Evaluation of Image Quality for High Heart Rates for Coronary Computed Tomographic Angiography with Advancement in CT Technology: The CONVERGE Registry
Abstract
:1. Introduction
2. Methods
2.1. Patient Population
2.2. Patient Preparation
2.3. Imaging Acquisition
2.4. Image Reconstruction
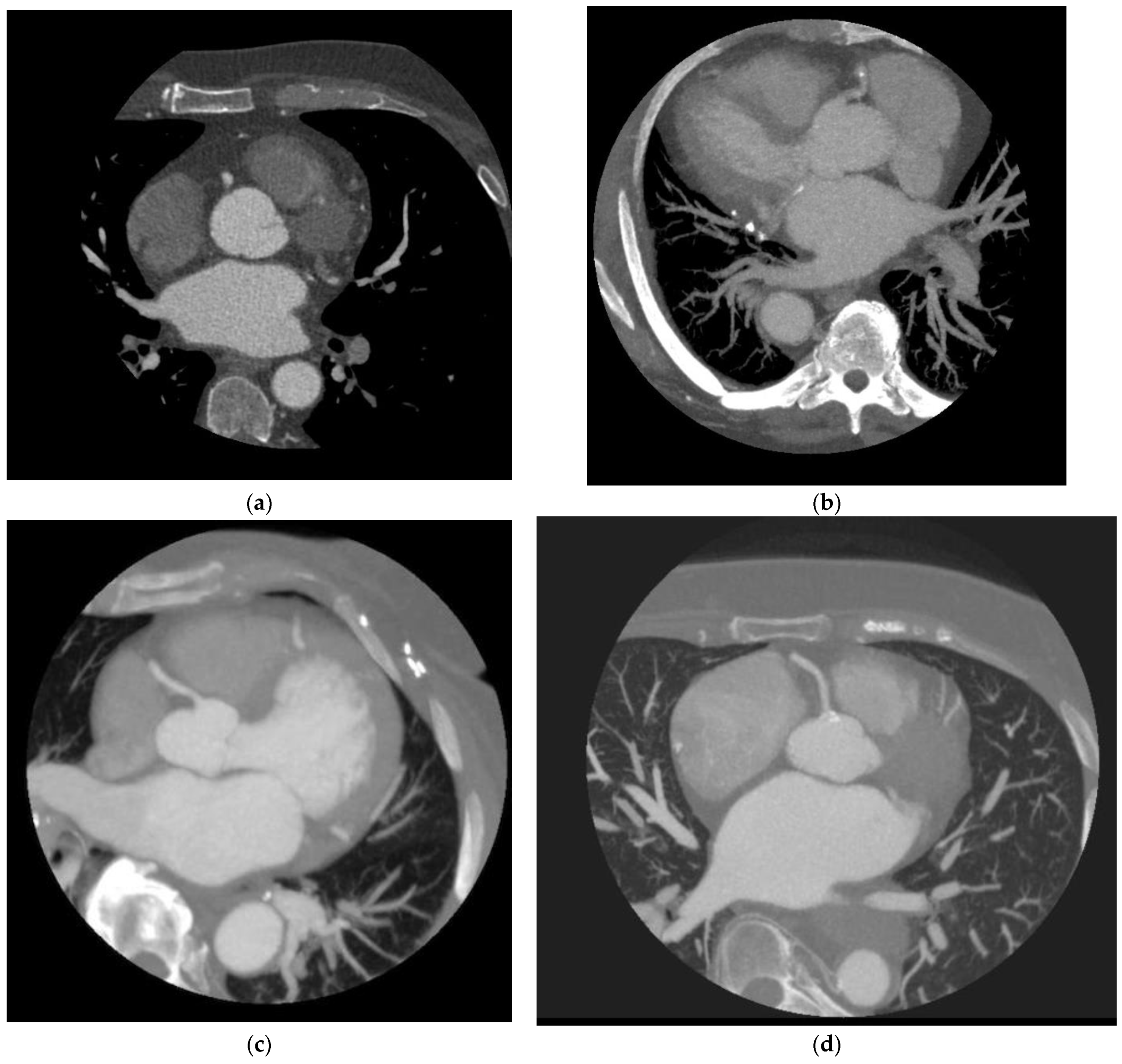
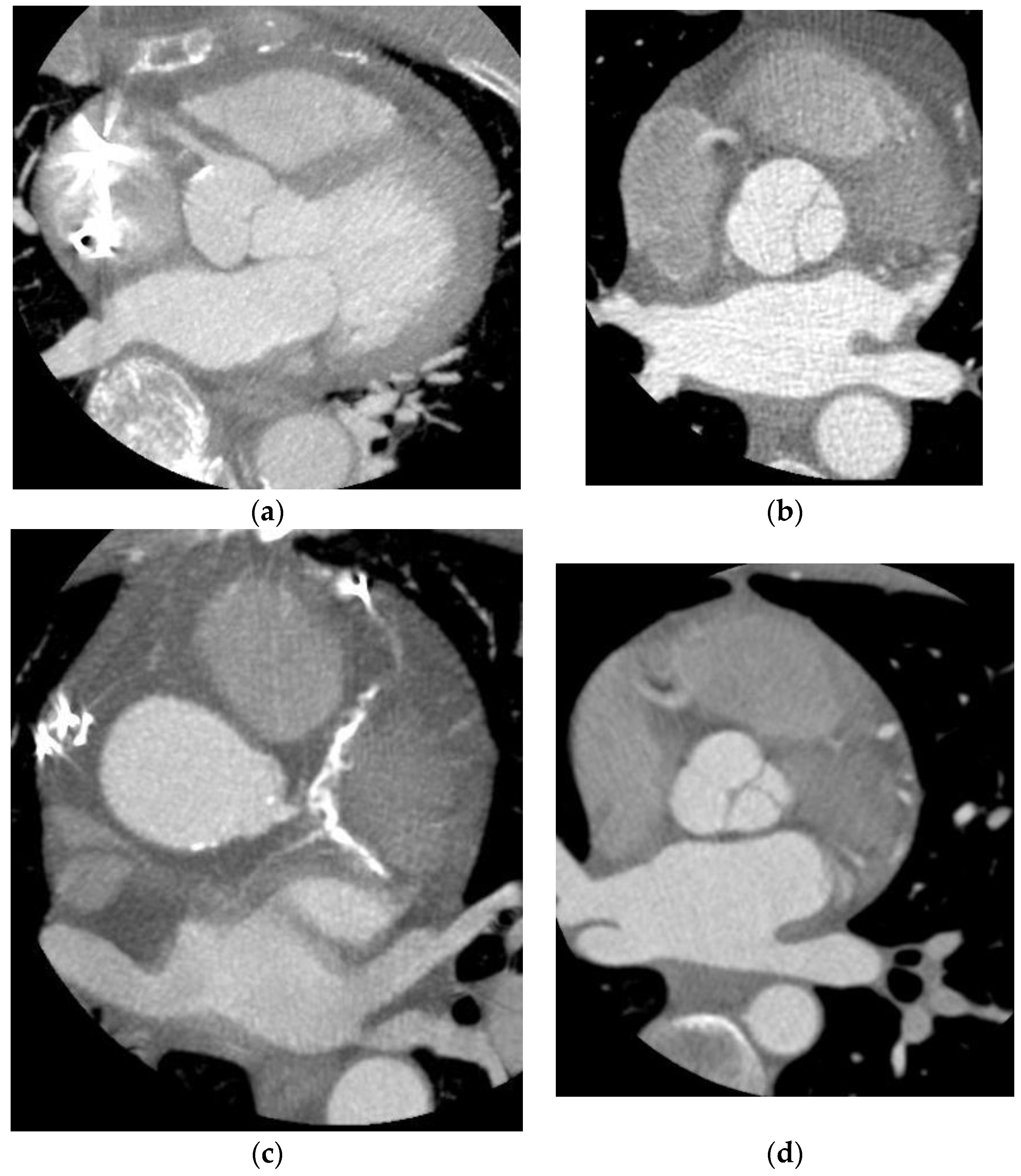
2.5. Image Quality Assessment
2.6. Quantitative Analysis
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Alani, A.; Nakanishi, R.; Budoff, M.J. Recent improvement in coronary computed tomography angiography diagnostic accuracy. Clin. Cardiol. 2014, 37, 428–433. [Google Scholar] [CrossRef]
- Fujimoto, S.; Matsutani, H.; Kondo, T.; Sano, T.; Kumamaru, K.; Takase, S.; Rybicki, F.J. Image quality and radiation dose stratified by patient heart rate for coronary 64- and 320-MDCT angiography. Am. J. Roentgenol. 2013, 200, 765–770. [Google Scholar] [CrossRef] [PubMed]
- Nakanishi, R.; Sankaran, S.; Grady, L.; Malpeso, J.; Yousfi, R.; Osawa, K.; Ceponiene, I.; Nazarat, N.; Rahmani, S.; Kissel, K.; et al. Automated estimation of image quality for coronary computed tomographic angiography using machine learning. Eur. Radiol. 2018, 28, 4018–4026. [Google Scholar] [CrossRef] [PubMed]
- Patel, N.; Li, D.; Nakanishi, R.; Fatima, B.; Andreini, D.; Pontone, G.; Conte, E.; O’Rourke, R.; Jayawardena, E.; Hamilton-Craig, C.; et al. Comparison of Whole Heart Computed Tomography Scanners for Image Quality Lower Radiation Dosing in Coronary Computed Tomography Angiography: The CONVERGE Registry. Acad. Radiol. 2019, 26, 1443–1449. [Google Scholar] [CrossRef]
- Klass, O.; Walker, M.; Siebach, A.; Stuber, T.; Feuerlein, S.; Juchems, M.; Hoffmann, M.H. Prospectively gated axial CT coronary angiography: Comparison of image quality and effective radiation dose between 64- and 256-slice CT. Eur. Radiol. 2010, 20, 1124. [Google Scholar] [CrossRef]
