Preoperative Risk Factors Associated with Increased Incidence of Postoperative Delirium: Systematic Review of Qualified Clinical Studies
Abstract
1. Introduction
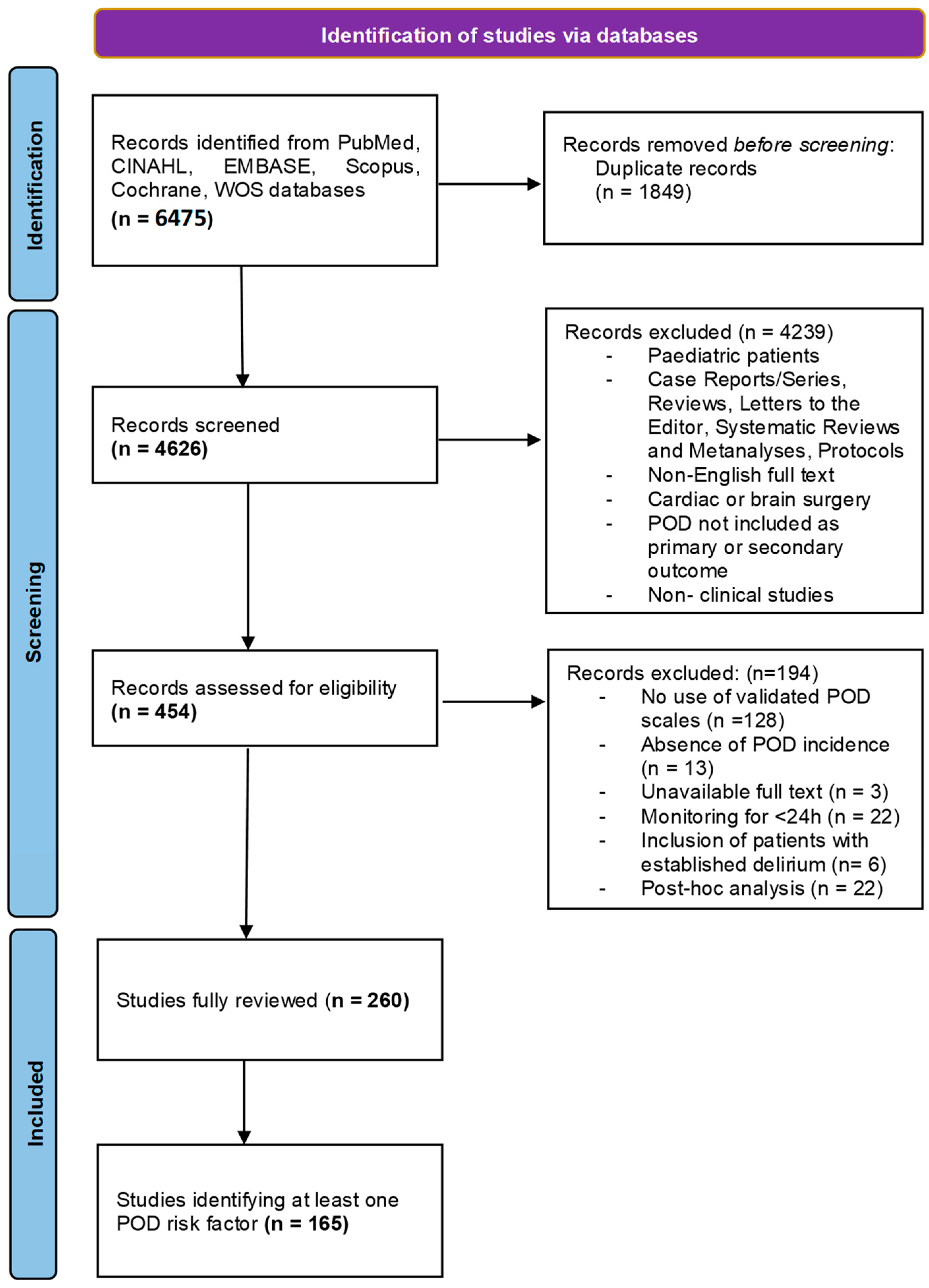
2. Methods
3. Results
3.1. Types of Scales Used
3.2. Demographics
3.3. Laboratory Testing
3.4. Cumulative Indicators
3.5. Comorbidities
3.6. Chronic Therapies
3.7. Habits
3.8. Type of Surgery
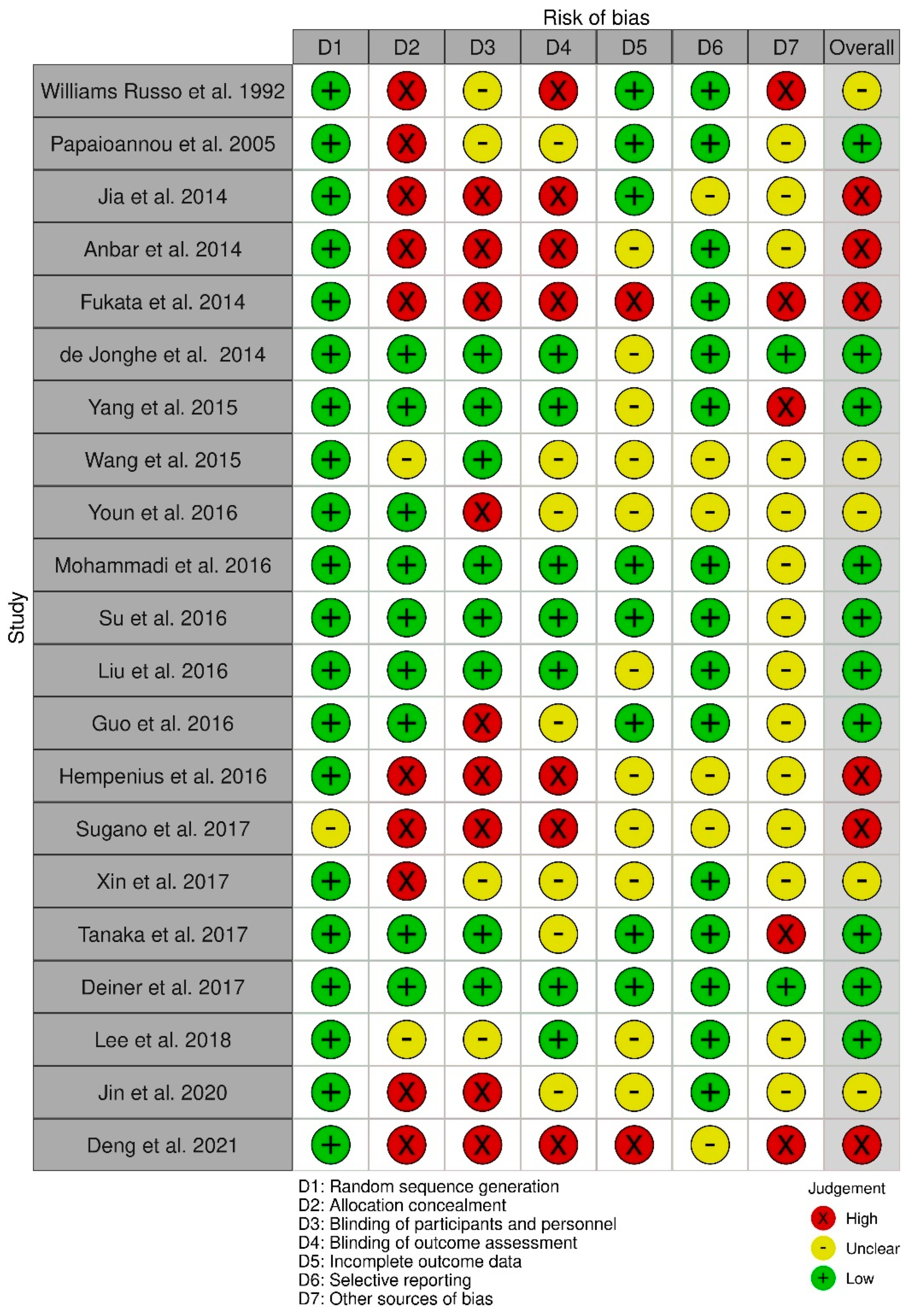
3.9. Risk of Bias Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Full List of Literature Search Strings
- PubMed: (delirium OR delirious OR confusion OR disorientation OR bewilderment) AND (postoperative OR “postoperative” OR post intervention OR “post intervention” OR “post-surgical” OR postsurgical OR “post-surgery” OR post surgery OR “anesthesia recovery” OR “anesthesia recovery” OR “anesthesia recovery period”[- Mesh] OR post anesthesia OR “post anesthesia” OR “post anesthesia”)
- EMBASE: (((‘delirium’/exp OR delirium OR delirious OR ‘confusion’/exp OR confusion OR ‘disorientation’/exp OR disorientation OR bewilderment) AND (‘postoperative complication’/exp OR postoperative OR ‘post-operative’ OR ‘postoperative period’/exp OR post-intervention OR ‘post intervention’ OR ‘post-surgical’ OR postsurgical OR ‘post-surgery’ OR post-surgery OR ‘anesthesia recovery’/exp OR ‘anesthesia recovery’ OR ‘anesthesia recovery’/exp OR ‘anesthesia recovery’ OR post anesthesia OR ‘post anesthesia’ OR ‘post anesthesia’)) OR ‘postoperative delirium’/exp) AND ([cochrane review]/lim OR [systematic review]/lim OR [meta-analysis]/lim OR [randomized controlled trial]/lim OR ‘observational study’ OR ‘case study’)
- CINAHL: (delirium OR delirious OR confusion OR disorientation OR bewilderment) AND (postoperative OR “postoperative” OR post intervention OR “post intervention” OR “post-surgical” OR postsurgical OR “post-surgery” OR post-surgery OR “anesthesia recovery” OR “anesthesia recovery” OR post anesthesia OR “post anesthesia” OR “post anesthesia”) Limiters—Publication Type: Case Study, MetaAnalysis, Randomized Controlled Trial, Systematic Review OR ((delirium OR delirious OR confusion OR disorientation OR bewilderment) AND (postoperative OR “postoperative” OR post intervention OR “post intervention” OR “post-surgical” OR postsurgical OR “post-surgery” OR post-surgery OR “anesthesia recovery” OR “anesthesia recovery” OR post anesthesia OR “post anesthesia” OR “post anesthesia”)) AND (observational study OR observational research) OR (MH “delirium” OR MH “confusion+”) AND ((MH “postoperative complications”) OR (MH “postoperative period”)) Limiters—Publication Type: Case Study, MetaAnalysis, Randomized Controlled Trial, Systematic Review OR (MH “delirium” OR MH “confusion+”) AND ((MH “postoperative complications”) OR (MH “postoperative period”)) AND ((observational study OR observational research))
- COCHRANE: #1 ((delirium OR delirious OR confusion OR disorientation OR bewilderment) AND (postoperative OR “postoperative” OR post intervention OR “post intervention” OR “post-surgical” OR postsurgical OR “post-surgery” OR post-surgery OR “anesthesia recovery” OR “anesthesia recovery” OR post anesthesia OR “post anesthesia” OR “post anesthesia”)):ti,ab,kw 1829 #2 MeSH descriptor: [Delirium] explode all trees 765 #3 MeSH descriptor: [Confusion] explode all trees 899 #4 #2 OR #3 899 #5 MeSH descriptor: [Postoperative Period] explode all trees 5872 #6 MeSH descriptor: [Postoperative Complications] explode all trees 39635 #7 MeSH descriptor: [Anesthesia Recovery Period] explode all trees 2031 #8 #5 OR #6 OR #7 43861 #9 #4 AND #8 326 #10 #1 OR #9 1853
- SCOPUS: TITLE-ABS (delirium OR delirious OR confusion OR disorientation OR bewilderment) AND TITLE-ABS (postoperative OR {post-operative} OR post intervention OR {post intervention} OR {post-surgical} OR postsurgical OR {post-surgery} OR post-surgery OR {anesthesia recovery} OR {anesthesia recovery} OR post anesthesia OR {post anesthesia} OR {post anesthesia}) AND TITLE-ABS ({systematic review} OR {case series} OR {randomized controlled trial} OR rct OR {meta-analysis} OR metanalysis OR {observational study})
- WEB OF SCIENCE: TITLE-ABS (delirium OR delirious OR confusion OR disorientation OR bewilderment) AND TITLE-ABS (postoperative OR {post-operative} OR post intervention OR {post intervention} OR {post-surgical} OR postsurgical OR {post-surgery} OR post-surgery OR {anesthesia recovery} OR {anesthesia recovery} OR post anesthesia OR {post anesthesia} OR {post anesthesia}) AND TITLE-ABS ({systematic review} OR {case series} OR {randomized controlled trial} OR rct OR {meta-analysis} OR metanalysis OR {observational study})
References
- ICD-10 Version:2016. Available online: https://icd.who.int/browse10/2016/en#/F05.8 (accessed on 21 June 2022).
