Safety of Total Knee Arthroplasty without Using a Tourniquet in Elderly Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Surgical Procedures
2.3. Data Collection
2.4. Statistical Analyses
3. Results
3.1. Patient Background
3.2. Perioperative Data
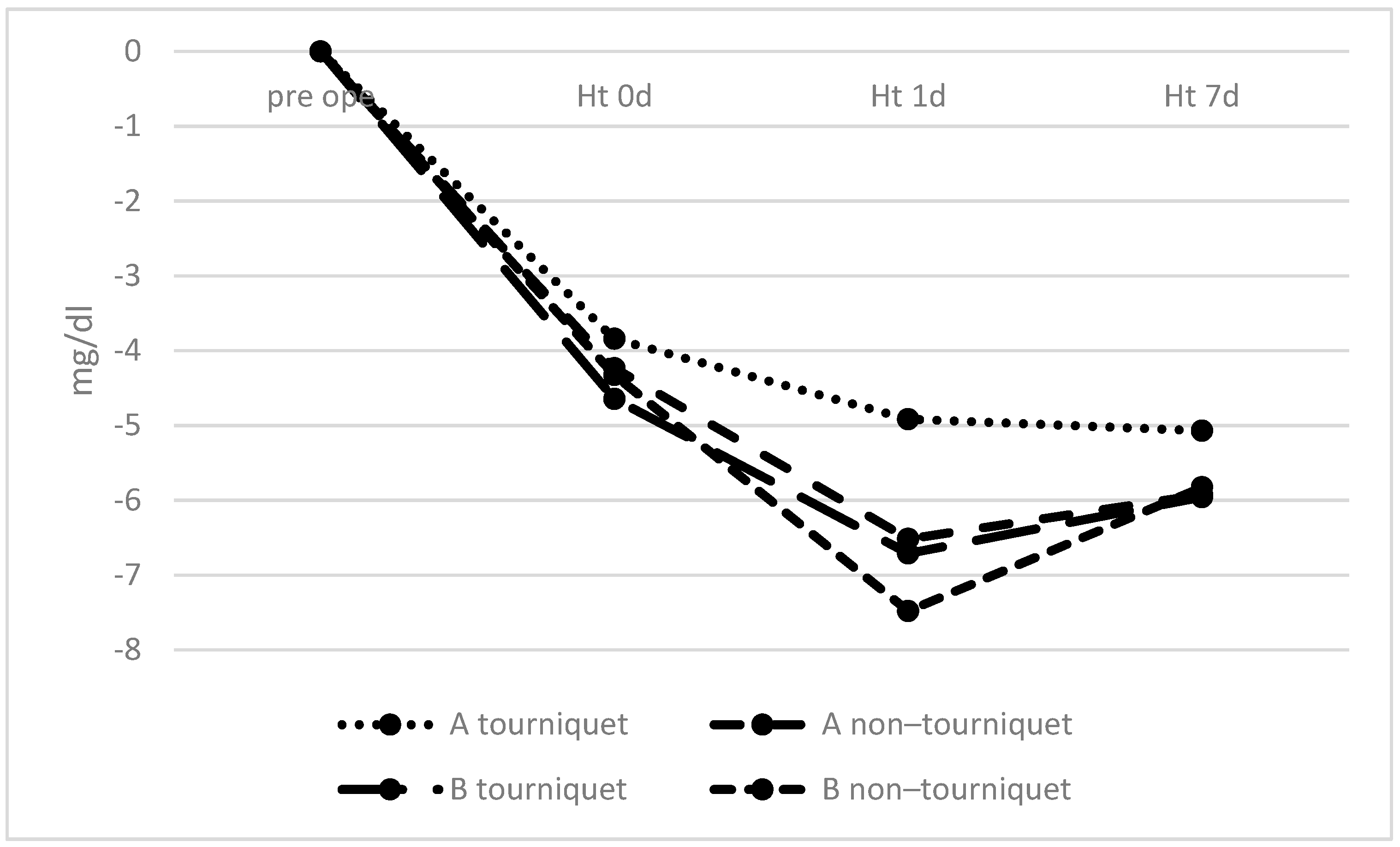
3.3. Changes in Hematological Data
3.4. Complications
3.5. Clinical Evaluations
3.6. Correlation with Age
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Austin, D.C.; Torchia, M.T.; Moschetti, W.E.; Jevsevar, D.S.; Keeney, B.J. Patient outcomes after total knee arthroplasty in patients older than 80 years. J. Arthroplast. 2018, 33, 3465–3473. [Google Scholar] [CrossRef]
- Murphy, B.P.D.; Dowsey, M.M.; Spelman, T.; Choong, P.F.M. The impact of older age on patient outcomes following primary total knee arthroplasty. Bone Jt. J. 2018, 100-B, 1463–1470. [Google Scholar] [CrossRef]
- Fang, M.; Noiseux, N.; Linson, E.; Cram, P. The effect of advancing age on total Joint replacement outcomes. Geriatr. Orthop. Surg. Rehabil. 2015, 6, 173–179. [Google Scholar] [CrossRef]
- Klasan, A.; Putnis, S.E.; Yeo, W.W.; Fritsch, B.A.; Coolican, M.R.; Parker, D.A. Advanced age is not a barrier to total knee arthroplasty: A detailed analysis of outcomes and complications in an elderly cohort compared with average age total knee arthroplasty patients. J. Arthroplast. 2019, 34, 1938–1945. [Google Scholar] [CrossRef]
