A Narrative Review of Specialist Parkinson’s Nurses: Evolution, Evidence and Expectation
Abstract
1. Introduction
2. Methods
3. Results
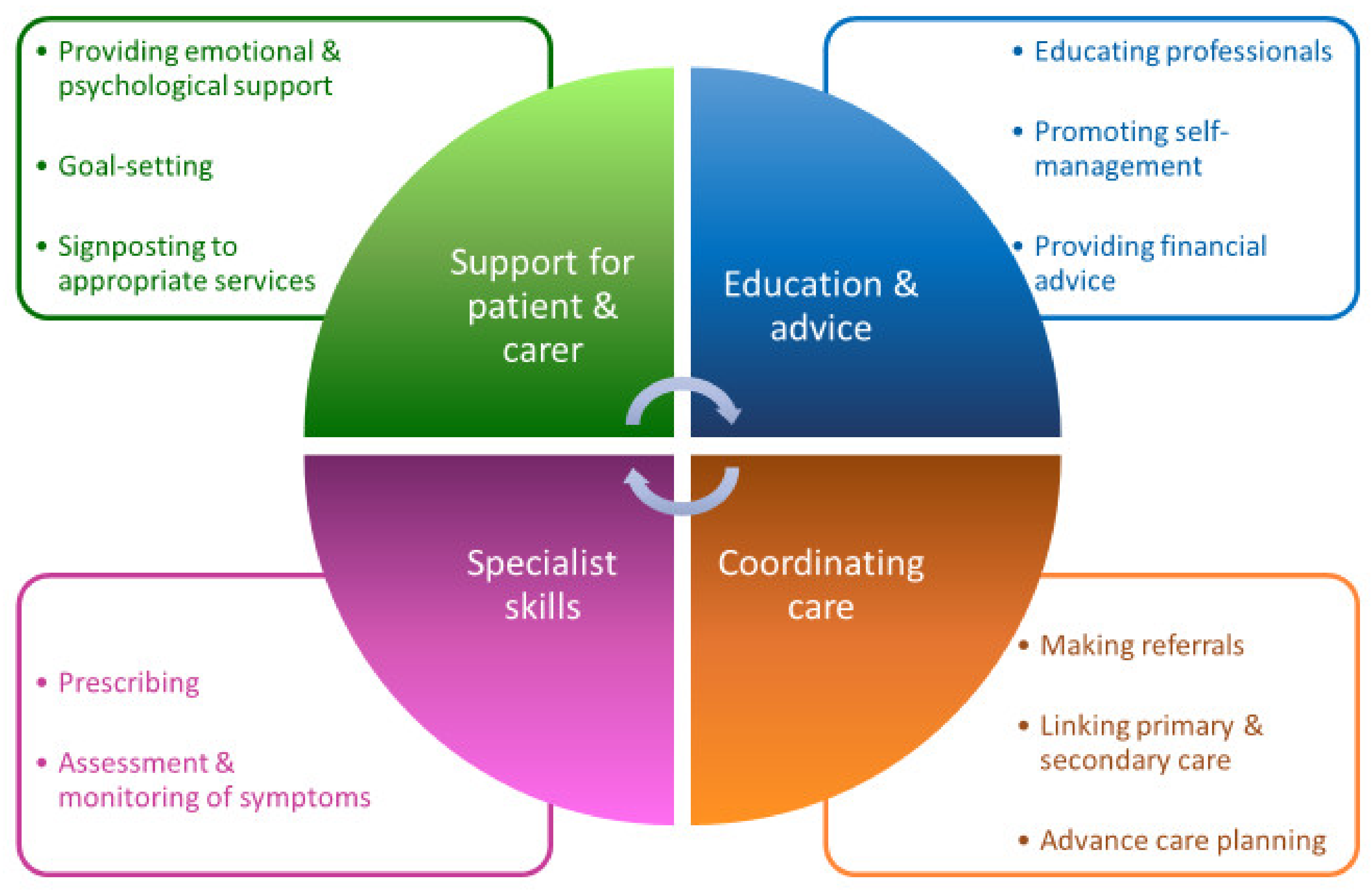
3.1. The Role of a Parkinson’s Disease Nurse Specialist
3.2. The Evidence for Effectiveness
3.3. International Implementation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Htay, M.; Whitehead, D. The Effectiveness of the Role of Advanced Nurse Practitioners Compared to Physician-Led or Usual Care: A Systematic Review. Int. J. Nurs. Stud. Adv. 2021, 3, 100034. [Google Scholar] [CrossRef]
- MacMahon, D.G.; Thomas, S. Practical approach to quality of life in Parkinson’s disease: The nurse’s role. J. Neurol. 1998, 245, S19–S22. [Google Scholar] [CrossRef] [PubMed]
- Reiter, F. The nurse-clinician. Am. J. Nurs. 1966, 66, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Montemuro, M.A. The evolution of the clinical nurse specialist: Response to the challenge of professional nursing practice. Clin. Nurse Spec. 1987, 1, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Tang, P. Evaluation on Nurse Specialist Pilot Scheme: Draft Report; Hospital Authority Head Office, Nursing Section: Hong Kong, China, 1993. [Google Scholar]
- Cooper, M.A.; McDowell, J.; Raeside, L.; ANP–CNS Group. The similarities and differences between advanced nurse practitioners and clinical nurse specialists. Br. J. Nurs. 2019, 28, 1308–1314. [Google Scholar] [CrossRef]
- Bird, H.A. Divided rheumatological care: The advent of the nurse practitioner? Ann. Rheum. Dis. 1983, 42, 354–355. [Google Scholar] [CrossRef]
- Akiboye, F.; Sihre, H.K.; Al Mulhem, M.; Rayman, G.; Nirantharakumar, K.; Adderley, N.J. Impact of diabetes specialist nurses on inpatient care: A systematic review. Diabet. Med. 2021, 38, e14573. [Google Scholar] [CrossRef]
- Naik, P. Multiple sclerosis specialist nursing in the UK: Results from the 2021 MS Trust nurse mapping survey. Br. J. Neurosci. Nurs. 2022, 18, 47–50. [Google Scholar] [CrossRef]
