The Effect of a Vegan Diet on the Cardiovascular System
Abstract
1. Introduction
2. Assessment of Vegan Nutrition concerning Health
3. Links between a Vegan Diet and Cardiovascular Diseases
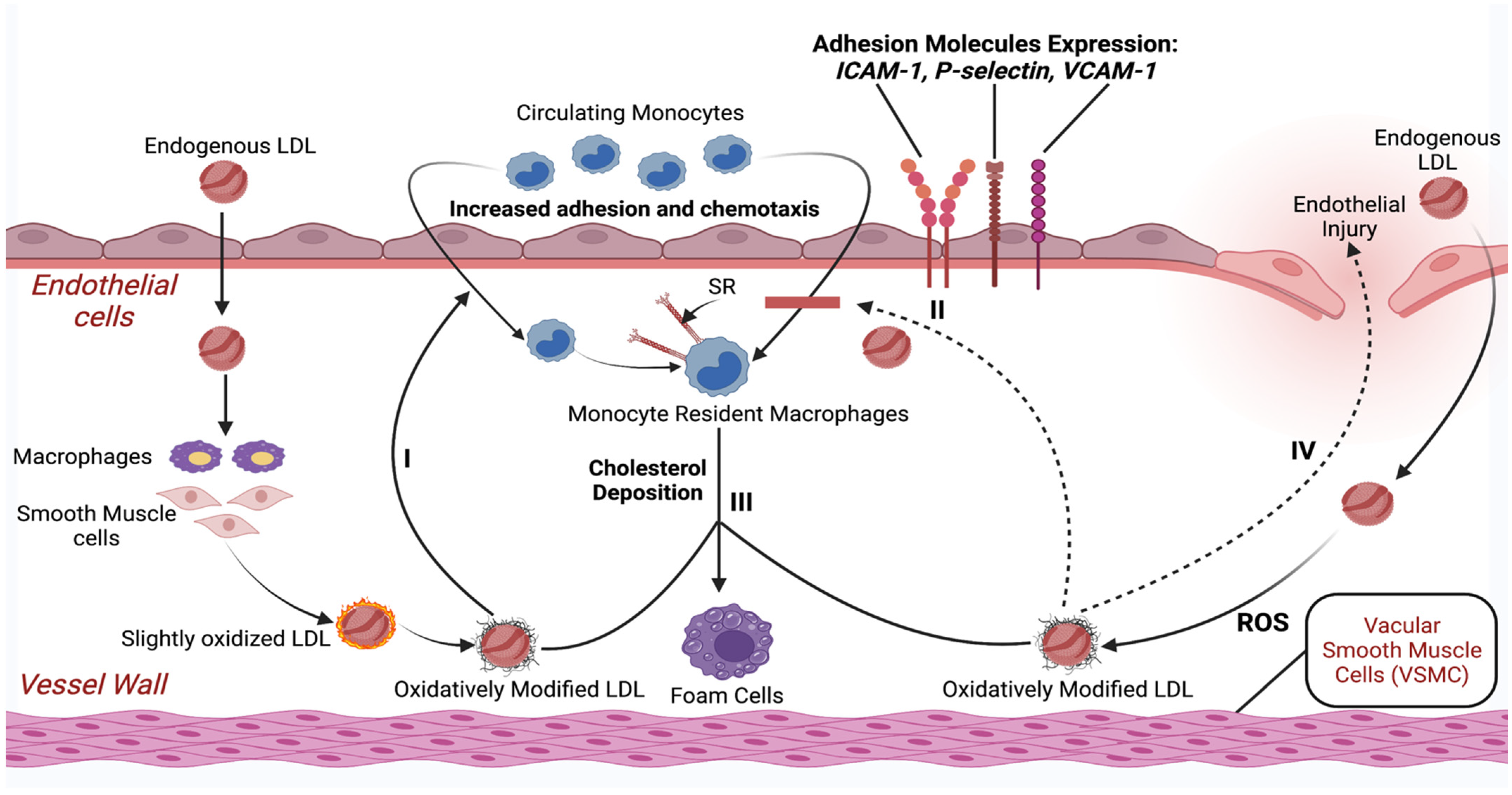
3.1. Inflammatory Response as a Result of Unhealthy Dietary Patterns
Chronic Inflammation of the Vessel Walls Due to Unhealthy Diet
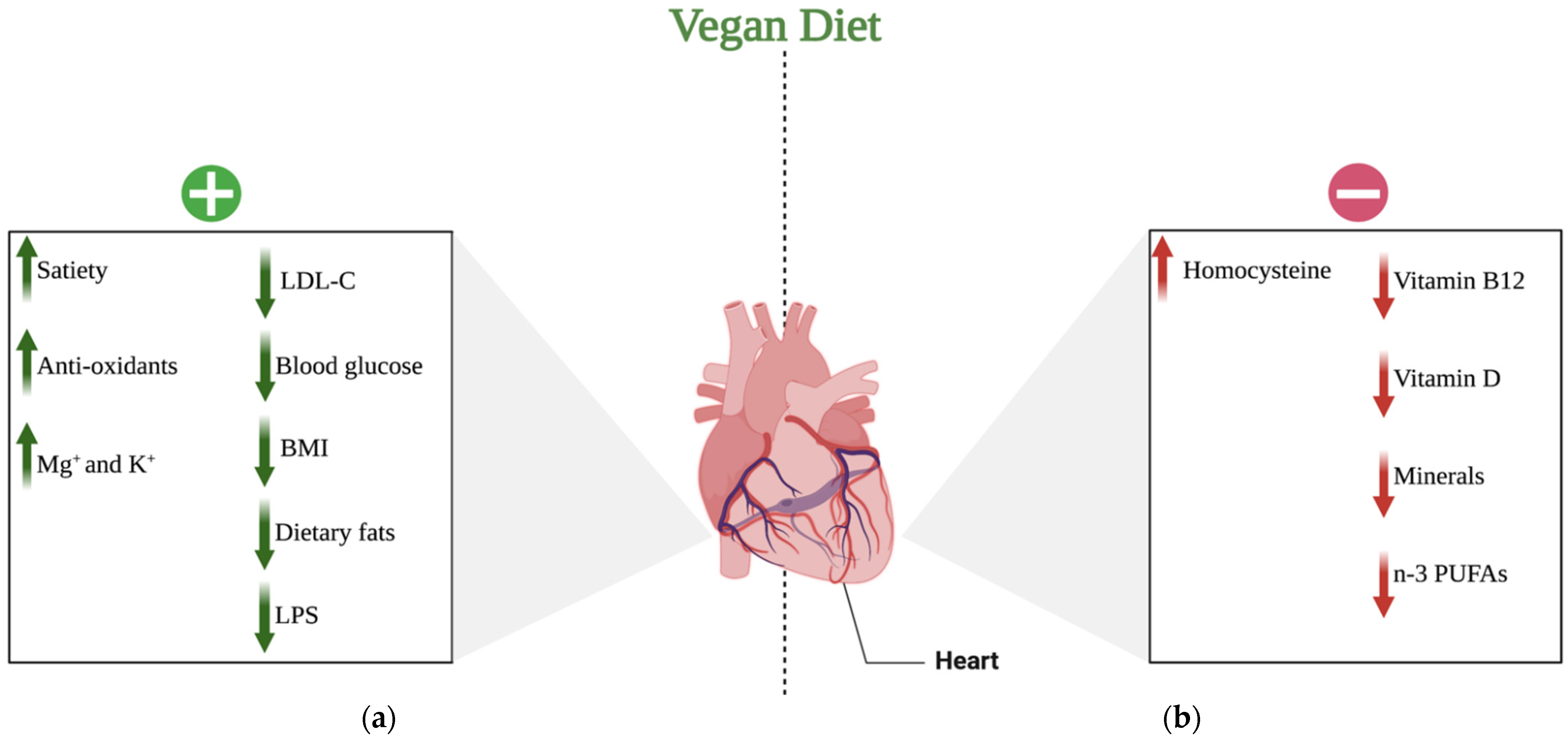
3.2. Benefits/Risks of a Vegan Diet for the Cardiovascular System
3.2.1. The Positive Effects of Veganism on the Cardiovascular System
3.2.2. The Negative Effect of Veganism on the Cardiovascular System
4. Therapeutic Implications
The Role of a Vegan Diet in the Prevention of CVD
5. Outlook and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Appleby, P.N.; Key, T.J. The Long-Term Health of Vegetarians and Vegans. Proc. Nutr. Soc. 2016, 75, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Orlich, M.J.; Jaceldo-Siegl, K.; Sabaté, J.; Fan, J.; Singh, P.N.; Fraser, G.E. Patterns of Food Consumption among Vegetarians and Non-Vegetarians. Br. J. Nutr. 2014, 112, 1644–1653. [Google Scholar] [CrossRef] [PubMed]
- Ferdowsian, H.R.; Barnard, N.D. Effects of Plant-Based Diets on Plasma Lipids. Am. J. Cardiol. 2009, 104, 947–956. [Google Scholar] [CrossRef] [PubMed]
- Ornish, D.; Scherwitz, L.W.; Billings, J.H.; Lance Gould, K.; Merritt, T.A.; Sparler, S.; Armstrong, W.T.; Ports, T.A.; Kirkeeide, R.L.; Hogeboom, C.; et al. Intensive Lifestyle Changes for Reversal of Coronary Heart Disease. JAMA 1998, 280, 2001–2007. [Google Scholar] [CrossRef]
- Rao, V.; Al-Weshahy, A. Plant-Based Diets and Control of Lipids and Coronary Heart Disease Risk. Curr. Atheroscler. Rep. 2008, 10, 478–485. [Google Scholar] [CrossRef]
- Craig, W.J. Health Effects of Vegan Diets. Am. J. Clin. Nutr. 2009, 89, 1627S–1633S. [Google Scholar] [CrossRef]
- Barnard, N.D.; Katcher, H.I.; Jenkins, D.J.; Cohen, J.; Turner-McGrievy, G. Vegetarian and Vegan Diets in Type 2 Diabetes Management. Nutr. Rev. 2009, 67, 255–263. [Google Scholar] [CrossRef]
- Le, L.; Sabaté, J. Beyond Meatless, the Health Effects of Vegan Diets: Findings from the Adventist Cohorts. Nutrients 2014, 6, 2131–2147. [Google Scholar] [CrossRef]
- Orlich, M.J.; Singh, P.N.; Sabaté, J.; Jaceldo-Siegl, K.; Fan, J.; Knutsen, S.; Beeson, W.L.; Fraser, G.E. Vegetarian Dietary Patterns and Mortality in Adventist Health Study 2. JAMA Intern. Med. 2013, 173, 1230. [Google Scholar] [CrossRef]
- Kim, H.; Caulfield, L.E.; Rebholz, C.M. Healthy Plant-Based Diets Are Associated with Lower Risk of All-Cause Mortality in US Adults. J. Nutr. 2018, 148, 624–631. [Google Scholar] [CrossRef]
- Dinu, M.; Abbate, R.; Gensini, G.F.; Casini, A.; Sofi, F. Vegetarian, Vegan Diets and Multiple Health Outcomes: A Systematic Review with Meta-Analysis of Observational Studies. Crit. Rev. Food Sci. Nutr. 2017, 57, 3640–3649. [Google Scholar] [CrossRef] [PubMed]
- Segovia-Siapco, G.; Sabaté, J. Health and Sustainability Outcomes of Vegetarian Dietary Patterns: A Revisit of the EPIC-Oxford and the Adventist Health Study-2 Cohorts. Eur. J. Clin. Nutr. 2019, 72, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Satija, A.; Hu, F.B. Plant-Based Diets and Cardiovascular Health. Trends Cardiovasc. Med. 2018, 28, 437–441. [Google Scholar] [CrossRef] [PubMed]
- Haddad, E.H.; Tanzman, J.S. What Do Vegetarians in the United States Eat? Am. J. Clin. Nutr. 2003, 78, 626S–632S. [Google Scholar] [CrossRef] [PubMed]
