Socioeconomic Inequalities in the Prevalence of Non-Communicable Diseases among Older Adults in India
Abstract
1. Introduction
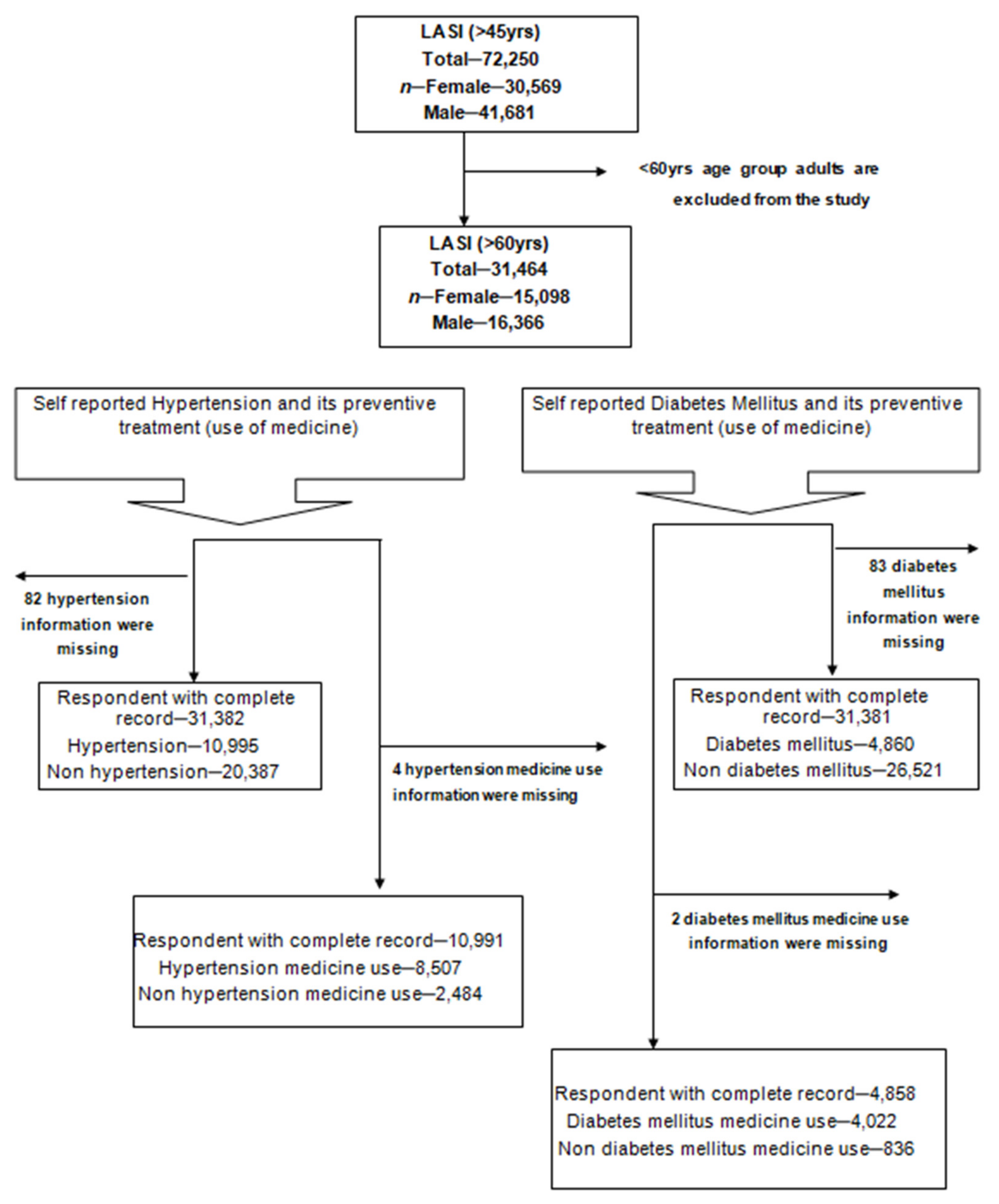
2. Materials and Methods
2.1. Data
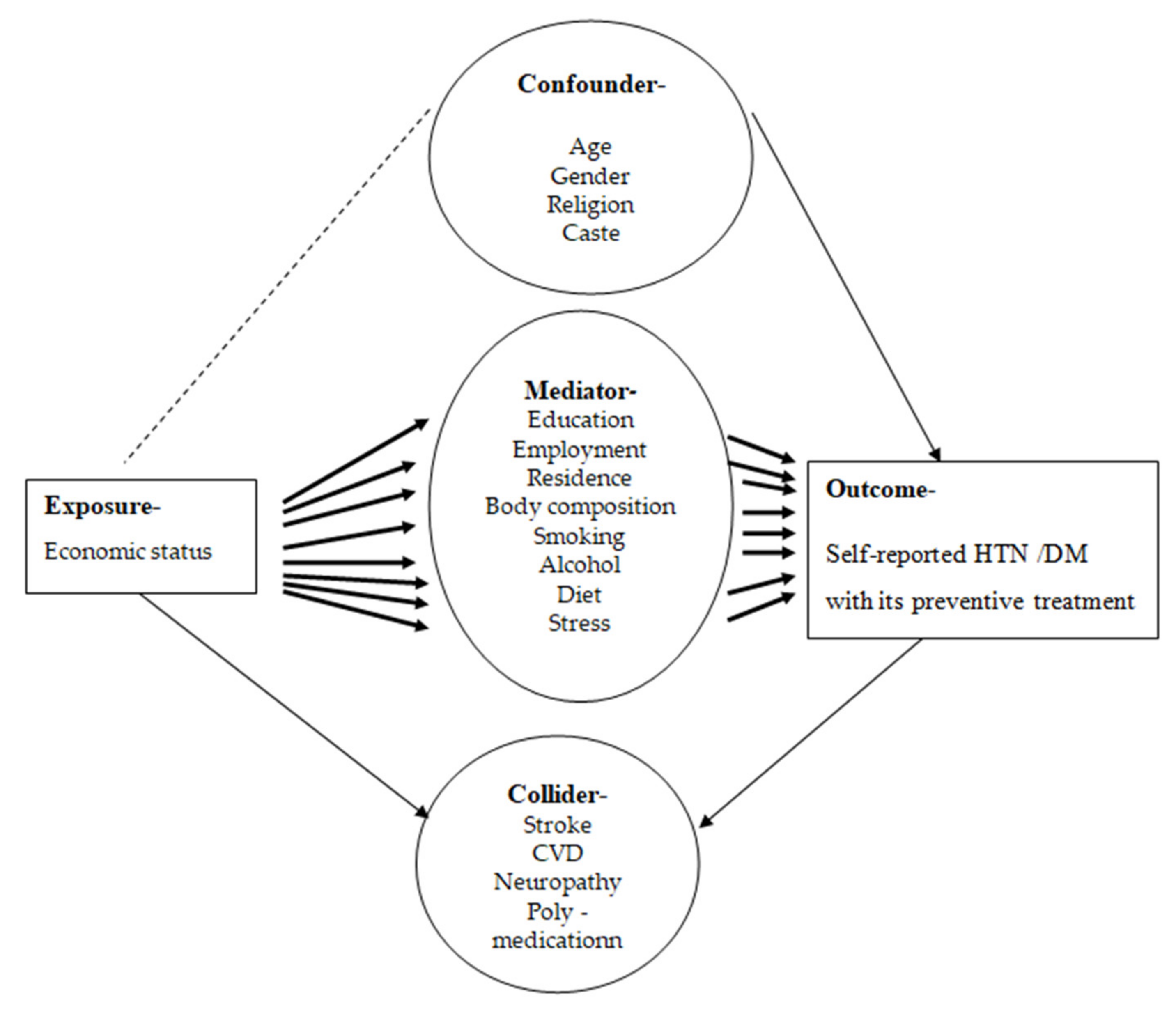
2.2. Variable Description
2.3. Statistical Analysis
2.3.1. The “Relative Index of Inequality”
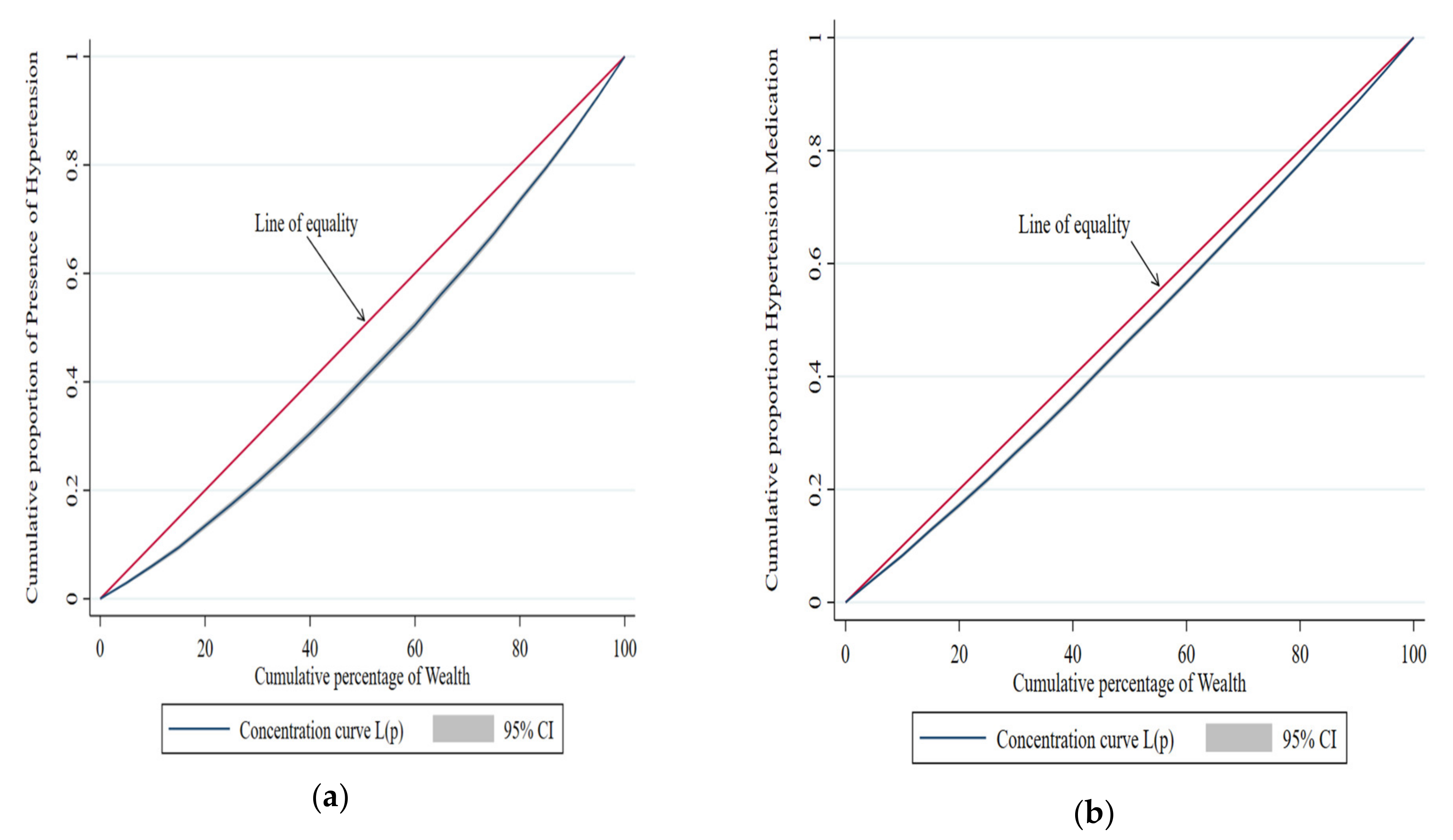
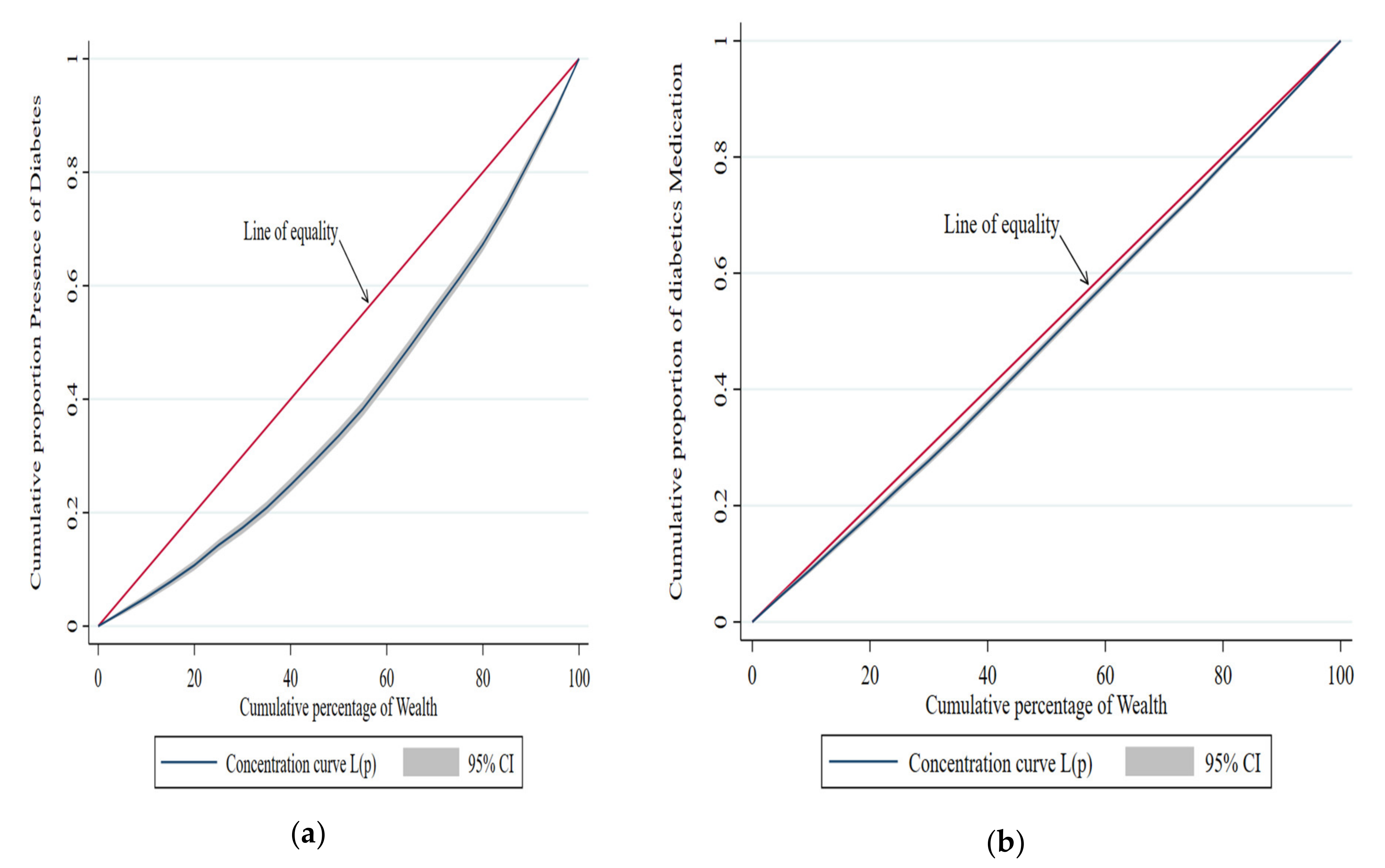
2.3.2. Concentration Index
2.3.3. “Decomposition Analysis” for “C”
3. Results
The ‘Cs’ Have Been Decomposed
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| NCD | Non-communicable diseases |
| GBD | Global burden of diseases |
| HTN | Hypertension |
| DM | Diabetes mellitus |
| SC | Scheduled caste |
| ST | Scheduled tribes |
| OBC | Other backward class |
| MPCE | Monthly per capita consumption expenditure |
| RII | Relative index of inequality |
| C | Economic-related concentration index |
| SES | Socioeconomic status |
| CI | Confidence interval |
References
- Wang, H.; Abbas, K.M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; Abolhassani, H.; Abreu, L.G.; Abrigo, M.R.M.; et al. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: A comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1160–1203. [Google Scholar] [CrossRef] [PubMed]
- Key_findings_wpp_2015.Pdf. Available online: https://population.un.org/wpp/publications/files/key_findings_wpp_2015.pdf (accessed on 12 March 2021).
