Innovative Non-Pharmacological Management of Delirium in Persons with Dementia: New Frontiers for Physiotherapy and Occupational Therapy?
Abstract
1. Introduction
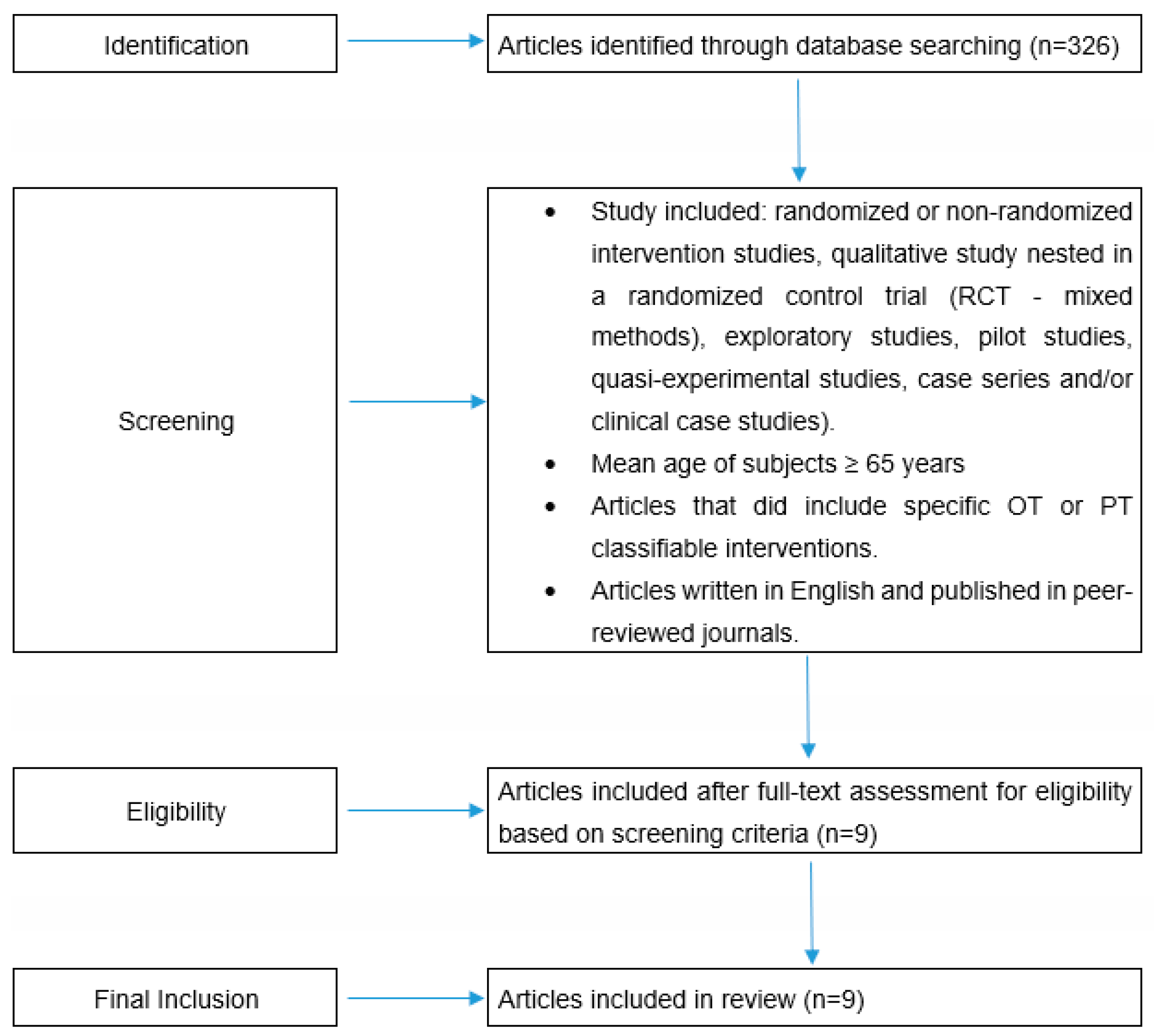
2. Materials and Methods
3. Results
3.1. Main Characteristics of the Selected Studies
3.2. Tools to Assess Delirium, Dementia or DSD and Assess Functional Status, Quality of Life of Patients and Caregivers
3.3. Rehabilitation Interventions and Results
- -
- Person-tailored exercises at a moderate intensity can improve motor performance, autonomy, cognitive functions and quality of life, but not delirium incidence [10].
