Feasibility and Adoption of a Focused Digital Wellness Program in Older Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and App Design
2.2. Study Measures
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Meskó, B.; Drobni, Z.; Bényei, É.; Gergely, B.; Győrffy, Z. Digital health is a cultural transformation of traditional healthcare. mHealth 2017, 3, 38. [Google Scholar] [CrossRef] [Green Version]
- Liu, F.; Zhao, S.; Li, Y. How many, how often, and how new? A multivariate profiling of mobile app users. J. Retail. Consum. Serv. 2017, 38, 71–80. [Google Scholar] [CrossRef]
- Toro-Ramos, T.; Lee, D.-H.; Kim, Y.; Michaelides, A.; Oh, T.J.; Kim, K.M.; Jang, H.C.; Lim, S. Effectiveness of a Smartphone Application for the Management of Metabolic Syndrome Components Focusing on Weight Loss: A Preliminary Study. Metab. Syndr. Relat. Disord. 2017, 15, 465–473. [Google Scholar] [CrossRef] [PubMed]
- Castro, S.C.M.; Chiguluri, V.; Gumpina, R. Outcomes of a digital health program with human coaching for diabetes risk reduction in a Medicare population. J. Aging Health 2018, 30, 692–710. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelley, G.; McClellan, P. Antihypertensive effects of aerobic exercise: A brief meta-analytic review of randomized controlled trials. Am. J. Hypertens. 1994, 7, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Valencia, W.M.; Stoutenberg, M.; Florez, H. Weight loss and physical activity for disease prevention in obese older adults: An important role for lifestyle management. Curr. Diabetes Rep. 2014, 14, 539. [Google Scholar] [CrossRef] [PubMed]
- Buchner, D.M. Physical Activity and Prevention of Cardiovascular Disease in Older Adults. Clin. Geriatr. Med. 2009, 25, 661–675. [Google Scholar] [CrossRef]
- Brawley, L.; Rejeski, W.J.; Gaukstern, J.E.; Ambrosius, W.T. Social Cognitive Changes Following Weight Loss and Physical Activity Interventions in Obese, Older Adults in Poor Cardiovascular Health. Ann. Behav. Med. 2012, 44, 353–364. [Google Scholar] [CrossRef] [Green Version]
- Chen, J.; Cade, J.E.; Allman-Farinelli, M. The Most Popular Smartphone Apps for Weight Loss: A Quality Assessment. JMIR mHealth uHealth 2015, 3, e104. [Google Scholar] [CrossRef]
- Figueroa, C.A.; Aguilera, A. The Need for a Mental Health Technology Revolution in the COVID-19 Pandemic. Front. Psychiatry 2020, 11, 523. [Google Scholar] [CrossRef]
- Torous, J.; Roberts, L.W. Needed innovation in digital health and smartphone applications for mental health: Transparency and trust. JAMA Psychiatry 2017, 74, 437–438. [Google Scholar] [CrossRef] [PubMed]
- Platt, A.; Outlay, C.; Sarkar, P.; Karnes, S. Evaluating User Needs in Wellness Apps. Int. J. Human-Comput. Interact. 2016, 32, 119–131. [Google Scholar] [CrossRef]
- Reyes, A.; Qin, P.; Brown, C.A. A standardized review of smartphone applications to promote balance for older adults. Disabil. Rehabil. 2016, 40, 690–696. [Google Scholar] [CrossRef] [PubMed]
- Fortuna, K.L.; Lohman, M.C.; Gill, L.E.; Bruce, M.L.; Bartels, S.J. Adapting a Psychosocial Intervention for Smartphone Delivery to Middle-Aged and Older Adults with Serious Mental Illness. Am. J. Geriatr. Psychiatry 2017, 25, 819–828. [Google Scholar] [CrossRef] [PubMed]
- Evangelista, L.; Steinhubl, S.R.; Topol, E.J. Digital health care for older adults. Lancet 2019, 393, 1493. [Google Scholar] [CrossRef]
- Mohadisdudis, H.M.; Ali, N.M. A study of smartphone usage and barriers among the elderly. In Proceedings of the 2014 3rd International Conference on User Science and Engineering (i-USEr), Shah Alam, Malaysia, 2–5 September 2014; pp. 109–114. [Google Scholar]
