Protein Ingredient in Saliva on Oral Dryness Patients Caused by Calcium Blocker
Abstract
1. Introduction
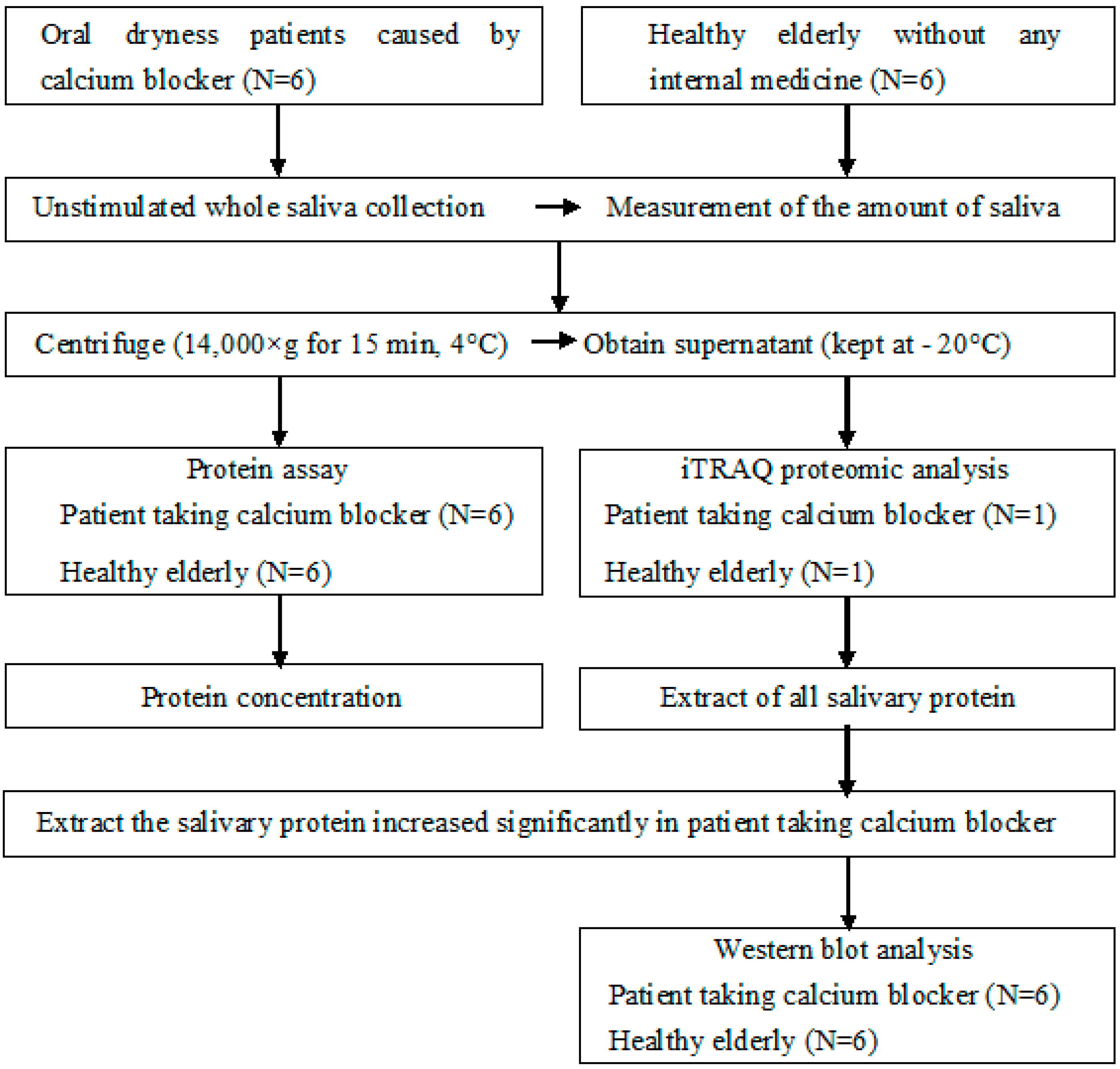
2. Materials and Methods
2.1. Subjects
2.2. Salivary Flow Rate and Protein Assay
2.3. iTRAQ (Isobaric Tag for Relative and Absolute Quantitation) Proteomic Analysis
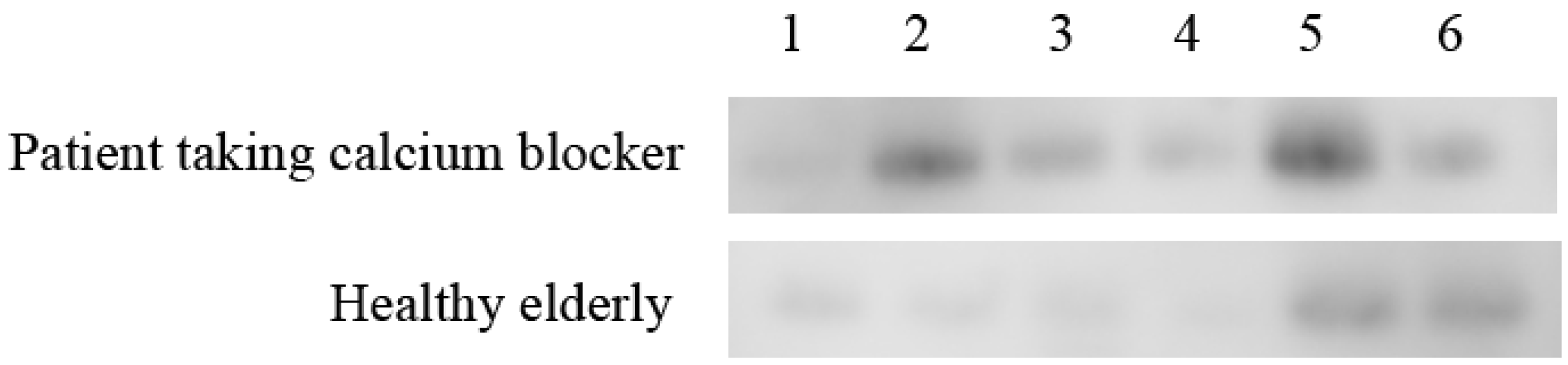
2.4. Western Blot Analysis
2.5. Statistical Analysis
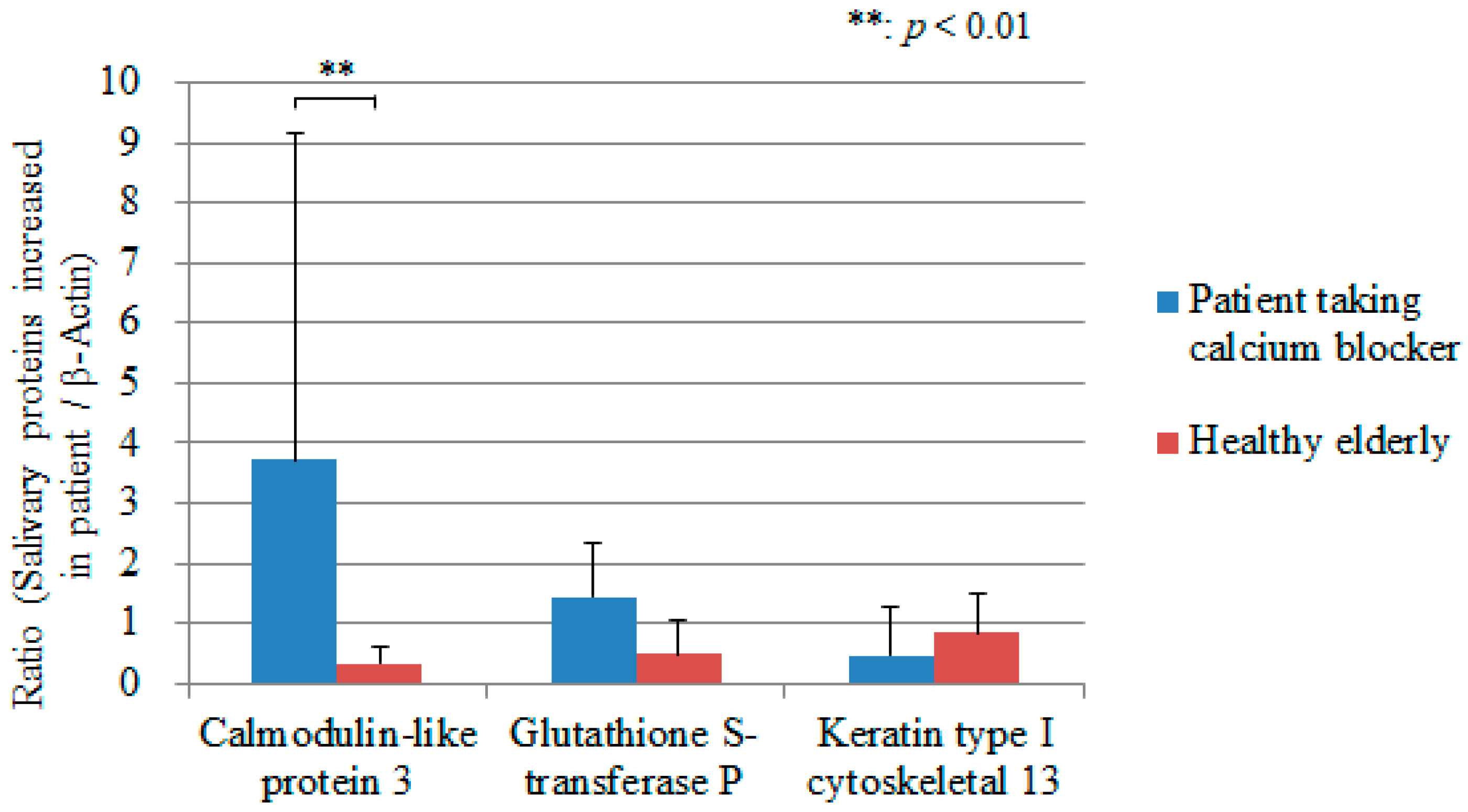
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Orellana, M.F.; Lagravère, M.O.; Boychuk, D.G.; Major, P.W.; Flores-Mir, C.; Ortho, C. Prevalence of xerostomia in population-based samples: A systematic review. J. Public. Health Dent. 2006, 5, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Tanasiewicz, M.; Hildebrandt, T.; Obersztyn, I. Xerostomia of various etiologies: A review of the literature. Adv. Clin. Exp. Med. 2016, 25, 199–206. [Google Scholar] [CrossRef] [PubMed]
- da Silva, L.; Kupek, E.; Peres, K.G. General health influences episodes of xerostomia: A prospective population-based study. Community Dent. Oral. Epidemiol. 2017, 45, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Millsop, J.W.; Wang, E.A.; Fazel, N. Etiology, evaluation, and management of xerostomia. Clin. Dermatol. 2017, 35, 468–476. