Sex Difference in Control of Low-Density Lipoprotein Cholesterol in Older Patients after Acute Coronary Syndrome
Abstract
1. Introduction
2. Methods
2.1. Study Design and Population
2.2. Sample Size Calculation
2.3. Data Collection
2.4. Variable Definition
2.4.1. Acute Coronary Syndrome (ACS)
- (1)
- ST-segment elevation myocardial infarction (STEMI): patients with acute chest pain and persistent (>20 min) ST-segment elevation on ECGs, with troponin changes.
- (2)
- Non-ST elevation myocardial infarction (NSTEMI): patients with acute chest discomfort but no persistent ST-segment elevation on ECGs, with troponin changes.
- (3)
- Unstable angina: unstable angina is defined as myocardial ischemia at rest or on minimal exertion in the absence of acute cardiomyocyte injury/necrosis (no troponin changes), without persistent ST-segment elevation.
2.4.2. Outcome Variable
2.4.3. Predictive Variables
Demographics and Lifestyle Factors
Comorbidities
Frailty
Statin Prescription at Discharge
2.5. Statistical Analysis
3. Results
3.1. Study Sample Characteristics
3.2. Statin Utilization
3.3. LDL-C Target Attainment
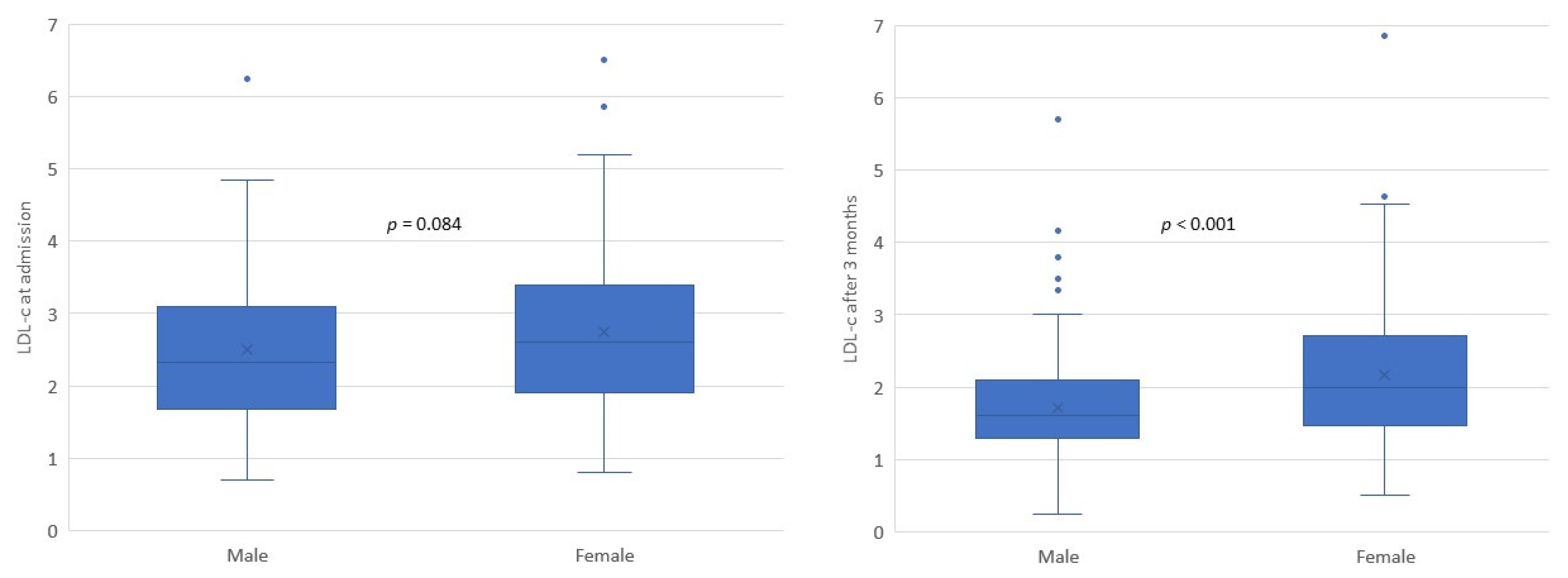
3.4. Sex Difference in Achieving LDL-C Target
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Clark, H. NCDs: A challenge to sustainable human development. Lancet 2013, 381, 510–511. [Google Scholar] [CrossRef]
- World Health Organisation. The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 10 September 2019).