- World Health Organization. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Marmot, M.; Friel, S.; Bell, R.; Houweling, T.A.; Taylor, S.; on behalf of the Commission on Social Determinants of Health. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet 2008, 372, 1661–1669. [Google Scholar] [CrossRef] [PubMed]
- Balarajan, Y.; Selvaraj, S.; Subramanian, S. Healthcare and equity in India. Lancet 2011, 377, 505–515. [Google Scholar] [CrossRef] [PubMed]
- Konings, P.; Harper, S.; Lynch, J.; Hosseinpoor, A.R.; Berkvens, D.; Lorant, V.; Geckova, A.M.; Speybroeck, N. Analysis of socioeconomic health inequalities using the concentration index. Int. J. Public Health 2009, 55, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Trends in the Black-White Life Expectancy Gap, 2003–200|Cerebrovascular Disease|JAMA|JAMA Network. Available online: https://jamanetwork.com/journals/jama/fullarticle/1172038 (accessed on 3 February 2022).
- Tobias, M.; Blakely, T.; Matheson, D.; Rasanathan, K.; Atkinson, J. Changing trends in indigenous inequalities in mortality: Lessons from New Zealand. Int. J. Epidemiol. 2009, 38, 1711–1722. [Google Scholar] [CrossRef] [PubMed]
- Naghavi, M.; Abajobir, A.A.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Adetokunboh, O.; Afshin, A.; Agrawal, A.; et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1151–1210. [Google Scholar] [CrossRef]
- Arokiasamy, P. India’s escalating burden of non-communicable diseases. Lancet Glob. Health 2018, 6, e1262–e1263. [Google Scholar] [CrossRef]
- Noncommunicable Diseases|National Health Portal. Available online: https://www.nhp.gov.in/healthilyliving/ncd2019 (accessed on 3 February 2022).
- The Changing Patterns of Cardiovascular Disease and Their Risk Factors in the States of India: The Global Burden of Disease Study 1990–2016—The Lancet Global Health. Available online: https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(18)30407-8/fulltext (accessed on 3 February 2022).
- India State-Level Disease Burden Initiative Diabetes Collaborators. The increasing burden of diabetes and variations among the states of India: The Global Burden of Disease Study 1990–2016. Lancet Glob. Health 2018, 6, e1352–e1362. [Google Scholar] [CrossRef]
- NCDs POLICY BRIEF–INDIA; February 2011, The World Bank, South Asia Human Development, Health Nutrition, and Population. Available online: https://documents1.worldbank.org/curated/en/281961505994118415/pdf/119405-BRI-P114171-PUBLIC-NCD-IN.pdf (accessed on 12 March 2021).
- Engelgau, M.M.; Karan, A.; Mahal, A. The Economic impact of Non-communicable Diseases on households in India. Glob. Health 2012, 8, 9. [Google Scholar] [CrossRef]
- Mondal, S.; Van Belle, S. India’s NCD strategy in the SDG era: Are there early signs of a paradigm shift? Glob. Health 2018, 14, 1–9. [Google Scholar] [CrossRef]
- Ataguba, J.E.; Akazili, J.; McIntyre, D. Socioeconomic-related health inequality in South Africa: Evidence from General Household Surveys. Int. J. Equity Health 2011, 10, 48. [Google Scholar] [CrossRef]
- Glover, J.D.; Hetzel, D.M.; Tennant, S.K. The socioeconomic gradient and chronic illness and associated risk factors in Australia. Aust. N. Z. Health Policy 2004, 1, 8. [Google Scholar] [CrossRef] [PubMed]
- Dalstra, A.A.J.; Kunst, E.A.; Borrell, C.; Breeze, E.; Cambois, E.; Costa, G.; Geurts, J.J.M.; Lahelma, E.; Van Oyen, H.; Rasmussen, N.K.; et al. Socioeconomic differences in the prevalence of common chronic diseases: An overview of eight European countries. Leuk. Res. 2005, 34, 316–326. [Google Scholar] [CrossRef] [PubMed]
- Di Cesare, M.; Khang, Y.-H.; Asaria, P.; Blakely, T.; Cowan, M.J.; Farzadfar, F.; Guerrero, R.; Ikeda, N.; Kyobutungi, C.; Msyamboza, K.P.; et al. Inequalities in non-communicable diseases and effective responses. Lancet 2013, 381, 585–597. [Google Scholar] [CrossRef] [PubMed]
- Corsi, D.J.; Subramanian, S.V. Association between socioeconomic status and self-reported diabetes in India: A cross-sectional multilevel analysis. BMJ Open 2012, 2, e000895. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Jindal, D.; Ajay, V.S.; Kondal, D.; Mandal, S.; Ghosh, S.; Ali, M.; Singh, K.; Huffman, M.D.; Tandon, N.; et al. Association between socioeconomic position and cardiovascular disease risk factors in rural north India: The Solan Surveillance Study. PLoS ONE 2019, 14, e0217834. [Google Scholar] [CrossRef]
- Corsi, D.J.; Subramanian, S.V. Socioeconomic Gradients and Distribution of Diabetes, Hypertension, and Obesity in India. JAMA Netw. Open 2019, 2, e190411. [Google Scholar] [CrossRef]
