Abstract
Background: Patient priorities care (PPC) is an effective age-friendly health systems (AFHS) approach to aligning care with goals derived from ‘what matters’. The purpose of this quality improvement program was to evaluate the fidelity and feasibility of the health priorities identification (HPI) process in VA Community Living Centers (CLC). Methods: PPC experts worked with local CLC staff to guide the integration of HPI into the CLC and utilized a Plan–Do–Study–Act (PDSA) model for this quality improvement project. PPC experts reviewed health priorities identification (HPI) encounters and interdisciplinary team (IDT) meetings for fidelity to the HPI process of PPC. Qualitative interviews with local CLC staff determined the appropriateness of the health priorities identification process in the CLC. Results: Over 8 months, nine facilitators completed twenty HPI encounters. Development of a Patient Health Priorities note template, staff education and PPC facilitator training improved fidelity and documentation of HPI encounters in the electronic health record. Facilitator interviews suggested that PPC is appropriate in this setting, not burdensome to staff and fostered a person-centered approach to AFHS. Conclusions: The HPI process is an acceptable and feasible approach to ask the ‘what matters’ component of AFHS in a CLC setting.
1. Introduction
Older adults with three or more chronic disorders (i.e., multiple chronic conditions (MCC)) spend on average two hours a day on healthcare tasks, a half day per healthcare encounter and receive one guideline-recommended drug that harms a coexisting condition [1,2]. Though older adults with MCC vary in their healthcare preferences, most value maintaining function over a shorter life span and prefer therapies directed toward symptom relief over those which may extend life, especially if disease-modifying therapies might impact function or cause more symptoms [3]. Age-friendly health systems (AFHS) are intended to redesign healthcare delivery to address domains of health most important to older adults. These domains, known collectively as the ‘4Ms’ of geriatrics (Matters Most; Medications; Mentation; Mobility) encompass the medical, psychosocial and functional conditions which impact older adults in all healthcare settings [4]. Patient priorities care (PPC) is an effective approach to eliciting, documenting, and sharing patient priorities, which are derived from ‘what matters’ and align healthcare to meet the goals of older adults with MCC [5]. The PPC approach is an iterative process, which uses the context of the patient’s health trajectory (e.g., disease progression), prognosis, abilities, motivation and functional recovery (e.g., physical or occupational) to set specific, realistic and actionable goals honoring those values, consistent with their care preferences.
PPC is a structured process whereby a clinician or other trained facilitator completes health priorities identification (HPI) with a patient: a process that explores the patient’s values; translates values into specific, actionable, realistic health outcome goals; identifies the most bothersome symptom, healthcare task or life/social circumstance which is getting in the way of achieving that goal; elicits healthcare preferences (what one is willing and able to do or receive); and determines the ‘one thing’ (a symptom, health problem or burdensome task) that most interferes with the patient’s healthcare goal [6]. The information from the HPI process can then help clinicians consider if current care is consistent with a patient’s health priorities in the context of the patient’s health trajectory (e.g., disease progression) and then guide serial trials of starting, stopping or continuing medical interventions and help align care with health outcome goals which are intrinsically linked to ‘what matters’ (i.e., values) [7]. This requires consistent clinician–patient and clinician–clinician communication to find ways to best align healthcare [7]. The PPC approach is effective in achieving patient-centered care through the reduction in treatment burden and unwanted care (medications, tests, and self-care tasks) and increasing care that aligns with values in ambulatory care settings with older adults, including veterans [8].
The importance of priority-driven care is evident in subacute rehabilitation and skilled nursing facilities, such as VA community living centers (CLCs). In these settings, the prevalence of older adults with MCC and functional impairments requiring multiple therapeutic interventions or decisions is high [9]. Over the past two decades, VA CLCs have committed to providing high-quality, person-centered care in an effort to de-institutionalize nursing home care [10,11]. The PPC approach can reduce the treatment burden while aligning care to achieve healthcare goals that honor one’s values [8,12,13]. However, the feasibility of health priorities identification, let alone its influence on care alignment using the PPC approach in a skilled nursing facility (SNF) setting, has not been previously explored. Thus, the focus of this quality improvement project was to evaluate the fidelity, feasibility and acceptability of the health priorities identification (HPI) process from the PPC approach within the context of VA Community Living Centers (CLC). Through this work, our intention is to describe the logistical considerations, workflow, staff impressions and EHR tools necessary to systematically ask ‘what matters’ for veterans during their CLC admission and translate those values into specific, realistic and actionable health outcome goals.