- Ho-Pham, L.T.; Vu, B.Q.; Lai, T.Q.; Nguyen, N.D.; Nguyen, T.V. Vegetarianism, Bone Loss, Fracture and Vitamin D: A Longitudinal Study in Asian Vegans and Non-Vegans. Eur. J. Clin. Nutr. 2012, 66, 75–82. [Google Scholar] [CrossRef]
- Ho-Pham, L.T.; Nguyen, P.L.T.; Le, T.T.T.; Doan, T.A.T.; Tran, N.T.; Le, T.A.; Nguyen, T.V. Veganism, Bone Mineral Density, and Body Composition: A Study in Buddhist Nuns. Osteoporos. Int. 2009, 20, 2087–2093. [Google Scholar] [CrossRef]
- Dary, O. Establishing Safe and Potentially Efficacious Fortification Contents for Folic Acid and Vitamin B12. Food Nutr. Bull. 2008, 29, S214–S224. [Google Scholar] [CrossRef]
- Malouf, R.; Grimley Evans, J. Folic Acid with or without Vitamin B12 for the Prevention and Treatment of Healthy Elderly and Demented People. Cochrane Database Syst. Rev. 2008, 4, CD004514. [Google Scholar] [CrossRef]
- Allès, B.; Baudry, J.; Méjean, C.; Touvier, M.; Péneau, S.; Hercberg, S.; Kesse-Guyot, E. Comparison of Sociodemographic and Nutritional Characteristics between Self-Reported Vegetarians, Vegans, and Meat-Eaters from the NutriNet-Santé Study. Nutrients 2017, 9, 1023. [Google Scholar] [CrossRef]
- Menal-Puey, S.; Marques-Lopes, I. Development of a Food Guide for the Vegetarians of Spain. J. Acad. Nutr. Diet 2017, 117, 1509–1516. [Google Scholar] [CrossRef]
- Agnoli, C.; Baroni, L.; Bertini, I.; Ciappellano, S.; Fabbri, A.; Papa, M.; Pellegrini, N.; Sbarbati, R.; Scarino, M.L.; Siani, V.; et al. Position Paper on Vegetarian Diets from the Working Group of the Italian Society of Human Nutrition. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 1037–1052. [Google Scholar] [CrossRef] [PubMed]
- Dyett, P.A.; Sabaté, J.; Haddad, E.; Rajaram, S.; Shavlik, D. Vegan Lifestyle Behaviors: An Exploration of Congruence with Health-Related Beliefs and Assessed Health Indices. Appetite 2013, 67, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Sobiecki, J.G.; Appleby, P.N.; Bradbury, K.E.; Key, T.J. High Compliance with Dietary Recommendations in a Cohort of Meat Eaters, Fish Eaters, Vegetarians, and Vegans: Results from the European Prospective Investigation into Cancer and Nutrition–Oxford Study. Nutr. Res. 2016, 36, 464–477. [Google Scholar] [CrossRef] [PubMed]
- Baroni, L.; Goggi, S.; Battaglino, R.; Berveglieri, M.; Fasan, I.; Filippin, D.; Griffith, P.; Rizzo, G.; Tomasini, C.; Tosatti, M.; et al. Vegan Nutrition for Mothers and Children: Practical Tools for Healthcare Providers. Nutrients 2018, 11, 5. [Google Scholar] [CrossRef]
- Leitzmann, C. Vegetarian Nutrition: Past, Present, Future. Am. Soc. Nutr. 2014, 100 (Suppl. S1), 496S–502S. [Google Scholar] [CrossRef] [PubMed]
- Tosh, S.M.; Yada, S. Dietary Fibres in Pulse Seeds and Fractions: Characterization, Functional Attributes, and Applications. Food Res. Int. 2010, 43, 450–460. [Google Scholar] [CrossRef]
- Hoover, R.; Hughes, T.; Chung, H.J.; Liu, Q. Composition, Molecular Structure, Properties, and Modification of Pulse Starches: A Review. Food Res. Int. 2010, 43, 399–413. [Google Scholar] [CrossRef]
- Kumar, M.; Tomar, M.; Punia, S.; Dhakane-Lad, J.; Dhumal, S.; Changan, S.; Senapathy, M.; Berwal, M.K.; Sampathrajan, V.; Sayed, A.A.S.; et al. Plant-Based Proteins and Their Multifaceted Industrial Applications. LWT 2022, 154, 112620. [Google Scholar] [CrossRef]
- Schüpbach, R.; Wegmüller, R.; Berguerand, C.; Bui, M.; Herter-Aeberli, I. Micronutrient Status and Intake in Omnivores, Vegetarians and Vegans in Switzerland. Eur. J. Nutr. 2017, 56, 283–293. [Google Scholar] [CrossRef]
