Rapid Support for Older Adults during the Initial Stages of the COVID-19 Pandemic: Results from a Geriatric Psychiatry Helpline
Abstract
1. Introduction
2. Materials and Methods
2.1. Establishment of a COVID-19 Helpline
2.2. Mental Health Status
2.2.1. Depression
2.2.2. Anxiety
2.3. Data Analysis
2.4. Ethics Approval and Consent to Participate
3. Results
3.1. I Demographics and Medical History
3.2. II Changes in Daily Life and Social Interaction
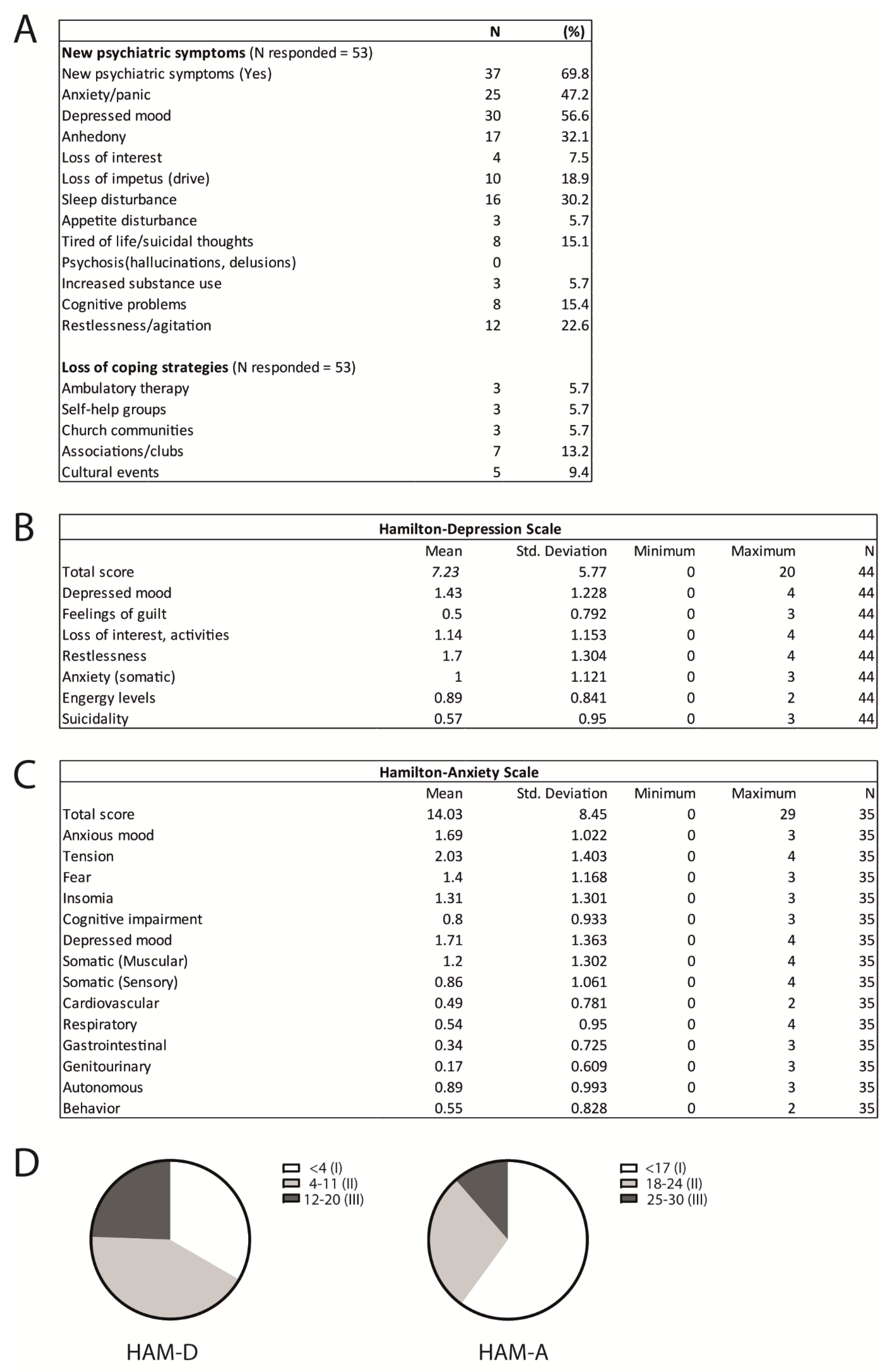
3.3. III Mental Health Status
3.3.1. Depression
3.3.2. Anxiety
3.4. IV Associations between Demographics Variables, Social Changes, and Mental Health Status during the Pandemic
3.5. V Help Provided
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected with SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574–1581. [Google Scholar] [CrossRef] [PubMed]
- Jordan, R.E.; Adab, P.; Cheng, K.K. Covid-19: Risk factors for severe disease and death. BMJ 2020, 368, m1198. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Yin, Y.; Hu, C.; Liu, X.; Zhang, X.; Zhou, S.; Jian, M.; Xu, H.; Prowle, J.; Hu, B.; et al. Clinical course and outcome of 107 patients infected with the novel coronavirus, SARS-CoV-2, discharged from two hospitals in Wuhan, China. Crit. Care 2020, 24, 188. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Daoust, J.-F. Elderly people and responses to COVID-19 in 27 Countries. PLoS ONE 2020, 15, e0235590. [Google Scholar] [CrossRef]
- Cole Steven, W.; Capitanio, J.P.; Chun, K.; Arevalo, J.M.G.; Ma, J.; Cacioppo, J.T. Myeloid differentiation architecture of leukocyte transcriptome dynamics in perceived social isolation. Proc. Natl. Acad. Sci. USA 2015, 112, 15142–15147. [Google Scholar] [CrossRef]
- Cole, S.W.; Hawkley, L.C.; Arevalo, J.M.; Sung, C.Y.; Rose, R.M.; Cacioppo, J.T. Social regulation of gene expression in human leukocytes. Genome Biol. 2007, 8, R189. [Google Scholar] [CrossRef]
- Santini, Z.I.; Jose, P.E.; Cornwell, E.Y.; Koyanagi, A.; Nielsen, L.; Hinrichsen, C.; Meilstrup, C.; Madsen, K.R.; Koushede, V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health 2020, 5, e62–e70. [Google Scholar] [CrossRef]
- Ngo, E.B. When Disasters and Age Collide: Reviewing Vulnerability of the Elderly. Nat. Hazards Rev. 2001, 2, 80–89. [Google Scholar] [CrossRef]
- Benke, C.; Autenrieth, L.K.; Asselmann, E.; Pané-Farré, C.A. Lockdown, quarantine measures, and social distancing: Associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. 2020, 293, 113462. [Google Scholar] [CrossRef]
- Rodríguez-Rey, R.; Garrido-Hernansaiz, H.; Collado, S. Psychological Impact and Associated Factors during the Initial Stage of the Coronavirus (COVID-19) Pandemic Among the General Population in Spain. Front. Psychol. 2020, 11, 1540. [Google Scholar] [CrossRef]
