Prevalence, Risk Factors and Outcomes Associated with Physical Restraint in Acute Medical Inpatients over 4 Years—A Retrospective Cohort Study
Abstract
:1. Introduction
2. Methods
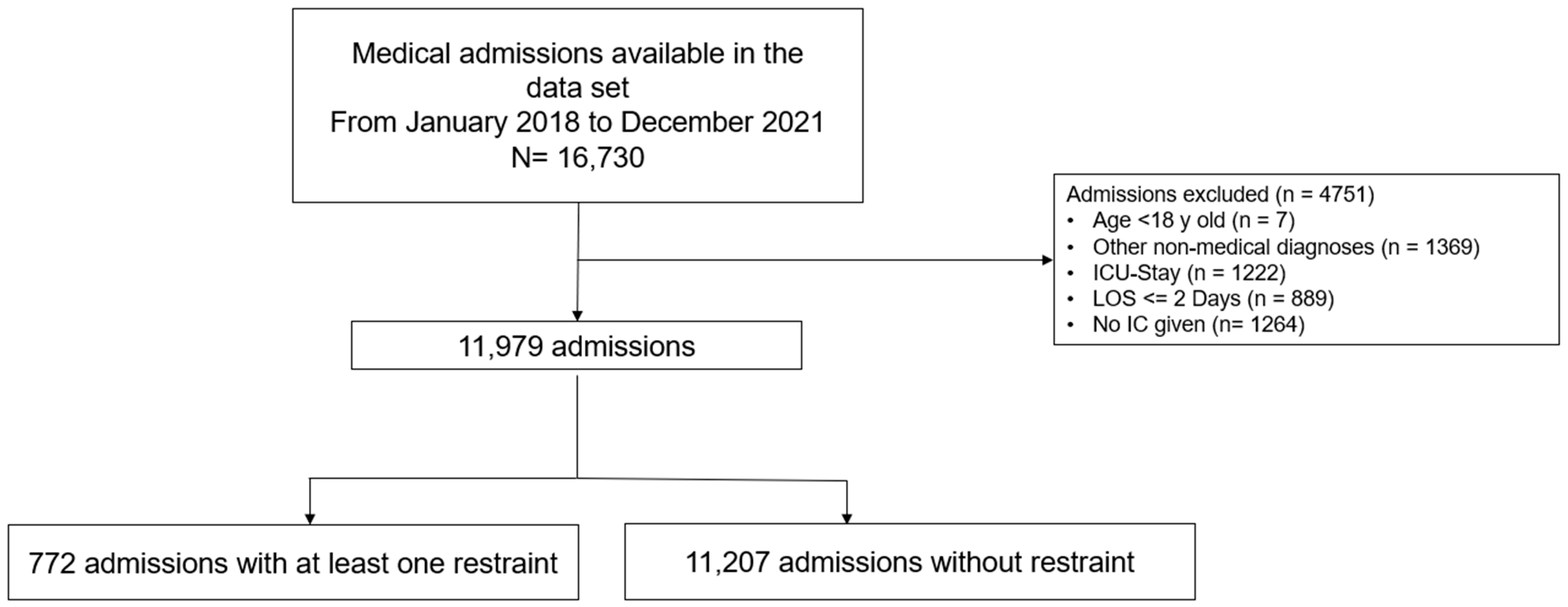
2.1. Inclusion and Exclusion Criteria
2.2. Outcomes
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Patient Cohort
3.2. Association of Physical Restraints and Outcome
3.3. Indication for the Use of Restraint and Medical Therapy
3.4. Trends over Time
4. Discussion
4.1. LOS and Nurses’ Time Expenditure
4.2. Comparing Fall and Type of Restraints
4.3. Differences between Wards of the Same Clinic
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bleijlevens, M.H.; Wagner, L.M.; Capezuti, E.; Hamers, J.P. International Physical Restraint W: Physical Restraints: Consensus of a Research Definition Using a Modified Delphi Technique. J. Am. Geriatr. Soc. 2016, 64, 2307–2310. [Google Scholar] [CrossRef] [PubMed]
- Gastmans, C.; Milisen, K. Use of physical restraint in nursing homes: Clinical-ethical considerations. J. Med. Ethics 2006, 32, 148–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benbenbishty, J.; Adam, S.; Endacott, R. Physical restraint use in intensive care units across Europe: The PRICE study. Intensive Crit. Care Nurs. 2010, 26, 241–245. [Google Scholar] [CrossRef] [PubMed]
- Minnick, A.F.; Mion, L.C.; Johnson, M.E.; Catrambone, C.; Leipzig, R. Prevalence and Variation of Physical Restraint Use in Acute Care Settings in the US. J. Nurs. Scholarsh. 2007, 39, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Kruger, C.; Mayer, H.; Haastert, B.; Meyer, G. Use of physical restraints in acute hospitals in Germany: A multi-centre cross-sectional study. Int. J. Nurs. Stud. 2013, 50, 1599–1606. [Google Scholar] [CrossRef]
- Kwok, T.; Bai, X.; Chui, M.Y.; Lai, C.K.; Ho, D.W.; Ho, F.K.; Woo, J. Effect of physical restraint reduction on older patients’ hospital length of stay. J. Am. Med. Dir. Assoc. 2012, 13, 645–650. [Google Scholar] [CrossRef]
- The Federal Assembly of the Swiss Confederation. The Publication Platform for Federal Law. The Civil Code Switzerland; The Federal Assembly of the Swiss Confederation: Bern, Switzerland, 1907. [Google Scholar]
- Raguan, B. Use of Physical Restraints in a General Hospital a cross sectional observational study. IMAJ 2015, 17, 633–638. [Google Scholar]