- Ference, B.A.; Ginsberg, H.N.; Graham, I.; Ray, K.K.; Packard, C.J.; Bruckert, E.; Hegele, R.A.; Krauss, R.M.; Raal, F.J.; Schunkert, H.; et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2017, 38, 2459–2472. [Google Scholar] [CrossRef] [PubMed]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur. Heart J. 2019, 41, 111–188. [Google Scholar] [CrossRef] [PubMed]
- Baigent, C.; Blackwell, L.; Emberson, J.; Holland, L.E.; Reith, C.; Bhala, N.; Peto, R.; Barnes, E.H.; Keech, A.; Simes, J.; et al. Efficacy and safety of more intensive lowering of LDL cholesterol: A meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010, 376, 1670–1681. [Google Scholar] [CrossRef]
- Alexander, K.P.; Newby, L.K.; Cannon, C.P.; Armstrong, P.W.; Gibler, W.B.; Rich, M.W.; Van de Werf, F.; White, H.D.; Weaver, W.D.; Naylor, M.D.; et al. Acute coronary care in the elderly, part I: Non-ST-segment-elevation acute coronary syndromes: A scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: In collaboration with the Society of Geriatric Cardiology. Circulation 2007, 115, 2549–2569. [Google Scholar] [CrossRef] [PubMed]
- Walli-Attaei, M.; Joseph, P.; Rosengren, A.; Chow, C.K.; Rangarajan, S.; Lear, S.A.; AlHabib, K.F.; Davletov, K.; Dans, A.; Lanas, F.; et al. Variations between women and men in risk factors, treatments, cardiovascular disease incidence, and death in 27 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet 2020, 396, 97–109. [Google Scholar] [CrossRef]
- Haider, A.; Bengs, S.; Luu, J.; Osto, E.; Siller-Matula, J.M.; Muka, T.; Gebhard, C. Sex and gender in cardiovascular medicine: Presentation and outcomes of acute coronary syndrome. Eur. Heart J. 2020, 41, 1328–1336. [Google Scholar] [CrossRef]
- Nhung, N.T.; Long, T.K.; Linh, B.N.; Vos, T.; Huong, N.T.; Anh, N.D. Estimation of Vietnam national burden of disease 2008. Asia Pac. J. Public Health 2014, 26, 527–535. [Google Scholar] [CrossRef]
- Hoang, V.M.; Dao, L.H.; Wall, S.; Nguyen, T.K.; Byass, P. Cardiovascular disease mortality and its association with socioeconomic status: Findings from a population-based cohort study in rural Vietnam, 1999–2003. Prev. Chronic Dis. 2006, 3, A89. [Google Scholar]
- Islam, S.M.; Purnat, T.D.; Phuong, N.T.; Mwingira, U.; Schacht, K.; Froschl, G. Non-communicable diseases (NCDs) in developing countries: A symposium report. Glob. Health 2014, 10, 81. [Google Scholar] [CrossRef]
- Ngo, A.D.; Rao, C.; Hoa, N.P.; Adair, T.; Chuc, N.T. Mortality patterns in Vietnam, 2006: Findings from a national verbal autopsy survey. BMC Res. Notes 2010, 3, 78. [Google Scholar] [CrossRef] [PubMed]
- Xing, Y.; Liu, J.; Hao, Y.; Liu, J.; Huo, Y.; Smith, S.C., Jr.; Ge, J.; Ma, C.; Han, Y.; Fonarow, G.C.; et al. Prehospital statin use and low-density lipoprotein cholesterol levels at admission in acute coronary syndrome patients with history of myocardial infarction or revascularization: Findings from the Improving Care for Cardiovascular Disease in China (CCC) project. Am. Heart J. 2019, 212, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Chinwong, D.; Patumanond, J.; Chinwong, S.; Siriwattana, K.; Gunaparn, S.; Hall, J.J.; Phrommintikul, A. Low-density lipoprotein cholesterol of less than 70 mg/dL is associated with fewer cardiovascular events in acute coronary syndrome patients: A real-life cohort in Thailand. Ther. Clin. Risk Manag. 2015, 11, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Chin, C.W.; Gao, F.; Le, T.; Tan, R. Lipid goal attainment and prescription behavior in asian patients with acute coronary syndromes: Experience from a tertiary hospital. Clin. Med. Insights Cardiol. 2013, 7, 51–57. [Google Scholar] [CrossRef]
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- Vietnam Heart Association. The 2015 Guidelines for the Diagnosis and Management of Dyslipidaemia. 2015. Available online: http://vnha.org.vn/cate.asp?cate_id=167 (accessed on 12 May 2019).