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (Dsm-5), 5th ed.; Psychiatric Pub Inc.: Washington, DC, USA, 2013. [Google Scholar]
- Fadayomi, A.B.; Ibala, R.; Bilotta, F.; Westover, M.B.; Akeju, O. A Systematic Review and Meta-Analysis Examining the Impact of Sleep Disturbance on Postoperative Delirium. Crit. Care Med. 2018, 46, E1204–E1212. [Google Scholar] [CrossRef] [PubMed]
- Daiello, L.A.; Racine, A.M.; Yun Gou, R.; Marcantonio, E.R.; Xie, Z.; Kunze, L.J.; Vlassakov, K.V.; Inouye, S.K.; Jones, R.N.; Alsop, D.; et al. Postoperative Delirium and Postoperative Cognitive Dysfunction: Overlap and Divergence. Anesthesiology 2019, 131, 477–491. [Google Scholar] [CrossRef] [PubMed]
- Wittmann, M.; Kirfel, A.; Jossen, D.; Mayr, A.; Menzenbach, J. The Impact of Perioperative and Predisposing Risk Factors on the Development of Postoperative Delirium and a Possible Gender Difference. Geriatrics 2022, 7, 65. [Google Scholar] [CrossRef] [PubMed]
- Inouye, S.K.; Westendorp, R.G.J.; Saczynski, J.S. Delirium in Elderly People. Lancet 2014, 383, 911–922. [Google Scholar] [CrossRef]
- Aldecoa, C.; Bettelli, G.; Bilotta, F.; Sanders, R.D.; Audisio, R.; Borozdina, A.; Cherubini, A.; Jones, C.; Kehlet, H.; Maclullich, A.; et al. European Society of Anaesthesiology Evidence-Based and Consensus-Based Guideline on Postoperative Delirium. Eur. J. Anaesthesiol. 2017, 34, 192–214. [Google Scholar] [CrossRef]
- Hála, M. Pathophysiology of Postoperative Delirium: Systemic Inflammation as a Response to Surgical Trauma Causes Diffuse Microcirculatory Impairment. Med. Hypotheses 2007, 68, 194–196. [Google Scholar] [CrossRef]
- Steiner, L.A. Postoperative Delirium. Part 1: Pathophysiology and Risk Factors. Eur. J. Anaesthesiol. 2011, 28, 628–636. [Google Scholar] [CrossRef]
- Hermanides, J.; Qeva, E.; Preckel, B.; Bilotta, F. Perioperative Hyperglycemia and Neurocognitive Outcome after Surgery: A Systematic Review. Minerva Anestesiol. 2018, 84, 1178–1188. [Google Scholar] [CrossRef]
- Borozdina, A.; Qeva, E.; Cinicola, M.; Bilotta, F. Perioperative Cognitive Evaluation. Curr. Opin. Anaesthesiol. 2018, 31, 756–761. [Google Scholar] [CrossRef]
- Falegnami, A.; Patriarca, R.; Costantino, F.; di Gravio, G.; Bilotta, F. Surveying Work-as-Done in Post-Operative Delirium Risk Factors Collection and Diagnosis Monitoring. Appl. Ergon. 2021, 92, 3347. [Google Scholar] [CrossRef]
- Viderman, D.; Brotfain, E.; Bilotta, F.; Zhumadilov, A. Risk Factors and Mechanisms of Postoperative Delirium After Intracranial Neurosurgical Procedures. Asian J. Anesthesiol. 2020, 58, 5–13. [Google Scholar] [CrossRef]
- Delp, S.; Mei, W.; Spies, C.D.; Neuner, B.; Aldecoa, C.; Bettelli, G.; Bilotta, F.; Sanders, R.D.; Kramer, S.; Weiss, B. Clinical Practice in the Management of Postoperative Delirium by Chinese Anesthesiologists: A Cross-Sectional Survey Designed by the European Society of Anaesthesiology. J. Int. Med. Res. 2020, 48, 7207. [Google Scholar] [CrossRef]
- Nishikawa, K.; Nakayama, M.; Omote, K.; Namiki, A. Recovery Characteristics and Post-Operative Delirium after Long-Duration Laparoscope-Assisted Surgery in Elderly Patients: Propofol-Based vs. Sevoflurane-Based Anesthesia. Acta Anaesthesiol. Scand. 2004, 48, 162–168. [Google Scholar] [CrossRef]
- Bilotta, F.; Giordano, G.; Pugliese, F. Preoperative Stratification for Postoperative Delirium: Obstructive Sleep Apnea Is a Predictor, the STOP-BANG Is Not? J. Thorac. Dis. 2019, 11, S202–S206. [Google Scholar] [CrossRef]
- Litaker, D.; Locala, J.; Franco, K.; Bronson, D.L.; Tannous, Z. Preoperative Risk Factors for Postoperative Delirium. Gen. Hosp. Psychiatry 2001, 23, 84–89. [Google Scholar] [CrossRef]
- Shah, S.; Weed, H.G.; He, X.; Agrawal, A.; Ozer, E.; Schuller, D.E. Alcohol-Related Predictors of Delirium after Major Head and Neck Cancer Surgery. Arch. Otolaryngol. Head Neck Surg. 2012, 138, 266–271. [Google Scholar] [CrossRef]
- Cotoia, A.; Mirabella, L.; Beck, R.; Matrella, P.; Assenzo, V.; Hazot, T.C.; Cinnella, G.; Liu, N.; Dambrosio, M. Effects of Closed-Loop Intravenous Anesthesia Guided by Bispectral Index in Adult Patients on Emergence Delirium: A Randomized Controlled Study. Minerva Anestesiol. 2018, 84, 437–446. [Google Scholar] [CrossRef]
- Todd, O.M.; Gelrich, L.; MacLullich, A.M.; Driessen, M.; Thomas, C.; Kreisel, S.H. Sleep Disruption at Home As an Independent Risk Factor for Postoperative Delirium. J. Am. Geriatr. Soc. 2017, 65, 949–957. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Bilotta, F.; Russo, G.; Trombi, M.; Verrengia, M.; Sangermano, C.; Sportelli, A.; Foti, L.; Villa, G.; Romagnoli, S. Comprehensive Analysis of Clinical Evidence on Postoperative Delirium: Literature Search and Screening of Original Studies That Used Validated Diagnostic Scales. PROSPERO 2021, CRD42021246906. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=246906 (accessed on 21 June 2022).
- Resources|Cochrane Bias. Available online: https://methods.cochrane.org/bias/resources (accessed on 21 June 2022).