- Bai, X.; Kwok, T.C.; Ip, I.N.; Woo, J.; Chui, M.Y.; Ho, F.K. Physical restraint use and older patients’ length of hospital stay. Health Psychol. Behav. Med. 2014, 2, 160–170. [Google Scholar] [CrossRef]
- Weinrebe, W.; Johannsdottir, E.; Karaman, M.; Fusgen, I. What does delirium cost? An economic evaluation of hyperactive delirium. Z Gerontol. Geriatr. 2016, 49, 52–58. [Google Scholar] [CrossRef] [Green Version]
- Thomann, S.; Zwakhalen, S.; Richter, D.; Bauer, S.; Hahn, S. Restraint use in the acute-care hospital setting: A cross-sectional multi-centre study. Int. J. Nurs. Stud. 2021, 114, 103807. [Google Scholar] [CrossRef]
- Park, J.; Jeong, E.; Lee, J. The Delirium Observation Screening Scale: A Systematic Review and Meta-Analysis of Diagnostic Test Accuracy. Clin. Nurs. Res. 2021, 30, 464–473. [Google Scholar] [CrossRef] [PubMed]
- Wei, L.A.; Fearing, M.A.; Sternberg, E.J.; Inouye, S.K. The Confusion Assessment Method: A systematic review of current usage. J. Am. Geriatr. Soc. 2008, 56, 823–830. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feng, Z.; Hirdes, J.P.; Smith, T.F.; Finne-Soveri, H.; Chi, I.; Du Pasquier, J.N.; Gilgen, R.; Ikegami, N.; Mor, V. Use of physical restraints and antipsychotic medications in nursing homes: A cross-national study. Int. J. Geriatr. Psychiatry 2009, 24, 1110–1118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lam, K.; Kwan, J.S.K.; Wai Kwan, C.; Chong, A.M.L.; Lai, C.K.Y.; Lou, V.W.Q.; Leung, A.Y.M.; Liu, J.Y.W.; Bai, X.; Chi, I. Factors Associated With the Trend of Physical and Chemical Restraint Use Among Long-Term Care Facility Residents in Hong Kong: Data From an 11-Year Observational Study. J. Am. Med. Dir. Assoc. 2017, 18, 1043–1048. [Google Scholar] [CrossRef]
- Strumpf, N.E.; Evans, L.K. Physical restraint of the hospitalized elderly: Perceptions of patients and nurses. Nurs. Res. 1988, 37, 132–137. [Google Scholar] [CrossRef]
- Wilson, C.; Rouse, L.; Rae, S.; Kar Ray, M. Mental health inpatients’ and staff members’ suggestions for reducing physical restraint: A qualitative study. J. Psychiatr. Ment. Health Nurs. 2018, 25, 188–200. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhuang, Y.; Lao, Y.; Qiao, L.; Chen, Y.; Guo, F. Development and implementation of a novel decision support tool on physical restraint use in critically ill adult patients. Int. J. Nurs. Pract. 2021, 28, e12961. [Google Scholar] [CrossRef]
