Effects of Wearing Face Masks on Cardiorespiratory Parameters at Rest and after Performing the Six-Minute Walk Test in Older Adults
Abstract
:1. Introduction
2. Materials and Methods
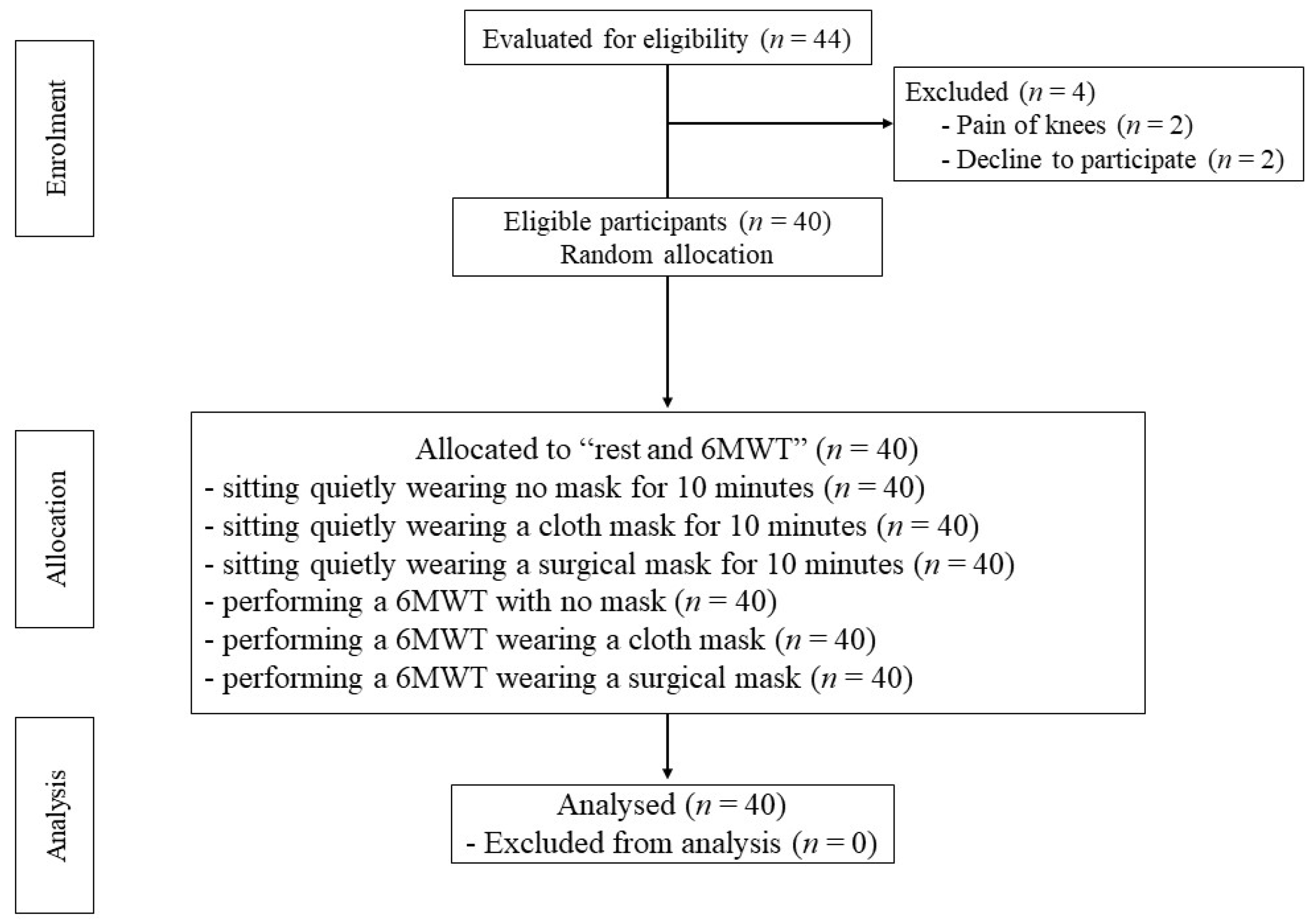
2.1. Study Design
2.2. Participants
2.3. Testing Procedure
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abboah-Offei, M.; Salifu, Y.; Adewale, B.; Bayuo, J.; Ofosu-Poku, R.; Opare-Lokko, E.B.A. A rapid review of the use of face mask in preventing the spread of COVID-19. Int. J. Nurs. Stud. Adv. 2021, 3, 100013. [Google Scholar] [CrossRef]
- Wu, Z.; McGoogan, J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Chia, P.Y.; Coleman, K.K.; Tan, Y.K.; Ong, S.W.X.; Gum, M.; Lau, S.K.; Lim, X.F.; Lim, A.S.; Sutjipto, S.; Lee, P.H.; et al. Detection of air and surface contamination by SARS-CoV-2 in hospital rooms of infected patients. Nat. Commun. 2020, 11, 2800. [Google Scholar] [CrossRef]
- Guo, Z.D.; Wang, Z.Y.; Zhang, S.F.; Li, X.; Li, L.; Li, C.; Cui, Y.; Fu, R.B.; Dong, Y.Z.; Chi, X.Y.; et al. Aerosol and Surface Distribution of Severe Acute Respiratory Syndrome Coronavirus 2 in Hospital Wards, Wuhan, China, 2020. Emerg. Infect. Dis. 2020, 26, 1583–1591. [Google Scholar] [CrossRef]
- World Health Organization. Advice for the Public: Coronavirus Disease (COVID-19); WHO: Geneva, Switzerland, 2021; Volume 3. [Google Scholar]
- Gandhi, M.; Beyrer, C.; Goosby, E. Masks Do More Than Protect Others During COVID-19: Reducing the Inoculum of SARS-CoV-2 to Protect the Wearer. J. Gen. Intern. Med. 2020, 35, 3063–3066. [Google Scholar] [CrossRef]
- Lyu, W.; Wehby, G.L. Community Use Of Face Masks And COVID-19: Evidence From A Natural Experiment Of State Mandates In The US. Health Aff. 2020, 39, 1419–1425. [Google Scholar] [CrossRef]
- De-Yñigo-Mojado, B.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Madera-García, J.; Rodriguez-Sanz, D.; Calvo-Lobo, C.; López-López, D.; Angulo-Carrere, M.T.; San-Antolín, M. Facial Hair Decreases Fit Factor of Masks and Respirators in Healthcare Providers. Biology 2021, 10, 1031. [Google Scholar] [CrossRef]
- Perrotta, F.; Corbi, G.; Mazzeo, G.; Boccia, M.; Aronne, L.; D’Agnano, V.; Komici, K.; Mazzarella, G.; Parrella, R.; Bianco, A. COVID-19 and the elderly: Insights into pathogenesis and clinical decision-making. Aging Clin. Exp. Res. 2020, 32, 1599–1608. [Google Scholar] [CrossRef]