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2011, 343, D5928. [Google Scholar] [CrossRef] [PubMed]
- Williams-Russo, P.; Urquhart, B.L.; Sharrock, N.E.; Charlson, M.E. Post-Operative Delirium: Predictors and Prognosis in Elderly Orthopedic Patients. J. Am. Geriatr. Soc. 1992, 40, 759–767. [Google Scholar] [CrossRef] [PubMed]
- Papaioannou, A.; Fraidakis, O.; Michaloudis, D.; Balalis, C.; Askitopoulou, H. The Impact of the Type of Anaesthesia on Cognitive Status and Delirium during the First Postoperative Days in Elderly Patients. Eur. J. Anaesthesiol. 2005, 22, 492–499. [Google Scholar] [CrossRef] [PubMed]
- Freter, S.H.; Dunbar, M.J.; MacLeod, H.; Morrison, M.; MacKnight, C.; Rockwood, K. Predicting Post-Operative Delirium in Elective Orthopaedic Patients: The Delirium Elderly At-Risk (DEAR) Instrument. Age Ageing 2005, 34, 169–171. [Google Scholar] [CrossRef]
- Schrader, S.L.P.; Wellik, K.E.; Demaerschalk, B.M.; Caselli, R.J.; Woodruff, B.K.; Wingerchuk, D.M. Adjunctive Haloperidol Prophylaxis Reduces Postoperative Delirium Severity and Duration in At-Risk Elderly Patients. Neurologist 2008, 14, 134–137. [Google Scholar] [CrossRef]
- da Cunha, P.T.S.; Artifon, A.N.; Lima, D.P.; Marques, W.V.; Rahal, M.A.; Ribeiro, R.R.; Kitadai, F.T. Hip Fractures in the Elderly: Surgical Treatment Timing and Its Correlation with Delirium and Infection. Acta Ortop. Bras. 2008, 16, 173–176. [Google Scholar] [CrossRef]
- Robinson, T.N.; Raeburn, C.D.; Angles, E.M.; Moss, M. Low Tryptophan Levels Are Associated with Postoperative Delirium in the Elderly. Am. J. Surg. 2008, 196, 670–674. [Google Scholar] [CrossRef]
- Gao, R.; Yang, Z.Z.; Li, M.; Shi, Z.C.; Fu, Q. Probable Risk Factors for Postoperative Delirium in Patients Undergoing Spinal Surgery. Eur. Spine J. 2008, 17, 1531. [Google Scholar] [CrossRef]
- Tognoni, P.; Simonato, A.; Robutti, N.; Pisani, M.; Cataldi, A.; Monacelli, F.; Carmignani, G.; Odetti, P. Preoperative Risk Factors for Postoperative Delirium (POD) after Urological Surgery in the Elderly. Arch Gerontol. Geriatr. 2011, 52, 21. [Google Scholar] [CrossRef]
- Patti, R.; Saitta, M.; Cusumano, G.; Termine, G.; di Vita, G. Risk Factors for Postoperative Delirium after Colorectal Surgery for Carcinoma. Eur. J. Oncol. Nurs. 2011, 15, 519–523. [Google Scholar] [CrossRef]
- Mangnall, L.T.; Gallagher, R.; Stein-Parbury, J. Postoperative Delirium After Colorectal Surgery in Older Patients. Am. J. Crit. Care 2011, 20, 45–55. [Google Scholar] [CrossRef]
- Lee, H.J.; Hwang, D.S.; Wang, S.K.; Chee, I.S.; Baeg, S.; Kim, J.L. Early Assessment of Delirium in Elderly Patients after Hip Surgery. Psychiatry Investig. 2011, 8, 340–347. [Google Scholar] [CrossRef]
- Jankowski, C.J.; Trenerry, M.R.; Cook, D.J.; Buenvenida, S.L.; Stevens, S.R.; Schroeder, D.R.; Warner, D.O. Cognitive and Functional Predictors and Sequelae of Postoperative Delirium in Elderly Patients Undergoing Elective Joint Arthroplasty. Anesth. Analg. 2011, 112, 1186–1193. [Google Scholar] [CrossRef]
- Do, T.D.; Lemogne, C.; Journois, D.; Safran, D.; Consoli, S.M. Low Social Support Is Associated with an Increased Risk of Postoperative Delirium. J. Clin. Anesth. 2012, 24, 126–132. [Google Scholar] [CrossRef]
- Jia, Y.; Jin, G.; Guo, S.; Gu, B.; Jin, Z.; Gao, X.; Li, Z. Fast-Track Surgery Decreases the Incidence of Postoperative Delirium and Other Complications in Elderly Patients with Colorectal Carcinoma. Langenbecks Arch. Surg. 2014, 399, 77–84. [Google Scholar] [CrossRef]
- Fineberg, S.J.; Nandyala, S.V.; Marquez-Lara, A.; Oglesby, M.; Patel, A.A.; Singh, K. Incidence and Risk Factors for Postoperative Delirium after Lumbar Spine Surgery. Spine 2013, 38, 1790–1796. [Google Scholar] [CrossRef]
- Large, M.C.; Reichard, C.; Williams, J.T.B.; Chang, C.; Prasad, S.; Leung, Y.; Dubeau, C.; Bales, G.T.; Steinberg, G.D. Incidence, Risk Factors, and Complications of Postoperative Delirium in Elderly Patients Undergoing Radical Cystectomy. Urology 2013, 81, 123–129. [Google Scholar] [CrossRef]
- Wu, Y.; Wang, J.; Wu, A.S.; Yue, Y. Do Fluctuations in Endogenous Melatonin Levels Predict the Occurrence of Postoperative Cognitive Dysfunction (POCD)? Int. J. Neurosci. 2014, 124, 787–791. [Google Scholar] [CrossRef]
- Deiner, S.; Lin, H.M.; Bodansky, D.; Silverstein, J.; Sano, M. Do Stress Markers and Anesthetic Technique Predict Delirium in the Elderly? Dement. Geriatr. Cogn. Disord. 2014, 38, 366–374. [Google Scholar] [CrossRef]
- de Jonghe, A.; van Munster, B.C.; Goslings, J.C.; Kloen, P.; van Rees, C.; Wolvius, R.; van Velde, R.; Levi, M.; de Haan, R.J.; de Rooij, S.E.; et al. Effect of Melatonin on Incidence of Delirium among Patients with Hip Fracture: A Multicentre, Double-Blind Randomized Controlled Trial. CMAJ 2014, 186, E547–E556. [Google Scholar] [CrossRef]
- Saporito, A.; Sturini, E. Incidence of Postoperative Delirium Is High Even in a Population without Known Risk Factors. J. Anesth. 2014, 28, 198–201. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.L.; Lin, H.C.; Lin, K.H.; Lin, L.S.; Hsieh, C.E.; Ko, C.J.; Hung, Y.J.; Lin, P.Y. Low Hemoglobin Level Is Associated with the Development of Delirium after Hepatectomy for Hepatocellular Carcinoma Patients. PLoS ONE 2015, 10, e0119199. [Google Scholar] [CrossRef] [PubMed]
- Tai, S.; Xu, L.; Zhang, L.; Fan, S.; Liang, C. Preoperative Risk Factors of Postoperative Delirium after Transurethral Prostatectomy for Benign Prostatic Hyperplasia. Int. J. Clin. Exp. Med. 2015, 8, 4569–4574. [Google Scholar] [CrossRef] [PubMed]
- Gottschalk, A.; Hubbs, J.; Vikani, A.R.; Gottschalk, L.B.; Sieber, F.E. The Impact of Incident Postoperative Delirium on Survival of Elderly Patients After Surgery for Hip Fracture Repair. Anesth. Analg. 2015, 121, 1336–1343. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Chen, J.; Wu, G. Variable Lung Protective Mechanical Ventilation Decreases Incidence of Postoperative Delirium and Cognitive Dysfunction during Open Abdominal Surgery. Int. J. Clin. Exp. Med. 2015, 8, 21208–21214. [Google Scholar]
- Raats, J.W.; van Eijsden, W.A.; Crolla, R.M.P.H.; Steyerberg, E.W.; van der Laan, L. Risk Factors and Outcomes for Postoperative Delirium after Major Surgery in Elderly Patients. PLoS ONE 2015, 10, 0136071. [Google Scholar] [CrossRef]
- Kratz, T.; Heinrich, M.; Schlauß, E.; Diefenbacher, A. Preventing Postoperative Delirium. Dtsch. Arztebl. Int. 2015, 112, 0289. [Google Scholar] [CrossRef]
- Liang, C.K.; Chu, C.L.; Chou, M.Y.; Lin, Y.T.; Lu, T.; Hsu, C.J.; Lam, H.C.; Chen, L.K. Developing a Prediction Model for Post-Operative Delirium and Long-Term Outcomes Among Older Patients Receiving Elective Orthopedic Surgery: A Prospective Cohort Study in Taiwan. Rejuvenation Res. 2015, 18, 347–355. [Google Scholar] [CrossRef]
- Mohammadi, M.; Ahmadi, M.; Khalili, H.; Cheraghchi, H.; Arbabi, M. Cyproheptadine for the Prevention of Postoperative Delirium: A Pilot Study. Ann. Pharmacother. 2016, 50, 180–187. [Google Scholar] [CrossRef]
- Jeong, D.M.; Kim, J.A.; Ahn, H.J.; Yang, M.; Heo, B.Y.; Lee, S.H. Decreased Incidence of Postoperative Delirium in Robot-Assisted Thoracoscopic Esophagectomy Compared with Open Transthoracic Esophagectomy. Surg. Laparosc. Endosc. Percutan. Tech. 2016, 26, 516–522. [Google Scholar] [CrossRef]
- Brown, C.H.; LaFlam, A.; Max, L.; Wyrobek, J.; Neufeld, K.J.; Kebaish, K.M.; Cohen, D.B.; Walston, J.D.; Hogue, C.W.; Riley, L.H. Delirium After Spine Surgery in Older Adults: Incidence, Risk Factors, and Outcomes. J. Am. Geriatr. Soc. 2016, 64, 2101–2108. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.Y.; Park, U.J.; Kim, H.T.; Cho, W.H. DELirium Prediction Based on Hospital Information (Delphi) in General Surgery Patients. Medicine 2016, 95, 3072. [Google Scholar] [CrossRef] [PubMed]