- Sheta, H.; Egstrup, K.; Husic, M.; Heinsen, L.; Nieman, K.; Lambrechtsen, J. Impact of a motion correction algorithm on image quality in patients undergoing CT angiography: A randomized controlled trial. Clin. Imaging 2017, 42, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Min, J.K.; Swaminathan, R.V.; Vass, M.; Gallagher, S.; Weinsaft, J.W. High-definition multidetector computed tomography for evaluation of coronary artery stents: Comparison to standard definition 64-detector row computed tomography. J. Cardiovasc. Comput. Tomogr. 2009, 3, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Fan, L.; Zhang, J.; Xu, D.; Dong, Z.; Li, X.; Zhang, L. CTCA image quality improvement by using snapshot freeze technique under prospective and retrospective electrocardiographic gating. J. Comput. Assist. Tomogr. 2015, 39, 202–206. [Google Scholar] [CrossRef] [PubMed]
- Carrascosa, P.; Deviggiano, A.; Capunay, C.; De Zan, M.; Goldsmit, A.; Rodriguez-Granillo, G.A. Effect of Intracycle Motion Correction Algorithm on Image Quality and Diagnostic Performance of Computed Tomography Coronary Angiography in Patients with Suspected Coronary Artery Disease. Acad. Radiol. 2015, 22, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y.; Ma, Y.; Fan, W.; Wang, Y.; Yu, M.; Vembar, M.; Guo, Q. Diagnostic accuracy of low-dose 256-slice multi-detector coronary CT angiography using iterative reconstruction in patients with suspected coronary artery disease. Eur. Radiol. 2014, 24, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Hemminger, E.J.; Girsky, E.J.; Budoff, M.J. Applications of computed tomography in clinical cardiac electrophysiology. J. Cardiovasc. Comput. Tomogr. 2007, 1, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Buttan, A.K.; Yang, E.H.; Budoff, M.J.; Vorobiof, G. Evaluation of valvular disease by cardiac computed tomography assessment. J. Cardiovasc. Comput. Tomogr. 