- World Health Organization. Advice on the Use of Masks in the Context of COVID-19: Interim Guidance, 5 June 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Sinkule, E.J.; Powell, J.B.; Goss, F.L. Evaluation of N95 respirator use with a surgical mask cover: Effects on breathing resistance and inhaled carbon dioxide. Ann. Occup. Hyg. 2013, 57, 384–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Person, E.; Lemercier, C.; Royer, A.; Reychler, G. Effect of a surgical mask on six minute walking distance. Rev. Mal. Respir. 2018, 35, 264–268. [Google Scholar] [CrossRef]
- Esposito, S.; Principi, N.; Leung, C.C.; Migliori, G.B. Universal use of face masks for success against COVID-19: Evidence and implications for prevention policies. Eur. Respir. J. 2020, 55, 2001260. [Google Scholar] [CrossRef]
- Chandrasekaran, B.; Fernandes, S. “Exercise with facemask; Are we handling a devil’s sword?”—A physiological hypothesis. Med. Hypotheses 2020, 144, 110002. [Google Scholar] [CrossRef]
- World Health Organization. Mask Use in the Context of COVID-19: Interim Guidance, 1 December 2020; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Reychler, G.; Straeten, C.V.; Schalkwijk, A.; Poncin, W. Effects of surgical and cloth facemasks during a submaximal exercise test in healthy adults. Respir. Med. 2021, 186, 106530. [Google Scholar] [CrossRef]
- Cabanillas-Barea, S.; Rodríguez-Sanz, J.; Carrasco-Uribarren, A.; López de Celis, C.; Rueda, V.; Zegarra-Chávez, D.; Cedeño, S.; Perez-Bellmunt, A. Effects of Using the Surgical Mask and FFP2 during the 6-Min Walking Test. A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 12420. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, M.H.; Bolina, A.F.; Luiz, R.B.; de Oliveira, K.F.; Virtuoso, J.S., Jr.; Rodrigues, R.A.; Silva, L.C.; da Cunha, D.F.; De Mattia, A.L.; Barichello, E. Body mass index as discriminator of the lean mass deficit and excess body fat in institutionalized elderly people. Geriatr. Nurs. 2015, 36, 202–206. [Google Scholar] [CrossRef]
- ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [CrossRef]
- Hill, B.; Annesley, S.H. Monitoring respiratory rate in adults. Br. J. Nurs. 2020, 29, 12–16. [Google Scholar] [CrossRef]
- Shein, S.L.; Whitticar, S.; Mascho, K.K.; Pace, E.; Speicher, R.; Deakins, K. The effects of wearing facemasks on oxygenation and ventilation at rest and during physical activity. PLoS ONE 2021, 16, e0247414. [Google Scholar] [CrossRef]