2. Materials and Methods
2.1. Setting
The implementation of the HPI process was conducted as a quality improvement program in a single VA CLC located in Seattle, Washington. The CLC has 30 beds available for short-term rehabilitative or skilled nursing admissions. The unit is staffed with two physicians; two advanced practice nurses; physical, occupational, speech and recreational therapists; two social workers, a psychologist and a registered dietician. Nursing staff works as a team (one registered nurse (RN), one licensed practice nurse (LPN) and two to three nursing assistants (NAs)) overseeing twelve to fifteen patients. The average length of stay for veterans in 2021 was 32.3 days. Interdisciplinary team (IDT) meetings involved members of the care team from a variety of health professional disciplines (registered nurse and minimum data set nurse; occupational and physical therapists; physician; chaplain; advanced practice nurse and/or physician; psychologist; social worker) and the patient, themselves.
2.2. Health Priorities Identification (HPI)
The HPI process from PPC follows five steps where a facilitator (1) explores the patient’s values (i.e., what matters) within four domains shown to be most salient to older, medically complex individuals (connecting; enjoying life; managing health; and functioning) [3,14]; (2) translates values (i.e., what matters) into specific, realistic, and actionable health outcome goals; (3) identifies the most bothersome symptom, healthcare task or life/social circumstance which is getting in the way of achieving that goal; (4) elicits care preferences (i.e., how willing or unwilling a person may be to engage in a health behavior, treatment or therapy to achieve a particular health outcome goal [15]); and (5) determines the ‘one thing’ that a person wants to focus on so that they can reach their health outcome goal. The identification of the patient’s health priorities not only clarifies care preferences influencing patient and/or family decision making around healthcare, but documents how healthcare could be aligned to achieve the patient’s health outcome goals rooted in what matters [16]. The process could involve engagement with family or surrogate decision makers if/when cognitive impairment makes communication of health priorities difficult.
2.3. Health Priorities Identification (HPI) Implementation Strategy
2.3.1. Implementation Team
A multidisciplinary team of national PPC and quality-improvement experts using a practice change framework guided the training and integration of the HPI process from the PPC approach into the CLC workflow [17]. The team consisted of physicians and advanced practiced nurses specialized in geriatrics, who have experience working in the CLC setting; are experts in PPC development and implementation; or are health systems researchers familiar with CLC workforce enhancement.
Individuals from this national expert team met with the CLC workforce and leadership to determine intervention readiness (i.e., willingness to adapt workflow and support staff to undergo training) of leadership, staff and setting. These pre-intervention meetings provided an opportunity for CLC leadership to learn about the PPC approach, outline current documentation processes for admissions and IDT meetings and determine how best to integrate HPI encounters into the normal CLC workflow.
2.3.2. HPI Facilitator Training
The CLC leadership identified frontline staff who would be most appropriate to train as HPI facilitators, based on those persons’ time, willingness to participate and lead a quality improvement project, and experience and clinical background (e.g., motivated to expand communication skills and training; prior clinical training or experience in geriatrics or palliative care; well respected by their colleagues). Facilitators conducted HPI encounters for patients newly admitted to the CLC and represented a variety of health professions (registered nurse; occupational and physical therapist; physician; chaplain; advanced practice nurse; psychologist). The process for training has been described previously [13]. In short, facilitators reviewed asynchronous training videos (ranging from 20 min to 50 min), which provide a framework for eliciting patient health priorities using a motivational interviewing approach. The first video provides a PPC overview. The subsequent videos build the skills necessary for identification of health priorities: (1) explore values; (2) translate values into specific, realistic, actionable health outcome goals; (3) identify the most bothersome problem or symptom; (4) elicit care preferences (e.g., willingness or ability to engage in health behaviors); and (5) determine the ‘one thing’ that is getting in the way of the health outcome goal. Facilitators were also trained in strategies to align healthcare to achieve patient-directed goals, mostly provided as recommendations to the healthcare team. The facilitators encouraged IDT members to discuss considerations for healthcare alignment with the patient during IDT meetings. After completing the asynchronous training, the team of national experts in PPC provided in-person observations, EHR review and feedback to CLC-based HPI facilitators to enhance their skills and practice of the HPI process. Facilitators were independent in the HPI process after completing training videos and conducting two to three observed HPI encounters with feedback.