- Lempp, H.; Baggott, R.; Scott, D.L.; Parker, L.; Bosworth, A.; Georgopoulou, S.; Firth, J. The value, impact and role of nurses in rheumatology outpatient care: Critical review of the literature. Musculoskelet. Care 2020, 18, 245–255. [Google Scholar] [CrossRef]
- GBD 2015 Neurological Disorders Collaborator Group. Global, regional, and national burden of neurological disorders during 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017, 16, 877–897. [Google Scholar] [CrossRef]
- GBD 2016 Parkinson’s Disease Collaborators. Global. regional, and national burden of Parkinson’s disease, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018, 17, 939–953. [Google Scholar] [CrossRef]
- Understanding Parkinson’s-Statistics. Parkinson’ Disease Foundation. Available online: https://www.parkinson.org/Understanding-Parkinsons/Statistics (accessed on 24 February 2022).
- Schrag, A.; Jahanshahi, M.; Quinn, N. What contributes to quality of life in patients with Parkinson’s disease? J. Neurol. Neurosurg. Psychiatry 2000, 69, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Rahman, S.; Griffin, H.J.; Quinn, N.P.; Jahanshahi, M. Quality of life in Parkinson’s disease: The relative importance of the symptoms. Mov. Disord. 2008, 23, 1428–1434. [Google Scholar] [CrossRef] [PubMed]
- Bhidayasiri, R.; Panyakaew, P.; Trenkwalder, C.; Jeon, B.; Hattori, N.; Jagota, P.; Wu, Y.R.; Moro, E.; Lim, S.Y.; Shang, H.; et al. Delivering patient-centered care in Parkinson’s disease: Challenges and consensus from an international panel. Parkinsonism Relat. Disord. 2020, 72, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Research Unit RCoP. Standards of Care for Patients with Neurological Disease. A Consensus; Report of a Working Group; Research Unit RCoP: London, UK, 1990; Volume 24, pp. 90–97. [Google Scholar]
- Tribute Paid to UK’s First Parkinson’s Specialist Nurse Nursing Times. 2015. Available online: https://www.nursingtimes.net/clinical-archive/neurology/tribute-paid-to-uks-first-parkinsons-specialist-nurse-17-09-2015/ (accessed on 24 February 2022).