- Zhou, J.; Rau, P.-L.P.; Salvendy, G. Older adults’ use of smart phones: An investigation of the factors influencing the acceptance of new functions. Behav. Inf. Technol. 2014, 33, 552–560. [Google Scholar] [CrossRef]
- Hall, A.K.; Bernhardt, J.M.; Dodd, V.; Vollrath, M.W. The digital health divide: Evaluating online health information access and use among older adults. Health Educ. Behav. 2015, 42, 202–209. [Google Scholar] [CrossRef] [Green Version]
- Hong, Y.A.; Cho, J. Has the Digital Health Divide Widened? Trends of Health-Related Internet Use among Older Adults from 2003 to 2011. J. Gerontol. Ser. B 2016, 72, 856–863. [Google Scholar] [CrossRef] [Green Version]
- Michaelides, A.; Raby, C.; Wood, M.; Farr, K.; Toro-Ramos, T. Weight loss efficacy of a novel mobile Diabetes Prevention Program delivery platform with human coaching. BMJ Open Diabetes Res. Care 2016, 4, e000264. [Google Scholar] [CrossRef] [Green Version]
- Sepah, S.C.; Jiang, L.; Ellis, R.J.; McDermott, K.; Peters, A.L. Engagement and outcomes in a digital Diabetes Prevention Program: 3-year update. BMJ Open Diabetes Res. Care 2017, 5, e000422. [Google Scholar] [CrossRef] [Green Version]
- Torous, J.; Michalak, E.E.; O’Brien, H.L. Digital Health and Engagement—Looking Behind the Measures and Methods. JAMA Netw. Open 2020, 3, e2010918. [Google Scholar] [CrossRef] [PubMed]
- Reichheld, F.F.; Covey, S.R. The Ultimate Question: Driving Good Profits and True Growth, 4th ed.; Harvard Business School Press: Boston, MA, USA, 2006. [Google Scholar]
- Hamilton, D.; Lane, J.V.; Gaston, P.; Patton, J.T.; MacDonald, D.J.; Simpson, A.H.R.W.; Howei, C.R. Assessing treatment outcomes using a single question: The net promoter score. Bone Jt. J. 2014, 96, 622–628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shanas, E. The Family as a Social Support System in Old Age. Gerontologist 1979, 19, 169–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, N.; Marvel, F.A.; Wang, J.; Martin, S.S. Digital Health Technologies to Promote Lifestyle Change and Adherence. Curr. Treat. Options Cardiovasc. Med. 2017, 19, 60. [Google Scholar] [CrossRef] [PubMed]
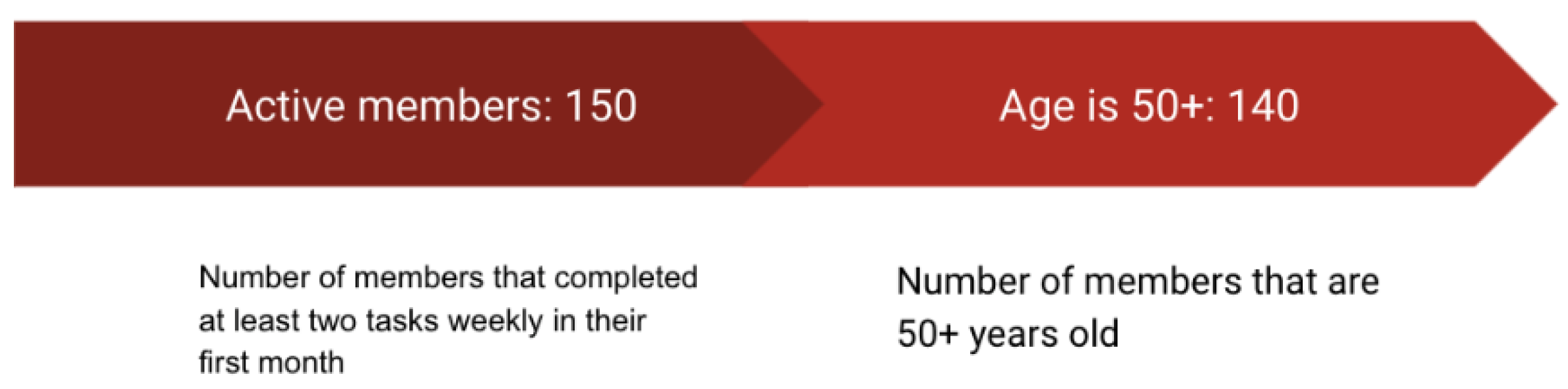
| Characteristic | n | Overall |
|---|---|---|
| Total Sample | 140 | |
| Age (in years) | Mean (59.82) median (60) | |
| Age (standard deviation) | 6.42 | |
| Age (range) | 50–80 | |
| Age Mode | 60 | |
| Female | 85 (61%) | |
| Male | 55 (39%) | |
| Active Users at 16 weeks (4 months) | 91 (65%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tam, E.; Boas, P.K.V.; Ruaro, F.; Flesch, J.; Wu, J.; Thomas, A.; Li, J.; Lopes, F. Feasibility and Adoption of a Focused Digital Wellness Program in Older Adults. Geriatrics 2021, 6, 54. https://doi.org/10.3390/geriatrics6020054
Tam E, Boas PKV, Ruaro F, Flesch J, Wu J, Thomas A, Li J, Lopes F. Feasibility and Adoption of a Focused Digital Wellness Program in Older Adults. Geriatrics. 2021; 6(2):54. https://doi.org/10.3390/geriatrics6020054
Chicago/Turabian StyleTam, Eric, Pedro Kondak Villas Boas, Fernando Ruaro, Juliane Flesch, Jennifer Wu, Amelia Thomas, James Li, and Felipe Lopes. 2021. "Feasibility and Adoption of a Focused Digital Wellness Program in Older Adults" Geriatrics 6, no. 2: 54. https://doi.org/10.3390/geriatrics6020054
APA StyleTam, E., Boas, P. K. V., Ruaro, F., Flesch, J., Wu, J., Thomas, A., Li, J., & Lopes, F. (2021). Feasibility and Adoption of a Focused Digital Wellness Program in Older Adults. Geriatrics, 6(2), 54. https://doi.org/10.3390/geriatrics6020054