2.4. Implementation Measurement and Analysis
The focus of this quality improvement project was to evaluate the fidelity and feasibility of the health priorities identification process in a CLC setting. Structured meeting notes documented the progression through the first steps of each PDSA cycle (i.e., Plan; Do). The implementation of HPI into normal CLC processes was measured at the end of the first and second PDSA cycle (i.e., Study). Fidelity was assessed as the completeness of HPI documentation for each of the core steps mentioned previously (patient values; specific, actionable, realistic health outcomes; bothersome symptoms; healthcare preferences; the ‘one thing’) as well as integration of the health outcome goal and ‘one thing’ from the HPI into IDT meeting documentation. An EHR review was conducted by national experts in the PPC approach who evaluated all HPI discussions for encounter completion, quality of documented health outcome goal and ‘one thing’ and if the health outcome goal and ‘one thing’ was consistent with stated values, similar to prior implementation studies. This was performed using a validated chart review tool and PPC facilitators were aware of this process [18].
Intervention adoption (i.e., feasibility) was measured through the ability to complete HPI discussions with all patients newly admitted into the CLC and acceptance of HPI process integration into clinical assessments and workflow by staff. Qualitative interviews were conducted one-on-one with CLC-based HPI facilitators. All trained providers were invited to participate, but only five agreed to an interview. The primary interviewer was a medical sociologist with expertise in qualitative methods. Additionally, the interviewer was not part of the national expert implementation team and did not provide training and feedback. The interviewer used a semi-structured interview guide meant to elicit open-ended discussion of overall experiences with and reaction to the PPC intervention. Themes explored in these interviews included factors concerning the impact of PPC on workflow; barriers to implementation (staff buy-in, organizational barriers, patient-level barriers, others); HPI training and resources; recommendations for implementation and sustainment of the HPI approach in the CLC. Qualitative data were analyzed using an inductive rapid analytic technique and individual interviews were summarized in a spreadsheet according to the main thematic categories [19]. The study team then looked across interviews to identify patterns and recurring experiences and observations expressed across interviews. These patterns were then transformed into themes or a pattern iteratively identified in the data as an important research finding.
3. Results
Over the eight months of HPI process implementation, nine facilitators were trained and documented twenty HPI discussions with patients. HPI discussions occurred between patients and facilitators only and outside the context of the admission. The average length of stay for these patients was 56 days with one readmission to the hospital and no deaths. All facilitators completed asynchronous training videos, observation and feedback sessions during the first PDSA cycle. During the quality improvement program, there was no turnover of trained facilitators or IDT team members and only minimal turnover of CLC nursing staff not involved in the implementation project.
The first PDSA cycle included the first 10 HPI encounters, took an average of 40 min and occurred within the first week after admission. Review of the EHR indicated that the HPI process occurred in 60% of new admissions (Table 1). For patients who had an identification conversation, 66% of encounters included all core steps of the HPI process and 66% clearly documented the ‘one thing’ in the facilitator note. Twenty-two percent of facilitator notes had healthcare goals, which were specific, actionable, measurable and realistic. All were connected to the patient’s values. As for IDT care plan notes, 44% had documentation of health outcome goals that were consistent with the ‘one thing’ listed in the HPI facilitator notes.

Table 1.
PDSA breakdown and lessons learned from implementation evaluation.
The second PDSA cycle included developments to the program such as the development of a ‘Patient Health Priorities’-specific EHR template and notes (similar to: https://patientprioritiescare.org/wp-content/uploads/2021/12/Health-Priorities-Identificatin-template-note_Version2.pdf, accessed on 31 May 2023) (Figure 1); assigning facilitators to complete HPI encounters with each new admission; educational sessions for IDT members regarding the purpose of the program, overview of the HPI process within the PPC approach, location of HPI documentation and how to consider patient priorities during IDT care planning meetings (Table 1). With these changes, HPI encounters occurred with all patients within the first week of admission to the CLC (100%), but still took an average of 40 min to complete. The ‘Patient Health Priorities’ template and notes made HPI encounters easily identifiable in the EHR by all IDT members and facilitator documentation of the HPI core steps were complete for all encounters (100%). The quality of HPI documentation also improved. The quality of health outcome goals increased (66%) as well as the articulation of the ‘one thing’ (90%). Review of IDT care plan notes indicated an improvement in the consistency between the health outcome goals documented in the IDT notes and HPI encounters (78%).