- Samannan, R.; Holt, G.; Calderon-Candelario, R.; Mirsaeidi, M.; Campos, M. Effect of Face Masks on Gas Exchange in Healthy Persons and Patients with Chronic Obstructive Pulmonary Disease. Ann. Am. Thorac. Soc. 2021, 18, 541–544. [Google Scholar] [CrossRef]
- Cheyne, W.S.; Harper, M.I.; Gelinas, J.C.; Sasso, J.P.; Eves, N.D. Mechanical cardiopulmonary interactions during exercise in health and disease. J. Appl. Physiol. 2020, 128, 1271–1279. [Google Scholar] [CrossRef]
- Ryan, K.L.; Cooke, W.H.; Rickards, C.A.; Lurie, K.G.; Convertino, V.A. Breathing through an inspiratory threshold device improves stroke volume during central hypovolemia in humans. J. Appl. Physiol. 2008, 104, 1402–1409. [Google Scholar] [CrossRef]
- Helgeson, S.A.; Burger, C.D.; Moss, J.E.; Zeiger, T.K.; Taylor, B.J. Facemasks and Walk Distance in Pulmonary Arterial Hypertension Patients. Mayo Clin. Proc. Innov. Qual. Outcomes 2021, 5, 835–838. [Google Scholar] [CrossRef]
- Kim, J.H.; Wu, T.; Powell, J.B.; Roberge, R.J. Physiologic and fit factor profiles of N95 and P100 filtering facepiece respirators for use in hot, humid environments. Am. J. Infect. Control 2016, 44, 194–198. [Google Scholar] [CrossRef]
- Mapelli, M.; Salvioni, E.; De Martino, F.; Mattavelli, I.; Gugliandolo, P.; Vignati, C.; Farina, S.; Palermo, P.; Campodonico, J.; Maragna, R.; et al. “You can leave your mask on”: Effects on cardiopulmonary parameters of different airway protective masks at rest and during maximal exercise. Eur. Respir. J. 2021, 58, 2004473. [Google Scholar] [CrossRef]
- Roberge, R.J.; Kim, J.H.; Benson, S.M. Absence of consequential changes in physiological, thermal and subjective responses from wearing a surgical mask. Respir. Physiol. Neurobiol. 2012, 181, 29–35. [Google Scholar] [CrossRef]
- Swiatek, K.M.; Lester, C.; Ng, N.; Golia, S.; Pinson, J.; Grinnan, D. Impact of Face Masks on 6-Minute Walk Test in Healthy Volunteers. Pulm. Circ. 2021, 11, 2045894020988437. [Google Scholar] [CrossRef]
- O’Keeffe, S.T.; Lye, M.; Donnellan, C.; Carmichael, D.N. Reproducibility and responsiveness of quality of life assessment and six minute walk test in elderly heart failure patients. Heart 1998, 80, 377–382. [Google Scholar] [CrossRef] [Green Version]