- Mott, S.; Poole, J.; Kenrick, M. Physical and chemical restraints in acute care: Their potential impact on the rehabilitation of older people. Int. J. Nurs. Pract. 2005, 11, 95–101. [Google Scholar] [CrossRef]
- Capezuti, E.; Strumpf, N.E.; Evans, L.K.; Grisso, J.A.; Maislin, G. The relationship between physical restraint removal and falls and injuries among nursing home residents. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1998, 53, M47–M52. [Google Scholar] [CrossRef] [Green Version]
- Shorr, R.I.; Guillen, M.K.; Rosenblatt, L.C.; Walker, K.; Caudle, C.E.; Kritchevsky, S.B. Restraint use, restraint orders, and the risk of falls in hospitalized patients. J. Am. Geriatr. Soc. 2002, 50, 526–529. [Google Scholar] [CrossRef]
- Hart, B.D.; Birkas, J.; Lachmann, M.; Saunders, L. Promoting positive outcomes for elderly persons in the hospital: Prevention and risk factor modification. AACN Clin. Issues 2002, 13, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Barton-Gooden, A.; Dawkins, P.E.; Bennett, J. Physical Restraint Usage at a Teaching Hospital: A Pilot Study. Clin. Nurs. Res. 2013, 24, 73–90. [Google Scholar] [CrossRef] [PubMed]
- Heinze, C.; Dassen, T.; Grittner, U. Use of physical restraints in nursing homes and hospitals and related factors: A cross-sectional study. J. Clin. Nurs. 2012, 21, 1033–1040. [Google Scholar] [CrossRef] [PubMed]
- Thomann, S.; Hahn, S.; Schmitt, K.U.; Barbezat, I.; Siegrist-Dreier, S.; Richter, D. Restraint use as a quality indicator for the hospital setting: A secondary data analysis. Swiss Med. Wkly. 2021, 151, w30043. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]



| Factor | Overall | Without Restraints | With Restraints | p-Value ¶ |
|---|---|---|---|---|
| n = 11,979 (100%) | n = 11,207 (93.6%) | n = 772 (6.4%) | ||
| Age, years | 68 (±16) | 68 (±16) | 78 (±12) | <0.001 |
| Female gender | 5257 (43.9%) | 4937 (44.1%) | 320 (41.5%) | 0.16 |
| Elixhauser CMI | 9.1 (±8.5) | 8.8 (±8.4) | 12.6 (±8.8) | <0.001 |
| DOS points | 0.8 (±1.7) | 0.6 (±1.3) | 3.3 (±2.3) | <0.001 |
| DOS compliance * | 972 (92.2%) | 762 (91.9%) | 210 (93.3%) | 0.48 |
| Major disease (ICD-10 Code) | ||||
| Diseases of the circulatory system | 3339 (27.9%) | 3169 (28.3%) | 170 (22.0%) | |
| Diseases of the respiratory system | 1861 (15.5%) | 1737 (15.5%) | 124 (16.1%) | |
| Neoplasms | 1759 (14.7%) | 1635 (14.6%) | 124 (16.1%) | |