- -
- Early mobilization can reduce 30-day readmission, falls, pressure sores and respiratory adverse events in ICU patients. Moreover, these interventions can improve independence in activity of daily living but cannot shorten the length of stay [12].
- -
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Overview | Delirium: Prevention, Diagnosis and Management | Guidance | NICE. Available online: https://www.nice.org.uk/guidance/cg103 (accessed on 10 October 2022).
- Duong, S.; Patel, T.; Chang, F. Dementia. Can. Pharm. J. CPJ 2017, 150, 118–129. [Google Scholar] [CrossRef]
- Ford, A.H.; Almeida, O.P. Almeida, Pharmacological interventions for preventing delirium in the elderly. Maturitas 2015, 81, 287–292. [Google Scholar] [CrossRef]
- Connelly, P.J.; James, R. SIGN guideline for the management of patients with dementia. Int. J. Geriatr. Psychiatry 2005, 21, 14–16. [Google Scholar] [CrossRef]
- Chalfont, G.; Milligan, C.; Simpson, J. A mixed methods systematic review of multimodal non-pharmacological interventions to improve cognition for people with dementia. Dementia 2020, 19, 1086–1130. [Google Scholar] [CrossRef]
- Cuevas-Lara, C.; Izquierdo, M.; Gutiérrez-Valencia, M.; Marín-Epelde, I.; Zambom-Ferraresi, F.; Contreras-Escámez, B.; Martínez-Velilla, N. Effectiveness of occupational therapy interventions in acute geriatric wards: A systematic review. Maturitas 2019, 127, 43–50. [Google Scholar] [CrossRef]
- Morandi, A.; Pozzi, C.; Milisen, K.; Hobbelen, H.; Bottomley, J.M.; Lanzoni, A.; Tatzer, V.C.; Carpena, M.G.; Cherubini, A.; Ranhoff, A.; et al. An interdisciplinary statement of scientific societies for the advancement of delirium care across Europe (EDA, EANS, EUGMS, COTEC, IPTOP/WCPT). BMC Geriatr. 2019, 19, 253. [Google Scholar] [CrossRef]
- Killington, M.; Walker, R.; Crotty, M. The chaotic journey: Recovering from hip fracture in a nursing home. Arch. Gerontol. Geriatr. 2016, 67, 106–112. [Google Scholar] [CrossRef]
- Martínez-Velilla, N.; Casas-Herrero, A.; Zambom-Ferraresi, F.; De Asteasu, M.L.S.; Lucia, A.; Galbete, A.; García-Baztán, A.; Alonso-Renedo, J.; González-Glaría, B.; Gonzalo-Lázaro, M.; et al. Effect of Exercise Intervention on Functional Decline in Very Elderly Patients During Acute Hospitalization: A Randomized Clinical Trial. JAMA Intern. Med. 2019, 179, 28–36. [Google Scholar] [CrossRef]
- Said, C.M.; Delahunt, M.; Hardidge, A.; Smith, P.; Tran, P.; McDonald, L.; Kefalianos, E.; Daniel, C.; Berney, S. Recumbent cycling to improve outcomes in people with hip fracture: A feasibility randomized trial. BMC Geriatr. 2021, 21, 394. [Google Scholar] [CrossRef]
- Fraser, D.; Spiva, L.; Forman, W.; Hallen, C. Original Research: Implementation of an Early Mobility Program in an ICU. Am. J. Nurs. 2015, 115, 49–58. [Google Scholar] [CrossRef]
- Álvarez, E.A.; Garrido, M.A.; Tobar, E.A.; Prieto, S.A.; Vergara, S.O.; Briceño, C.D.; González, F.J. Occupational therapy for delirium management in elderly patients without mechanical ventilation in an intensive care unit: A pilot randomized clinical trial. J. Crit. Care 2017, 37, 85–90. [Google Scholar] [CrossRef]