- Su, X.; Meng, Z.T.; Wu, X.H.; Cui, F.; Li, H.L.; Wang, D.X.; Zhu, X.; Zhu, S.N.; Maze, M.; Ma, D. Dexmedetomidine for Prevention of Delirium in Elderly Patients after Non-Cardiac Surgery: A Randomised, Double-Blind, Placebo-Controlled Trial. Lancet 2016, 388, 1893–1902. [Google Scholar] [CrossRef]
- Liu, Y.; Ma, L.; Gao, M.; Guo, W.; Ma, Y. Dexmedetomidine Reduces Postoperative Delirium after Joint Replacement in Elderly Patients with Mild Cognitive Impairment. Aging Clin. Exp. Res. 2016, 28, 729–736. [Google Scholar] [CrossRef] [PubMed]
- Winter, A.; Steurer, M.P.; Dullenkopf, A. Postoperative Delirium Assessed by Post Anesthesia Care Unit Staff Utilizing the Nursing Delirium Screening Scale: A Prospective Observational Study of 1000 Patients in a Single Swiss Institution. BMC Anesthesiol. 2015, 15, 184. [Google Scholar] [CrossRef] [PubMed]
- Moerman, S.; Vochteloo, A.J.H.; Tuinebreijer, W.E.; Maier, A.B.; Mathijssen, N.M.C.; Nelissen, R.G.H.H. Factors Associated with the Course of Health-Related Quality of Life after a Hip Fracture. Arch. Orthop. Trauma Surg. 2016, 136, 935–943. [Google Scholar] [CrossRef]
- Stukenberg, S.; Franck, M.; Spies, C.D.; Neuner, B.; Myers, I.; Radtke, F.M. How Can Postoperative Delirium Be Predicted in Advance? A Secondary Analysis Comparing Three Methods of Early Assessment in Elderly Patients. Minerva Anestesiol. 2016, 82, 751–759. [Google Scholar]
- Zhang, Z.Y.; Gao, D.P.; Yang, J.J.; Sun, X.R.; Zhang, H.; Hu, J.; Fang, Z.Y.; Yang, J.J.; Ji, M.H. Impact of Length of Red Blood Cells Transfusion on Postoperative Delirium in Elderly Patients Undergoing Hip Fracture Surgery: A Cohort Study. Injury 2016, 47, 408–412. [Google Scholar] [CrossRef]
- Guo, Y.; Sun, L.; Li, L.; Jia, P.; Zhang, J.; Jiang, H.; Jiang, W. Impact of Multicomponent, Nonpharmacologic Interventions on Perioperative Cortisol and Melatonin Levels and Postoperative Delirium in Elderly Oral Cancer Patients. Arch. Gerontol. Geriatr. 2016, 62, 112–117. [Google Scholar] [CrossRef]
- De Castro, S.M.; Ünlü, Ç.; Tuynman, J.B.; Honig, A.; van Wagensveld, B.A.; Steller, E.P.; Vrouenraets, B.C. Incidence and Risk Factors of Delirium in the Elderly General Surgical Patient. Am. J. Surg. 2014, 208, 26–32. [Google Scholar] [CrossRef]
- Watne, L.O.; Idland, A.V.; Fekkes, D.; Raeder, J.; Frihagen, F.; Ranhoff, A.H.; Chaudhry, F.A.; Engedal, K.; Wyller, T.B.; Hassel, B. Increased CSF Levels of Aromatic Amino Acids in Hip Fracture Patients with Delirium Suggests Higher Monoaminergic Activity. BMC Geriatr. 2016, 16, 149. [Google Scholar] [CrossRef]
- van Grootven, B.; Detroyer, E.; Devriendt, E.; Sermon, A.; Deschodt, M.; Flamaing, J.; Dubois, C.; Milisen, K. Is Preoperative State Anxiety a Risk Factor for Postoperative Delirium among Elderly Hip Fracture Patients? Geriatr. Gerontol. Int. 2016, 16, 948–955. [Google Scholar] [CrossRef]
- Hempenius, L.; Slaets, J.P.J.; van Asselt, D.; de Bock, T.H.; Wiggers, T.; van Leeuwen, B.L. Long Term Outcomes of a Geriatric Liaison Intervention in Frail Elderly Cancer Patients. PLoS ONE 2016, 11, e0143364. [Google Scholar] [CrossRef]
- Franck, M.; Nerlich, K.; Neuner, B.; Schlattmann, P.; Brockhaus, W.R.; Spies, C.D.; Radtke, F.M. No Convincing Association between Post-Operative Delirium and Post-Operative Cognitive Dysfunction: A Secondary Analysis. Acta Anaesthesiol. Scand. 2016, 60, 1404–1414. [Google Scholar] [CrossRef]
- Pinho, C.; Cruz, S.; Santos, A.; Abelha, F.J. Postoperative Delirium: Age and Low Functional Reserve as Independent Risk Factors. J. Clin. Anesth. 2016, 33, 507–513. [Google Scholar] [CrossRef]
- Zheng, Y.B.; Ruan, G.M.; Fu, J.X.; Su, Z.L.; Cheng, P.; Lu, J.Z. Postoperative Plasma 8-Iso-Prostaglandin F2α Levels Are Associated with Delirium and Cognitive Dysfunction in Elderly Patients after Hip Fracture Surgery. Clin. Chim. Acta 2016, 455, 149–153. [Google Scholar] [CrossRef]
- Sun, L.; Jia, P.; Zhang, J.; Zhang, X.; Zhang, Y.; Jiang, H.; Jiang, W.; Guo, Y. Production of Inflammatory Cytokines, Cortisol, and Aβ1-40 in Elderly Oral Cancer Patients with Postoperative Delirium. Neuropsychiatr. Dis. Treat. 2016, 12, 2789–2795. [Google Scholar] [CrossRef]
- Sugano, N.; Aoyama, T.; Sato, T.; Kamiya, M.; Amano, S.; Yamamoto, N.; Nagashima, T.; Ishikawa, Y.; Masudo, K.; Taguri, M.; et al. Randomized Phase II Study of TJ-54 (Yokukansan) for Postoperative Delirium in Gastrointestinal and Lung Malignancy Patients. Mol. Clin. Oncol. 2017, 7, 569–573. [Google Scholar] [CrossRef]
- van der Zanden, V.; Beishuizen, S.J.; Scholtens, R.M.; de Jonghe, A.; de Rooij, S.E.; van Munster, B.C. The Effects of Blood Transfusion on Delirium Incidence. J. Am. Med. Dir. Assoc. 2016, 17, 748–753. [Google Scholar] [CrossRef]
- Tei, M.; Wakasugi, M.; Kishi, K.; Tanemura, M.; Akamatsu, H. Incidence and Risk Factors of Postoperative Delirium in Elderly Patients Who Underwent Laparoscopic Surgery for Colorectal Cancer. Int. J. Colorectal. Dis. 2016, 31, 67–73. [Google Scholar] [CrossRef]
- Chu, C.S.; Liang, C.K.; Chou, M.Y.; Lin, Y.T.; Hsu, C.J.; Chou, P.H.; Chu, C.L. Short-Form Mini Nutritional Assessment as a Useful Method of Predicting the Development of Postoperative Delirium in Elderly Patients Undergoing Orthopedic Surgery. Gen. Hosp. Psychiatry 2016, 38, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Neerland, B.E.; Hall, R.J.; Seljeflot, I.; Frihagen, F.; MacLullich, A.M.J.; Ræder, J.; Wyller, T.B.; Watne, L.O. Associations Between Delirium and Preoperative Cerebrospinal Fluid C-Reactive Protein, Interleukin-6, and Interleukin-6 Receptor in Individuals with Acute Hip Fracture. J. Am. Geriatr. Soc. 2016, 64, 1456–1463. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Jia, P.; Zhang, J.; Wang, X.; Jiang, H.; Jiang, W. Prevalence and Risk Factors of Postoperative Delirium in Elderly Hip Fracture Patients. J. Int. Med. Res. 2016, 44, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Xue, P.; Wu, Z.; Wang, K.; Tu, C.; Wang, X. Incidence and Risk Factors of Postoperative Delirium in Elderly Patients Undergoing Transurethral Resection of Prostate: A Prospective Cohort Study. Neuropsychiatr. Dis. Treat. 2016, 12, 137. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Hatakeyama, S.; Okamoto, T.; Yamamoto, H.; Hosogoe, S.; Tobisawa, Y.; Yoneyama, T.; Hashiba, E.; Yoneyama, T.; Hashimoto, Y.; et al. Slow Gait Speed and Rapid Renal Function Decline Are Risk Factors for Postoperative Delirium after Urological Surgery. PLoS ONE 2016, 11, 0153961. [Google Scholar] [CrossRef]
- El-Gabalawy, R.; Patel, R.; Kilborn, K.; Blaney, C.; Hoban, C.; Ryner, L.; Funk, D.; Legaspi, R.; Fisher, J.A.; Duffin, J.; et al. A Novel Stress-Diathesis Model to Predict Risk of Post-Operative Delirium: Implications for Intra-Operative Management. Front. Aging Neurosci. 2017, 9, 274. [Google Scholar] [CrossRef]
- Mazzola, P.; Ward, L.; Zazzetta, S.; Broggini, V.; Anzuini, A.; Valcarcel, B.; Brathwaite, J.S.; Pasinetti, G.M.; Bellelli, G.; Annoni, G. Association Between Preoperative Malnutrition and Postoperative Delirium After Hip Fracture Surgery in Older Adults. J. Am. Geriatr. Soc. 2017, 65, 1222–1228. [Google Scholar] [CrossRef]
- Petersen, P.B.; Jørgensen, C.C.; Kehlet, H.; Madsen, F.; Hansen, T.B.; Husted, H.; Laursen, M.B.; Hansen, L.T.; Kjærsgaard-Andersen, P.; Solgaard, S. Delirium after Fast-Track Hip and Knee Arthroplasty—A Cohort Study of 6331 Elderly Patients. Acta Anaesthesiol. Scand. 2017, 61, 767–772. [Google Scholar] [CrossRef]
- Xin, X.; Xin, F.; Chen, X.; Zhang, Q.; Li, Y.; Huo, S.; Chang, C.; Wang, Q. Hypertonic Saline for Prevention of Delirium in Geriatric Patients Who Underwent Hip Surgery. J. Neuroinflamm. 2017, 14, 1–9. [Google Scholar] [CrossRef]
- Cunningham, E.L.; Mawhinney, T.; Beverland, D.; O’Brien, S.; Mcauley, D.F.; Cairns, R.; Passmore, P.; McGuinness, B. Observational Cohort Study Examining Apolipoprotein E Status and Preoperative Neuropsychological Performance as Predictors of Post-Operative Delirium in an Older Elective Arthroplasty Population. Age Ageing 2017, 46, 779–786. [Google Scholar] [CrossRef]