- Saunders, A.V.; Davis, B.C.; Garg, M.L. Omega-3 Polyunsaturated Fatty Acids and Vegetarian Diets. Med. J. Aust. 2012, 1, 22–26. [Google Scholar] [CrossRef]
- van Winckel, M.; vande Velde, S.; de Bruyne, R.; van Biervliet, S. Clinical Practice: Vegetarian Infant and Child Nutrition. Eur. J. Pediatr. 2011, 170, 1489–1494. [Google Scholar] [CrossRef] [PubMed]
- Gibson, R.A.; Muhlhausler, B.; Makrides, M. Conversion of Linoleic Acid and Alpha-Linolenic Acid to Long-Chain Polyunsaturated Fatty Acids (LCPUFAs), with a Focus on Pregnancy, Lactation and the First 2 Years of Life. Matern. Child. Nutr. 2011, 7, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Hever, J. Plant-Based Diets: A Physician’s Guide. Perm. J. 2016, 20, 15-082. [Google Scholar] [CrossRef] [PubMed]
- Grant, B.F.; Chou, S.P.; Saha, T.D.; Pickering, R.P.; Kerridge, B.T.; Ruan, W.J.; Huang, B.; Jung, J.; Zhang, H.; Fan, A.; et al. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001-2002 to 2012–2013. JAMA Psychiatry 2017, 74, 911. [Google Scholar] [CrossRef]
- Martínez Steele, E.; Baraldi, L.G.; Louzada, M.L.d.C.; Moubarac, J.-C.; Mozaffarian, D.; Monteiro, C.A. Ultra-Processed Foods and Added Sugars in the US Diet: Evidence from a Nationally Representative Cross-Sectional Study. BMJ Open 2016, 6, e009892. [Google Scholar] [CrossRef] [PubMed]
- Chassaing, B.; van de Wiele, T.; de Bodt, J.; Marzorati, M.; Gewirtz, A.T. Dietary Emulsifiers Directly Alter Human Microbiota Composition and Gene Expression Ex Vivo Potentiating Intestinal Inflammation. Gut 2017, 66, 1414–1427. [Google Scholar] [CrossRef] [PubMed]
- Carrera-Bastos, P.; O’Keefe, F.; Lindeberg, S.; Cordain, L. The Western Diet and Lifestyle and Diseases of Civilization. Res. Rep. Clin. Cardiol. 2011, 2, 2–15. [Google Scholar] [CrossRef]
- Bentley, J.U.S. Trends in Food Availability and a Dietary Assessment of Loss-Adjusted Food Availability, 1970–2014. Econ. Inf. Bull. 2017, 166, 2–30. [Google Scholar] [CrossRef]
- Richards, J.L.; Yap, Y.A.; McLeod, K.H.; Mackay, C.R.; Mariño, E. Dietary Metabolites and the Gut Microbiota: An Alternative Approach to Control Inflammatory and Autoimmune Diseases. Clin. Transl. Immunol. 2016, 5, e82. [Google Scholar] [CrossRef]
- Bishehsari, F.; Magno, E.; Swanson, G.; Desai, V.; Voigt, R.M.; Forsyth, C.B.; Keshavarzian, A. Alcohol and Gut-Derived Inflammation. Alcohol Res. 2017, 38, 163–171. [Google Scholar]
- Lerner, A.; Matthias, T. Changes in Intestinal Tight Junction Permeability Associated with Industrial Food Additives Explain the Rising Incidence of Autoimmune Disease. Autoimmun. Rev. 2015, 14, 479–489. [Google Scholar] [CrossRef]
- Dickinson, S.; Hancock, D.P.; Petocz, P.; Ceriello, A.; Brand-Miller, J. High-Glycemic Index Carbohydrate Increases Nuclear Factor-B Activation in Mononuclear Cells of Young, Lean Healthy Subjects. Am. J. Clin. Nutr. 2008, 87, 1188–1193. [Google Scholar] [CrossRef] [PubMed]
- Schnabel, L.; Kesse-Guyot, E.; Allès, B.; Touvier, M.; Srour, B.; Hercberg, S.; Buscail, C.; Julia, C. Association Between Ultraprocessed Food Consumption and Risk of Mortality Among Middle-Aged Adults in France. JAMA Intern. Med. 2019, 179, 490. [Google Scholar] [CrossRef]
- Rank, F.; Eir, M.; Tampfer, J.S.; Nn, J.O.A.; Anson, E.M.; Imm, R.R.; Olditz, R.A.C.; Osner, E.A.R.; Harles, C.; Ennekens, H.H.; et al. Dietary Fat Intake and the Risk of Coronary Heart Disease in Women. N. Engl. J. Med. 1997, 337, 1491–1499. [Google Scholar] [CrossRef]