- Rockwood, K.; Song, X.; MacKnight, C.; Bergman, H.; Hogan, D.B.; McDowell, I.; Mitnitski, A. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005, 173, 489–495. [Google Scholar] [CrossRef]
- Dent, E.; Lien, C.; Lim, W.S.; Wong, W.C.; Wong, C.H.; Ng, T.P.; Woo, J.; Dong, B.; de la Vega, S.; Hua Poi, P.J.; et al. The Asia-Pacific Clinical Practice Guidelines for the Management of Frailty. J. Am. Med. Dir. Assoc. 2017, 18, 564–575. [Google Scholar] [CrossRef]
- Muessig, J.M.; Nia, A.M.; Masyuk, M.; Lauten, A.; Sacher, A.L.; Brenner, T.; Franz, M.; Bloos, F.; Ebelt, H.; Schaller, S.J.; et al. Clinical Frailty Scale (CFS) reliably stratifies octogenarians in German ICUs: A multicentre prospective cohort study. BMC Geriatr. 2018, 18, 162. [Google Scholar] [CrossRef]
- Kim, H.S.; Wu, Y.; Lin, S.J.; Deerochanawong, C.; Zambahari, R.; Zhao, L.; Zhang, Q.; Yan, P. Current status of cholesterol goal attainment after statin therapy among patients with hypercholesterolemia in Asian countries and region: The Return on Expenditure Achieved for Lipid Therapy in Asia (REALITY-Asia) study. Curr. Med. Res. Opin. 2008, 24, 1951–1963. [Google Scholar] [CrossRef]
- Chiang, C.E.; Ferrières, J.; Gotcheva, N.N.; Raal, F.J.; Shehab, A.; Sung, J.; Henriksson, K.M.; Hermans, M.P. Suboptimal Control of Lipid Levels: Results from 29 Countries Participating in the Centralized Pan-Regional Surveys on the Undertreatment of Hypercholesterolaemia (CEPHEUS). J. Atheroscler. Thromb. 2016, 23, 567–587. [Google Scholar] [CrossRef][Green Version]
- Xanthopoulou, I.; Davlouros, P.; Siahos, S.; Perperis, A.; Zaharioglou, E.; Alexopoulos, D. First-line treatment patterns and lipid target levels attainment in very high cardiovascular risk outpatients. Lipids Health Dis. 2013, 12, 170. [Google Scholar] [CrossRef] [PubMed]
- Kauffman, A.B.; Olson, K.L.; Youngblood, M.L.; Zadvorny, E.B.; Delate, T.; Merenich, J.A. Attainment of low-density lipoprotein cholesterol goals in coronary artery disease. J. Clin. Lipidol. 2010, 4, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Karalis, D.G.; Victor, B.; Ahedor, L.; Liu, L. Use of Lipid-Lowering Medications and the Likelihood of Achieving Optimal LDL-Cholesterol Goals in Coronary Artery Disease Patients. Cholesterol 2012, 2012, 861924. [Google Scholar] [CrossRef] [PubMed]
- Karp, I.; Chen, S.-F.; Pilote, L. Sex differences in the effectiveness of statins after myocardial infarction. CMAJ Can. Med. Assoc. J. 2007, 176, 333–338. [Google Scholar] [CrossRef]
- Mombelli, G.; Bosisio, R.; Calabresi, L.; Magni, P.; Pavanello, C.; Pazzucconi, F.; Sirtori, C.R. Gender-related lipid and/or lipoprotein responses to statins in subjects in primary and secondary prevention. J. Clin. Lipidol. 2015, 9, 226–233. [Google Scholar] [CrossRef]