- Bhattacharya, B.; Maung, A.; Barre, K.; Maerz, L.; Rodriguez-Davalos, M.I.; Schilsky, M.; Mulligan, D.C.; Davis, K.A. Postoperative Delirium Is Associated with Increased Intensive Care Unit and Hospital Length of Stays after Liver Transplantation. J. Surg. Res. 2017, 207, 223–228. [Google Scholar] [CrossRef]
- Wu, X.M.; Xu, W.C.; Yu, Y.J.; Han, L.; Zhang, J.; Yang, L.J. Postoperative Serum Thioredoxin Concentrations Correlate with Delirium and Cognitive Dysfunction after Hip Fracture Surgery in Elderly Patients. Clin. Chim. Acta 2017, 466, 93–97. [Google Scholar] [CrossRef]
- Beishuizen, S.J.E.; Scholtens, R.M.; van Munster, B.C.; de Rooij, S.E. Unraveling the Relationship between Delirium, Brain Damage, and Subsequent Cognitive Decline in a Cohort of Individuals Undergoing Surgery for Hip Fracture. J. Am. Geriatr. Soc. 2017, 65, 130–136. [Google Scholar] [CrossRef]
- Elsamadicy, A.A.; Adogwa, O.; Lydon, E.; Sergesketter, A.; Kaakati, R.; Mehta, A.I.; Vasquez, R.A.; Cheng, J.; Bagley, C.A.; Karikari, I.O. Depression as an Independent Predictor of Postoperative Delirium in Spine Deformity Patients Undergoing Elective Spine Surgery. J. Neurosurg. Spine 2017, 27, 209–214. [Google Scholar] [CrossRef]
- Xiang, D.; Xing, H.; Tai, H.; Xie, G. Preoperative C-Reactive Protein as a Risk Factor for Postoperative Delirium in Elderly Patients Undergoing Laparoscopic Surgery for Colon Carcinoma. Biomed. Res. Int. 2017, 2017, 5635640. [Google Scholar] [CrossRef]
- Wang, L.; Seok, S.; Kim, S.; Kim, K.; Lee, S.; Lee, K. The Risk Factors of Postoperative Delirium after Total Knee Arthroplasty. J. Knee Surg. 2017, 30, 600–605. [Google Scholar] [CrossRef]
- Mosk, C.A.; van Vugt, J.L.A.; de Jonge, H.; Witjes, C.D.M.; Buettner, S.; Ijzermans, J.N.M.; van der Laan, L. Low Skeletal Muscle Mass as a Risk Factor for Postoperative Delirium in Elderly Patients Undergoing Colorectal Cancer Surgery. Clin. Interv. Aging 2018, 13, 2097. [Google Scholar] [CrossRef]
- Tahir, M.; Malik, S.S.; Ahmed, U.; Kozdryk, J.; Naqvi, S.H.; Malik, A. Risk Factors for Onset of Delirium after Neck of Femur Fracture Surgery: A Prospective Observational Study. SICOT J. 2018, 4, 2018018. [Google Scholar] [CrossRef]
- Susano, M.J.; Scheetz, S.D.; Grasfield, R.H.; Cheung, D.; Xu, X.; Kang, J.D.; Smith, T.R.; Lu, Y.; Groff, M.W.; Chi, J.H.; et al. Retrospective Analysis of Perioperative Variables Associated with Postoperative Delirium and Other Adverse Outcomes in Older Patients After Spine Surgery. J. Neurosurg. Anesthesiol. 2019, 31, 385–391. [Google Scholar] [CrossRef]
- Gutierrez, R.; Egaña, J.I.; Saez, I.; Reyes, F.; Briceño, C.; Venegas, M.; Lavado, I.; Penna, A. Intraoperative Low Alpha Power in the Electroencephalogram Is Associated with Postoperative Subsyndromal Delirium. Front. Syst. Neurosci. 2019, 13, 56. [Google Scholar] [CrossRef]
- Zhao, B.; Ni, Y.; Tian, X. Low Plasma Cholinesterase Activity Is Associated With Postoperative Delirium After Noncardiac Surgery in Elderly Patients: AProspective Observational Study. Psychosomatics 2019, 60, 190–196. [Google Scholar] [CrossRef] [PubMed]
- Tao, L.; Xiaodong, X.; Qiang, M.; Jiao, L.; Xu, Z. Prediction of Postoperative Delirium by Comprehensive Geriatric Assessment among Elderly Patients with Hip Fracture. Ir. J. Med. Sci. 2019, 188, 1311–1315. [Google Scholar] [CrossRef] [PubMed]
- Oe, S.; Togawa, D.; Yamato, Y.; Hasegawa, T.; Yoshida, G.; Kobayashi, S.; Yasuda, T.; Banno, T.; Arima, H.; Mihara, Y.; et al. Preoperative Age and Prognostic Nutritional Index Are Useful Factors for Evaluating Postoperative Delirium Among Patients With Adult Spinal Deformity. Spine 2019, 44, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Wada, S.; Inoguchi, H.; Sadahiro, R.; Matsuoka, Y.J.; Uchitomi, Y.; Sato, T.; Shimada, K.; Yoshimoto, S.; Daiko, H.; Shimizu, K. Preoperative Anxiety as a Predictor of Delirium in Cancer Patients: A Prospective Observational Cohort Study. World J. Surg. 2019, 43, 134–142. [Google Scholar] [CrossRef]
- Peng, J.; Wu, G.; Chen, J.; Chen, H. Preoperative C-Reactive Protein/Albumin Ratio, a Risk Factor for Postoperative Delirium in Elderly Patients After Total Joint Arthroplasty. J. Arthroplasty 2019, 34, 2601–2605. [Google Scholar] [CrossRef]
- Li, Q.H.; Yu, L.; Yu, Z.W.; Fan, X.L.; Yao, W.X.; Ji, C.; Deng, F.; Luo, X.Z.; Sun, J.L. Relation of Postoperative Serum S100A12 Levels to Delirium and Cognitive Dysfunction Occurring after Hip Fracture Surgery in Elderly Patients. Brain Behav. 2019, 9, e01176. [Google Scholar] [CrossRef]
- Wang, Y.; Yu, H.; Qiao, H.; Li, C.; Chen, K.; Shen, X. Risk Factors and Incidence of Postoperative Delirium in Patients Undergoing Laryngectomy. Otolaryngol. Head Neck Surg. 2019, 161, 807–813. [Google Scholar] [CrossRef]
- Roijers, J.P.; Hopmans, C.J.; Janssen, T.L.; Mulder, P.G.H.; Buimer, M.G.; Ho, G.H.; de Groot, H.G.W.; Veen, E.J.; van der Laan, L. The Role of Delirium and Other Risk Factors on Mortality in Elderly Patients with Critical Limb Ischemia Undergoing Major Lower Limb Amputation. Ann. Vasc. Surg. 2019, 60, 270–278.e2. [Google Scholar] [CrossRef]
- Shim, E.J.; Noh, H.L.; Lee, K.M.; Hwang, H.; Son, K.L.; Jung, D.; Kim, W.H.; Kong, S.H.; Suh, Y.S.; Lee, H.J.; et al. Trajectory of Severity of Postoperative Delirium Symptoms and Its Prospective Association with Cognitive Function in Patients with Gastric Cancer: Results from a Prospective Observational Study. Support Care Cancer 2019, 27, 2999–3006. [Google Scholar] [CrossRef]
- de Jong, L.; van Rijckevorsel, V.A.J.I.M.; Raats, J.W.; Klem, T.M.A.L.; Kuijper, T.M.; Roukema, G.R. Delirium after Hip Hemiarthroplasty for Proximal Femoral Fractures in Elderly Patients: Risk Factors and Clinical Outcomes. Clin. Interv. Aging 2019, 14, 427–435. [Google Scholar] [CrossRef]
- Mueller, A.; Spies, C.D.; Eckardt, R.; Weiss, B.; Pohrt, A.; Wernecke, K.D.; Schmidt, M. Anticholinergic Burden of Long-Term Medication Is an Independent Risk Factor for the Development of Postoperative Delirium: A Clinical Trial. J. Clin. Anesth. 2020, 61, 109632. [Google Scholar] [CrossRef]
- Yuan, Y.; Li, Z.; Yang, N.; Han, Y.; Ji, X.; Han, D.; Wang, X.; Li, Y.; Liu, T.; Yuan, F.; et al. Exosome α-Synuclein Release in Plasma May Be Associated with Postoperative Delirium in Hip Fracture Patients. Front. Aging Neurosci. 2020, 12, 67. [Google Scholar] [CrossRef]
- Lu, G.W.; Chou, Y.E.; Jin, W.L.; Su, X.B. Usefulness of Postoperative Serum Translocator Protein as a Predictive Marker for Delirium after Breast Cancer Surgery in Elderly Women. J. Int. Med. Res. 2020, 48, 1–10. [Google Scholar] [CrossRef]
- Wu, J.; Gao, S.; Zhang, S.; Yu, Y.; Liu, S.; Zhang, Z.; Mei, W. Perioperative Risk Factors for Recovery Room Delirium after Elective Non-Cardiovascular Surgery under General Anaesthesia. Perioper. Med. 2021, 10, 1–12. [Google Scholar] [CrossRef]
- Flikweert, E.R.; Izaks, G.J.; Knobben, B.A.S.; Stevens, M.; Wendt, K. The Development of a Comprehensive Multidisciplinary Care Pathway for Patients with a Hip Fracture: Design and Results of a Clinical Trial. BMC Musculoskelet. Disord. 2014, 15, 188. [Google Scholar] [CrossRef]
- Anbar, R.; Beloosesky, Y.; Cohen, J.; Madar, Z.; Weiss, A.; Theilla, M.; Koren Hakim, T.; Frishman, S.; Singer, P. Tight Calorie Control in Geriatric Patients Following Hip Fracture Decreases Complications: A Randomized, Controlled Study. Clin. Nutr. 2014, 33, 23–28. [Google Scholar] [CrossRef]
- Wang, N.Y.; Hirao, A.; Sieber, F. Association between Intraoperative Blood Pressure and Postoperative Delirium in Elderly Hip Fracture Patients. PLoS ONE 2015, 10, e0123892. [Google Scholar] [CrossRef]