- Goel, R.; Rondon, A.J.; Sydnor, K.; Blevins, K.; O’Malley, M.; Purtill, J.J.; Austin, M.S. Tourniquet use does not affect functional outcomes or pain after total knee arthroplasty: A prospective, double-blinded, randomized controlled trial. J. Bone Jt. Surg. Am. 2019, 101, 1821–1828. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, I.; Chawla, A.; Underwood, M.; Price, A.J.; Metcalfe, A.; Hutchinson, C.E.; Warwick, J.; Seers, K.; Parsons, H.; Wall, P.D.H. Time to reconsider the routine use of tourniquets in total knee arthroplasty surgery. Bone Jt. J. 2021, 103-B, 830–839. [Google Scholar] [CrossRef] [PubMed]
- Nadler, S.B.; Hidalgo, J.H.; Bloch, T. Prediction of blood volume in normal human adults. Surgery 1962, 51, 224–232. [Google Scholar] [PubMed]
- The Seventh Annual Report of the American Joint Replacement Registry on Hip and Knee Arthroplasty; AAOS: Rosemont, IL, USA, 2020; 101p, Available online: http://connect.ajrr.net/2020-ajrr-annual-report (accessed on 21 July 2021).
- The 17th Annual Report of National Joint Registry 2020 NJR; 309p, Available online: https://reports.njrcentre.org.uk (accessed on 21 July 2021).
- Annual Report. Swedish Knee Arthroplasty Register; Lund, Sweden, 2020; 99p, Available online: https://www.myknee.se/en/ (accessed on 21 July 2021).
- Annual Report. Australian Orthopaedic Association National Joint Replacement Registry AOA; Adelade, SA, Australia, 2020; 468p, Available online: https://aoanjrr.sahmri.com/annual-reports-2020 (accessed on 21 July 2021).