| Diseases of the digestive system | 1245 (10.4%) | 1178 (10.5%) | 67 (8.7%) | |
| Certain infectious and parasitic diseases | 1026 (8.6%) | 946 (8.4%) | 80 (10.4%) | |
| Diseases of the nervous system | 566 (4.7%) | 508 (4.5%) | 58 (7.5%) | |
| Diseases of the genitourinary system | 524 (4.4%) | 482 (4.3%) | 42 (5.4%) | |
| Disease of connective tissue | 534 (4.5%) | 519 (4.6%) | 15 (1.9%) | |
| Endocrine, nutritional and metabolic diseases | 343 (2.9%) | 324 (2.9%) | 19 (2.5%) | |
| Mental and behavioral disorders | 219 (1.8%) | 165 (1.5%) | 54 (7.0%) | |
| Others | 563 (4.7%) | 544 (4.9%) | 19 (2.5%) | <0.001 |
| Place of discharge | ||||
| Outpatient care | 8662 (72.3%) | 8340 (74.4%) | 322 (41.7%) | |
| Rehabilitation facility | 2637 (22.0%) | 2290 (20.4%) | 347 (44.9%) | |
| Year of admission | ||||
| 2018 | 2964 (24.7%) | 2815 (25.1%) | 149 (19.3%) | 0.004 |
| 2019 | 3154 (26.3%) | 2943 (26.3%) | 211 (27.3%) | |
| 2020 | 3034 (25.3%) | 2823 (25.2%) | 211 (27.3%) | |
| 2021 | 2827 (23.6%) | 2626 (23.4%) | 201 (26.0%) | |
| LOS, days | 6 (4–9) | 5 (3–9) | 8 (5–14) | <0.001 |
| Nurses’ time expenditure, hours per admission | 187 (13–255) | 182 (136–243) | 309 (242–402) | <0.001 |
| In-hospital death | 680 (5.7%) | 577 (5.1%) | 103 (13.3%) | <0.001 |
| Without Restraints | With Restraints | Blanket Restrictions | Belts | Bedrails | Sensor Mats | |
|---|---|---|---|---|---|---|
| n = 11,207 (98.3%) | n = 772 (1.7%) | n = 132 (17.1%) | n = 34 (4.4%) | n = 80 (10.4%) | n = 666 (86.3%) | |
| Female gender | 4937 (44.1%) | 320 (41.5%) | 54 (40.9%) | 6 (18%) | 39 (49%) | 280 (42.0%) |
| DOS points | 0.6 (±1.3) | 3.3 (±2.3) | 4.6 (±2.5) | 4.3 (±2.5) | 4.6 (±2.4) | 3.1 (±2.1) |
| DOS compliance | 762 (91.9%) | 210 (93.3%) | 35 (95%) | 5 (71%) | 17 (100%) | 188 (93.5%) |
| Year of admission | ||||||
| 2018 | 2815 (25.1%) | 149 (19.3%) | 32 (24.2%) | 14 (41%) | 27 (34%) | 112 (16.8%) |
| 2019 | 2943 (26.3%) | 211 (27.3%) | 45 (34.1%) | 10 (29%) | 18 (23%) | 185 (27.8%) |
| 2020 | 2823 (25.2%) | 211 (27.3%) | 33 (25.0%) | 6 (18%) | 21 (26%) | 185 (27.8%) |
| 2021 | 2626 (23.4%) | 201 (26%) | 22 (16.7%) | 4 (12%) | 14 (18%) | 184 (27.6%) |
| Place of discharges | ||||||
| Outpatient care | 8340 (74.4%) | 322 (41.7%) | 39 (29.5%) | 8 (24%) | 28 (35%) | 286 (42.9%) |
| Rehabilitation facility | 2290 (20.4%) | 347 (44.9%) | 70 (53.0%) | 19 (56%) | 34 (43%) | 300 (45.0%) |
| Clinical outcomes | ||||||