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef]
- Davies, R. Coronavirus and the Social Impacts on Great Britain Data—Office for National Statistics. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/bulletins/coronavirusandthesocialimpactsongreatbritain/3july2020 (accessed on 3 July 2020).
- Meng, H.; Xu, Y.; Dai, J.; Zhang, Y.; Liu, B.; Yang, H. Analyze the psychological impact of COVID-19 among the elderly population in China and make corresponding suggestions. Psychiatry Res. 2020, 289, 112983. [Google Scholar] [CrossRef]
- Klaiber, P.; Wen, J.H.; DeLongis, A.; Sin, N.L. The Ups and Downs of Daily Life During COVID-19: Age Differences in Affect, Stress, and Positive Events. J. Gerontol. Ser. B 2021, 76, e30–e37. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- di Santo, S.G.; Franchini, F.; Filiputti, B.; Martone, A.; Sannino, S. The Effects of COVID-19 and Quarantine Measures on the Lifestyles and Mental Health of People Over 60 at Increased Risk of Dementia. Front. Psychiatry 2020, 11, 578628. [Google Scholar] [CrossRef] [PubMed]
- Geoffroy, P.A.; Le Goanvic, V.; Sabbagh, O.; Richoux, C.; Weinstein, A.; Dufayet, G.; Lejoyeux, M. Psychological Support System for Hospital Workers during the Covid-19 Outbreak: Rapid Design and Implementation of the Covid-Psy Hotline. Front. Psychiatry 2020, 11, 511. [Google Scholar] [CrossRef]
- Soklaridis, S.; Lin, E.; Lalani, Y.; Rodak, T.; Sockalingam, S. Mental health interventions and supports during COVID-19 and other medical pandemics: A rapid systematic review of the evidence. Gen. Hosp. Psychiatry 2020, 66, 133–146. [Google Scholar] [CrossRef]
- Xiang, Y.-T.; Yang, Y.; Li, W.; Zhang, L.; Zhang, Q.; Cheung, T.; Ng, C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020, 7, 228–229. [Google Scholar] [CrossRef]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- McIntyre, R.; Kennedy, S.; Bagby, R.M.; Bakish, D. Assessing full remission. J. Psychiatry Neurosci. 2002, 27, 235–239. [Google Scholar]
- Hamilton, M. Hamilton Anxiety Rating Scale (HAM-A). J. Med. 1959, 65, 601. [Google Scholar] [CrossRef]
- Maier, W.; Buller, R.; Philipp, M.; Heuser, I. The Hamilton Anxiety Scale: Reliability, validity and sensitivity to change in anxiety and depressive disorders. J. Affect. Disord. 1988, 14, 61–68. [Google Scholar] [CrossRef]
- Shear, M.K.; Bilt, J.V.; Rucci, P.; Endicott, J.; Lydiard, B.; Otto, M.W.; Pollack, M.H.; Chandler, L.; Williams, J.; Ali, A.; et al. Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH-A). Depress. Anxiety 2001, 13, 166–178. [Google Scholar] [CrossRef]
- Bu, F.; Mak, H.W.; Fancourt, D.; Rigotti, C.; Volpert, V.; Derrode, S.; Bertoglio, J.-P.; Bienvenue, A.; Goffard, P.-O.; Eyraud-Loisel, A.; et al. Rates and predictors of uptake of formal and informal mental health support during the COVID-19 pandemic an analysis of 26740 adults in the UK in lockdown. medRxiv 2021. [Google Scholar] [CrossRef]