- Surendranath, S. Parkinson’s nurses: A light in the darkness. Nurs. Older People 2014, 26, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, H.; Wilson-Barnett, J.; Richardson, G. Evaluation of the role of the Parkinson’s disease nurse specialist. Int. J. Nurs. Stud. 2000, 37, 337–349. [Google Scholar] [CrossRef]
- Titova, N.; Chaudhuri, K.R. Personalized medicine in Parkinson’s disease: Time to be precise. Mov. Disord. 2017, 32, 1147–1154. [Google Scholar] [CrossRef]
- Gibson, G. What can the treatment of Parkinson’s disease learn from dementia care; Applying a bio-psycho-social approach to Parkinson’s disease. Int. J. Older People Nurs. 2017, 12, e12159. [Google Scholar] [CrossRef]
- Calne, S. Nursing care of patients with idiopathic parkinsonism. Nurs. Times 1994, 90, 38–39. [Google Scholar]
- Competencies: A Competency Framework for Nurses Working in Parkinson’s Disease Management Parkinson’s UK2016 [3rd Edition]. Available online: https://www.parkinsons.org.uk/professionals/resources/competency-framework-nurses-working-parkinsons-disease-management-3rd (accessed on 24 February 2022).
- Noble, C. Parkinson’s disease and the role of nurse specialists. Elder Care 1998, 10, 43–44. [Google Scholar] [CrossRef] [PubMed]
- Whitehouse, C. A new source of support. The nurse practitioner role in Parkinson’s disease and dystonia. Prof. Nurse 1994, 9, 448–450. [Google Scholar] [PubMed]
- Van der Eijk, M.; Faber, M.J.; Al Shamma, S.; Munneke, M.; Bloem, B.R. Moving towards patient-centered healthcare for patients with Parkinson’s disease. Parkinsonism Relat. Disord. 2011, 17, 360–364. [Google Scholar] [CrossRef] [PubMed]
- Greenwell, K.; Gray, W.K.; van Wersch, A.; van Schaik, P.; Walker, R. Predictors of the psychosocial impact of being a carer of people living with Parkinson’s disease: A systematic review. Parkinsonism Relat. Disord. 2015, 21, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Vlaanderen, F.P.; Rompen, L.; Munneke, M.; Stoffer, M.; Bloem, B.R.; Faber, M.J. The Voice of the Parkinson Customer. J. Park. Dis. 2019, 9, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Hellqvist, C.; Bertero, C. Support supplied by Parkinson’s disease specialist nurses to Parkinson’s disease patients and their spouses. Appl. Nurs. Res. 2015, 28, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Jahanshahi, M.; Brown, R.G.; Whitehouse, C.; Quinn, N.; Marsden, C.D. Contact with a Nurse Practitioner: A Short-Term Evaluation Study in Parkinson’s Disease and Dystonia. Behav. Neurol. 1994, 7, 189–196. [Google Scholar] [CrossRef]
- Kessler, D.; Hauteclocque, J.; Grimes, D.; Mestre, T.; Côtéd, D.; Liddy, C. Development of the Integrated Parkinson’s Care Network (IPCN): Using co-design to plan collaborative care for people with Parkinson’s disease. Qual. Life Res. 2019, 28, 1355–1364. [Google Scholar] [CrossRef]
- Bhidayasiri, R.; Boonpang, K.; Jitkritsadakul, O.; Calne, S.M.; Henriksen, T.; Trump, S.; Chaiwong, S.; Susang, P.; Boonrod, N.; Sringean, J.; et al. Understanding the role of the Parkinson’s disease nurse specialist in the delivery of apomorphine therpy. Parkinsonism Relat. Disord. 2016, 33 (Suppl. 1), S49–S55. [Google Scholar] [CrossRef]