- Lopez-Garcia, E.; Schulze, M.B.; Meigs, J.B.; Manson, J.E.; Rifai, N.; Stampfer, M.J.; Willett, W.C.; Hu, F.B. Nutritional Epidemiology Consumption of Trans Fatty Acids Is Related to Plasma Biomarkers of Inflammation and Endothelial Dysfunction. J. Nutr. 2005, 135, 562–566. [Google Scholar] [CrossRef]
- Simionescu, N.; Vasile, E.; Lupu, F.; Popescu, G. Prelesional Events in Atherogenesis. Accumulation of Extracellular Cholesterol-Rich Liposomes in the Arterial Intima and Cardiac Valves of the Hyperlipidemic Rabbit. Am. J. Pathol. 1986, 123, 109–125. [Google Scholar]
- Schwartz, C.J.; Valente, A.J.; Sprague, E.A.; Kelley, J.L.; Nerem, R.M. The Pathogenesis of Atherosclerosis: An Overview. Clin. Cardiol. 1991, 14, 1–16. [Google Scholar] [CrossRef]
- Ross, R. Atherosclerosis: A Problem of the Biology of Arterial Wall Cells and Their Interactions with Blood Components. Arteriosclerosis 1981, 1, 293–311. [Google Scholar] [CrossRef]
- Virmani, R.; Kolodgie, F.D.; Burke, A.P.; Farb, A.; Schwartz, S.M. Lessons from Sudden Coronary Death. Arter. Thromb Vasc. Biol. 2000, 20, 1262–1275. [Google Scholar] [CrossRef]
- Shi, W.; Haberland, M.E.; Jien, M.L.; Shih, D.M.; Lusis, A.J. Endothelial Responses to Oxidized Lipoproteins Determine Genetic Susceptibility to Atherosclerosis in Mice. Circulation 2000, 102, 75–81. [Google Scholar] [CrossRef]
- Golia, E.; Limongelli, G.; Natale, F.; Fimiani, F.; Maddaloni, V.; Pariggiano, I.; Bianchi, R.; Crisci, M.; D’Acierno, L.; Giordano, R.; et al. Inflammation and Cardiovascular Disease: From Pathogenesis to Therapeutic Target. Curr. Atheroscler. Rep. 2014, 16, 435. [Google Scholar] [CrossRef]
- Panés, J.; Perry, M.; Granger, D.N. Leukocyte-Endothelial Cell Adhesion: Avenues for Therapeutic Intervention. Br. J. Pharmacol. 1999, 126, 537. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, J.; van Daalen, K.R.; Thayyil, A.; Cocco, M.T.d.A.R.R.; Caputo, D.; Oliver-Williams, C. A Systematic Review of the Association Between Vegan Diets and Risk of Cardiovascular Disease. J. Nutr. 2021, 151, 1539–1552. [Google Scholar] [CrossRef] [PubMed]
- Fontana, L.; Meyer, T.E.; Klein, S.; Holloszy, J.O. Long-Term Low-Calorie Low-Protein Vegan Diet and Endurance Exercise Are Associated with Low Cardiometabolic Risk. Rejuvenation Res. 2007, 10, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Giovannucci, E.; Boffetta, P.; Fadnes, L.T.; Keum, N.N.; Norat, T.; Greenwood, D.C.; Riboli, E.; Vatten, L.J.; Tonstad, S. Fruit and Vegetable Intake and the Risk of Cardiovascular Disease, Total Cancer and All-Cause Mortality—A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Int. J. Epidemiol. 2017, 46, 1029. [Google Scholar] [CrossRef] [PubMed]
- Sacks, F.M.; Lichtenstein, A.H.; Wu, J.H.Y.; Appel, L.J.; Creager, M.A.; Kris-Etherton, P.M.; Miller, M.; Rimm, E.B.; Rudel, L.L.; Robinson, J.G.; et al. Dietary Fats and Cardiovascular Disease: A Presidential Advisory From the American Heart Association. Circulation 2017, 136, e1–e23. [Google Scholar] [CrossRef]
- Jafari, S.; Hezaveh, E.; Jalilpiran, Y.; Jayedi, A.; Wong, A.; Safaiyan, A.; Barzegar, A. Plant-based diets and risk of disease mortality: A systematic review and meta-analysis of cohort studies. Crit. Rev. Food Sci. Nutr. 2021, 62, 7760–7772. [Google Scholar] [CrossRef]
- Holscher, H.D. Dietary Fiber and Prebiotics and the Gastrointestinal Microbiota. Gut Microbes 2017, 8, 172. [Google Scholar] [CrossRef]