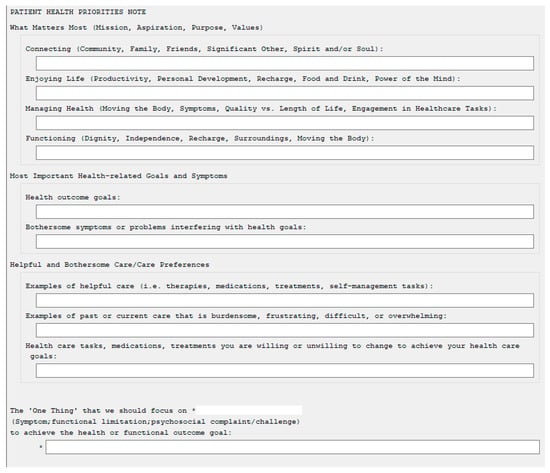
Figure 1.
Patient Health Priorities Note Template Example with HPI Core Steps.
Qualitative interviews with five facilitators indicated that the HPI process of PPC is very appropriate for the CLC setting, benefits patient care, and requires intentional leadership and interdisciplinary collaboration to achieve patient care alignment and build a more person-centered culture. Those interviewed felt that the HPI process of the PPC approach supported provider work (regardless of license or role) and at times made it easier (Table 2). The HPI process is sustainable and impactful as long as information gained from these discussions is incorporated in team-based meetings. Documentation is not burdensome but should be located in a consistent place in the EHR so that all providers can easily reference patient priorities. Leadership support and sponsorship facilitates program adoption and is essential for initial start-up and sustainability. Threats and barriers identified by those interviewed include staffing vacancies (causing cross-cover of duties and reduction in admissions), patient-related cognitive impairment (e.g., dementia, poor health literacy, psychological distress or serious mental health diagnosis), resistance to culture change (shift in way clinicians view and speak to veterans), and confidence in ability to probe if/when the conversation stalls (flexibility and creativity with exploration of values and priorities) (Table 2).

Table 2.
Staff Impressions of HPI Integration into the Community Living Center Workflow.
4. Discussion
We demonstrated that the HPI process of the PPC approach is a feasible and acceptable method for eliciting the ‘what matters’ component of AFHS in the CLC setting. Fidelity evaluation of HPI documentation also suggests that many different healthcare professionals can be trained in this process and determine health outcome goals and the ‘one thing’ rooted in what matters to facilitate person-centered care alignment in a CLC setting. The HPI process and documentation was not burdensome to staff, complemented normal workflow processes and was quickly mastered. Based on qualitative interviews, facilitators felt that the HPI process aligned with their clinical work, did not add significant time and provided a supportive framework for exploring what matters. The development of specific, measurable, realistic healthcare goals connected to stated values was improved by deliberate modifications in the second PDSA cycle (e.g., EHR tools and enhanced IDT member awareness of HPI encounters). Lastly, qualitative feedback from our program evaluation indicated that the HPI process changed how providers ‘see their patients.’ Facilitators shared that the HPI process of PPC helped them connect with a patients’ humanity and not see them as a combination of their health complications or functional limitations. Prior work in PPC and other serious illness communication programs supports this finding [12,20]. Setting aside time and space for conversations, which explore who a person is and what is most important to them, can develop a culture of person-centered care.
Patients in SNFs have medical and psychological complexity greater than community counterparts, have undergone a recent change in functional status and have a high risk of mortality [9,21]. Thus, it is appropriate for clinicians in these settings to reexamine if patient health priorities and their medical plan align if/when current care plans are discordant with a patient’s stated goals [22]. In 2015, the Agency for Healthcare Research and Quality (AHRQ) presented the SHARE approach, a streamlined shared decision-making model to help patients with their clinicians choose between evidence-based options, which are often in equipoise [23]. The SHARE approach comprises five steps (Seek, Help, Assess, Reach, Evaluate) with training that informs clinicians on how to perform each step [24]. PPC and SHARE approaches elevate the importance of providing care based on a person’s values and preferences [25]. However, the PPC approach provides the opportunity for healthcare providers to explore a person’s values and preferences in the context of their disease trajectory and clarify health outcome goals based on what healthcare tasks or treatments patients are willing or unwilling to participate in. Using the PPC approach to align care with ‘what matters’ can guide Age-Friendly Care delivered in any setting.