- Geldsetzer, P.; Manne-Goehler, J.; Theilmann, M.; Davies, J.I.; Awasthi, A.; Vollmer, S.; Jaacks, L.M.; Bärnighausen, T.; Atun, R. Diabetes and Hypertension in India. JAMA Intern. Med. 2018, 178, 363–372. [Google Scholar] [CrossRef]
- Yusuf, S.; Islam, S.; Chow, C.K.; Rangarajan, S.; Dagenais, G.; Diaz, R.; Gupta, R.; Kelishadi, R.; Iqbal, R.; Avezum, A.; et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): A prospective epidemiological survey. Lancet 2011, 378, 1231–1243. [Google Scholar] [CrossRef]
- McWilliams, J.M.; Meara, E.; Zaslavsky, A.M.; Ayanian, J.Z. Differences in Controlof Cardiovascular Disease and Diabetes by Race, Ethnicity, and Education: U.S. Trends from 1999 to 2006 and Effects of Medicare Coverage. Ann. Intern. Med. 2009, 150, 505–515. [Google Scholar] [CrossRef]
- Su, R.; Cai, L.; Cui, W.; He, J.; You, D.; Golden, A. Multilevel Analysis of Socioeconomic Determinants on Diabetes Prevalence, Awareness, Treatment and Self-Management in Ethnic Minorities of Yunnan Province, China. Int. J. Environ. Res. Public Health 2016, 13, 751. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.F.; Ettner, S.L.; Piette, J.; Weinberger, M.; Gregg, E.; Shapiro, M.F.; Karter, A.J.; Safford, M.; Waitzfelder, B.; Prata, P.A.; et al. Socioeconomic Position and Health among Persons with Diabetes Mellitus: A Conceptual Framework and Review of the Literature. Epidemiologic Rev. 2004, 26, 63–77. [Google Scholar] [CrossRef] [PubMed]
- Budreviciute, A.; Damiati, S.; Sabir, D.K.; Onder, K.; Schuller-Goetzburg, P.; Plakys, G.; Katileviciute, A.; Khoja, S.; Kodzius, R. Management and Prevention Strategies for Non-communicable Diseases (NCDs) and Their Risk Factors. Front. Public Health 2020, 8, 574111. [Google Scholar] [CrossRef] [PubMed]
- Arora, M.; Chauhan, K.; John, S.; Mukhopadhyay, A. Multi-Sectoral Action for Addressing Social Determinants of Noncommunicable Diseases and Mainstreaming Health Promotion in National Health Programmes in India. Indian J. Community Med. 2011, 36 (Suppl. S1), 43–49. [Google Scholar] [CrossRef]
- GBD 2015 SDG Collaborators. Measuring the health-related Sustainable Development Goals in 188 countries: A baseline analysis from the Global Burden of Disease Study 2015. Lancet 2016, 388, 1813–1850. [Google Scholar] [CrossRef]
- Lasi_india_report_2020.Pdf. Available online: https://lasi-india.org/public/documentation/LASI_India_Report_2020.pdf (accessed on 4 February 2022).
- Longitudinal Ageing Study in India (LASI)|International Institute for Population Sciences (IIPS). Available online: https://www.iipsindia.ac.in/lasi (accessed on 4 February 2022).
- Shrivastava, U.; Misra, A.; Mohan, V.; Unnikrishnan, R.; Bachani, D. Obesity, Diabetes and Cardiovascular Diseases in India: Public Health Challenges. Curr. Diabetes Rev. 2016, 13, 65–80. [Google Scholar] [CrossRef]
- Lall, D.; Engel, N.; Devadasan, N.; Horstman, K.; Criel, B. Challenges in primary care for diabetes and hypertension: An observational study of the Kolar district in rural India. BMC Health Serv. Res. 2019, 19, 44. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, L.; Hsiao, W. Ill health and its potential influence on household consumptions in rural China. Health Policy 2006, 78, 167–177. [Google Scholar] [CrossRef]
- Sergeant, J.C. Relative index of inequality: Definition, estimation, and inference. Biostatistics 2005, 7, 213–224. [Google Scholar] [CrossRef]
- Costa-Font, J.; Hernández-Quevedo, C. Measuring inequalities in health: What do we know? What do we need to know? Health Policy 2012, 106, 195–206. [Google Scholar] [CrossRef]
- Hosseinpoor, A.R.; Bergen, N.; Kunst, A.; Harper, S.; Guthold, R.; Rekve, D.; D’Espaignet, E.T.; Naidoo, N.; Chatterji, S. Socioeconomic inequalities in risk factors for non communicable diseases in low-income and middle-income countries: Results from the World Health Survey. BMC Public Health 2012, 12, 912. [Google Scholar] [CrossRef] [PubMed]
- On Decomposing the Causes of Health Sector Inequalities with an Application to Malnutrition Inequalitiesin Vietnam. Available online: https://openknowledge.worldbank.org/handle/10986/19426 (accessed on 4 February 2022).
- O’Donnell, O.; Van Doorslaer, E.; Wagstaff, A.; Lindelow, M. Analyzing Health Equity Using Household Survey Data, October 2007. Available online: https://elibrary.worldbank.org/doi/epdf/10.1596/978-0-8213-6933-3 (accessed on 4 February 2022).