- Goonan, R.; Nicks, R.; Jolliffe, L.; Pritchard, E. Implementation of a Person-Centred Activity Program on a Sub-Acute Inpatient Dementia Ward. Phys. Occup. Ther. Geriatr. 2019, 37, 171–182. [Google Scholar] [CrossRef]
- Pozzi, C.; Lucchi, E.; Lanzoni, A.; Gentile, S.; Trabucchi, M.; Bellelli, G.; Morandi, A. Preliminary Evidence of a Positive Effect of Occupational Therapy in Patients with Delirium Superimposed on Dementia. J. Am. Med. Dir. Assoc. 2017, 18, 1091–1092. [Google Scholar] [CrossRef]
- Pozzi, C.; Lanzoni, A.; Lucchi, E.; Salimbeni, I.; DeVreese, L.P.; Bellelli, G.; Fabbo, A.; Morandi, A. Activity-based occupational therapy intervention for delirium superimposed on dementia in nursing home setting: A feasibility study. Aging Clin. Exp. Res. 2019, 32, 827–833. [Google Scholar] [CrossRef]
- Bolton, L.; Loveard, T. Te Kete Marie—The peaceful basket: An initiative for supporting people with dementia or delirium. Int. J. Palliat. Nurs. 2016, 22, 130–136. [Google Scholar] [CrossRef]
- Wei, L.A.; Fearing, M.A.; Sternberg, E.J.; Inouye, S.K. The Confusion Assessment Method: A Systematic Review of Current Usage. J. Am. Geriatr. Soc. 2008, 56, 823–830. [Google Scholar] [CrossRef]
- Marcantonio, E.R.; Ngo, L.H.; O’Connor, M.; Jones, R.; Crane, P.K.; Metzger, E.D.; Inouye, S.K. 3D-CAM: Derivation and Validation of a 3-Minute Diagnostic Interview for CAM-defined Delirium. Ann. Intern. Med. 2014, 161, 554–561. [Google Scholar] [CrossRef]
- Ely, E.W.; Margolin, R.; Francis, J.; May, L.; Truman, B.; Dittus, R.; Speroff, T.; Gautam, S.; Bernard, G.R.; Inouye, S.K. Evaluation of delirium in critically ill patients: Validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit. Care Med. 2001, 29, 1370–1379. [Google Scholar] [CrossRef]
- Sessler, C.N.; Gosnell, M.S.; Grap, M.J.; Brophy, G.M.; O’Neal, P.V.; Keane, K.A.; Tesoro, E.P.; Elswick, R.K. The Richmond Agitation–Sedation Scale. Am. J. Respir. Crit. Care Med. 2002, 166, 1338–1344. [Google Scholar] [CrossRef]
- Chester, J.G.; Harrington, M.B.; Rudolph, J.L.; on behalf of the VA Delirium Working Group. Serial administration of a modified Richmond Agitation and Sedation Scale for delirium screening. J. Hosp. Med. 2012, 7, 450–453. [Google Scholar] [CrossRef]
- Voyer, P.; Champoux, N.; Desrosiers, J.; Landreville, P.; McCusker, J.; Monette, J.; Savoie, M.; Richard, S.; Carmichael, P.-H. Recognizing acute delirium as part of your routine [RADAR]: A validation study. BMC Nurs. 2015, 14, 19. [Google Scholar] [CrossRef]
- de Jonghe, J.F.M.; Kalisvaart, K.J.; Timmers, J.F.M.; Kat, M.G.; Jackson, J.C. Delirium-O-Meter: A nurses’ rating scale for monitoring delirium severity in geriatric patients. Int. J. Geriatr. Psychiatry 2005, 20, 1158–1166. [Google Scholar] [CrossRef]
- Trzepacz, P.T.; Mittal, D.; Torres, R.; Kanary, K.; Norton, J.; Jimerson, N. Validation of the Delirium Rating Scale-revised-98: Comparison with the delirium rating scale and the cognitive test for delirium. J. Neuropsychiatry Clin. Neurosci. 2001, 13, 229–242. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Morris, J.C. Clinical Dementia Rating: A Reliable and Valid Diagnostic and Staging Measure for Dementia of the Alzheimer Type. Int. Psychogeriatr. 1997, 9, 173–176. [Google Scholar] [CrossRef]