- Turkington, R.; Mulvenna, M.; Bond, R.; Ennis, E.; Potts, C.; Moore, C.; Hamra, L.; Morrissey, J.; Isaksen, M.; Scowcroft, E.; et al. Behavior of Callers to a Crisis Helpline Before and during the COVID-19 Pandemic: Quantitative Data Analysis. JMIR Ment. Health 2020, 7, e22984. [Google Scholar] [CrossRef] [PubMed]
- Guessoum, S.B.; Lachal, J.; Radjack, R.; Carretier, E.; Minassian, S.; Benoit, L.; Moro, M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020, 291, 113264. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef] [PubMed]
- Luchetti, M.; Lee, J.H.; Aschwanden, D.; Sesker, A.; Strickhouser, J.E.; Terracciano, A.; Sutin, A.R. The trajectory of loneliness in response to COVID-19. Am. Psychol. 2020, 75, 897–908. [Google Scholar] [CrossRef] [PubMed]
- Shapira, S.; Yeshua-Katz, D.; Cohn-Schwartz, E.; Aharonson-Daniel, L.; Sarid, O.; Clarfield, A.M. A pilot randomized controlled trial of a group intervention via Zoom to relieve loneliness and depressive symptoms among older persons during the COVID-19 outbreak. Internet Interv. 2021, 24, 100368. [Google Scholar] [CrossRef]
- Beauchet, O.; Cooper-Brown, L.; Ivensky, V.; Launay, C.P. Telemedicine for housebound older persons during the Covid-19 pandemic. Maturitas 2020, 142, 8–10. [Google Scholar] [CrossRef] [PubMed]
- Office, E.E.; Rodenstein, M.S.; Merchant, T.S.; Pendergrast, T.R.; Lindquist, L.A. Reducing Social Isolation of Seniors during COVID-19 through Medical Student Telephone Contact. J. Am. Med. Dir. Assoc. 2020, 21, 948–950. [Google Scholar] [CrossRef] [PubMed]


| N or M (SD) | (%) | |
|---|---|---|
| Comorbidities (N responded = 52) | 46 | 88.5 |
| Cardiovascular | 24 | 46.2 |
| Chronic lung disease | 14 | 26.9 |
| Diabetes | 8 | 15.4 |
| Current or previously diagnosed cancer | 12 | 23.1 |
| Neurological diseases | 10 | 19.2 |
| Number of daily medications (N responded = 48) | ||
| Less than one | 13 | 27.1 |
| More than one | 35 | 72.9 |
| Kind of daily medication (N responded = 48) | ||
| Psychiatric medication | 15 | 31.3 |
| Antihypertensive or cardiac medication | 18 | 37.5 |
| Antidiabetic medication | 6 | 12.5 |
| COPD or asthma medication | 10 | 20.8 |
| Prediagnosed with psychiatric disease (N responded = 52) | 20 | 38.5 |
| Anxiety | 4 | 7.7 |
| Depression | 17 | 32.7 |
| Psychosis | 1 | 1.9 |
| Addiction | 4 | 7.7 |
| Psychiatric treatment (N responded = 52) | ||
| Currently seeing a psychiatrist | 11 | 21.2 |
| Previously seen a psychiatrist | 5 | 9.6 |
| Never in psychiatric treatment | 33 | 67.3 |
| Previous Psychotherapy experience (N responded = 52) | ||
| No previous therapy | 35 | 67.3 |
| Consultation or less than 6 months | 7 | 13.5 |
| Psychotherapy more than 6 months | 4 | 7.7 |