- Xu, K. Analysing health equity using household survey data: A guide to techniques and their implementation. Bull. World Health Organ. 2008, 86, 816. [Google Scholar] [CrossRef]
- Ramachandran, A.; Snehalatha, C.; Kapur, A.; Vijay, V.; Mohan, V.; Das, A.K.; Rao, P.V.; Yajnik, C.S.; Kumar, K.M.P.; Nair, J.D. High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia 2001, 44, 1094–1101. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Hu, J.; McCoy, T.P.; Li, G.; Zhu, J.; Lei, M.; Yuan, J.; Peng, J.; Kong, L. Socioeconomic Status and the Prevalence of Type 2 Diabetes Among Adults in Northwest China. Diabetes Educ. 2015, 41, 599–608. [Google Scholar] [CrossRef]
- Vellakkal, S.; Millett, C.; Basu, S.; Khan, Z.; Aitsi-Selmi, A.; Stuckler, D.; Ebrahim, S. Are estimates of socioeconomic inequalities in chronic disease artefactually narrowed by self-reported measures of prevalence in low-income and middle-income countries? Findings from the WHO-SAGE survey. J. Epidemiol. Community Health 2014, 69, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.-J.; Dong, G.-H.; Wang, D.; Liu, M.-M.; Lin, Q.; Tian, S.; Xu, L.-X.; Hou, H.; Ren, Y.-F.; Lee, Y.L. Prevalence, awareness, treatment, control, and risk factors associated with hypertension in urban adults from 33 communities of China: The CHPSNE study. J. Hypertens. 2011, 29, 1303–1310. [Google Scholar] [CrossRef]
- Fu, C.; Chen, Y.; Wang, F.; Wang, X.; Song, J.; Jiang, Q. High prevalence of hyperglycaemia and the impact of high household income in transforming Rural China. BMC Public Health 2011, 11, 862. [Google Scholar] [CrossRef]
- Vellakkal, S.; Subramanian, S.V.; Millett, C.; Basu, S.; Stuckler, D.; Ebrahim, S. Socioeconomic Inequalities in Non-Communicable Diseases Prevalence in India: Disparities between Self-Reported Diagnoses and Standardized Measures. PLoS ONE 2013, 8, e68219. [Google Scholar] [CrossRef]
- Singh, P.K.; Singh, L.; Dubey, R.; Singh, S.; Mehrotra, R. Socioeconomic determinants of chronic health diseases among older Indian adults: A nationally representative cross-sectional multilevel study. BMJ Open 2019, 9, e028426. [Google Scholar] [CrossRef]
- Robbins, J.M.; Vaccarino, V.; Zhang, H.; Kasl, S.V. Socioeconomic status and diagnosed diabetes incidence. Diabetes Res. Clin. Pract. 2005, 68, 230–236. [Google Scholar] [CrossRef]
- Kaplan, M.S.; Huguet, N.; Feeny, D.H.; McFarland, B.H. Self-reported hypertension prevalence and income among older adults in Canada and the United States. Soc. Sci. Med. 2010, 70, 844–849. [Google Scholar] [CrossRef] [PubMed]
- Korda, R.J.; Paige, E.; Yiengprugsawan, V.; Latz, I.; Friel, S. Income-related inequalities in chronic conditions, physical functioning and psychological distress among older people in Australia: Cross-sectional findings from the 45 and up study. BMC Public Health 2014, 14, 741. [Google Scholar] [CrossRef] [PubMed]
- Stringhini, S.; Viswanathan, B.; Gédéon, J.; Paccaud, F.; Bovet, P. The social transition of risk factors for cardiovascular disease in the African region: Evidence from three cross-sectional surveys in the Seychelles. Int. J. Cardiol. 2012, 168, 1201–1206. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.C.K.; Pomeroy, E.; Walimbe, S.R.; Popkin, B.M.; Yajnik, C.S. The Elevated Susceptibility to DiabetesinIndia: An Evolutionary Perspective. Front. Public Health 2016, 4, 45. [Google Scholar] [CrossRef]
- Prabhakaran, D.; Singh, K.; Roth, G.A.; Banerjee, A.; Pagidipati, N.J.; Huffman, M.D. Cardiovascular Diseases in India Compared With the United States. J. Am. Coll. Cardiol. 2018, 72, 79–95. [Google Scholar] [CrossRef]
- Lin, X.; Xu, Y.; Pan, X.; Xu, J.; Ding, Y.; Sun, X.; Song, X.; Ren, Y.; Shan, P.F. Global, regional, and national burden and trend of diabetes in 195 countries and territories: An analysis from 1990 to 2025. Sci. Rep. 2020, 10, 14790. [Google Scholar] [CrossRef]
- Khan, J.A.; Trujillo, A.J.; Ahmed, S.; Siddiquee, A.T.; Alam, N.; Mirelman, A.J.; Koehlmoos, T.P.; Niessen, L.W.; Peters, D.H. Distribution of chronic disease mortality and deterioration in household socioeconomic status in rural Bangladesh: An analysis over a 24-year period. Int. J. Epidemiol. 2015, 44, 1917–1926. [Google Scholar] [CrossRef][Green Version]
- Carrieri, V.; Wuebker, A. Assessing inequalities in preventive care use in Europe. Health Policy 2013, 113, 247–257. [Google Scholar] [CrossRef]