- Redelmeier, D.A.; Bayoumi, A.M.; Goldstein, R.S.; Guyatt, G.H. Interpreting small differences in functional status: The Six Minute Walk test in chronic lung disease patients. Am. J. Respir. Crit. Care Med. 1997, 155, 1278–1282. [Google Scholar] [CrossRef]
| Variables | n = 40 (F = 25, M = 15) |
|---|---|
| Sex, n (%) | |
| Female | 25 (62.5) |
| Males | 15 (37.5) |
| Age (years) | 69.60 ± 3.46 |
| Weight (kg) | 51.03 ± 5.91 |
| High (cm) | 155.23 ± 8.47 |
| BMI (kg/m2) | 21.14 ± 1.26 |
| Heart rate (bpm) | 80.0 ± 10.86 |
| Respiratory rate (breaths per minute) | 16.5 ± 2.41 |
| Systolic blood pressure (mmHg) | 139.73 ± 14.99 |
| Diastolic blood pressure (mmHg) | 74.70 ± 7.97 |
| SpO2 (%) | 98 ± 1.05 |
| Comorbidities; n (%) | |
| -None | 17 (42.5) |
| -Hypertension | 12 (30) |
| -Diabetes mellitus | 6 (15) |
| -Dyslipidemia | 5 (12.5) |
| Variables | Duration | No Mask | Cloth Mask | Surgical Mask | p-Value |
|---|---|---|---|---|---|
| Respiratory rate (breaths per minute) | Before sitting | 17.2 ± 1.63 | 17.1 ± 1.91 | 17.3 ± 2.36 | 0.06 |
| After sitting | 17.3 ± 1.97 | 19.0 ± 2.90 | 18.8 ± 2.98 | ||
| Heart rate (bpm) | Before sitting | 75.9 ± 8.82 | 75.9 ± 7.93 | 75.2 ± 8.79 | 0.75 |
| After sitting | 76.3 ± 8.28 | 77.7 ± 8.23 | 77.6 ± 5.55 | ||
| Systolic blood pressure (mmHg) | Before sitting | 140.72 ± 14.13 | 138.75 ± 9.65 | 141.85 ± 7.38 | 0.85 |
| After sitting | 141.20 ± 9.01 | 140.88 ± 7.00 | 142.88 ± 6.27 | ||
| Diastolic blood pressure (mmHg) | Before sitting | 76.03 ± 7.50 | 76.73 ± 6.62 | 77.23 ± 7.55 | 0.10 |
| After sitting | 76.53 ± 7.38 | 76.95 ± 6.52 | 77.55 ± 6.06 | ||
| SpO2 (%) | Before sitting | 98.18 ± 0.81 | 98.40 ± 0.71 | 98.25 ± 0.71 | 0.38 |
| After sitting | 98.10 ± 0.90 | 98.98 ± 0.73 | 97.98 ± 0.86 |
| Variables | Duration | No Mask | Cloth Mask | Surgical Mask | p-Value |
|---|---|---|---|---|---|
| Respiratory rate (breaths per minute) | Pre-6MWT | 19.0 ± 1.27 | 20.0 ± 32.48 | 20.0 ± 2.68 | 0.95 |
| Post-6MWT | 22.2 ± 2.98 | 23.0 ± 4.10 | 23.1 ± 3.15 | ||
| Heart rate (bpm) | Pre-6MWT | 75.9 ± 9.58 | 79.1 ± 11.35 | 80.2 ± 10.50 | 0.84 |
| Post-6MWT | 81.6 ± 10.77 | 83.1 ± 12.02 | 84.1 ± 11.42 | ||
| Systolic blood pressure (mmHg) | Pre-6MWT | 136.78 ± 10.37 | 132.90 ± 13.17 | 130.68 ± 13.63 | 0.37 |
| Post-6MWT | 140.00 ± 10.43 | 140.20 ± 10.34 | 138.78 ± 11.92 | ||
| Diastolic blood pressure (mmHg) | Pre-6MWT | 78.30 ± 7.56 | 78.90 ± 9.37 | 79.78 ± 8.87 | 0.76 |