- Pedersen, S.W.; Suedmeyer, M.; Liu, L.W.C.; Domagk, D.; Forbes, A.; Bergmann, L.; Onuk, K.; Yegin, A.; van Laar, T. The role and structure of the multidisciplinary team in the management of advanced Parkinson’s disease with a focus on the use of levodopa–carbidopa intestinal gel. J. Multidiscip. Health 2017, 10, 13–27. [Google Scholar] [CrossRef]
- Jarman, B.; Hurwitz, B.; Cook, A.; Bajekal, M.; Lee, A. Effects of community based nurses specialising in Parkinson’s disease on health outcome and costs: Randomised controlled trial. BMJ 2002, 324, 1072–1075. [Google Scholar] [CrossRef]
- Connor, K.I.; Cheng, E.M.; Barry, F.; Siebens, H.C.; Lee, M.L.; Ganz, D.A.; Mittman, B.S.; Connor, M.K.; Edwards, L.K.; McGowan, M.G.; et al. Randomized trial of care management to improve Parkinson disease care quality. Neurology 2019, 92, e1831–e1842. [Google Scholar] [CrossRef] [PubMed]
- Hurwitz, B.; Jarman, B.; Cook, A.; Bajekal, M. Scientific evaluation of community-based Parkinson’s disease nurse specialists on patient outcomes and health care costs. J. Eval. Clin. Pract. 2005, 11, 97–110. [Google Scholar] [CrossRef] [PubMed]
- Connor, K.; Cheng, E.; Siebens, H.C.; Lee, M.L.; Mittman, B.S.; Ganz, D.A.; Vickrey, B. Study protocol of “CHAPS”: A randomized controlled trial protocol of Care Coordination for Health Promotion and Activities in Parkinson’s Disease to improve the quality of care for individuals with Parkinson’s disease. BMC Neurol. 2015, 15, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Wagner, E.H. Organizing Care for Patients with Chronic Illness Revisited. Milbank Q. 2019, 97, 659–664. [Google Scholar] [CrossRef]
- Nurse Course. Parkinson’s Foundation. 2022. Available online: https://www.parkinson.org/expert-care/Professional-Education/Online-Courses/Nursing-Course (accessed on 24 February 2022).
- Edmond, J. Safra Visiting Nurse Faculty Program Parkinson’s Foundation. 2022. Available online: https://www.parkinson.org/expert-care/Professional-Education/Nurse-Faculty?_ga=2.194627629.180908347.1528722069-396416467.1479824002 (accessed on 24 February 2022).
- Standard for Practice: Parkinson’s Disease and Movement Disorder Nurse Specialists: Australasian Neuroscience Nurses’ Association (Movement Disorder Chapter). 2017. [First edition]. 2017. Available online: https://www.anna.asn.au/wp-content/uploads/PDMDNS-Standards-for-Practice-2017-09.pdf (accessed on 24 February 2022).
- Lee, J.M.; Shine, J.M.; Lewis, S.J. What matters to people with Parkinson’s disease living in Australia? J. Clin. Neurosci. 2015, 22, 338–341. [Google Scholar] [CrossRef]
- Parkinson’s Disease Services: Model of Care for the Older Person in Western Australia: Department of Health, State of Western Australia. 2008. Available online: https://ww2.health.wa.gov.au/~/media/Files/Corporate/general%20documents/Health%20Networks/Neurosciences%20and%20the%20Senses/Parkinsons-Disease-Model-of-Care.pdf (accessed on 24 February 2022).
- Living with Parkinson’s Disease—Update. Deloitte Access Economics: Parkinson’s Australia. 2011. Available online: https://www2.deloitte.com/au/en/pages/economics/articles/living-with-parkinsons-disease.html (accessed on 24 February 2022).
- Australian Demographic Statistics Dec 2011 Australian Bureau of Statistics. 2011. Available online: https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/3101.0Main+Features1Dec%202011?OpenDocument= (accessed on 24 February 2022).