- Dhingra, D.; Michael, M.; Rajput, H.; Patil, R.T. Dietary Fibre in Foods: A Review. J. Food Sci. Technol. 2012, 49, 255. [Google Scholar] [CrossRef]
- Hervik, A.K.; Svihus, B. The Role of Fiber in Energy Balance. J. Nutr. Metab. 2019, 2019, 4983657. [Google Scholar] [CrossRef]
- Pandey, K.B.; Rizvi, S.I. Plant Polyphenols as Dietary Antioxidants in Human Health and Disease. Oxid. Med. Cell Longev. 2009, 2, 270. [Google Scholar] [CrossRef]
- Habauzit, V.; Morand, C. Evidence for a Protective Effect of Polyphenols-Containing Foods on Cardiovascular Health: An Update for Clinicians. Ther. Adv. Chronic. Dis. 2012, 3, 87. [Google Scholar] [CrossRef]
- Tangney, C.C.; Rasmussen, H.E. Polyphenols, Inflammation, and Cardiovascular Disease. Curr. Atheroscler. Rep. 2013, 15, 324. [Google Scholar] [CrossRef] [PubMed]
- Key, T.J.; Appleby, P.N.; Rosell, M.S. Health Effects of Vegetarian and Vegan Diets. Proc. Nutr. Soc. 2006, 65, 35–41. [Google Scholar] [CrossRef]
- Pickering, R.; Bradlee, M.; Singer, M.; Moore, L. Higher Intakes of Potassium and Magnesium, but Not Lower Sodium, Reduce Cardiovascular Risk in the Framingham Offspring Study. Nutrients 2021, 13, 269. [Google Scholar] [CrossRef]
- O’Neill, L.A.J. Targeting Signal Transduction as a Strategy to Treat Inflammatory Diseases. Nat. Rev. Drug. Discov. 2006, 5, 549–564. [Google Scholar] [CrossRef]
- Hwang, D.H.; Kim, J.A.; Lee, J.Y. Mechanisms for the Activation of Toll-like Receptor 2/4 by Saturated Fatty Acids and Inhibition by Docosahexaenoic Acid. Eur. J. Pharmacol. 2016, 785, 24. [Google Scholar] [CrossRef]
- Fritsche, K.L. The Science of Fatty Acids and Inflammation. Adv. Nutr. 2015, 6, 293S–301S. [Google Scholar] [CrossRef]
- Willett, W.C. The Role of Dietary N-6 Fatty Acids in the Prevention of Cardiovascular Disease. J. Cardiovasc. Med. 2007, 8, S42–S45. [Google Scholar] [CrossRef]
- Petersson, H.; Basu, S.; Cederholm, T.; Risérus, U. Serum Fatty Acid Composition and Indices of Stearoyl-CoA Desaturase Activity Are Associated with Systemic Inflammation: Longitudinal Analyses in Middle-Aged Men. Br. J. Nutr. 2008, 99, 1186–1189. [Google Scholar] [CrossRef]
- Benatar, J.R.; Stewart, R.A.H. Cardiometabolic risk factors in vegans; A meta-analysis of observational studies. PLoS ONE 2018, 13, e0209086. [Google Scholar] [CrossRef] [PubMed]
- Jabri, A.; Kumar, A.; Verghese, E.; Alameh, A.; Kumar, A.; Khan, M.S.; Khan, S.U.; Michos, E.D.; Kapadia, S.R.; Reed, G.W.; et al. Meta-Analysis of Effect of Vegetarian Diet on Ischemic Heart Disease and All-Cause Mortality. Am. J. Prev. Cardiol. 2021, 7, 100182. [Google Scholar] [CrossRef] [PubMed]
- Dybvik, J.S.; Svendsen, M.; Aune, D. Vegetarian and vegan diets and the risk of cardiovascular disease, ischemic heart disease and stroke: A systematic review and meta-analysis of prospective cohort studies. Eur. J. Nutr. 2022, 62, 51–69. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.-W.; Yu, L.-H.; Tu, Y.-K.; Cheng, H.-Y.; Chen, L.-Y.; Loh, C.-H.; Chen, T.-L. Risk of Incident Stroke among Vegetarians Compared to Nonvegetarians: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Nutrients 2021, 13, 3019. [Google Scholar] [CrossRef] [PubMed]
- Shenoy, V.; Mehendale, V.; Prabhu, K.; Shetty, R.; Rao, P. Correlation of Serum Homocysteine Levels with the Severity of Coronary Artery Disease. Indian J. Clin. Biochem. 2014, 29, 339. [Google Scholar] [CrossRef]
- Ankar, A.; Bhimji, S.S. Vitamin B12 Deficiency; StatPearls: Treasure Island, FL, USA, 2022.