Implementation of PPC into a setting such as an SNF requires commitment from leadership and staff to make integration of this approach feasible and sustainable. Lessons learned from our implementation evaluation mirror those observed in other serious illness communication programs and are helpful for a variety of healthcare dissemination practices and could guide PPC implementation in other non-VA settings [20]. We found that transparent and consistent EHR documentation elevated the significance of the HPI encounter and a patient’s stated values and goals. The use of EHR templates, trainings and feedback sessions strengthen facilitator skills in defining healthcare goals, which translated to clearer communication to IDT members. Implementation champions, or in this case, facilitators, should include persons who are motivated, respected by their colleagues, diverse in clinical and cultural backgrounds and willing to share the ‘work’ of implementation. Lastly, HPI encounters and documentation take time and may conflict with other work-related tasks and patient care. Leadership support is instrumental to overcoming the effort required for program integration that in the short-term competes with other setting-specific priorities, such as staffing, documentation, and other quality improvement and assurance initiatives. If the leadership team sets a clear tone of support and expectation of documenting change, then the implementation is more likely. Resources and time need to be allocated for staff training as well as encouragement for modifications to workflow or clinical tasks. Having multiple HPI facilitators of different clinical backgrounds was essential to the sustainability of this program in a CLC setting. It provided flexibility in times of staffing shortage, increased turnover and a diversity of clinical perspectives. Though the HPI process was not perceived as burdensome, sharing the role of HPI facilitation with others made integration more sustainable for the CLC staff. To help integration, the national PPC team has active websites with toolkits to support implementation in VA and non-VA settings (Implementation Toolkit—Patient Priorities Care; Patient Priorities Care VA Implementation Toolkit—Patient Priorities Care VA Implementation Toolkit).
There are several limitations to our study. Future studies will need to explore how HPI encounters and documentation can inform care alignment in the CLC and thus improve the patient experience of care vs. measures of quality of care. Though we reviewed integration of the HPI process of the PPC approach in IDT documentation, we did not analyze how the articulation of patient-stated priorities and goals was translated into distinct treatment decisions nor how those goals might need to change due to acute changes to health status (i.e., hospitalizations). A larger, prospective study with a control group could better evaluate if the PPC approach is associated with treatment differences observed in the medical record, such as length of stay, which was significantly longer during our QI intervention. Other systematic changes (e.g., changes to IDT documentation better incorporating patient preferences and priorities; staff education of the PPC approach; culture change and increased familiarity with HPI documentation) could improve the care alignment in IDT based on the HPI encounter. Second, our study was limited to a small VA-based CLC. Though there are many similarities between CLC populations and settings and community-based SNFs, it may be difficult to generalize our successes with implementation in other SNF settings where staff turnover might be higher. Lastly, our qualitative interviews were limited in scope and omitted the voice of the veteran and/or family. The interviewer did not oversee PPC training or feedback and interviews were blinded to the implementation team and CLC leadership. However, the low number of interviewees may bias the interpretations given and limit the generalizability of staff perceptions of the acceptability of this approach. Future work can explore the impact of the HPI process on patient/family perceptions of quality of care and other measures of ‘value-based’ care which impact SNF ratings, reimbursement and incentive payments.
5. Conclusions
Identification of health priorities using the core steps from the PPC approach is feasible in the context of normal CLC operations and can reliably translate ‘what matters,’ into specific, realistic and actionable health outcome goals. Implementation requires motivated workforce champions, supportive leadership and uncomplicated EHR tools. Our work will help guide other institutions interested in becoming Age-Friendly and incorporating PPC as their method for guiding patient care around ‘what matters’.
Author Contributions
Formal Analysis, K.C.R., A.D.N., L.M.S., S.W.C. and C.G.; Data Curation, E.M. and L.K.; Writing—Original Draft Preparation, all authors; Writing—Review and Editing, all authors; Visualization, E.M. and L.K.; Project Administration, K.C.R., L.M.S. and L.K. All authors have read and agreed to the published version of the manuscript.