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.F.; Kim, Y.; Yoo, T.; Han, P.; Inman, J.C. Burning mouth syndrome: A systematic review of treatments. Oral Dis. 2018, 24, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Fleming, M.; Craigs, C.L.; Bennett, M.I. Palliative care assessment of dry mouth: What matters most to patients with advanced disease? Support. Care Cancer 2020, 28, 1121–1129. [Google Scholar] [CrossRef] [PubMed]
- Sreebny, L.M.; Schwartz, S.S. A reference guide to drugs and dry mouth, 2nd ed. Gerodontology 1997, 14, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Navazesh, M.; Christensen, C.; Brightman, V. Clinical criteria for the diagnosis of salivary gland hypofunction. J. Dent. Res. 1992, 71, 1363–1369. [Google Scholar] [CrossRef]
- Porter, S.R.; Scully, C.; Hegarty, A.M. An update of the etiology and management of xerostomia. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 97, 28–46. [Google Scholar] [CrossRef]
- Sreebny, L.M. Saliva in health and disease: An appraisal and update. Int. Dent. J. 2000, 50, 140–161. [Google Scholar] [CrossRef]
- Hattori, T.; Wang, P.L. Calcium antagonists cause dry mouth by inhibiting resting saliva secretion. Life Sci. 2007, 81, 683–690. [Google Scholar] [CrossRef] [PubMed]