- Baszczuk, A.; Kopczyński, Z. Hyperhomocysteinemia in Patients with Cardiovascular Disease. Postepy Hig. Med. Dosw. 2014, 68, 579–589. [Google Scholar] [CrossRef]
- Cybulska, B.; Kłosiewicz-Latoszek, L. Homocysteine—Is It Still an Important Risk Factor for Cardiovascular Disease? Kardiol. Pol. 2015, 73, 1092–1096. [Google Scholar] [CrossRef]
- Pawlak, R. Is Vitamin B12 Deficiency a Risk Factor for Cardiovascular Disease in Vegetarians? Am. J. Prev. Med. 2015, 48, e11–e26. [Google Scholar] [CrossRef]
- Chan, J.; Jaceldo-Siegl, K.; Fraser, G.E. Serum 25-Hydroxyvitamin D Status of Vegetarians, Partial Vegetarians, and Nonvegetarians: The Adventist Health Study-2. Am. J. Clin. Nutr. 2009, 89, 1686S–1692S. [Google Scholar] [CrossRef]
- Kendrick, J.; Targher, G.; Smits, G.; Chonchol, M. 25-Hydroxyvitamin D Deficiency Is Independently Associated with Cardiovascular Disease in the Third National Health and Nutrition Examination Survey. Atherosclerosis 2009, 205, 255–260. [Google Scholar] [CrossRef]
- Martini, L.A.; Wood, R.J. Vitamin D Status and the Metabolic Syndrome. Nutr. Rev. 2022, 64, 479. [Google Scholar] [CrossRef] [PubMed]
- Kheiri, B.; Abdalla, A.; Osman, M.; Ahmed, S.; Hassan, M.; Bachuwa, G. Vitamin D Deficiency and Risk of Cardiovascular Diseases: A Narrative Review. Clin. Hypertens. 2018, 24, 9. [Google Scholar] [CrossRef] [PubMed]
- Brøndum-Jacobsen, P.; Benn, M.; Jensen, G.B.; Nordestgaard, B.G. 25-Hydroxyvitamin D Levels and Risk of Ischemic Heart Disease, Myocardial Infarction, and Early Death: Population-Based Study and Meta-Analyses of 18 and 17 Studies. Arterioscler Thromb. Vasc. Biol. 2012, 32, 2794–2802. [Google Scholar] [CrossRef] [PubMed]
- Menzel, J.; Jabakhanji, A.; Biemann, R.; Mai, K.; Abraham, K.; Weikert, C. Systematic review and meta-analysis of the associations of vegan and vegetarian diets with inflammatory biomarkers. Sci. Rep. 2020, 10, 1–11. [Google Scholar] [CrossRef]
- de Jesus, N.M.; Wang, L.; Herren, A.W.; Wang, J.; Shenasa, F.; Bers, D.M.; Lindsey, M.L.; Ripplinger, C.M. Atherosclerosis Exacerbates Arrhythmia Following Myocardial Infarction: Role of Myocardial Inflammation. Heart Rhythm. Off. J. Heart Rhythm. Soc. 2015, 12, 169. [Google Scholar] [CrossRef]
- Huang, T.; Yang, B.; Zheng, J.; Li, G.; Wahlqvist, M.L.; Li, D. Systematic Review Cardiovascular Disease Mortality and Cancer Incidence in Vegetarians: A Meta-Analysis and Systematic Review. Ann. Nutr. Metab. 2012, 60, 233–240. [Google Scholar] [CrossRef]
- Marrone, G.; Guerriero, C.; Palazzetti, D.; Lido, P.; Marolla, A.; di Daniele, F.; Noce, A. Vegan Diet Health Benefits in Metabolic Syndrome. Nutrients 2021, 13, 817. [Google Scholar] [CrossRef]
- Esselstyn, C.B., Jr.; Gendy, G.; Doyle, J.; Golubic, M.; Roizen, M.F. A way to reverse CAD? J. Fam. Pract. 2014, 63, 356–364b. [Google Scholar]
- Rizzo, N.S.; Jaceldo-Siegl, K.; Sabate, J.; Fraser, G.E. Nutrient Profiles of Vegetarian and Nonvegetarian Dietary Patterns. J. Acad. Nutr. Diet. 2013, 113, 1610–1619. [Google Scholar] [CrossRef]
- Kaartinen, K.; Lammi, K.; Hypen, M.; Nenonen, M.; Hänninen, O. Vegan Diet Alleviates Fibromyalgia Symptoms. Scand. J. Rheumatol. 2009, 29, 308–313. [Google Scholar] [CrossRef]
- Barnard, N.D.; Scialli, A.R.; Turner-McGrievy, G.; Lanou, A.J.; Glass, J. The Effects of a Low-Fat, Plant-Based Dietary Intervention on Body Weight, Metabolism, and Insulin Sensitivity. Am. J. Med. 2005, 118, 991–997. [Google Scholar] [CrossRef] [PubMed]
- Turner-McGrievy, G.M.; Barnard, N.D.; Scialli, A.R. A Two-Year Randomized Weight Loss Trial Comparing a Vegan Diet to a More Moderate Low-Fat Diet. Obesity 2007, 15, 2276–2281. [Google Scholar] [CrossRef] [PubMed]
- Elkan, A.C.; Sjöberg, B.; Kolsrud, B.; Ringertz, B.; Hafström, I.; Frostegård, J. Gluten-Free Vegan Diet Induces Decreased LDL and Oxidized LDL Levels and Raised Atheroprotective Natural Antibodies against Phosphorylcholine in Patients with Rheumatoid Arthritis: A Randomized Study. Arthritis Res. Ther. 2008, 10, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Barnard, N.D.; Cohen, J.; Jenkins, D.J.A.; Turner-McGrievy, G.; Gloede, L.; Green, A.; Ferdowsian, H. A Low-Fat Vegan Diet and a Conventional Diabetes Diet in the Treatment of Type 2 Diabetes: A Randomized, Controlled, 74-Wk Clinical Trial. Am. J. Clin. Nutr. 2009, 89, 1588S–1596S. [Google Scholar] [CrossRef]
- Ferdowsian, H.R.; Barnard, N.D.; Hoover, V.J.; Katcher, H.I.; Levin, S.M.; Green, A.A.; Cohen, J.L. A Multicomponent Intervention Reduces Body Weight and Cardiovascular Risk at a GEICO Corporate Site. Am. J. Health Promot. 2010, 24, 384–387. [Google Scholar] [CrossRef]
- Mishra, S.; Xu, J.; Agarwal, U.; Gonzales, J.; Levin, S.; Barnard, N.D. A Multicenter Randomized Controlled Trial of a Plant-Based Nutrition Program to Reduce Body Weight and Cardiovascular Risk in the Corporate Setting: The GEICO Study. Eur. J. Clin. Nutr. 2013, 67, 718–724. [Google Scholar] [CrossRef]
- Wright, N.; Wilson, L.; Smith, M.; Duncan, B.; McHugh, P. The BROAD Study: A Randomised Controlled Trial Using a Whole Food Plant-Based Diet in the Community for Obesity, Ischaemic Heart Disease or Diabetes. Nutr. Diabetes 2017, 7, e256. [Google Scholar] [CrossRef]
- Jakše, B.; Pinter, S.; Jakše, B.; Bučar Pajek, M.; Pajek, J. Effects of an Ad Libitum Consumed Low-Fat Plant-Based Diet Supplemented with Plant-Based Meal Replacements on Body Composition Indices. Biomed Res. Int. 2017, 2017, 9626390. [Google Scholar] [CrossRef]