| Post-6MWT | 81.68 ± 8.92 | 80.48 ± 8.71 | 81.38 ± 9.23 | ||
| SpO2 (%) | Pre-6MWT | 98.18 ± 0.64 | 98.03 ± 1.03 | 98.33 ± 0.62 | 0.57 |
| Post-6MWT | 97.50 ± 1.09 | 97.68 ± 1.16 | 97.83 ± 1.15 | ||
| RPE | Post-6MWT | 7.03 ± 1.21 | 8.25 ± 1.66 | 7.35 ± 1.23 | <0.01 |
| Distance (m) | Post-6MWT | 390.65 ± 43.62 | 382.73 ± 49.560 | 383.80 ± 68.36 | 0.78 |
| Variables | Duration | No Mask | Surgical Mask | Cloth Mask | p-Value |
|---|---|---|---|---|---|
| Heart rate (bpm) | Rest | 76.33 ± 8.29 | 77.55 ± 5.55 | 77.73 ± 8.23 | 0.90 |
| 6MWT | 81.60 ± 10.77 | 84.10 ± 11.42 | 83.08 ± 12.02 | ||
| Respiratory rate (breaths per minute) | Rest | 17.33 ± 1.97 | 18.78 ± 2.98 | 18.95 ± 2.90 | 0.65 |
| 6MWT | 22.25 ± 2.98 | 23.13 ± 3.15 | 22.98 ± 4.10 | ||
| Systolic blood pressure (mmHg) | Rest | 141.20 ± 9.01 | 142.88 ± 6.27 | 140.87 ± 7.00 | 0.46 |
| 6MWT | 140.00 ± 10.43 | 138.78 ± 11.92 | 140.20 ± 10.34 | ||
| Diastolic blood pressure (mmHg) | Rest | 76.53 ± 7.38 | 77.55 ± 6.06 | 76.95 ± 6.52 | 0.79 |
| 6MWT | 81.68 ± 8.92 | 81.38 ± 9.23 | 80.48 ± 8.71 | ||
| SpO2 (%) | Rest | 98.10 ± 0.90 | 97.98 ± 0.86 | 97.98 ± 0.73 | 0.35 |
| 6MWT | 97.50 ± 1.09 | 97.83 ± 1.15 | 97.68 ± 1.16 | ||
| RPE | Rest | 6.00 ± 0.00 | 6.15 ± 0.43 | 6.32 ± 0.62 | 0.01 |
| 6MWT | 7.02 ± 1.21 | 7.35 ± 1.23 | 8.25 ± 1.66 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amput, P.; Wongphon, S. Effects of Wearing Face Masks on Cardiorespiratory Parameters at Rest and after Performing the Six-Minute Walk Test in Older Adults. Geriatrics 2022, 7, 62. https://doi.org/10.3390/geriatrics7030062
Amput P, Wongphon S. Effects of Wearing Face Masks on Cardiorespiratory Parameters at Rest and after Performing the Six-Minute Walk Test in Older Adults. Geriatrics. 2022; 7(3):62. https://doi.org/10.3390/geriatrics7030062
Chicago/Turabian StyleAmput, Patchareeya, and Sirima Wongphon. 2022. "Effects of Wearing Face Masks on Cardiorespiratory Parameters at Rest and after Performing the Six-Minute Walk Test in Older Adults" Geriatrics 7, no. 3: 62. https://doi.org/10.3390/geriatrics7030062
APA StyleAmput, P., & Wongphon, S. (2022). Effects of Wearing Face Masks on Cardiorespiratory Parameters at Rest and after Performing the Six-Minute Walk Test in Older Adults. Geriatrics, 7(3), 62. https://doi.org/10.3390/geriatrics7030062