- Yang, X.; Li, Z.; Gao, C.; Liu, R. Effect of Dexmedetomidine on Preventing Agitation and Delirium after Microvascular Free Flap Surgery: A Randomized, Double-Blind, Control Study. J. Oral Maxillofac. Surg. 2015, 73, 1065–1072. [Google Scholar] [CrossRef]
- Hempenius, L.; Slaets, J.P.J.; van Asselt, D.Z.B.; Schukking, J.; de Bock, G.H.; Wiggers, T.; van Leeuwen, B.L. Interventions to Prevent Postoperative Delirium in Elderly Cancer Patients Should Be Targeted at Those Undergoing Nonsuperficial Surgery with Special Attention to the Cognitive Impaired Patients. Eur. J. Surg. Oncol. 2015, 41, 28–33. [Google Scholar] [CrossRef]
- Hall, R.J.; Watne, L.O.; Idland, A.V.; Raeder, J.; Frihagen, F.; MacLullich, A.M.J.; Staff, A.C.; Wyller, T.B.; Fekkes, D. Cerebrospinal Fluid Levels of Neopterin Are Elevated in Delirium after Hip Fracture. J. Neuroinflamm. 2016, 13, 1–9. [Google Scholar] [CrossRef]
- Maekawa, Y.; Sugimoto, K.; Yamasaki, M.; Takeya, Y.; Yamamoto, K.; Ohishi, M.; Ogihara, T.; Shintani, A.; Doki, Y.; Mori, M.; et al. Comprehensive Geriatric Assessment Is a Useful Predictive Tool for Postoperative Delirium after Gastrointestinal Surgery in Old-Old Adults. Geriatr. Gerontol. Int. 2016, 16, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, P.; Goodman, S.; Sommer, B.R.; Maloney, W.; Huddleston, J.; Lemmens, H.J. The Effect of Desflurane versus Propofol Anesthesia on Postoperative Delirium in Elderly Obese Patients Undergoing Total Knee Replacement: A Randomized, Controlled, Double-Blinded Clinical Trial. J. Clin. Anesth. 2017, 39, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Pan, Z.; Huang, K.; Huang, W.; Kim, K.H.; Wu, H.; Yu, Y.; Kim, K.N.; Yi, S.; Shin, D.A.; Vora, D.; et al. The Risk Factors Associated with Delirium after Lumbar Spine Surgery in Elderly Patients. Quant. Imaging Med. Surg. 2019, 9, 700. [Google Scholar] [CrossRef] [PubMed]
- Deiner, S.; Luo, X.; Lin, H.M.; Sessler, D.I.; Saager, L.; Sieber, F.E.; Lee, H.B.; Sano, M. Intraoperative Infusion of Dexmedetomidine for Prevention of Postoperative Delirium and Cognitive Dysfunction in Elderly Patients Undergoing Major Elective Noncardiac Surgery: A Randomized Clinical Trial. JAMA Surg. 2017, 152, e171505. [Google Scholar] [CrossRef] [PubMed]
- Ganai, S.; Lee, K.F.; Merrill, A.; Lee, M.H.; Bellantonio, S.; Brennan, M.; Lindenauer, P. Adverse Outcomes of Geriatric Patients Undergoing Abdominal Surgery Who Are at High Risk for Delirium. Arch. Surg. 2007, 142, 1072–1078. [Google Scholar] [CrossRef]
- Lee, J.K.; Park, Y.S. Delirium after Spinal Surgery in Korean Population. Spine 2010, 35, 1729–1732. [Google Scholar] [CrossRef]
- Vasunilashorn, S.M.; Dillon, S.T.; Inouye, S.K.; Ngo, L.H.; Fong, T.G.; Jones, R.N.; Travison, T.G.; Schmitt, E.M.; Alsop, D.C.; Freedman, S.D.; et al. High C-Reactive Protein Predicts Delirium Incidence, Duration, and Feature Severity After Major Noncardiac Surgery. J. Am. Geriatr. Soc. 2017, 65, e109–e116. [Google Scholar] [CrossRef]
- Jin, L.; Yao, R.; Heng, L.; Pang, B.; Sun, F.G.; Shen, Y.; Zhong, J.F.; Zhao, P.P.; Wu, C.Y.; Li, B.P. Ultrasound-Guided Continuous Thoracic Paravertebral Block Alleviates Postoperative Delirium in Elderly Patients Undergoing Esophagectomy: A Randomized Controlled Trial. Medicine 2020, 99, e19896. [Google Scholar] [CrossRef]
- Cerejeira, J.; Batista, P.; Nogueira, V.; Vaz-Serra, A.; Mukaetova-Ladinska, E.B. The Stress Response to Surgery and Postoperative Delirium: Evidence of Hypothalamic-Pituitary-Adrenal Axis Hyperresponsiveness and Decreased Suppression of the GH/IGF-1 Axis. J. Geriatr. Psychiatry Neurol. 2013, 26, 185–194. [Google Scholar] [CrossRef]
- Lee, C.; Lee, C.H.; Lee, G.; Lee, M.; Hwang, J. The Effect of the Timing and Dose of Dexmedetomidine on Postoperative Delirium in Elderly Patients after Laparoscopic Major Non-Cardiac Surgery: A Double Blind Randomized Controlled Study. J. Clin. Anesth. 2018, 47, 27–32. [Google Scholar] [CrossRef]
- Fukata, S.; Kawabata, Y.; Fujisiro, K.; Katagawa, Y.; Kuroiwa, K.; Akiyama, H.; Terabe, Y.; Ando, M.; Kawamura, T.; Hattori, H. Haloperidol Prophylaxis Does Not Prevent Postoperative Delirium in Elderly Patients: A Randomized, Open-Label Prospective Trial. Surg. Today 2014, 44, 2305–2313. [Google Scholar] [CrossRef]
- Monacelli, F.; Signori, A.; Prefumo, M.; Giannotti, C.; Nencioni, A.; Romairone, E.; Scabini, S.; Odetti, P. Delirium, Frailty, and Fast-Track Surgery in Oncogeriatrics: Is There a Link? Dement. Geriatr. Cogn. Disord. Extra 2018, 8, 33–41. [Google Scholar] [CrossRef]
- Youn, Y.C.; Shin, H.W.; Choi, B.S.; Kim, S.Y.; Lee, J.Y.; Ha, Y.C. Rivastigmine Patch Reduces the Incidence of Postoperative Delirium in Older Patients with Cognitive Impairment. Int. J. Geriatr. Psychiatry 2017, 32, 1079–1084. [Google Scholar] [CrossRef]
- Punjasawadwong, Y.; Pipanmekaporn, T.; Wongpakaran, N. Abstract PR164. Anesth. Analg. 2016, 123, 211. [Google Scholar] [CrossRef]
- Xu, W.B.; Hu, Q.H.; Wu, C.N.; Fan, Z.K.; Song, Z.F. Serum Soluble Fibrinogen-like Protein 2 Concentration Predicts Delirium after Acute Pancreatitis. Brain Behav. 2019, 9, e01261. [Google Scholar] [CrossRef]
- Fuchita, M.; Khan, S.H.; Perkins, A.J.; Gao, S.; Wang, S.; Kesler, K.A.; Khan, B.A. Perioperative Risk Factors for Postoperative Delirium in Patients Undergoing Esophagectomy. Ann. Thorac. Surg. 2019, 108, 190–195. [Google Scholar] [CrossRef]
- Culley, D.J.; Flaherty, D.; Fahey, M.C.; Rudolph, J.L.; Javedan, H.; Huang, C.C.; Wright, J.; Bader, A.M.; Hyman, B.T.; Blacker, D.; et al. Poor Performance on a Preoperative Cognitive Screening Test Predicts Postoperative Complications in Older Orthopedic Surgical Patients. Anesthesiology 2017, 127, 765–774. [Google Scholar] [CrossRef]
- Deng, Y.; Wang, R.; Li, S.; Zhu, X.; Wang, T.; Wu, J.; Zhang, J. Methylene Blue Reduces Incidence of Early Postoperative Cognitive Disorders in Elderly Patients Undergoing Major Non-Cardiac Surgery: An Open-Label Randomized Controlled Clinical Trial. J. Clin. Anesth. 2021, 68, 110108. [Google Scholar] [CrossRef]
- Liu, P.; Li, Y.W.; Wang, X.S.; Zou, X.; Zhang, D.Z.; Wang, D.X.; Li, S.Z. High Serum Interleukin-6 Level Is Associated with Increased Risk of Delirium in Elderly Patients after Noncardiac Surgery: A Prospective Cohort Study. Chin. Med. J. 2013, 126, 3621–3627. [Google Scholar] [CrossRef]
- Park, E.A.; Kim, M.Y. Postoperative Delirium Is Associated with Negative Outcomes and Long-Term Mortality in Elderly Koreans: A Retrospective Observational Study. Medicina 2019, 55, 618. [Google Scholar] [CrossRef]
- Rudolph, J.L.; Marcantonio, E.R. Postoperative Delirium: Acute Change with Long-Term Implications. Anesth. Analg. 2011, 112, 1202. [Google Scholar] [CrossRef] [PubMed]
- Onuma, H.; Inose, H.; Yoshii, T.; Hirai, T.; Yuasa, M.; Kawabata, S.; Okawa, A. Preoperative Risk Factors for Delirium in Patients Aged ≥75 Years Undergoing Spinal Surgery: A Retrospective Study. J. Int. Med. Res. 2020, 48, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ballweg, T.; White, M.; Parker, M.; Casey, C.; Bo, A.; Farahbakhsh, Z.; Kayser, A.; Blair, A.; Lindroth, H.; Pearce, R.A.; et al. Association between Plasma Tau and Postoperative Delirium Incidence and Severity: A Prospective Observational Study. Br. J. Anaesth. 2021, 126, 458–466. [Google Scholar] [CrossRef] [PubMed]
- Flink, B.J.; Rivelli, S.K.; Cox, E.A.; White, W.D.; Falcone, G.; Vail, T.P.; Young, C.C.; Bolognesi, M.P.; Krystal, A.D.; Trzepacz, P.T.; et al. Obstructive Sleep Apnea and Incidence of Postoperative Delirium after Elective Knee Replacement in the Nondemented Elderly. Anesthesiology 2012, 116, 788–796. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.M.; Parvizi, J.; Hanssen, A.D.; Gay, P.C. Postoperative Complications in Patients with Obstructive Sleep Apnea Syndrome Undergoing Hip or Knee Replacement: A Case-Control Study. Mayo Clin. Proc. 2001, 76, 897–905. [Google Scholar] [CrossRef]