- Zhou, Q.; Zhou, Y.; Wu, H.; Wu, Y.; Qian, Q.; Zhao, H.; Zhu, Y.; Fu, P. Changes of hemoglobin and hematocrit in elderly patients receiving lower joint arthroplasty without allogeneic blood transfusion. Chin. Med. J. 2015, 128, 75–78. [Google Scholar] [CrossRef]
- Ozkunt, O.; Sariyilmaz, K.; Gemalmaz, H.C.; Dikici, F. The effect of tourniquet usage on cement penetration in total knee arthroplasty: A prospective randomized study of 3 methods. Medicine 2018, 97, e9668. [Google Scholar] [CrossRef] [PubMed]
- Alexandersson, M.; Wang, E.Y.; Eriksson, S. A small difference in recovery between total knee arthroplasty with and without tourniquet use the first 3 months after surgery: A randomized controlled study. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1035–1042. [Google Scholar] [CrossRef]
- Ejaz, A.; Laursen, A.C.; Jakobsen, T.; Rasmussen, S.; Nielsen, P.T.; Laursen, M.B. Absence of a tourniquet does not affect fixation of cemented TKA: A randomized RSA study of 70 patients. J. Arthroplast. 2015, 30, 2128–2132. [Google Scholar] [CrossRef]
- Jawhar, A.; Stetzelberger, V.; Kollowa, K.; Obertacke, U. Tourniquet application does not affect the periprosthetic bone cement penetration in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2071–2081. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Song, M.; Chen, J.; Li, C.; Lin, W.; Ye, G.; Wu, G.; Li, A.; Cai, Y.; Wu, H.; et al. Does tourniquet use affect the periprosthetic bone cement penetration in total knee arthroplasty? A meta-analysis. J. Orthop. Surg. Res. 2020, 15, 602. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, I.; Chawla, A.; Underwood, M.; Price, A.J.; Metcalfe, A.; Hutchinson, C.; Warwick, J.; Seers, K.; Parsons, H.; Wall, P.D. Tourniquet use for knee replacement surgery. Cochrane Database Syst. Rev. 2020, 12, CD012874. [Google Scholar] [CrossRef][Green Version]
- Jawhar, A.; Skeirek, D.; Stetzelberger, V.; Kollowa, K.; Obertacke, U. No effect of tourniquet in primary total knee arthroplasty on muscle strength, functional outcome, patient satisfaction and health status: A randomized clinical trial. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 1045–1054. [Google Scholar] [CrossRef] [PubMed]
- Hasanain, M.S.; Apostu, D.; Alrefaee, A.; Tarabichi, S. Comparing the effect of tourniquet vs tourniquet-less in simultaneous bilateral total knee arthroplasties. J. Arthroplast. 2018, 33, 2119–2124. [Google Scholar] [CrossRef]
- Palanne, R.; Rantasalo, M.; Vakkuri, A.; Madanat, R.; Olkkola, K.T.; Lahtinen, K.; Reponen, E.; Linko, R.; Vahlberg, T.; Skants, N. Effects of anaesthesia method and tourniquet use on recovery following total knee arthroplasty: A randomised controlled study. Br. J. Anaesth. 2020, 125, 762–772. [Google Scholar] [CrossRef]
- Ledin, H.; Aspenberg, P.; Good, L. Tourniquet use in total knee replacement does not improve fixation, but appears to reduce final range of motion. Acta Orthop. 2012, 83, 499–503. [Google Scholar] [CrossRef]
- Wang, K.; Ni, S.; Li, Z.; Zhong, Q.; Li, R.; Li, H.; Ke, Y.; Lin, J. The effects of tourniquet use in total knee arthroplasty: A randomized, controlled trial. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2849–2857. [Google Scholar] [CrossRef]
- Fan, Y.; Jin, J.; Sun, Z.; Li, W.; Lin, J.; Weng, X.; Qiu, G. The limited use of a tourniquet during total knee arthroplasty: A randomized controlled trial. Knee 2014, 21, 1263–1268. [Google Scholar] [CrossRef]