- He, X.J.; Wu, X.Z.; Wellner, R.B.; Baum, B.J. Muscarinic receptor regulation of Ca2+ mobilization in a human salivary cell line. Pflugers. Arch. 1989, 413, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Salo, T.; Oikarinen, K.S.; Oikarinen, A.I. Effect of phenytoin and nifedipine on collagen gene expression in human gingival fibroblasts. J. Oral Pathol. Med. 1990, 19, 404–407. [Google Scholar] [CrossRef] [PubMed]
- Seymour, R.A.; Thomason, J.M.; Nolan, A. Oral lesions in organ transplant patients. J. Oral Pathol. Med. 1997, 26, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, M.; Wong, D.T.; Hirayama, A.; Soga, T.; Tomita, M. Capillary electrophoresis mass spectrometry-based saliva metabolomics identified oral, breast and pancreatic cancer-specific profiles. Metabolomics 2010, 6, 78–95. [Google Scholar] [CrossRef]
- Walsh, N.P.; Montague, J.C.; Callow, N.; Rowlands, A.V. Saliva flow rate, total protein concentration and osmolality as potential markers of whole body hydration status during progressive acute dehydration in humans. Arch. Oral Biol. 2004, 49, 149–154. [Google Scholar] [CrossRef]
- Bellagambi, F.G.; Lomonaco, T.; Salvo, P.; Vivaldi, F.; Hangouët, M.; Ghimenti, S.; Biagini, D.; Francesco, F.D.; Fuoco, R.; Errachid, A. Saliva sampling: Methods and devices. An overview. Trends Analyt. Chem. 2020, 124, 115781. [Google Scholar] [CrossRef]