- Kahleova, H.; Dort, S.; Holubkov, R.; Barnard, N.D. A Plant-Based High-Carbohydrate, Low-Fat Diet in Overweight Individuals in a 16-Week Randomized Clinical Trial: The Role of Carbohydrates. Nutrients 2018, 10, 1302. [Google Scholar] [CrossRef]
- Barnard, N.D.; Levin, S.M.; Gloede, L.; Flores, R. Turning the Waiting Room into a Classroom: Weekly Classes Using a Vegan or a Portion-Controlled Eating Plan Improve Diabetes Control in a Randomized Translational Study. J. Acad. Nutr. Diet. 2018, 118, 1072–1079. [Google Scholar] [CrossRef]
- Cardiol, J.; Ther, C.; Rose, S.; Strombom, A. A Comprehensive Review of the Prevention and Treatment of Heart Disease with a Plant-Based Diet. J. Cardiol. Cardiovasc. Ther. 2018, 12, 110–121. [Google Scholar] [CrossRef]
- Rose, S.; Strombom, A. Preventing Stroke with a Plant-Based Diete. Open Access J. Neurol. Neurosurg. 2020, 14, 027–034. [Google Scholar] [CrossRef]
- de Biase, S.G.; Fernandes, S.F.C.; Gianini, R.J.; Duarte, J.L.G. Vegetarian Diet and Cholesterol and Triglycerides Levels. Arq. Bras. Cardiol. 2007, 88, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Banaszak, M.; Górna, I.; Przysławski, J. Non-Pharmacological Treatments for Insulin Resistance: Effective Intervention of Plant-Based Diets—A Critical Review. Nutrients 2022, 14, 1400. [Google Scholar] [CrossRef]
- Barnard, N.D.; Goldman, D.M.; Loomis, J.F.; Kahleova, H.; Levin, S.M.; Neabore, S.; Batts, T.C. Plant-Based Diets for Cardiovascular Safety and Performance in Endurance Sports. Nutrients 2019, 11, 130. [Google Scholar] [CrossRef]
- Barnard, N.D.; Alwarith, J.; Rembert, E.; Brandon, L.; Nguyen, M.; Goergen, A.; Horne, T.; do Nascimento, G.F.; Lakkadi, K.; Tura, A.; et al. A Mediterranean Diet and Low-Fat Vegan Diet to Improve Body Weight and Cardiometabolic Risk Factors: A Randomized, Cross-over Trial. J. Am. Coll. Nutr. 2020, 41, 127–139. [Google Scholar] [CrossRef]
- Choi, E.Y.; Allen, K.; McDonnough, M.; Massera, D.; Ostfeld, R.J. A Plant-Based Diet and Heart Failure: Case Report and Literature Review. J. Geriatr. Cardiol. 2017, 14, 375. [Google Scholar] [CrossRef]
- Nuwamanya, S.; Lea, A.; Abraham, P.; Varghese, R.; Kendall, J. In Patients with Type II Diabetes, is a Vegan Diet Associated with Better Glycemic Control Compared with a Conventional Diabetes Diet? Evid. Based Pract. 2022, 25, 19–20. [Google Scholar] [CrossRef]
- Remde, A.; DeTurk, S.N.; Almardini, A.; Steiner, L.; Wojda, T. Plant-predominant eating patterns—How effective are they for treating obesity and related cardiometabolic health outcomes?—A systematic review. Nutr. Rev. 2021, 80, 1094–1104. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Pettersen, B.J.; Anousheh, R.; Fan, J.; Jaceldo-Siegl, K.; Fraser, G.E. Vegetarian Diets and Blood Pressure among White Subjects: Results from the Adventist Health Study-2 (AHS-2). Public Health Nutr. 2012, 15, 1909. [Google Scholar] [CrossRef]
- Gibbs, J.; Gaskin, E.; Ji, C.; Miller, M.A.; Cappuccio, F.P. The Effect of Plant-Based Dietary Patterns on Blood Pressure: A Systematic Review Andmeta-Analysis of Controlled Intervention Trials. J. Hypertens. 2021, 39, 23–37. [Google Scholar] [CrossRef]
- Termannsen, A.D.; Clemmensen, K.K.B.; Thomsen, J.M.; Nørgaard, O.; Díaz, L.J.; Torekov, S.S.; Quist, J.S.; Færch, K. Effects of Vegan Diets on Cardiometabolic Health: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Obes. Rev. 2022, 23, e13462. [Google Scholar] [CrossRef]
- Lopez, P.D.; Cativo, E.H.; Atlas, S.A.; Rosendorff, C. The Effect of Vegan Diets on Blood Pressure in Adults: A Meta-Analysis of Randomized Controlled Trials. Am. J. Med. 2019, 132, 875–883.e7. [Google Scholar] [CrossRef]
- Bakaloudi, D.R.; Halloran, A.; Rippin, H.L.; Oikonomidou, A.C.; Dardavesis, T.I.; Williams, J.; Wickramasinghe, K.; Breda, J.; Chourdakis, M. Intake and Adequacy of the Vegan Diet. A Systematic Review of the Evidence. Clin. Nutr. 2021, 40, 3503–3521. [Google Scholar] [CrossRef]
- Kahleova, H.; Tura, A.; Hill, M.; Holubkov, R.; Barnard, N.D. A Plant-Based Dietary Intervention Improves Beta-Cell Function and Insulin Resistance in Overweight Adults: A 16-Week Randomized Clinical Trial. Nutrients 2018, 10, 189. [Google Scholar] [CrossRef]
- Brown, J.C.; Gerhardt, T.E.; Kwon, E. Risk Factors For Coronary Artery Disease; CRC Press: Boca Raton, FL, USA, 2022; pp. 1–219. [Google Scholar] [CrossRef]
| Micronutrients | Recommended Daily Intake | Sources in a Vegan Diet | Supplementation |
|---|---|---|---|
| Iron | 32 mg (women), 14 mg (men) | Leafy greens (kale, spinach, broccoli, seeds, soybeans) | Yes |
| Calcium | 525 mg | Nuts, kale, seeds, tofu, kidney beans | Yes |
| Zinc | 11 mg (men), 8 mg (women) | Nuts, seeds, whole grain, beans | Yes |
| Iodine | 150 μg | Seaweed, iodized salt | Yes |
| Vitamin B12 | 6 μg | Foods enriched with B12 (plant milk, some soy products, and some breakfast cereals) | Yes |
| Vitamin D | 600–800 IU | Fortified soy milk, mushrooms, fortified cereals, fortified orange juice, almond and rice milk | Yes |
| Omega-3 | 200–300 mg of DHA | Flax seeds, chia seeds, hemp seeds, walnuts, leafy greens (present as ALA) | Yes |
| Authors | Study Information | Intervention Diet | Duration | Outcomes | Main Findings |
|---|---|---|---|---|---|
| Kaartinen et al., 2000 [91] | A non-randomized, controlled study including 28 women with fibromyalgia (66% overweight) | Low-salt, lactobacteria-rich vegan diet | 3 months | Joint pain, sleep quality, VAS, BMI | ↓Weight (BMI = −4 kg/m2; p = 0.0001) |