- Buetow, S.; Giddings, L.S.; Williams, L.; Nayar, S. Parkinson’s Society of New Zealand Members with Parkinson’s D. Perceived unmet needs for health care among Parkinson’s Society of New Zealand members with Parkinson’s disease. Parkinsonism Relat. Disord. 2008, 14, 495–500. [Google Scholar] [CrossRef]
- Stocchi, F.; Bloem, B.R. Move for Change Part II: A European survey evaluating the impact of the EPDA Charter for people with Parkinson’s disease. Eur. J. Neurol. 2013, 20, 461–472. [Google Scholar] [CrossRef]
- Neurology Atlas: Country Resources for Neurological Disorders: World Health Organisation. 2004. Available online: https://apps.who.int/iris/handle/10665/43075 (accessed on 24 February 2022).
- Dotchin, C.; Msuya, O.; Kissima, J.; Massawe, J.; Mhina, A.; Moshy, A.; Aris, E.; Jusabani, A.; Whiting, D.; Masuki, G.; et al. The prevalence of Parkinson’s disease in rural Tanzania. Mov. Disord. 2008, 23, 1567–1672. [Google Scholar] [CrossRef]
- Williams, U.; Bandmann, O.; Walker, R. Parkinson’s Disease in Sub-Saharan Africa: A Review of Epidemiology, Genetics and Access to Care. J. Mov. Disord. 2018, 11, 53–64. [Google Scholar] [CrossRef]
- Mokaya, J.; Dotchin, C.L.; Gray, W.K.; Hooker, J.; Walker, R.W. The Accessibility of Parkinson’s Disease Medication in Kenya: Results of a National Survey. Mov. Disord. Clin. Pract. 2016, 3, 376–381. [Google Scholar] [CrossRef]
- Walker, R. Half the People in the World with Parkinson’s Disease Have Probably Not Been Diagnosed–Yet… British Geriatrics Society. 2017. Available online: https://www.bgs.org.uk/blog/half-the-people-in-the-world-with-parkinson%E2%80%99s-disease-have-probably-not-been-diagnosed%E2%80%A6 (accessed on 24 February 2022).
- Walker, R.; Ebeneezer, L.; Dotchin, C.; Hind, L.; Msuya, M.; Daniels, M. A Parkinson’s disease nurse specialist course for East Africa [abstract]. In Movement Disorders; Wiley-Blackwell: Hoboken, NJ, USA, 2013. [Google Scholar]
- International Parkinson and Movement Disorder Society. First African PD Nurse Specialist Course. 2012. Available online: https://www.movementdisorders.org/MDS/Regional-Sections/Sub-Saharan-Africa/First-African-PD-Nurse-Specialist-Course.htm (accessed on 24 February 2022).
- Walker, R. Parkinson’s Disease in Sub-Saharan Africa: Report from the Chair. International Parkinson and Movement Disorder Society. Available online: https://www.movementdisorders.org/MDS/About/Committees--Other-Groups/MDS-Task-Forces/Task-Force-on-Africa/Parkinsons-disease-in-sub-Saharan-Africa.htm (accessed on 24 February 2022).
- Chulalongkorn Centre of Excellence for Parkinson’s Disease & Related Disorders: Faculties and Staff; Parkinson Nurse Specialists and Officers. Available online: http://www.chulapd.org/en/about-us/2/ (accessed on 24 February 2022).