- Huang, Z.Y.; Pei, F.X.; Ma, J.; Yang, J.; Zhou, Z.K.; Kang, P.D.; Shen, B. Comparison of three different tourniquet application strategies for minimally invasive total knee arthroplasty: A prospective non-randomized clinical trial. Arch. Orthop. Trauma Surg. 2014, 134, 561–570. [Google Scholar] [CrossRef] [PubMed]
- Kvederas, G.; Porvaneckas, N.; Andrijauskas, A.; Svensen, C.H.; Ivaskevicius, J.; Mazunaitis, J.; Marmaite, U.; Andrijauskas, P. A randomized double-blind clinical trial of tourniquet application strategies for total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2790–2799. [Google Scholar] [CrossRef] [PubMed]

| Variables | Group A (Age < 76), n = 56 | Group B (Age ≥ 76), n = 47 | ||
|---|---|---|---|---|
| Tourniquet group | use, n = 29 | no use, n = 27 | use, n = 23 | no use, n = 24 |
| Age, years | 68.4 ± 6.6 | 69.6 ± 5.4 | 80.1 ± 3.7 | 80.6 ± 3.2 |
| Sex, male/female | 4/25 | 5/22 | 1/22 | 4/20 |
| Body height, cm | 152.5 ± 7.7 | 155.8 ± 8.0 | 146.4 ± 7.3 | 151.5 ± 6.9 |
| Body weight, kg | 61.4 ± 13.5 | 64.4 ± 10.8 | 52.8 ± 8.1 | 56.0 ± 7.8 |
| ASA, median [IQR] | 2 (1–2) | 2 (1–2) | 2 (2–2) | 2 (2–2) |
| Antiplatelet agents | 2/29 (6.9%) | 2/27 (7.4%) | 0/23 (0%) | 0/24 (0%) |
| Variables | Group A (Age < 76) | Group B (Age ≥ 76) | ANOVA p Value | ||
|---|---|---|---|---|---|
| Tourniquet Group | Use | No Use | Use | No Use | |
| Operation time, min | 92.0 ± 15.8 * | 99.8 ± 19.2 | 88.6 ± 15.1 † | 108.6 ± 32.5 *,† | 0.009 |
| Perioperative blood loss, mL | 179.2 ± 113.3 § | 261.0 ± 127.2 § | 183.4 ± 85.3 | 204.0 ± 96.5 | 0.046 |
| Estimated blood loss, mL | 391.4 ± 151.1 | 389.7 ± 178.6 | 393.3 ± 225.2 | 345.7 ± 165.6 | 0.770 |
| Transfusions | 29/29 (100%) | 26/27 (96.4%) | 22/23 (95.5%) | 22/24 (91.7%) | 0.466 |
| Variables | Group A (Age < 76) | Group B (Age ≥ 76) | ANOVA p Value | ||
|---|---|---|---|---|---|
| Tourniquet Group | Use | No Use | Use | No Use | |
| ROM (preoperative), extension | 10.2 ± 10.0 | 4.9 ± 8.3 | 6.7 ± 5.6 | 6.2 ± 8.8 | 0.126 |
| ROM (preoperative), flexion | 126.8 ± 14.6 | 116.9 ± 27.5 | 118.7 ± 22.0 | 122.1 ± 15.2 | 0.307 |
| ROM (4 weeks), extension | 3.3 ± 5.2 | 2.0 ± 3.5 | 1.7 ± 3.6 | 2.1 ± 4.1 | 0.529 |
| ROM (4 weeks), flexion | 106.9 ± 13.5 | 109.0 ± 17.4 | 109.6 ± 9.4 | 110.6 ± 8.6 | 0.756 |
| KS score (preoperative), point | 52.3 ± 4.7 | 54.6 ± 10.1 | 49.3 ± 5.8 | 50.0 ± 7.6 | 0.054 |
| KS score (4 weeks), point | 74.6 ± 5.8 | 75.6 ± 6.5 | 72.7 ± 6.3 | 75.2 ± 5.4 | 0.355 |
| Age | Pearson’s Correlation Coefficient (r) |
|---|---|
| vs. Height | −0.269 |
| vs. Weight | −0.400 |
| vs. KS score (pre) | −0.255 |
| vs. change in Hb (1 d) | −0.281 |
| vs. change in Hb (7 d) | −0.22 |
| vs. change in Ht (1 d) | −0.295 |
| vs. change in Ht (7 d) | −0.220 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miyamoto, S.; Kosugi, M.; Sasaki, S.; Okazaki, K. Safety of Total Knee Arthroplasty without Using a Tourniquet in Elderly Patients. Geriatrics 2021, 6, 100. https://doi.org/10.3390/geriatrics6040100
Miyamoto S, Kosugi M, Sasaki S, Okazaki K. Safety of Total Knee Arthroplasty without Using a Tourniquet in Elderly Patients. Geriatrics. 2021; 6(4):100. https://doi.org/10.3390/geriatrics6040100
Chicago/Turabian StyleMiyamoto, Satoshi, Masahide Kosugi, Shin Sasaki, and Ken Okazaki. 2021. "Safety of Total Knee Arthroplasty without Using a Tourniquet in Elderly Patients" Geriatrics 6, no. 4: 100. https://doi.org/10.3390/geriatrics6040100
APA StyleMiyamoto, S., Kosugi, M., Sasaki, S., & Okazaki, K. (2021). Safety of Total Knee Arthroplasty without Using a Tourniquet in Elderly Patients. Geriatrics, 6(4), 100. https://doi.org/10.3390/geriatrics6040100