Funding
Funding for this project was supported by the Office of Geriatrics and Extended Care and Veterans Integrated Services (VISN) 20 and analysis was partly supported by the use of facilities and resources at the Center for Innovations in Quality, Effectiveness and Safety (CIN 13-413), Michael E. DeBakey VA Medical Center, Houston, TX, USA.
Institutional Review Board Statement
Local VA research service guidelines were followed and the study was granted a non-research designation not requiring formal IRB review.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the sensitive nature of staff interviews.
Acknowledgments
We would like to thank Whitney Mills and Caroline Madgril for their assistance and guidance during early stages of this project. We would also like to acknowledge the tireless work of Kathryn Anderson and Sarah Punshon who participated in this quality improvement and worked to change patient care for the better.
Conflicts of Interest
The authors declare that they have no conflict of interest.
References
- Stange, K.C. In This Issue: Challenges of Managing Multimorbidity. Ann. Fam. Med. 2012, 10, 2–3. [Google Scholar] [CrossRef]
- Tinetti, M.E. The gap between clinical trials and the real world: Extrapolating treatment effects from younger to older adults. JAMA Intern. Med. 2014, 174, 397–398. [Google Scholar] [CrossRef]
- Naik, A.D.; Martin, L.A.; Moye, J.; Karel, M.J. Health Values and Treatment Goals of Older, Multimorbid Adults Facing Life-Threatening Illness. J. Am. Geriatr. Soc. 2016, 64, 625–631. [Google Scholar] [CrossRef]
- Institute for Healthcare Improvement: What is an Age-Friendly System. Available online: http://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Pages/default.aspx (accessed on 24 March 2022).
- Tinetti, M.E.; Costello, D.M.; Naik, A.D.; Davenport, C.; Hernandez-Bigos, K.; Van Liew, J.R.; Esterson, J.; Kiwak, E.; Dindo, L. Outcome Goals and Health Care Preferences of Older Adults with Multiple Chronic Conditions. JAMA Netw. Open 2021, 4, e211271. [Google Scholar] [CrossRef]
- Naik, A.; Tinetti, M.; Dindo, L. Available online: https://patientprioritiescare.org/wp-content/uploads/2022/02/ppc-health-priorities-1024x576.jpg (accessed on 8 April 2022).
- Tinetti, M.; Dindo, L.; Smith, C.D.; Blaum, C.; Costello, D.; Ouellet, G.; Rosen, J.; Hernandez-Bigos, K.; Geda, M.; Naik, A. Challenges and strategies in patients’ health priorities-aligned decision-making for older adults with multiple chronic conditions. PLoS ONE 2019, 14, e0218249. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Naik, A.D.; Dindo, L.; Costello, D.M.; Esterson, J.; Geda, M.; Rosen, J.; Hernandez-Bigos, K.; Smith, C.D.; Ouellet, G.M.; et al. Association of Patient Priorities-Aligned Decision-Making with Patient Outcomes and Ambulatory Health Care Burden Among Older Adults With Multiple Chronic Conditions: A Nonrandomized Clinical Trial. JAMA Intern. Med. 2019, 179, 1688–1697. [Google Scholar] [CrossRef]
- Van den Brink, A.M.; Gerritsen, D.L.; Voshaar, R.C.; Koopmans, R.T. Residents with mental-physical multimorbidity living in long-term care facilities: Prevalence and characteristics. A systematic review. Int. Psychogeriatr. 2013, 25, 531–548. [Google Scholar] [CrossRef]
- Hojlo, C. The VA’s Transformation of Nursing Home Care: From Nursing Homes to Community Living Centers. Generations 2010, 34, 43–48. [Google Scholar]
- Thomas, K.S.; Cote, D.; Makineni, R.; Intrator, O.; Kinosian, B.; Phibbs, C.S.; Allen, S.M. Change in VA Community Living Centers 2004–2011: Shifting Long-Term Care to the Community. J. Aging Soc. Policy 2018, 30, 93–108. [Google Scholar] [CrossRef]