- Roggenbach, J.; Klamann, M.; von Haken, R.; Bruckner, T.; Karck, M.; Hofer, S. Sleep-Disordered Breathing Is a Risk Factor for Delirium after Cardiac Surgery: A Prospective Cohort Study. Crit. Care 2014, 18, 1–10. [Google Scholar] [CrossRef]
- Kudoh, A.; Katagai, H.; Takazawa, T. Anesthesia with Ketamine, Propofol, and Fentanyl Decreases the Frequency of Postoperative Psychosis Emergence and Confusion in Schizophrenic Patients. J. Clin. Anesth. 2002, 14, 107–110. [Google Scholar] [CrossRef]
- Chaiwat, O.; Chanidnuan, M.; Pancharoen, W.; Vijitmala, K.; Danpornprasert, P.; Toadithep, P.; Thanakiattiwibun, C. Postoperative Delirium in Critically Ill Surgical Patients: Incidence, Risk Factors, and Predictive Scores. BMC Anesthesiol. 2019, 19, 1–10. [Google Scholar] [CrossRef]
- Berggren, D.; Gustafson, Y.; Eriksson, B.; Bucht, G.; Hansson, L.I.; Reiz, S.; Winblad, B. Postoperative Confusion after Anesthesia in Elderly Patients with Femoral Neck Fractures. Anesth. Analg. 1987, 66, 497–504. [Google Scholar] [CrossRef]
- Seo, J.S.; Park, S.W.; Lee, Y.S.; Chung, C.; Kim, Y.B. Risk Factors for Delirium after Spine Surgery in Elderly Patients. J. Korean Neurosurg. Soc. 2014, 56, 28–33. [Google Scholar] [CrossRef]
- Lynch, E.P.; Lazor, M.A.; Gellis, J.E.; Orav, J.; Goldman, L.; Marcantonio, E.R. The Impact of Postoperative Pain on the Development of Postoperative Delirium. Anesth. Analg. 1998, 86, 781–785. [Google Scholar] [CrossRef]
- Zhang, Y.; He, S.T.; Nie, B.; Li, X.Y.; Wang, D.X. Emergence Delirium Is Associated with Increased Postoperative Delirium in Elderly: A Prospective Observational Study. J. Anesth. 2020, 34, 675–687. [Google Scholar] [CrossRef]
- Radtke, F.M.; Franck, M.; MacGuill, M.; Seeling, M.; Lütz, A.; Westhoff, S.; Neumann, U.; Wernecke, K.D.; Spies, C.D. Duration of Fluid Fasting and Choice of Analgesic Are Modifiable Factors for Early Postoperative Delirium. Eur. J. Anaesthesiol. 2010, 27, 411–416. [Google Scholar] [CrossRef]
- Knaak, C.; Brockhaus, W.R.; Spies, C.; Borchers, F.; Piper, S.K.; Radtke, F.M.; Lachmann, G. Presurgical Cognitive Impairment Is Associated with Postoperative Delirium and Postoperative Cognitive Dysfunction. Minerva Anestesiol. 2020, 86, 394–403. [Google Scholar] [CrossRef]
- Contín, A.M.; Perez-Jara, J.; Alonso-Contín, A.; Enguix, A.; Ramos, F. Postoperative Delirium after Elective Orthopedic Surgery. Int. J. Geriatr. Psychiatry 2005, 20, 595–597. [Google Scholar] [CrossRef]
- Shin, Y.H.; Kim, D.K.; Jeong, H.J. Impact of Surgical Approach on Postoperative Delirium in Elderly Patients Undergoing Gastrectomy: Laparoscopic versus Open Approaches. Korean J. Anesthesiol. 2015, 68, 379. [Google Scholar] [CrossRef]
- Tan, C.B.; Ng, J.; Jeganathan, R.; Kawai, F.; Pan, C.X.; Pollock, S.; Turner, J.; Cohen, S.; Chorost, M. Cognitive Changes after Surgery in the Elderly: Does Minimally Invasive Surgery Influence the Incidence of Postoperative Cognitive Changes Compared to Open Colon Surgery? Dement. Geriatr. Cogn. Disord 2015, 39, 125–131. [Google Scholar] [CrossRef]
- Humeidan, M.L.; Reyes, J.P.C.; Mavarez-Martinez, A.; Roeth, C.; Nguyen, C.M.; Sheridan, E.; Zuleta-Alarcon, A.; Otey, A.; Abdel-Rasoul, M.; Bergese, S.D. Effect of Cognitive Prehabilitation on the Incidence of Postoperative Delirium Among Older Adults Undergoing Major Noncardiac Surgery: The Neurobics Randomized Clinical Trial. JAMA Surg. 2021, 156, 1. [Google Scholar] [CrossRef]
- Melegari, G.; Albertini, G.; Romani, A.; Malaguti, S.; Traccitto, F.; Giuliani, E.; Cavallini, G.M.; Bertellini, E.; Barbieri, A. Why Should You Stay One Night? Prospective Observational Study of Enhanced Recovery in Elderly Patients. Aging Clin. Exp. Res. 2021, 33, 1955–1961. [Google Scholar] [CrossRef]
- Windmann, V.; Spies, C.; Knaak, C.; Wollersheim, T.; Piper, S.K.; Vorderwülbecke, G.; Kurpanik, M.; Kuenz, S.; Lachmann, G. Intraoperative Hyperglycemia Increases the Incidence of Postoperative Delirium. Minerva Anestesiol. 2019, 85, 1201–1210. [Google Scholar] [CrossRef]
- Vlisides, P.E.; Das, A.R.; Thompson, A.M.; Kunkler, B.; Zierau, M.; Cantley, M.J.; McKinney, A.M.; Giordani, B. Home-Based Cognitive Prehabilitation in Older Surgical Patients: A Feasibility Study. J. Neurosurg. Anesthesiol. 2019, 31, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Coburn, M.; Sanders, R.D.; Maze, M.; Rossaint, R.; Belda, J.; Borghi, B.; Rosencher, N.; Arnold, G.; Albaladejo, P.; Capdevila, X.; et al. The Hip Fracture Surgery in Elderly Patients (HIPELD) Study: Protocol for a Randomized, Multicenter Controlled Trial Evaluating the Effect of Xenon on Postoperative Delirium in Older Patients Undergoing Hip Fracture Surgery. Trials 2012, 13, 180. [Google Scholar] [CrossRef] [PubMed]
- Morino, T.; Hino, M.; Yamaoka, S.; Misaki, H.; Ogata, T.; Imai, H.; Miura, H. Risk Factors for Delirium after Spine Surgery: An Age-Matched Analysis. Asian. Spine J. 2018, 12, 703. [Google Scholar] [CrossRef] [PubMed]
- Adogwa, O.; Elsamadicy, A.A.; Vuong, V.D.; Fialkoff, J.; Cheng, J.; Karikari, I.O.; Bagley, C.A. Association between Baseline Cognitive Impairment and Postoperative Delirium in Elderly Patients Undergoing Surgery for Adult Spinal Deformity. J. Neurosurg Spine. 2018, 28, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Clemmesen, C.G.; Lunn, T.H.; Kristensen, M.T.; Palm, H.; Foss, N.B. Effect of a Single Pre-Operative 125 Mg Dose of Methylprednisolone on Postoperative Delirium in Hip Fracture Patients; a Randomised, Double-Blind, Placebo-Controlled Trial. Anaesthesia 2018, 73, 1353–1360. [Google Scholar] [CrossRef]
- Sieber, F.; Neufeld, K.J.; Gottschalk, A.; Bigelow, G.E.; Oh, E.S.; Rosenberg, P.B.; Mears, S.C.; Stewart, K.J.; Ouanes, J.P.P.; Jaberi, M.; et al. Depth of Sedation as an Interventional Target to Reduce Postoperative Delirium: Mortality and Functional Outcomes of the Strategy to Reduce the Incidence of Postoperative Delirium in Elderly Patients Randomised Clinical Trial. Brit J. Anaesth. 2019, 122, 480. [Google Scholar] [CrossRef]
- Hassel, B.; Mariussen, E.; Idland, A.V.; Dahl, G.T.; Ræder, J.; Frihagen, F.; Berg, J.P.; Chaudhry, F.A.; Wyller, T.B.; Watne, L.O. CSF Sodium at Toxic Levels Precedes Delirium in Hip Fracture Patients. Neurotoxicology 2018, 69, 11–16. [Google Scholar] [CrossRef]
- Racine, A.M.; Fong, T.G.; Gou, Y.; Travison, T.G.; Tommet, D.; Erickson, K.; Jones, R.N.; Dickerson, B.C.; Metzger, E.; Marcantonio, E.R.; et al. Clinical Outcomes in Older Surgical Patients with Mild Cognitive Impairment. Alzheimers Dement. 2018, 14, 590. [Google Scholar] [CrossRef]
- Mu, D.L.; Zhang, D.Z.; Wang, D.X.; Wang, G.; Li, C.J.; Meng, Z.T.; Li, Y.W.; Liu, C.; Li, X.Y. Parecoxib Supplementation to Morphine Analgesia Decreases Incidence of Delirium in Elderly Patients After Hip or Knee Replacement Surgery: A Randomized Controlled Trial. Anesth. Analg. 2017, 124, 1992–2000. [Google Scholar] [CrossRef]
- Nadler, J.W.; Evans, J.L.; Fang, E.; Preud’Homme, X.A.; Daughtry, R.L.; Chapman, J.B.; Bolognesi, M.P.; Attarian, D.E.; Wellman, S.S.; Krystal, A.D. A Randomised Trial of Peri-Operative Positive Airway Pressure for Postoperative Delirium in Patients at Risk for Obstructive Sleep Apnoea after Regional Anaesthesia with Sedation or General Anaesthesia for Joint Arthroplasty. Anaesthesia 2017, 72, 729–736. [Google Scholar] [CrossRef]
- Westhoff, D.; Witlox, J.; Koenderman, L.; Kalisvaart, K.J.; de Jonghe, J.F.M.; van Stijn, M.F.M.; Houdijk, A.P.J.; Hoogland, I.C.M.; MacLullich, A.M.J.; van Westerloo, D.J.; et al. Preoperative Cerebrospinal Fluid Cytokine Levels and the Risk of Postoperative Delirium in Elderly Hip Fracture Patients. J. Neuroinflamm. 2013, 10, 122. [Google Scholar] [CrossRef]