- Freitas, S.; Simões, M.R.; Marôco, J.; Alves, L.; Santana, I. Construct Validity of the Montreal Cognitive Assessment (MoCA). J. Int. Neuropsychol. Soc. JINS 2012, 18, 242–250. [Google Scholar] [CrossRef]
- Jorm, A.F. A short form of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): Development and cross-validation. Psychol. Med. 1994, 24, 145–153. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61−65. [Google Scholar]
- Tinetti, M.E.; Richman, D.; Powell, L. Powell, Falls Efficacy as a Measure of Fear of Falling. J. Gerontol. 1990, 45, P239–P243. [Google Scholar] [CrossRef]
- Gómez, J.F.; Curcio, C.-L.; Alvarado, B.; Zunzunegui, M.V.; Guralnik, J. Validity and reliability of the Short Physical Performance Battery (SPPB). Colomb. Médica CM 2013, 44, 165–171. [Google Scholar]
- Kimmel, L.A.; Elliott, J.E.; Sayer, J.M.; Holland, A.E. Assessing the Reliability and Validity of a Physical Therapy Functional Measurement Tool—The Modified Iowa Level of Assistance Scale—In Acute Hospital Inpatients. Phys. Ther. 2016, 96, 176–182. [Google Scholar] [CrossRef]
- Kidd, D.; Stewart, G.; Baldry, J.; Johnson, J.; Rossiter, D.; Petruckevitch, A.; Thompson, A.J. The Functional Independence Measure: A comparative validity and reliability study. Disabil. Rehabil. 1995, 17, 10–14. [Google Scholar] [CrossRef]
- Nancarrow, S.A.; Booth, A.; Ariss, S.; Smith, T.; Enderby, P.; Roots, A. Ten principles of good interdisciplinary team work. Hum. Resour. Health 2013, 11, 19. [Google Scholar] [CrossRef]
- Rawlinson, C.; Carron, T.; Cohidon, C.; Arditi, C.; Hong, Q.N.; Pluye, P.; Peytremann-Bridevaux, I.; Gilles, I. An Overview of Reviews on Interprofessional Collaboration in Primary Care: Effectiveness. Int. J. Integr. Care 2021, 21, 31. [Google Scholar] [CrossRef]
- Moore, A.; Patterson, C.; White, J.; House, S.T.; Riva, J.J.; Nair, K.; Brown, A.; Kadhim-Saleh, A.; McCann, D. Interprofessional and integrated care of the elderly in a family health team. Can. Fam. Physician 2012, 58, e436–e441. [Google Scholar]
- Oh-Park, M.; Chen, P.; Romel-Nichols, V.; Hreha, K.; Boukrina, O.; Barrett, A. Delirium screening and management in inpatient rehabilitation facilities. Am. J. Phys. Med. Rehabil. 2018, 97, 754–762. [Google Scholar] [CrossRef]
- Gitlin, L.N.; Winter, L.; Earland, M.T.V.; Herge, M.E.A.; Chernett, M.N.L.; Piersol, C.; Burke, J.P. The Tailored Activity Program to Reduce Behavioral Symptoms in Individuals with Dementia: Feasibility, Acceptability, and Replication Potential. Gerontol. 2009, 49, 428–439. [Google Scholar] [CrossRef]
- Grey, T.; Fleming, R.; Goodenough, B.J.; Xidous, D.; Möhler, R.; O’Neill, D. Hospital design for older people with cognitive impairment including dementia and delirium: Supporting inpatients and accompanying persons. Cochrane Database Syst. Rev. 2019, 2019, CD013482. [Google Scholar] [CrossRef]
- Xidous, D.; Grey, T.; Kennelly, S.P.; McHale, C.; O’Neill, D. Dementia Friendly Hospital Design: Key Issues for Patients and Accompanying Persons in an Irish Acute Care Public Hospital. HERD 2020, 13, 48–67. [Google Scholar] [CrossRef]
- Emartins, S.; Efernandes, L. Delirium in Elderly People: A Review. Front. Neurol. 2012, 3, 101. Available online: https://www.frontiersin.org/article/10.3389/fneur.2012.00101 (accessed on 14 November 2022).