2012, 6, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Koplay, M.; Erdogan, H.; Avci, A.; Sivri, M.; Demir, K.; Guler, I.; Demir, L.S.; Paksoy, Y. Radiation dose and diagnostic accuracy of high-pitch dual-source coronary angiography in the evaluation of coronary artery stenoses. Diagn. Interv. Imaging 2016, 97, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Ondrejkovic, M.; Salat, D.; Cambal, D.; Klepanec, A. Radiation dose and image quality of CT coronary angiography in patients with high heart rate or irregular heart rhythm using a 16-cm wide detector CT scanner. Medicine 2022, 101, e30583. [Google Scholar] [CrossRef] [PubMed]
| Total | 4 cm Scanner | 16 cm Scanner | ||
|---|---|---|---|---|
| Number of Subjects | 104 | 52 | 52 | |
| Mean Std. | Mean Std. | Mean Std. | p | |
| Age | 60.6 ± 15.3 | 58.6 ± 16.8 | 62.6 ± 13.4 | 0.189 |
| BMI | 27.8 ± 5.1 | 27.9 ± 5.1 | 27.8 ± 5.2 | 0.912 |
| Heart Rate | 74.9 ± 7.2 | 75.1 ± 7.1 | 74.6 ± 7.4 | 0.426 |
| Radiation dose | 3.9 ± 4.5 | 5.6 ± 5.3 | 2.1 ± 2.6 | <0.0001 |
| kVp | ||||
| 100 | 56 | 28 | 24 | |
| 120 | 48 | 28 | 24 | |
| ASIR | ||||
| 0 | 20 | 19 | 1 | |
| 30 | 21 | 21 | 0 | |
| 40 | 6 | 6 | 0 | |
| 50 | 7 | 5 | 2 | |
| 60 | 50 | 1 | 49 | |
| Total | 4 cm Scanner | 16 cm Scanner | Difference | ||
|---|---|---|---|---|---|
| Number of Subjects | 104 | 52 | 52 | ||
| Mean Std. | Mean Std. | Mean Std. | Mean Std. | p | |
| Aorta Signal-to-noise | 10.1 ± 4.3 | 8.7 ± 4.0 | 11.5 ± 4.2 | (2.8) ± 4.1 | 0.0001 |
| Aorta Contrast-to-noise | 7.6 ± 3.8 | 6.3 ± 3.5 | 9.0 ± 3.7 | (2.7) ± 3.6 | 0.0002 |
| LV Contrast-to-noise | 6.5 ± 3.3 | 5.2 ± 3.6 | 7.9 ± 2.1 | (2.7) ± 3.0 | <0.0001 |
| Total | 4 cm Scanner | 16 cm Scanner | |
|---|---|---|---|
| Number of Subjects | 104 | 52 | 52 |
| CTA Image Quality | |||
| Excellent | 41 | 4 | 37 |
| Good | 20 | 10 | 10 |
| Fair | 13 | 9 | 4 |
| Poor | 30 | 29 | 1 |
| Ondrejkovic et al. [14] | Ondrejkovic et al. [14] | ||
|---|---|---|---|
| Number of Subjects | 52 | 154 | 104 (Regular rhythm > 70 bpm) |
| Mean Std. | Mean Std. | ||
| Age | 62.6 ± 16.8 | 62 ± 11 | |
| Heart Rate | 74.6 ± 7.1 | 80 ± 12 | |
| Weight | 87 ± 18 | 85 ± 16 | |
| Radiation Dose | 2.1 ± 2.6 | 3.0 ± 1.5 | |
| Scanner | 256 Row—16 cm | 256 Row—16 cm | 256 Row—16 cm |
