 14 (6.6%) | 3 (6.7%) |
| Complications | 16 (7.5%) | 4 (8.9%) |
| Lead failure | 11 (5.2%) | 1 (2.2%) |
| Perioperative complications | 6 (2.8%) | 2 (4.4%) |
| Infection | 0 (0.0%) | 0 (0.0%) |
| Other complications | 0 (0.0%) | 1 (2.2%) |
| Univariable | Adjusted | |||
|---|---|---|---|---|
| Outcomes | HR (95% CI) | p-Value | HR (95% CI) | p-Value |
| Appropriate therapy | 0.48 (0.25–0.93) | 0.030 | 0.44 (0.20–0.95) † | 0.036 |
| Appropriate shock | 0.45 (0.21–0.99) | 0.048 | 0.50 (0.21–1.20) † | 0.122 |
| Appropriate ATP | 0.48 (0.23–0.99) | 0.046 | 0.40 (0.16–1.00) † | 0.049 |
| All-cause mortality | 0.48 (0.20–1.11) | 0.086 | 1.12 (0.45–2.79) ‡ | 0.805 |
| Inappropriate shock | 0.99 (0.28–3.43) | 0.982 | 1.28 (0.33–4.92) § | 0.717 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noordman, A.B.P.; Rienstra, M.; Blaauw, Y.; Mulder, B.A.; Maass, A.H. Sex Differences in Outcomes of Patients with an Implantable Cardioverter-Defibrillator for the Secondary Prevention of Sudden Cardiac Death. J. Cardiovasc. Dev. Dis. 2024, 11, 116. https://doi.org/10.3390/jcdd11040116
Noordman ABP, Rienstra M, Blaauw Y, Mulder BA, Maass AH. Sex Differences in Outcomes of Patients with an Implantable Cardioverter-Defibrillator for the Secondary Prevention of Sudden Cardiac Death. Journal of Cardiovascular Development and Disease. 2024; 11(4):116. https://doi.org/10.3390/jcdd11040116
Chicago/Turabian StyleNoordman, Alwin B. P., Michiel Rienstra, Yuri Blaauw, Bart A. Mulder, and Alexander H. Maass. 2024. "Sex Differences in Outcomes of Patients with an Implantable Cardioverter-Defibrillator for the Secondary Prevention of Sudden Cardiac Death" Journal of Cardiovascular Development and Disease 11, no. 4: 116. https://doi.org/10.3390/jcdd11040116
APA StyleNoordman, A. B. P., Rienstra, M., Blaauw, Y., Mulder, B. A., & Maass, A. H. (2024). Sex Differences in Outcomes of Patients with an Implantable Cardioverter-Defibrillator for the Secondary Prevention of Sudden Cardiac Death. Journal of Cardiovascular Development and Disease, 11(4), 116. https://doi.org/10.3390/jcdd11040116