- Covinsky, K. Hospital-Acquired Disability: An Overview. Innov. Aging 2017, 1 (Suppl. S1), 963. [Google Scholar] [CrossRef]
- Graff, M.J.L.; Vernooij-Dassen, M.J.M.; Thijssen, M.; Dekker, J.; Hoefnagels, W.H.L.; Rikkert, M.G.M.O. Rikkert, Community based occupational therapy for patients with dementia and their care givers: Randomised controlled trial. BMJ 2006, 333, 1196. [Google Scholar] [CrossRef]
- Pozzi, C.; Lanzoni, A.; Lucchi, E.; Bergamini, L.; Bevilacqua, P.; Manni, B.; Garzetta, G.; Barbieri, S.; Khazri, S.; Chattat, R.; et al. A pilot study of community-based occupational therapy for persons with dementia (COTID-IT Program) and their caregivers: Evidence for applicability in Italy. Aging Clin. Exp. Res. 2018, 31, 1299–1304. [Google Scholar] [CrossRef]
- Cohen, C.; Pereira, F.; Kampel, T.; Bélanger, L. Integration of family caregivers in delirium prevention care for hospitalized older adults: A case study analysis. J. Adv. Nurs. 2021, 77, 318–330. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Bennett, S.; Laver, K.; Voigt-Radloff, S.; Letts, L.; Clemson, L.; Graff, M.; Wiseman, J.; Gitlin, L. Occupational therapy for people with dementia and their family carers provided at home: A systematic review and meta-analysis. BMJ Open 2019, 9, e026308. [Google Scholar] [CrossRef]
- Mosk, C.A.; Mus, M.; Vroemen, J.P.; van der Ploeg, T.; Vos, D.I.; Elmans, L.H.; van der Laan, L. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin. Interv. Aging 2017, 12, 421–430. [Google Scholar] [CrossRef]
| Author Year | Study Design | Setting | N | Mean Population Age | Diagnosis on Admission/Characteristics of the Cohort | Tools to Assess Delirium | Tools to Assess Dementia | Tools to Assess Functional Status | Tools to Assess Quality of Life for Patients and Caregiver | Rehabilitation Intervention | Results |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Killington 2016 [9] | Qualitative study nested in a RCT | orthogeriatrics ward | 28 | 87.5 | Hip fractures | Not reported | MMSE | Not reported | Qualitative interview for caregivers and staff | - Mobilization - Activities of daily living | - Improvement of functional outcomes |
| Martinez-Velilla 2019 [10] | RCT | ACE Unit | 370 | 87.1 | Vulnerable population with a high level of functional reserve | CAM | MMSE | BI, SPPB handgrip strength | GDS EuroQoL 5D | - Balance and walking exercises at moderate intensity (twice daily) with PT - Resistance (2–3 sets of 8–10 exercises—30–60% load maximum equivalent) - Squats (standing up from a chair), leg press; bilateral knee extension - Active involvement of the caregiver - Patient education | - Improvement on SPPB (<0.001), Barthel Index (<0.001), MMSE (<0.001), GDS (<0.001), EuroQoL–5D (<0.001) and handgrip strength (<0.001) in experimental vs. usual-care group - Higher incidence of delirium in the experimental than usual care group (14.6% vs. 8.3%) |
| Said 2021 [11] | Single-blinded randomized controlled pilot trial | orthogeriatrics ward | 51 | 83.5 | Hip fractures | 3D CAM SHORT CAM | MOCA IQCODE short form | Modified ILAS Gait Speed (m/s) | EuroQoL 5D EuroQoL-VAS | - Mobilization recumbent cycling in bed | - No functional improvement |
| Fraser 2015 [12] | Retrospective longitudinal study | Intensive Care Unit | 132 | 64.7 | Respiratory or gastrointestinal or cardiac or sepsis or neurologic problems | RASS CAM-ICU | Not reported | BI | Not reported | - Checking the correct positioning in bed every two hours - Generic exercises: sitting on the bed’s edge, standing, transferring to chair and walking | - Reduced rate of ICU readmission after 30 days (<0.001) - Reduced falls, sore pressures, adverse respiratory events (<0.001) - Barthel Index improvement (<0.001) - No reduction in days spent in ICU |