- Ouellet, G.M.; Kiwak, E.; Costello, D.M.; Green, A.R.; Geda, M.; Naik, A.D.; Tinetti, M.E. Clinician Perspectives on Incorporating Patients’ Values-Based Health Priorities in Decision-Making. J. Am. Geriatr. Soc. 2021, 69, 267–269. [Google Scholar] [CrossRef]
- Jd, J.F.; Dindo, L.; Catic, A.; Johnson, A.; Amspoker, A.B.; Gravier, A.; Dawson, D.B.; Tinetti, M.E.; Naik, A.D. Feasibility of Clinicians Aligning Health Care with Patient Priorities in Geriatrics Ambulatory Care. J. Am. Geriatr. Soc. 2020, 68, 2112–2116. [Google Scholar] [CrossRef]
- Naik, A.D.; Dindo, L.N.; Liew, J.R.; Hundt, N.E.; Vo, L.; Hernandez-Bigos, K.; Esterson, J.; Geda, M.; Rosen, J.; Blaum, C.S.; et al. Development of a Clinically Feasible Process for Identifying Individual Health Priorities. J. Am. Geriatr. Soc. 2018, 66, 1872–1879. [Google Scholar] [CrossRef]
- Warren, C.; McGraw, A.P.; Van Boven, L. Values and preferences: Defining preference construction. WIREs Cogn. Sci. 2011, 2, 193–205. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Esterson, J.; Ferris, R.; Posner, P.; Blaum, C.S. Patient Priority–Directed Decision Making and Care for Older Adults with Multiple Chronic Conditions. Clin. Geriatr. Med. 2016, 32, 261–275. [Google Scholar] [CrossRef]
- Solberg, L.I. Improving Medical Practice: A Conceptual Framework. Ann. Fam. Med. 2007, 5, 251–256. [Google Scholar] [CrossRef]
- Blaum, C.S.; Rosen, J.; Naik, A.D.; Smith, C.D.; Dindo, L.; Vo, L.; Ba, K.H.; Esterson, J.; Geda, M.; Ferris, R.; et al. Feasibility of Implementing Patient Priorities Care for Older Adults with Multiple Chronic Conditions. J. Am. Geriatr. Soc. 2018, 66, 2009–2016. [Google Scholar] [CrossRef]
- Neal, J.W.; Neal, Z.P.; VanDyke, E.; Kornbluh, M. Expediting the Analysis of Qualitative Data in Evaluation:A Procedure for the Rapid Identification of Themes From Audio Recordings (RITA). Am. J. Eval. 2015, 36, 118–132. [Google Scholar] [CrossRef]
- Lagrotteria, A.; Swinton, M.; Simon, J.; King, S.; Boryski, G.; Ma, I.W.Y.; Dunne, F.; Singh, J.; Bernacki, R.E.; You, J.J. Clinicians’ Perspectives After Implementation of the Serious Illness Care Program: A Qualitative Study. JAMA Netw. Open 2021, 4, e2121517. [Google Scholar] [CrossRef]
- Lage, D.E.; Caudry, D.J.; Ackerly, D.C.; Keating, N.L.; Grabowski, D.C. The Care Continuum for Hospitalized Medicare Beneficiaries Near Death. Ann. Intern. Med. 2018, 168, 748. [Google Scholar] [CrossRef]
- Davenport, C.; Ouellet, J.; Tinetti, M.E. Use of the Patient-Identified Top Health Priority in Care Decision-making for Older Adults With Multiple Chronic Conditions. JAMA Netw. Open 2021, 4, e2131496. [Google Scholar] [CrossRef]
- The Agency for Healthcare Research and Quality: The Share Approach. Available online: https://www.ahrq.gov/health-literacy/curriculum-tools/shareddecisionmaking/index.html (accessed on 8 June 2022).
- The Agency for Healthcare Quality. The SHARE Approach-Essential Steps of Shared Decision Making: Quick Reference Guide. Available online: https://www.ahrq.gov/health-literacy/professional-training/shared-decision/tool/resource-2.html (accessed on 8 June 2020).
- Van Haitsma, K.; Abbott, K.M.; Arbogast, A.; Bangerter, L.R.; Heid, A.R.; Behrens, L.L.; Madrigal, C. A Preference-Based Model of Care: An Integrative Theoretical Model of the Role of Preferences in Person-Centered Care. Gerontologist 2020, 60, 376–384. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).