| Barnard et al., 2005 [92] | An RCT including 64 overweight, post-menopausal women | Low-fat vegan diet | 14 weeks | Dietary intake, weight, and composition, resting metabolic rate, insulin sensitivity | ↓Weight (Weight = −5.8 kg ± 3.2 kg; p = 0.012) |
| Turner-McGrievy et al., 2007 [93] | An RCT including 62 overweight, post-menopausal women | Low-fat vegan diet | 14 weeks | Weight loss maintenance and diet adherence | ↓Weight (Weight: 1 year = −4.9 kg and 2 year = −3.1 kg; p < 0.05) |
| Elkan et al., 2008 [94] | An RCT including 68 individuals with rheumatoid arthritis | 1-day low-energy fast with a gluten-free vegan diet for 1 year | 1 year | Blood lipids, oxLDL, anti-PC, BMI | ↓Weight (Weight = −4.2 kg; BMI = −1.4 kg/m2; p < 0.001) |
| Barnard et al., 2009 [95] | An RCT including 99 T2DM individuals | Low-fat vegan diet with low GI | 74 weeks | HbA1c, plasma lipids, weight | ↓Weight (Weight: Non-completers = −4.4 kg and completers = −6.8 kg; p = 0.25) |
| Ferdowsian et al., 2010 [96] | A non-randomized, controlled study including 113 overweight and/or pre-existing T2DM patients | Low-fat vegan diet | 22 weeks | Body weight changes, anthropometric measures, BP, lipid profile, dietary intake | ↓Weight (Weight = −5.1 kg ±0.6 kg; BMI = −2.0 kg/m2; p < 0.001) |
| Mishra et al., 2013 [97] | An RCT including 291 overweight and/or T2DM patients | Low-fat vegan diet | 18 weeks | Dietary intake, body weight, plasma lipids, BP, HbA1c | ↓Weight (Weight: Non-completers = −2.9 kg and completers = −4.3 kg; BMI: Non-completers = −1.04 kg/m2 and completers = −1.5 kg/m2; p < 0.001) |
| Wright et al., 2017 [98] | An RCT including 65 participants with obesity and T2DM and/or ischemic heart disease and/or hypertension and/or hypercholesterolemia | Low-fat WFPB diet (type of vegan diet) | 12 weeks | BMI, cholesterol | ↓Weight (Weight: 6 months = −12.1 kg and 12 months = −11.5 kg; BMI: 6 months = −4.4 kg/m2 and 12 months = −4.2 kg/m2; p < 0.0001) |
| Jakse et al., 2017 [99] | A non-randomized, controlled study involving 325 patients willing to participate after attending a lecture | Low-fat vegan diet followed by supplementation of two daily meal replacements | 10 weeks | % Body fat, visceral fat, weight, muscle mass | ↓Weight, Body fat + Preservation of muscle mass (Weight = −5.6 kg; p < 0.001) |
| Kahleova et al., 2018 [100] | An RCT including 75 overweight participants | Low-fat, high-carbohydrate vegan diet | 16 weeks | Weight, body composition, insulin resistance | ↓Weight, ↑Carbohydrate, fiber intake (Weight = −6.5 kg; BMI = −2.0 kg/m2; p < 0.001) |
| Barnard et al., 2018 [101] | An RCT consisting of 45 patients with T2DM | Low-fat vegan diet with low GI | 20 weeks | Body weight, HbA1c, plasma lipids, urinary albumin, BP | ↓Weight (Weight = −6.3 kg; BMI = −2.3 kg/m2; p = 0.10 for weight and 0.075 for BMI) |
| Dietary Pattern | Includes | Outcome and Cardiovascular Effect |
|---|---|---|
| Vegan Diet | Vegetables, grains, nuts, fruits, legumes (dried beans, peas and lentils), and foods made from plants | ↓SFAs and sodium intake ↓BMI, promotes weight loss ↓blood glucose ↑vasodilation (↓SBP,↓DBP) ↓LDL-C and dietary fats ↓T2DM ↓ApoB and ApoE ↓risk of stroke, LV hypertrophy and LV diastolic dysfunction |
| Lacto-ovo Vegetarian Diet | Grains, fruits and vegetables, legumes, seeds, nuts, dairy products and eggs | ↓SFAs and sodium intake ↓BMI, promotes weight loss ↓SBP ↓LDL-C ↓T2DM ↓risk of heart disease and stroke |
| Pescatarian Diet | Fruits, vegetables, grains, legumes, eggs, dairy, nuts, seeds, seafood | ↓BMI, promotes weight loss ↓BP ↓TC ↓diabetes ↓ heart attacks, atherosclerosis and strokes |
| Omnivorous Diet | Plants, animals, algae and fungi | ↑SFAs and sodium intake ↑BMI ↑SBP ↑LDL-C ↑cancer, diabetes, heart disease |
| Mediterranean Diet | Whole grains, olive oil, fruits, vegetables, beans and other legumes, nuts, herbs, spices, meat, seafood | ↓BMI, promotes weight loss ↓BP ↓LDL-C ↓thrombosis ↓heart disease, stroke |
| Western (American) Diet | Meat, highly processed foods (high in carbohydrates), dairy products (high fat), grains, refined sugar and saturated fats, low in fruits and vegetables, alcohol | ↑SFAs and sodium intake ↑BMI and obesity risk ↑risk of high LDL-C ↑risk of hypertension ↑inflammation, atherosclerosis, oxidative stress ↑heart attack risk (a third of heart attack deaths worldwide) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koutentakis, M.; Surma, S.; Rogula, S.; Filipiak, K.J.; Gąsecka, A. The Effect of a Vegan Diet on the Cardiovascular System. J. Cardiovasc. Dev. Dis. 2023, 10, 94. https://doi.org/10.3390/jcdd10030094
Koutentakis M, Surma S, Rogula S, Filipiak KJ, Gąsecka A. The Effect of a Vegan Diet on the Cardiovascular System. Journal of Cardiovascular Development and Disease. 2023; 10(3):94. https://doi.org/10.3390/jcdd10030094
Chicago/Turabian StyleKoutentakis, Michail, Stanisław Surma, Sylwester Rogula, Krzysztof J. Filipiak, and Aleksandra Gąsecka. 2023. "The Effect of a Vegan Diet on the Cardiovascular System" Journal of Cardiovascular Development and Disease 10, no. 3: 94. https://doi.org/10.3390/jcdd10030094
APA StyleKoutentakis, M., Surma, S., Rogula, S., Filipiak, K. J., & Gąsecka, A. (2023). The Effect of a Vegan Diet on the Cardiovascular System. Journal of Cardiovascular Development and Disease, 10(3), 94. https://doi.org/10.3390/jcdd10030094