- MOH. National Survey of Risk Factors of NCDs in Vietnam; Ministry of Health: Hanoi, Vietnam, 2016. [Google Scholar]
- Van Minh, H.; Giang, K.B.; Ngoc, N.B.; Hai, P.T.; Huyen, D.T.; Khue, L.N.; Lam, N.T.; Nga, P.T.; Quan, N.T.; Xuyen, N.T. Prevalence of tobacco smoking in Vietnam: Findings from the Global Adult Tobacco Survey 2015. Int. J. Public Health 2017, 62 (Suppl. S1), 121–129. [Google Scholar] [CrossRef]
- Yudi, M.B.; Farouque, O.; Andrianopoulos, N.; Ajani, A.E.; Kalten, K.; Brennan, A.L.; Lefkovits, J.; Hiew, C.; Oqueli, E.; Reid, C.M.; et al. The prognostic significance of smoking cessation after acute coronary syndromes: An observational, multicentre study from the Melbourne interventional group registry. BMJ Open 2017, 7, e016874. [Google Scholar] [CrossRef]
- Lovatt, S.; Wong, C.W.; Holroyd, E.; Butler, R.; Phan, T.; Patwala, A.; Loke, Y.K.; Mallen, C.D.; Kwok, C.S. Smoking cessation after acute coronary syndrome: A systematic review and meta-analysis. Int. J. Clin. Pract. 2021, 75, e14894. [Google Scholar] [CrossRef]
| Variables | All Participants (n = 232) |
|---|---|
| Age | 75.4 ± 9.4 |
| Sex: | |
| Female | 93 (40.1) |
| Male | 139 (59.9) |
| BMI: | |
| Underweight | 20 (8.6) |
| Normal | 111 (47.8) |
| Overweight | 48 (20.7) |
| Obese | 53 (22.8) |
| Sedentary lifestyle | 101 (43.5) |
| Smoking | 35 (15.1) |
| History of using statin before admission | 121 (52.2) |
| History of myocardial infarction | 40 (17.2) |
| History of percutaneous coronary intervention | 65 (28.0) |
| Treated with percutaneous coronary intervention during admission | 128 (55.2) |
| ACS types: | |
| STEMI | 34 (14.7) |
| NSTEMI | 122 (52.6) |
| Unstable angina | 76 (32.8) |
| Frailty (CFS score ≥ 5) | 149 (64.2) |
| Total number of comorbidities | 3.16 ± 1.22 |
| Cardiovascular comorbidities: | |
| Hypertension | 220 (94.8) |
| Heart failure | 120 (51.7) |
| Diabetes | 106 (45.7) |
| Atrial fibrillation | 18 (7.8) |
| Peripheral artery disease | 17 (7.3) |
| Stroke/transient ischemic attack | 13 (5.6) |
| Non-cardiovascular comorbidities: | |
| Stomach problem | 143 (61.9) |
| Chronic kidney disease | 52 (22.4) |
| Urinary problem | 10 (4.3) |
| Cancer | 9 (3.9) |
| Gout | 8 (3.4) |
| Chronic obstructive pulmonary disease | 7 (3.0) |
| Osteoarthritis | 7 (3.0) |
| Anemia | 6 (2.6) |
| Anxiety | 4 (1.7) |
| Dementia | 2 (0.9) |
| Thyroid problem | 1 (0.4) |
| Variables | All Participants (n = 232) | Did Not Achieve LDL-C Target after 3 Months (n = 101) | Achieved LDL-C Target after 3 Months (n = 131) | p |
|---|---|---|---|---|
| Statin types: | ||||
| Atorvastatin 10 mg | 8 (3.4) | 4 (4.0) | 4 (3.1) | 0.101 |
| Atorvastatin 20 mg | 76 (32.8) | 40 (39.6) | 36 (27.5) | |
| Rosuvastatin 10 mg | 10 (4.3) | 6 (5.9) | 4 (3.1) | |