- Dotchin, C.; Jusabani, A.; Walker, R. Three year follow up of levodopa plus carbidopa treatment in a prevalent cohort of patients with Parkinson’s disease in Hai, Tanzania. J. Neurol. 2011, 258, 1649–1656. [Google Scholar] [CrossRef] [PubMed]
- Mshana, G.; Dotchin, C.L.; Walker, R.W. ‘We call it the shaking illness’: Perceptions and experiences of Parkinson’s disease in rural northern Tanzania. BMC Public Health 2011, 11, 219. [Google Scholar] [CrossRef] [PubMed]
- Cubo, E.; Doumbe, J.; Njiengwe, E.; Onana, P.; Garoña, R.; Alcalde, J.; Seco, J.; Mariscal, N.; Epundugu, B.M.; Cubo, S.; et al. A Parkinson’s disease tele-education program for health care providers in Cameroon. J. Neurol. Sci. 2015, 357, 285–287. [Google Scholar] [CrossRef]
- Connor, K.I.; Siebens, H.C.; Mittman, B.S.; Ganz, D.A.; Barry, F.; Ernst, E.J.; Edwards, L.K.; McGowan, M.G.; McNeese-Smith, D.K.; Cheng, E.M.; et al. Quality and extent of implementation of a nurse-led care management intervention: Care coordination for health promotion and activities in Parkinson’s disease (CHAPS). BMC Health Serv. Res. 2020, 20, 1–17. [Google Scholar] [CrossRef]
- Van der Marck, M.A.; Munneke, M.; Mulleners, W.; Hoogerwaard, E.M.; Borm, G.F.; Overeem, S.; Bloem, B.R.; IMPACT Study Group. Integrated multidisciplinary care in Parkinson’s disease: A non-randomised, controlled trial (IMPACT). Lancet Neurol. 2013, 12, 947–956. [Google Scholar] [CrossRef]
- Eggers, C.; Dano, R.; Schill, J.; Fink, G.R.; Hellmich, M.; Timmermann, L.; on behalf of the CPN Study Group. Patient-centered integrated healthcare improves quality of life in Parkinson’s disease patients: A randomized controlled trial. J. Neurol. 2018, 265, 764–773. [Google Scholar] [CrossRef] [PubMed]
- Radder, D.L.M.; Lennaerts, H.H.; Vermeulen, H.; van Asseldonk, T.; Delnooz, C.C.S.; Hagen, R.H.; Munneke, M.; Bloem, B.R.; de Vries, N.M. The cost-effectiveness of specialized nursing interventions for people with Parkinson’s disease: The NICE-PD study protocol for a randomized controlled clinical trial. Trials 2020, 21, 1–11. [Google Scholar] [CrossRef]
- Chen, Y.; Lu, T.; Jiang, X.; Huang, X. The effectiveness of specialized nursing interventions for patients with Parkinson disease: A randomized controlled study protocol. Medicine 2021, 100, e23972. [Google Scholar] [CrossRef]
- NICE. Clinical Guideline [NG71]. Parkinson’s Disease in Adults. 19 July 2017. Available online: https://www.nice.org.uk/guidance/ng71/resources/parkinsons-disease-in-adults-pdf-1837629189061 (accessed on 24 February 2022).
- UK Parkinson’s Audit: Summary Report: UK Parkinson’s Excellence Network. Available online: https://www.parkinsons.org.uk/sites/default/files/2020-01/CS3524%20Parkinson%27s%20UK%20Audit%20-%20Summary%20Report%202019%20%281%29.pdf (accessed on 24 February 2022).
- Parkinson’s UK. Parkinson’s nurses in Scotland: Providing Effective, Safe, Person-Centred Care. 2013. Available online: https://www.parkinsons.org.uk/sites/default/files/2017-12/scotlandnursereport.pdf (accessed on 24 February 2022).
- Axelrod, L.; Gage, H.; Kaye, J.; Bryan, K.; Trend, P.; Wade, D. Workloads of Parkinson’s specialist nurses: Implications for implementing national service guidelines in England. J. Clin. Nurs. 2010, 19, 3575–3580. [Google Scholar] [CrossRef]
- Protect Parkinson’s Nurses in England and Save the NHS Money: Parkinson’s UK. 2011. Available online: https://cdn.ps.emap.com/wp-content/uploads/sites/3/2011/07/ProtectParkinsonsnursesEngland.pdf (accessed on 24 February 2022).