| LOS, days | 5 (3–9) | 8 (5–14) | 8 (5.5–15) | 13 (6–21) | 11 (6–18) | 8 (5–13) |
| Nurses’ time expenditure hours, hours per admission | 182 (136–243) | 309 (242–402) | 341 (266–447) | 344 (255–472) | 376 (288–476) | 304 (238–393) |
| Fall without restraint or after start of a restraint | 300 (2.7%) | 174 (22.5%) | 35 (26.5%) | 11 (32%) | 29 (36%) | 146 (21.9%) |
| Time difference between fall and restraint, hours * | N/A | −19 (±161) | −20 (±151) | −96 (±191) | −34 (±195) | −22 (±168) |
| Fall during first restraint use | N/A | 46 (6.0%) | 7 (5.3%) | 0 (0%) | 7 (9%) | 39 (5.9%) |
| Restraint duration per total counts of restraints, hours | N/A | 42 (±57) | 25 (±23) | 18 (±21) | 58 (±102) | 42 (±51) |
| In-hospital death | 577 (5.1%) | 103 (13.3%) | 23 (17.4%) | 7 (21%) | 18 (23%) | 80 (12.0%) |
| Outcomes | Nurses’ Time Expenditure, Hours per Admission | LOS, Days | Fall | In-Hospital Death | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | β | 95% CI | p-Value | β | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value |
| Physical restraint yes vs. no | 96.29 | 87.12–105.45 | <0.01 | 2.81 | 2.31–3.31 | <0.01 | 8.85 | 6.85–11.45 | <0.01 | 1.92 | 1.49–2.48 | <0.01 |
| Constant/Baseline | 12.12 | −0.65–24.89 | 0.06 | 4.28 | 3.58–4.98 | <0.01 | 0.005 | 0.002–0.01 | <0.01 | 0.001 | 0.001–0.003 | <0.01 |
| Age, years | 1.67 | 1.52–1.82 | <0.01 | 0.01 | 0.005–0.02 | <0.01 | 1.02 | 1.01–1.03 | <0.01 | 1.04 | 1.03–1.05 | <0.01 |
| Female, gender | 7.18 | 2.75–11.61 | <0.01 | −0.19 | −0.44–0.05 | 0.12 | 0.86 | 0.68–1.09 | 0.21 | 0.94 | 0.79–1.11 | 0.47 |
| Elixhauser CMI | 18.76 | 16.31–21.21 | <0.01 | 1.57 | 1.43–1.70 | <0.01 | 1.45 | 1.32–1.60 | <0.01 | 1.37 | 1.27–1.47 | <0.01 |
| Year of admission | ||||||||||||
| 2018 | Ref. | Ref. | Ref. | Ref. | ||||||||
| 2019 | 3.13 | −2.85–9.10 | 0.31 | 0.02 | −0.32–0.35 | 0.92 | 0.75 | 0.55–1.02 | 0.07 | 0.93 | 0.73–1.18 | 0.53 |
| 2020 | 30.66 | 24.67–36.65 | <0.01 | −0.30 | −0.63–0.04 | 0.08 | 0.74 | 0.54–1.01 | 0.06 | 0.85 | 0.66–1.08 | 0.17 |
| 2021 | 30.15 | 23.70–36.61 | <0.01 | −0.003 | −0.35–0.34 | 0.98 | 0.73 | 0.53–1.01 | 0.06 | 1.08 | 0.85–1.37 | 0.51 |
| Major disease (ICD-10 Code) | ||||||||||||
| Diseases of the circulatory system | Ref. | Ref. | Ref. | Ref. | ||||||||
| Diseases of the respiratory system | 75.18 | 69.10–81.27 | <0.01 | 0.77 | 0.44–1.11 | <0.01 | 1.22 | 0.87–1.72 | 0.25 | 1.58 | 1.21–2.05 | <0.01 |