| Rosuvastatin 20 mg | 138 (59.5) | 51 (50.5) | 87 (66.4) | |
| Statin strength: | ||||
| High-intensity statins | 138 (59.5) | 51 (50.5) | 87 (66.4) | 0.014 |
| Non-high-intensity statins | 94 (40.5) | 50 (49.5) | 44 (33.6) | |
| Variables | All Participants (n = 232) | Not Achieving LDL-C Target after 3 Months (n = 101) | Achieving LDL-C Target after 3 Months (n = 131) | p |
|---|---|---|---|---|
| Statin monotherapy | 218 (94.0) | 95 (94.1) | 123 (93.9) | 0.958 |
| Statin plus ezetimibe | 14 (6.0) | 6 (5.9) | 8 (6.1) |
| Factors | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| Unadjusted Odds Ratios for LDL-C Target Achievement (95% CI) | p | Adjusted Odds Ratios for LDL-C Target Achievement (95% CI) | p | |
| Female (vs. male) | 0.34 (0.20–0.59) | <0.001 | 0.25 (0.13–0.51) | <0.001 |
| Age | 0.98 (0.95–1.01) | 0.148 | 1.07 (1.02–1.13) | 0.011 |
| Smoking | 0.25 (0.11–0.55) | <0.001 | 0.10 (0.04–0.29) | <0.001 |
| Having sedentary lifestyle | 0.27 (0.15–0.46) | <0.001 | 0.13 (0.05–0.33) | <0.001 |
| Overweight and obesity (body mass index ≥23) | 1.78 (1.04–3.03) | 0.034 | 1.27 (0.64–2.50) | 0.491 |
| Serum LDL-C level at admission (mmol/L) | 0.70 (0.55–0.90) | 0.005 | 0.58 (0.42–0.81) | 0.001 |
| History of using statin before this admission | 0.60 (0.35–1.01) | 0.053 | 0.48 (0.24–0.99) | 0.048 |
| Receiving percutaneous coronary intervention | 1.13 (0.67–1.90) | 0.646 | 1.00 (0.49–2.05) | 0.999 |
| High-intensity statins prescribed at discharge (vs. non-high-intensity statin) | 1.94 (1.14–3.30) | 0.015 | 2.56 (1.23–5.35) | 0.012 |
| Frailty | 0.57 (0.33–0.10) | 0.050 | 0.75 (0.35–1.59) | 0.447 |
| Total number of comorbidities | 1.03 (0.83–1.27) | 0.819 | 1.10 (0.82–1.45) | 0.540 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, T.V.; Tran, D.T.T.; Ngo, T.T.K.; Nguyen, T.N. Sex Difference in Control of Low-Density Lipoprotein Cholesterol in Older Patients after Acute Coronary Syndrome. Geriatrics 2022, 7, 71. https://doi.org/10.3390/geriatrics7040071
Nguyen TV, Tran DTT, Ngo TTK, Nguyen TN. Sex Difference in Control of Low-Density Lipoprotein Cholesterol in Older Patients after Acute Coronary Syndrome. Geriatrics. 2022; 7(4):71. https://doi.org/10.3390/geriatrics7040071
Chicago/Turabian StyleNguyen, Tan Van, Dieu Thi Thanh Tran, Trinh Thi Kim Ngo, and Tu Ngoc Nguyen. 2022. "Sex Difference in Control of Low-Density Lipoprotein Cholesterol in Older Patients after Acute Coronary Syndrome" Geriatrics 7, no. 4: 71. https://doi.org/10.3390/geriatrics7040071
APA StyleNguyen, T. V., Tran, D. T. T., Ngo, T. T. K., & Nguyen, T. N. (2022). Sex Difference in Control of Low-Density Lipoprotein Cholesterol in Older Patients after Acute Coronary Syndrome. Geriatrics, 7(4), 71. https://doi.org/10.3390/geriatrics7040071