- Rundall, T.G.; Wheeler, J.R.C. The Effect of Income on Use of Preventive Care: An Evaluation of Alternative Explanations. J. Health Soc. Behav. 1979, 20, 397. [Google Scholar] [CrossRef]
- Chentli, F.; Azzoug, S.; Mahgoun, S. Diabetes mellitus in elderly. Indian J. Endocrinol. Metab. 2015, 19, 744–752. [Google Scholar] [CrossRef]
- Gatimu, S.M.; John, T.W. Socioeconomic inequalities in hypertension in Kenya: A decomposition analysis of 2015 Kenya STEPwise survey on non-communicable diseases risk factors. Int. J. Equity Health 2020, 19, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Neufcourt, L.; Zins, M.; Berkman, L.F.; Grimaud, O. Socioeconomic disparities and risk of hypertension among older Americans: The Health and Retirement Study. J. Hypertens. 2021, 39, 2497–2505. [Google Scholar] [CrossRef] [PubMed]
- Thrift, A.G.; Ragavan, R.S.; Riddell, M.A.; Joshi, R.; Thankappan, K.R.; Chow, C.; Oldenburg, B.; Mahal, A.S.; Kalyanram, K.; Kartik, K.; et al. Hypertension in Rural India: The Contribution of Socioeconomic Position. J. Am. Heart Assoc. 2020, 9, e014486. [Google Scholar] [CrossRef] [PubMed]
| Characteristics Profile of the Respondents Aged 60 and above Population (n = 31,464) | |||
|---|---|---|---|
| Variables | n | Proportion | CI |
| HTN and its preventive care | |||
| HTN | 10,995 | 0.33 | [0.32–0.34] |
| Currently on medication | 8507 | 0.77 a | [0.76–0.79] |
| Diabetics and its preventive care | |||
| DM | 4860 | 0.14 | [0.13–0.15] |
| Currently on medicine | 4022 | 0.82 b | [0.79–0.84] |
| Demographic variables | |||
| Age group | |||
| 60–69 | 18,974 | 0.59 | [0.57–0.60] |
| 70–79 | 9101 | 0.3 | [0.29–0.31] |
| 80 and above | 3389 | 0.11 | [0.11–0.12] |
| Place of residence | |||
| Rural | 20,725 | 0.71 | [0.69–0.72] |
| Urban | 10,739 | 0.29 | [0.28–0.31] |
| Gender | |||
| Male | 15,098 | 0.47 | [0.46–0.49] |
| Female | 15,366 | 0.53 | [0.51–0.54] |
| Cast group | |||
| Schedule caste | 5140 | 0.19 | [0.19–0.20] |
| Schedule tribe | 5173 | 0.08 | [0.08–0.09] |
| Other backward class (OBC) | 11,886 | 0.46 | [0.45–0.48] |
| Others | 8218 | 0.26 | [0.25–0.27] |
| Economic status | |||
| Poorest | 6484 | 0.22 | [0.21–0.23] |
| Poorer | 6477 | 0.22 | [0.21–0.23] |
| Middle | 6416 | 0.21 | [0.20–0.22] |
| Richer | 6170 | 0.19 | [0.18–0.20] |
| Richest | 5917 | 0.16 | [0.15–0.17] |
| Education level | |||
| Illiterate | 16,889 | 0.57 | [0.55–0.58] |
| Primary or below | 7560 | 0.23 | [0.22–0.23] |
| Secondary | 5560 | 0.17 | [0.16–0.18] |
| college and above | 1455 | 0.04 | [0.04–0.05] |
| Marital status | |||
| Married | 19,920 | 0.62 | [0.60–0.63] |
| Single | 11,544 | 0.38 | [0.37–0.40] |
| Religion | |||
| Hindu | 23,037 | 0.82 | [0.81–0.83] |
| Muslim | 3731 | 0.11 | [0.10–0.12] |
| Christian | 3150 | 0.03 | [0.03–0.03] |
| Other | 1546 | 0.04 | [0.03–0.04] |
| Employment status | |||
| Unemployed | 9307 | 0.42 | [0.41–0.43] |
| Employed | 13,373 | 0.58 | [0.57–0.59] |
| HTN and Its Preventive Care | Diabetes Mellitus and Its Preventive Care | |||
|---|---|---|---|---|
| Presence of HTN | Currently on Medication | Presence of DM | Currently on Medication | |
| Respondents (n) | 31,464 | 10,995 | 31,464 | 4860 |
| Poorest, % (95%CI) a | 5.66 [5.20–6.21] | 12.01 [10.72–13.43] | 2.16 [1.89–2.46] | 11.47 [9.43–13.89] |
| Poorer, % (95%CI) a | 6.26 [5.81–6.74] | 14.37 [12.94–15.92] | 2.25 [2.0–2.52] | 12.35 [10.33–14.71] |
| Middle, % (95%CI) a | 6.52 [5.97–7.12] | 15.07 [13.87–16.36] | 2.61 [2.30–2.95] | 13.92 [11.72–16.47] |
| Richer, % (95%CI) a | 7.28 [6.47–8.18] | 18.09 [16.27–20.05] | 3.51 [2.80–4.39] | 21.32 [18.15–24.88] |
| Richest, % (95%CI) a | 7.06 [6.27–7.95] | 17.87 [16.03–19.87] | 3.73 [2.97–4.66] | 22.54 [19.10–26.40] |
| RII b, (95%CI) | 0.29 *** [0.28–0.30] | 0.75 *** [0.73–0.76] | 0.16 *** [0.15–0.17] | 0.81 *** [0.79–0.83] |
| RII c, (95%CI) | 0.18 *** [0.17–0.20] | 0.56 *** [0.53–0.60] | 0.06 *** [0.05–0.07] | 0.69 *** [0.64–0.76] |
| C, (95%CI) | 0.13 *** [0.09–0.16] | 0.10 *** [0.07–0.13] | 0.10 *** [0.06–0.14] | 0.09 *** [0.04–0.15] |
| HTN and Its Preventive Care | Diabetes Mellitus and Its Preventive Care | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Presence of HTN | Currently on Medication | Presence of DM | Currently on Medication | |||||||||
| dy/dx | Con. | %con. | dy/dx | Con. | %con. | dy/dx | Con. | %con. | dy/dx | Con. | %con. | |
| Age Group (Ref: 60–69 years) | ||||||||||||
| 70–79 | 0.018 * | <0.001 | 0.056 | 0.015 | <0.001 | 0.06 | −0.004 | <0.001 | −0.015 | −0.001 | <0.001 | −0.005 |