| Continuous psychotherapy over years | 6 | 11.5 |
| Depression | ||||||
|---|---|---|---|---|---|---|
| Variables | N | Mean | SD | T | Cohen’s d | p |
| Living Alone | ||||||
| No | 22 | 8.41 | 5.578 | 1.371 | 0.41 | 0.178 |
| Yes | 22 | 6.05 | 5.851 | |||
| Previous diagnosis of psychiatric disease | ||||||
| No | 26 | 5.00 | 4.964 | −3.441 | 1.05 | 0.001 |
| Yes | 18 | 10.44 | 5.437 | |||
| Psychiatric medication | ||||||
| No | 26 | 5.58 | 4.933 | −3.33 | 1.08 | 0.002 |
| Yes | 15 | 11.13 | 5.475 | |||
| High frequency social contact | ||||||
| No | 32 | 7.09 | 6.061 | −0.584 | 0.20 | 0.563 |
| Yes | 11 | 8.27 | 4.798 | |||
| COVID high-risk group | ||||||
| No | 24 | 8.00 | 6.386 | 0.972 | 0.21 | 0.337 |
| Yes | 20 | 6.3 | 4.943 | |||
| r | p | |||||
| Age | −0.293 | 0.054 | ||||
| Anxiety | ||||||
| Variables | N | Mean | SD | T | p | |
| Living Alone | ||||||
| No | 17 | 17.53 | 8.84 | 2.569 | 0.87 | 0.015 |
| Yes | 18 | 10.72 | 6.755 | |||
| Previous diagnosis of psychiatric disease | ||||||
| No | 20 | 9.9 | 7.174 | −4.006 | 1.37 | >0.001 |
| Yes | 15 | 19.53 | 6.854 | |||
| Psychiatric medication | ||||||
| No | 21 | 11.43 | 7.972 | −2.97 | 1.07 | 0.006 |
| Yes | 12 | 19.67 | 7.075 | |||
| High frequency social contact | ||||||
| No | 27 | 13.07 | 8.185 | −1.236 | 0.50 | 0.225 |
| Yes | 8 | 17.25 | 9.114 | |||
| COVID high-risk group | ||||||
| No | 19 | 13.63 | 9.552 | −0.299 | 0.10 | 0.762 |
| Yes | 16 | 14.5 | 7.22 | |||
| r | p | |||||
| Age | −0.34 | 0.045 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wahl, A.-S.; Benson, G.; Hausner, L.; Schmitt, S.; Knoll, A.; Ferretti-Bondy, A.; Hefter, D.; Froelich, L. Rapid Support for Older Adults during the Initial Stages of the COVID-19 Pandemic: Results from a Geriatric Psychiatry Helpline. Geriatrics 2021, 6, 30. https://doi.org/10.3390/geriatrics6010030
Wahl A-S, Benson G, Hausner L, Schmitt S, Knoll A, Ferretti-Bondy A, Hefter D, Froelich L. Rapid Support for Older Adults during the Initial Stages of the COVID-19 Pandemic: Results from a Geriatric Psychiatry Helpline. Geriatrics. 2021; 6(1):30. https://doi.org/10.3390/geriatrics6010030
Chicago/Turabian StyleWahl, Anna-Sophia, Gloria Benson, Lucrezia Hausner, Sandra Schmitt, Annika Knoll, Adriana Ferretti-Bondy, Dimitri Hefter, and Lutz Froelich. 2021. "Rapid Support for Older Adults during the Initial Stages of the COVID-19 Pandemic: Results from a Geriatric Psychiatry Helpline" Geriatrics 6, no. 1: 30. https://doi.org/10.3390/geriatrics6010030
APA StyleWahl, A.-S., Benson, G., Hausner, L., Schmitt, S., Knoll, A., Ferretti-Bondy, A., Hefter, D., & Froelich, L. (2021). Rapid Support for Older Adults during the Initial Stages of the COVID-19 Pandemic: Results from a Geriatric Psychiatry Helpline. Geriatrics, 6(1), 30. https://doi.org/10.3390/geriatrics6010030