| Beta Blocker | Oral and Intravenous | Intravenous Only | Intravenous Only |
| Male/Female | 31/21 | 86/68 | |
| Excellent | 37 (71%) | 22 (14%) | 16 (15%) |
| Good | 10 (19%) | 101 (66%) | 68 (65%) |
| Fair | 4 (7.7%) | 25 (16%) | 17 (16%) |
| Poor | 1 (1.9%) | 6 (3.9%) | 3 (2.9%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdelkarim, A.; Roy, S.K.; Kinninger, A.; Salek, A.; Baranski, O.; Andreini, D.; Pontone, G.; Conte, E.; O’Rourke, R.; Hamilton-Craig, C.; et al. Evaluation of Image Quality for High Heart Rates for Coronary Computed Tomographic Angiography with Advancement in CT Technology: The CONVERGE Registry. J. Cardiovasc. Dev. Dis. 2023, 10, 404. https://doi.org/10.3390/jcdd10090404
Abdelkarim A, Roy SK, Kinninger A, Salek A, Baranski O, Andreini D, Pontone G, Conte E, O’Rourke R, Hamilton-Craig C, et al. Evaluation of Image Quality for High Heart Rates for Coronary Computed Tomographic Angiography with Advancement in CT Technology: The CONVERGE Registry. Journal of Cardiovascular Development and Disease. 2023; 10(9):404. https://doi.org/10.3390/jcdd10090404
Chicago/Turabian StyleAbdelkarim, Ayman, Sion K. Roy, April Kinninger, Azadeh Salek, Olivia Baranski, Daniele Andreini, Gianluca Pontone, Edoardo Conte, Rachael O’Rourke, Christian Hamilton-Craig, and et al. 2023. "Evaluation of Image Quality for High Heart Rates for Coronary Computed Tomographic Angiography with Advancement in CT Technology: The CONVERGE Registry" Journal of Cardiovascular Development and Disease 10, no. 9: 404. https://doi.org/10.3390/jcdd10090404
APA StyleAbdelkarim, A., Roy, S. K., Kinninger, A., Salek, A., Baranski, O., Andreini, D., Pontone, G., Conte, E., O’Rourke, R., Hamilton-Craig, C., & Budoff, M. J. (2023). Evaluation of Image Quality for High Heart Rates for Coronary Computed Tomographic Angiography with Advancement in CT Technology: The CONVERGE Registry. Journal of Cardiovascular Development and Disease, 10(9), 404. https://doi.org/10.3390/jcdd10090404