| 80 and above | 0.002 | <0.001 | −0.006 | 0.018 | <0.001 | −0.098 | −0.031 *** | <0.001 | 0.168 | −0.083 ** | <0.001 | 0.48 |
| Place of residence (Ref: rural) | ||||||||||||
| Urban | 0.098 *** | <0.001 | 0.636 | 0.132 *** | 0.001 | 1.091 | 0.086 *** | <0.001 | 0.726 | 0.076 *** | <0.001 | 0.675 |
| Gender (Ref: female) | ||||||||||||
| Male | −0.086 *** | −0.005 | −3.553 | −0.042 ** | −0.002 | −1.99 | −0.001 | <0.001 | −0.03 | −0.062 ** | −0.003 | −3.211 |
| Cast Group (Ref: schedule caste) | ||||||||||||
| Schedule tribe | −0.080 *** | 0.002 | 1.303 | −0.025 | <0.001 | 0.527 | −0.032 ** | <0.001 | 0.681 | −0.017 | <0.001 | 0.373 |
| Other backwardclass (OBC) | 0.009 | <0.001 | 0.099 | 0.047 *** | <0.001 | 0.671 | 0.016 ** | <0.001 | 0.239 | 0 | <0.001 | 0.005 |
| None of them | 0.023 * | 0.003 | 2.571 | 0.051 ** | 0.007 | 7.304 | 0.012 | 0.002 | 1.81 | 0.015 | 0.002 | 2.381 |
| Economic Status (Ref: poorest) | ||||||||||||
| Poorer | 0.035 *** | −0.009 | −7.089 | 0.065 *** | −0.017 | −16.71 | 0.013 | −0.003 | −3.444 | 0.02 | −0.005 | −5.44 |
| Middle | 0.054 *** | 0.003 | 2.268 | 0.072 *** | 0.004 | 3.818 | 0.027 *** | 0.001 | 1.471 | 0.012 | <0.001 | 0.065 |
| Richer | 0.083 *** | 0.023 | 17.787 | 0.108 *** | 0.03 | 29.69 | 0.055 *** | 0.015 | 15.41 | 0.115 *** | 0.032 | 33.969 |
| Richest | 0.104 *** | 0.037 | 28.61 | 0.143 *** | 0.052 | 50.17 | 0.072 *** | 0.026 | 25.85 | 0.107 *** | 0.039 | 40.64 |
| Education Level (Ref: illiterate) | ||||||||||||
| Primary or below | 0.095 *** | 0.002 | 1.627 | 0.054 *** | 0.001 | 1.175 | 0.068 *** | 0.001 | 1.52 | 0.057 ** | 0.001 | 1.35 |
| Secondary | 0.128 *** | 0.009 | 7.443 | 0.066 *** | 0.005 | 4.873 | 0.092 *** | 0.007 | 6.917 | 0.050 * | 0.004 | 3.994 |
| college and above | 0.133 *** | 0.001 | 0.952 | 0.094 *** | 0.001 | 0.856 | 0.088 *** | <0.001 | 0.816 | −0.036 | <0.001 | −0.354 |
| Marital Status (Ref: single) | ||||||||||||
| Married | −0.002 | <0.001 | −0.225 | 0.016 | 0.002 | 2.046 | 0.015 ** | 0.002 | 2.033 | 0.055 ** | 0.007 | 7.839 |
| Religion (Ref: Hindu) | ||||||||||||
| Muslim | 0.027 * | <0.001 | −0.1 | −0.018 | <0.001 | 0.086 | −0.014 | <0.001 | 0.066 | 0.041 | <0.001 | −0.209 |
| Christian | 0.082 *** | <0.001 | −0.01 | 0.101 *** | <0.001 | −0.016 | 0.073 *** | <0.001 | −0.012 | 0.05 | <0.001 | −0.009 |
| Other | 0.056 *** | <0.001 | 0.17 | 0.025 | <0.001 | 0.097 | 0.015 | <0.001 | 0.061 | 0.024 | <0.001 | 0.099 |
| Employment Status (Ref: unemployment) | ||||||||||||
| Employed | −0.108 *** | 0.003 | 2.45 | −0.090 *** | 0.003 | 2.611 | −0.060 *** | 0.002 | 1.78 | −0.076 *** | 0.002 | 2.374 |
| HTN and Its Preventive Care | Diabetes Mellitus and Its Preventive Care | |||
|---|---|---|---|---|
| Presence of HTN | Currently on Medication | Presence of DM | Currently on Medication | |
| Age-sex groups, Con. (% con.) | −0.005 (−3.503%) | −0.002 (−2.028%) | <0.001 (0.123%) | −0.003 (−2.736%) |
| Economic status, Con. (% con.) | 0.054 (41.576%) | 0.069 (66.968%) | 0.039 (39.287%) | 0.066 (68.938%) |
| Other factors, Con. (% con.) | 0.02 (16.916%) | 0.02 (21.321%) | 0.014 (16.637%) | 0.016 (18.518%) |
| Residual, Con. (% con.) | 0.061 (45.001) | 0.013 (13.739%) | 0.047 (43.953%) | 0.011 (15.280%) |
| C | 0.13 | 0.10 | 0.10 | 0.09 |
| Age-sex adjusted C | 0.135 | 0.102 | 0.10 | 0.093 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khura, B.; Mohanty, P.; Patnaik, L.; Pradhan, K.B.; Khubchandani, J.; Padhi, B.K. Socioeconomic Inequalities in the Prevalence of Non-Communicable Diseases among Older Adults in India. Geriatrics 2022, 7, 137. https://doi.org/10.3390/geriatrics7060137
Khura B, Mohanty P, Patnaik L, Pradhan KB, Khubchandani J, Padhi BK. Socioeconomic Inequalities in the Prevalence of Non-Communicable Diseases among Older Adults in India. Geriatrics. 2022; 7(6):137. https://doi.org/10.3390/geriatrics7060137
Chicago/Turabian StyleKhura, Bikash, Parimala Mohanty, Lipilekha Patnaik, Keerti Bhusan Pradhan, Jagdish Khubchandani, and Bijaya Kumar Padhi. 2022. "Socioeconomic Inequalities in the Prevalence of Non-Communicable Diseases among Older Adults in India" Geriatrics 7, no. 6: 137. https://doi.org/10.3390/geriatrics7060137
APA StyleKhura, B., Mohanty, P., Patnaik, L., Pradhan, K. B., Khubchandani, J., & Padhi, B. K. (2022). Socioeconomic Inequalities in the Prevalence of Non-Communicable Diseases among Older Adults in India. Geriatrics, 7(6), 137. https://doi.org/10.3390/geriatrics7060137