- Witlox, J.; Slor, C.J.; Jansen, R.W.M.M.; Kalisvaart, K.J.; van Stijn, M.F.M.; Houdijk, A.P.J.; Eikelenboom, P.; van Gool, W.A.; de Jonghe, J.F.M. The Neuropsychological Sequelae of Delirium in Elderly Patients with Hip Fracture Three Months after Hospital Discharge. Int. Psychogeriatr. 2013, 25, 1521–1531. [Google Scholar] [CrossRef]
- Mézière, A.; Paillaud, E.; Belmin, J.; Pariel, S.; Herbaud, S.; Canouï-Poitrine, F.; le Thuaut, A.; Marty, J.; Plaud, B. Delirium in Older People after Proximal Femoral Fracture Repair: Role of a Preoperative Screening Cognitive Test. Ann. Fr. Anesth Reanim. 2013, 32, e91–e96. [Google Scholar] [CrossRef]
- Lundström, M.; Olofsson, B.; Stenvall, M.; Karlsson, S.; Nyberg, L.; Englund, U.; Borssén, B.; Svensson, O.; Gustafson, Y. Postoperative Delirium in Old Patients with Femoral Neck Fracture: A Randomized Intervention Study. Aging Clin. Exp. Res. 2007, 19, 178–186. [Google Scholar] [CrossRef]
- Leung, J.M.; Sands, L.P.; Rico, M.; Petersen, K.L.; Rowbotham, M.C.; Dahl, J.B.; Ames, C.; Chou, D.; Weinstein, P. Pilot Clinical Trial of Gabapentin to Decrease Postoperative Delirium in Older Patients. Neurology 2006, 67, 1251–1253. [Google Scholar] [CrossRef]
- Kalisvaart, K.J.; de Jonghe, J.F.M.; Bogaards, M.J.; Vreeswijk, R.; Egberts, T.C.G.; Burger, B.J.; Eikelenboom, P.; van Gool, W.A. Haloperidol Prophylaxis for Elderly Hip-Surgery Patients at Risk for Delirium: A Randomized Placebo-Controlled Study. J. Am. Geriatr. Soc. 2005, 53, 1658–1666. [Google Scholar] [CrossRef]
- Kudoh, A.; Katagai, H.; Takase, H.; Takazawa, T. Effect of Preoperative Discontinuation of Antipsychotics in Schizophrenic Patients on Outcome during and after Anaesthesia. Eur. J. Anaesth. 2004, 21, 414–416. [Google Scholar] [CrossRef]
- Kudoh, A.; Takase, H.; Takazawa, T. A Comparison of Anesthetic Quality in Propofol-Spinal Anesthesia and Propofol-Fentanyl Anesthesia for Total Knee Arthroplasty in Elderly Patients. J. Clin. Anesth. 2004, 16, 405–410. [Google Scholar] [CrossRef]
- Kudoh, A.; Katagai, H.; Takazawa, T. Antidepressant Treatment for Chronic Depressed Patients Should Not Be Discontinued Prior to Anesthesia. Can. J. Anaesth. 2002, 49, 132–136. [Google Scholar] [CrossRef]
- Aizawa, K.I.; Kanai, T.; Saikawa, Y.; Takabayashi, T.; Kawano, Y.; Miyazawa, N.; Yamamoto, T. A Novel Approach to the Prevention of Postoperative Delirium in the Elderly after Gastrointestinal Surgery. Surg. Today 2002, 32, 310–314. [Google Scholar] [CrossRef]
- Marcantonio, E.R.; Flacker, J.M.; John Wright, R.; Resnick, N.M. Reducing Delirium after Hip Fracture: A Randomized Trial. J. Am. Geriatr. Soc. 2001, 49, 516–522. [Google Scholar] [CrossRef] [PubMed]
- Milisen, K.; Foreman, M.D.; Abraham, I.L.; de Geest, S.; Godderis, J.; Vandermeulen, E.; Fischler, B.; Delooz, H.H.; Spiessens, B.; Broos, P.L.O. A Nurse-Led Interdisciplinary Intervention Program for Delirium in Elderly Hip-Fracture Patients. J. Am. Geriatr. Soc. 2001, 49, 523–532. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, T.; Cai, J.; Ishikura, T.; Kobayashi, M.; Naka, T.; Kaibara, N. Prophylactic Consecutive Administration of Haloperidol Can Reduce the Occurrence of Postoperative Delirium in Gastrointestinal Surgery. Yonago Acta. Med. 1999, 42, 179–184. [Google Scholar]
- Dimartini, A.F.; Trzepacz, P.T.; Pajer, K.A.; Faett, D.; Fung, J. Neuropsychiatric Side Effects of FK506 vs. Cyclosporine A: First-Week Postoperative Findings. Psychosomatics 1997, 38, 565–569. [Google Scholar] [CrossRef]
- Oh, E.S.; Leoutsakos, J.M.; Rosenberg, P.B.; Pletnikova, A.M.; Khanuja, H.S.; Sterling, R.S.; Oni, J.K.; Sieber, F.E.; Fedarko, N.S.; Akhlaghi, N.; et al. Effects of Ramelteon on the Prevention of Postoperative Delirium in Older Patients Undergoing Orthopedic Surgery: The RECOVER Randomized Controlled Trial. Am. J. Geriatr. Psychiatry 2021, 29, 90–100. [Google Scholar] [CrossRef]
- Oh, T.K.; Park, H.Y.; Shin, H.J.; Jeon, Y.T.; Do, S.H.; Hwang, J.W. The Role of Perioperative Statin Use in the Prevention of Delirium After Total Knee Replacement Under Spinal Anesthesia. J. Arthroplast. 2018, 33, 3666–3671. [Google Scholar] [CrossRef]
- Kin, K.; Yasuhara, T.; Tomita, Y.; Umakoshi, M.; Morimoto, J.; Date, I. SF-36 Scores Predict Postoperative Delirium after Surgery for Cervical Spondylotic Myelopathy. J. Neurosurg. Spine. 2019, 30, 777–782. [Google Scholar] [CrossRef]
- Chevillon, C.; Hellyar, M.; Madani, C.; Kerr, K.; Kim, S.C. Preoperative Education on Postoperative Delirium, Anxiety, and Knowledge in Pulmonary Thromboendarterectomy Patients. Am. J. Crit. Care 2015, 24, 164–171. [Google Scholar] [CrossRef]
- Hempenius, L.; Slaets, J.P.J.; van Asselt, D.; de Bock, G.H.; Wiggers, T.; van Leeuwen, B.L. Outcomes of a Geriatric Liaison Intervention to Prevent the Development of Postoperative Delirium in Frail Elderly Cancer Patients: Report on a Multicentre, Randomized, Controlled Trial. PLoS ONE 2013, 8, e64834. [Google Scholar] [CrossRef]
- Cerejeira, J.M.S.; Nogueira, V.; Luís, P.; Vaz-Serra, A.; Mukaetova-Ladinska, E.B. The Cholinergic System and Inflammation: Common Pathways in Delirium Pathophysiology. J. Am. Geriatr. Soc. 2012, 60, 669–675. [Google Scholar] [CrossRef]
- Lee, H.; Ju, J.W.; Oh, S.Y.; Kim, J.; Jung, C.W.; Ryu, H.G. Impact of Timing and Duration of Postoperative Delirium: A Retrospective Observational Study. Surgery 2018, 164, 137–143. [Google Scholar] [CrossRef]
- Lee, H.; Yang, S.M.; Chung, J.; Oh, H.W.; Yi, N.J.; Suh, K.S.; Oh, S.Y.; Ryu, H.G. Effect of Perioperative Low-Dose Dexmedetomidine on Postoperative Delirium After Living-Donor Liver Transplantation: A Randomized Controlled Trial. Transplant. Proc. 2020, 52, 239–245. [Google Scholar] [CrossRef]
- Mevorach, L.; Forookhi, A.; Farcomeni, A.; Romagnoli, S.; Bilotta, F. Perioperative Risk Factors Associated with Increased Incidence of Postoperative Delirium: Systematic Review, Meta-Analysis, and Grading of Recommendations Assessment, Development, and Evaluation System Report of Clinical Literature. Br. J. Anaesth. 2022, 130, e254–e262. [Google Scholar] [CrossRef]

| Risk Factor | ||
|---|---|---|
| Demographics | ||
| Age | ≥60 | |
| Gender * | Female | |
| Education | <8 years | |
| Laboratory # | ||
| Albumin | <3.9 g/dL | |
| CRP | >7 mg/L | |
| Hemoglobin | >13.16 g/dL | |
| Glucose | >8.4 mmol/L | |
| TNF-a | >8.2 nmol/L | |
| IL-6 | >17.9 pg/mL | |
| Cumulative scores | ||
| MMSE | <17 | |
| CCI | ≥2 | |
| Mini–Cog | ≤2 | |
| Comorbidities | ||
| Diabetes | Yes | |
| Stroke | Yes | |
| Chronic therapies | ||
| Benzodiazepines | Yes | |
| Habits | ||
| Alcohol abuse | Yes | |
| Surgery | ||
| Emergency | Yes | |
| Intrathoracic, intrabdominal, Orthopedic, spinal, peripheral vascular | Yes | |
| Minimally invasive * | Yes | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karageorgos, V.; Mevorach, L.; Silvetti, M.; Bilotta, F. Preoperative Risk Factors Associated with Increased Incidence of Postoperative Delirium: Systematic Review of Qualified Clinical Studies. Geriatrics 2023, 8, 24. https://doi.org/10.3390/geriatrics8010024
Karageorgos V, Mevorach L, Silvetti M, Bilotta F. Preoperative Risk Factors Associated with Increased Incidence of Postoperative Delirium: Systematic Review of Qualified Clinical Studies. Geriatrics. 2023; 8(1):24. https://doi.org/10.3390/geriatrics8010024
Chicago/Turabian StyleKarageorgos, Vlasios, Lior Mevorach, Melissa Silvetti, and Federico Bilotta. 2023. "Preoperative Risk Factors Associated with Increased Incidence of Postoperative Delirium: Systematic Review of Qualified Clinical Studies" Geriatrics 8, no. 1: 24. https://doi.org/10.3390/geriatrics8010024
APA StyleKarageorgos, V., Mevorach, L., Silvetti, M., & Bilotta, F. (2023). Preoperative Risk Factors Associated with Increased Incidence of Postoperative Delirium: Systematic Review of Qualified Clinical Studies. Geriatrics, 8(1), 24. https://doi.org/10.3390/geriatrics8010024