| Alvarez 2017 [13] | RCT | Intensive Care Unit | 160 | 86.0 | Sepsis; renal or hepatic failure; hemorraghe, acute respiratory syndrom, cardiac failure | CAM-ICU Delirium rating scale | MMSE | FIM Hand grip strength | Not reported | - Sensorial stimulation (i.e., lights, tactile body stimulation) - Mobilization - Cognitive stimulation - Passive and active exercises of the upper limbs - Family participation (twice a day) | - Decrease of delirium duration and functional improvement (FIM and handgrip strength) |
| Gonaan 2017 [14] | Prospective observational study | Dementia ward Hospital | 30 | 80.3 | Dementia or/and delirium | Not reported | MMSE | BI | Not reported | - Person-centered care (occupational story, tailored and meaningful activities) - Caregiver’s participation in the rehabilitation session - Staff education | - Decrease of behavioral disorders |
| Pozzi 2017 [15] | Case series | Rehabilitation Hospital | 6 | 84.1 | DSD | RASS | MMSE | BI Tinetti Scale | Not reported | - OT intervention (twice a day, 5 days, 40 min per day). - Sensorial and cognitive stimulation, meaningful occupations - Family education and involvement in the rehabilitation sessions - Environmental changes to promote rest, sleep-wake cycle improvement and reorientation | - Functional improvement - High rate (83%) of discharge to home |
| Pozzi 2020 [16] | Feasibility Study | Nursing home | 22 | 86.4 | DSD | m-RASS RADAR Delirium-O-Meter | MMSE CDR | BI Tinetti Scale | COPM (proxy) | - Caregiver education and involvement in the rehabilitation sessions - Multisensorial and cognitive stimulation with meaningful and tailored activities - Environmental changes to promote activities and rest | - Functional and occupational improvement from delirium diagnosis to resolution |
| Bolton & Loveard 2016 [17] | Case series | Hospice | 88 | Not reported | Dementia and/or delirium | Not reported | MOCA | Not reported | Qualitative interview for staff | - Meaningful and tailored activities - Environmental changes to improve orientation - Staff training to improve competence in the use of nonpharmacological strategies. - Caregiver education and involvement in the sessions | - OT was feasible in all patients - Patients’ agitation decrease |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pozzi, C.; Tatzer, V.C.; Strasser-Gugerell, C.; Cavalli, S.; Morandi, A.; Bellelli, G. Innovative Non-Pharmacological Management of Delirium in Persons with Dementia: New Frontiers for Physiotherapy and Occupational Therapy? Geriatrics 2023, 8, 28. https://doi.org/10.3390/geriatrics8020028
Pozzi C, Tatzer VC, Strasser-Gugerell C, Cavalli S, Morandi A, Bellelli G. Innovative Non-Pharmacological Management of Delirium in Persons with Dementia: New Frontiers for Physiotherapy and Occupational Therapy? Geriatrics. 2023; 8(2):28. https://doi.org/10.3390/geriatrics8020028
Chicago/Turabian StylePozzi, Christian, Verena C. Tatzer, Cornelia Strasser-Gugerell, Stefano Cavalli, Alessandro Morandi, and Giuseppe Bellelli. 2023. "Innovative Non-Pharmacological Management of Delirium in Persons with Dementia: New Frontiers for Physiotherapy and Occupational Therapy?" Geriatrics 8, no. 2: 28. https://doi.org/10.3390/geriatrics8020028
APA StylePozzi, C., Tatzer, V. C., Strasser-Gugerell, C., Cavalli, S., Morandi, A., & Bellelli, G. (2023). Innovative Non-Pharmacological Management of Delirium in Persons with Dementia: New Frontiers for Physiotherapy and Occupational Therapy? Geriatrics, 8(2), 28. https://doi.org/10.3390/geriatrics8020028