| Neoplasms | 52.31 | 45.78–58.85 | <0.01 | 3.37 | 3.02–3.73 | <0.01 | 2.12 | 1.56–2.88 | <0.01 | 3.77 | 2.99–4.77 | <0.01 |
| Diseases of the digestive system | 49.66 | 42.70–56.62 | <0.01 | 0.49 | 0.11–0.87 | 0.01 | 0.84 | 0.54–1.30 | 0.43 | 0.77 | 0.53–1.13 | 0.19 |
| Certain infectious and parasitic diseases | 81.98 | 74.50–89.45 | <0.01 | 1.19 | 0.78–1.59 | <0.01 | 1.19 | 0.79–1.79 | 0.40 | 2.75 | 2.09–3.60 | <0.01 |
| Class of insurance | −13.00 | −19.75–(−6.25) | <0.01 | −0.37 | −0.74–0.01 | 0.05 | 1.02 | 0.73–1.44 | 0.89 | 0.94 | 0.73–1.21 | 0.65 |
| Medical Wards | ||||||||||||
| 1 | Ref. | Ref. | Ref. | Ref. | ||||||||
| 2 | 23.52 | 16.33–30.71 | <0.01 | −0.31 | −0.70–0.08 | 0.12 | 1.02 | 0.68–1.53 | 0.91 | 1.25 | 0.93–1.69 | 0.14 |
| 3 | 2.67 | −4.62–9.96 | 0.47 | 0.35 | −0.05–0.75 | 0.09 | 1.18 | 0.79–1.77 | 0.43 | 1.07 | 0.79–1.45 | 0.67 |
| 4 | 3.05 | −5.98–12.08 | 0.51 | 0.76 | 0.27–1.24 | <0.01 | 1.20 | 0.75–1.92 | 0.44 | 1.09 | 0.78–1.54 | 0.61 |
| 5 | 0.83 | −7.266–8.92 | 0.84 | 0.35 | −0.09–0.79 | 0.12 | 1.17 | 0.76–1.82 | 0.48 | 1.24 | 0.90–1.72 | 0.19 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spennato, U.; Lerjen, N.; Siegwart, J.; Mueller, B.; Schuetz, P.; Koch, D.; Struja, T. Prevalence, Risk Factors and Outcomes Associated with Physical Restraint in Acute Medical Inpatients over 4 Years—A Retrospective Cohort Study. Geriatrics 2023, 8, 15. https://doi.org/10.3390/geriatrics8010015
Spennato U, Lerjen N, Siegwart J, Mueller B, Schuetz P, Koch D, Struja T. Prevalence, Risk Factors and Outcomes Associated with Physical Restraint in Acute Medical Inpatients over 4 Years—A Retrospective Cohort Study. Geriatrics. 2023; 8(1):15. https://doi.org/10.3390/geriatrics8010015
Chicago/Turabian StyleSpennato, Umberto, Nathalie Lerjen, Jennifer Siegwart, Beat Mueller, Philipp Schuetz, Daniel Koch, and Tristan Struja. 2023. "Prevalence, Risk Factors and Outcomes Associated with Physical Restraint in Acute Medical Inpatients over 4 Years—A Retrospective Cohort Study" Geriatrics 8, no. 1: 15. https://doi.org/10.3390/geriatrics8010015
APA StyleSpennato, U., Lerjen, N., Siegwart, J., Mueller, B., Schuetz, P., Koch, D., & Struja, T. (2023). Prevalence, Risk Factors and Outcomes Associated with Physical Restraint in Acute Medical Inpatients over 4 Years—A Retrospective Cohort Study. Geriatrics, 8(1), 15. https://doi.org/10.3390/geriatrics8010015