- Brown, S.; Dalkin, S.M.; Bate, A.; Bradford, R.; Allen, C.; Brittain, K.; Clarke, A.; Hand, A. Exploring and understanding the scope and value of the Parkinson’s nurse in the UK (The USP Project): A realist economic evaluation protocol. BMJ Open 2020, 10, e037224. [Google Scholar] [CrossRef]


| Author | Year | Duration (months) | Setting | Study Arms | Participants | Outcome Measure(s) | Key Findings (Intervention Group vs. Control) | |
|---|---|---|---|---|---|---|---|---|
| Number Enrolled | Mean Age (yrs) | |||||||
| Jahanshahi et al. [31] | 1994 | 6 | 1 tertiary centre in England | Intervention 2. home visits and 5 telephone contacts with a nurse practitioner Control No contact with nurse practitioner (1:1 randomisation) | 40 (PD) | 63.7 | -9 psychosocial measures assessed via a set of self-completed questionnaires (including BDI, STAI, AIS) -7 questions to assess patient satisfaction | 7 contacts with a nurse practitioner: -did not appear to positively or negatively impact psychological wellbeing. -was highly valued by patients. -led to a high rate of referrals to other health care professionals |
| Reynolds et al. [20] | 2000 | 12 | 3 UK outpatient clinics | Intervention Hospital-based PDNS care only (group B) or predominantly PDNS with Consultant neurologist follow-up (2 to 5 contacts during the study period) (group C) Control (group A) Consultant follow-up care only (Randomisation according to ‘established pattern of care’ at each centre) | 185 | Group A: 65.1 B: 68.5 C: 67.6 | -Health state assessed via 6 questionnaires (HADS, SF-36, PDQ-39, Functional Disability Scale, Patient and Carer Satisfaction Survey, Social requirements), from which 22 dimensions were derived -Healthcare costs | -PDNSs led to similar outcomes but at increased cost -Medical and nursing specialists valued the complementary expertise of PDNSs |
| Jarman et al. [35] | 2002 | 24 | 9 regions of England (community-based) | Intervention Community-based care from a nurse specialist who advised GP (8 nurse-led assessments per year on average). Control Standard care from GP (Randomisation within practices with variable randomisation ratio to equate workload) | 1859 | Approx. 1/3 in each group: 18– 70, 71–77, > 77 | Primary outcomes -Objective health measures (stand up test, dot in square score, mortality, proportion sustaining fracture) -Patient wellbeing (PDQ-39, EuroQoL; global subjective wellbeing question) -Healthcare costs Secondary outcomes Medication; Referrals | -Little effect on the objective health measures -Improved sense of wellbeing with no increase in healthcare costs |
| Connor et al. [36] | 2019 | 24 | 5 medical centres in the U.S.A. | Intervention A coordinated, nurse-led, chronic care management intervention Control Usual outpatient care (1:1 randomisation at patient level) | 328 | 71.0 | Primary outcome: adherence to 38 quality of care indicators Secondary outcomes: Health-related quality of life; perceptions of care quality (structured telephone survey interviews) Healthcare costs | -Improved adherence to PD quality of care indicators -Moderate evidence of a reduction in depressive symptoms (PHQ-2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tenison, E.; James, A.; Ebenezer, L.; Henderson, E.J. A Narrative Review of Specialist Parkinson’s Nurses: Evolution, Evidence and Expectation. Geriatrics 2022, 7, 46. https://doi.org/10.3390/geriatrics7020046
Tenison E, James A, Ebenezer L, Henderson EJ. A Narrative Review of Specialist Parkinson’s Nurses: Evolution, Evidence and Expectation. Geriatrics. 2022; 7(2):46. https://doi.org/10.3390/geriatrics7020046
Chicago/Turabian StyleTenison, Emma, Alice James, Louise Ebenezer, and Emily J. Henderson. 2022. "A Narrative Review of Specialist Parkinson’s Nurses: Evolution, Evidence and Expectation" Geriatrics 7, no. 2: 46. https://doi.org/10.3390/geriatrics7020046
APA StyleTenison, E., James, A., Ebenezer, L., & Henderson, E. J. (2022). A Narrative Review of Specialist Parkinson’s Nurses: Evolution, Evidence and Expectation. Geriatrics, 7(2), 46. https://doi.org/10.3390/geriatrics7020046