- Lomonaco, T.; Ghimenti, S.; Biagini, D.; Bramanti, E.; Onor, M.; Bellagambi, F.G.; Fuoco, R.; Francesco, F.D. The effect of sampling procedures on the urate and lactate concentration in oral fluid. Microchem. J. 2018, 136, 255–262. [Google Scholar] [CrossRef]
- Dawes, C. Physiological factors affecting salivary flow rate, oral sugar clearance, and the sensation of dry mouth in man. J. Dent. Res. 1987, 66, 648–653. [Google Scholar] [CrossRef]
- Mizuhashi, F.; Koide, K.; Toya, S.; Nashida, T. Salivary level of antimicrobial protein chromogranin A in relation to the salivary flow rate and swallowing function. Med Res. Archives. 2016, 4, 1–13. [Google Scholar] [CrossRef]
- Djukić, L.J.; Roganović, J.; Brajović, M.D.; Bokonjić, D.; Stojić, D. The effects of anti-hypertensives and type 2 diabetes on salivary flow and total antioxidant capacity. Oral Dis. 2015, 21, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Thumbigere-Math, V.; Michalowicz, B.S.; de Jong, E.P.; Griffin, T.J.; Basi, D.L.; Hughes, P.J.; Tsai, M.L.; Swenson, K.K.; Rockwell, L.; Gopalakrishnan, R. Salivary proteomics in bisphosphonate-related osteonecrosis of the jaw. Oral Dis. 2015, 21, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Stolle, T.; Grondinger, F.; Dunkel, A.; Meng, C.; Médard, G.; Kuster, B.; Hofmann, T. Salivary proteome patterns affecting human salt taste sensitivity. J. Agric. Food Chem. 2017, 65, 9275–9286. [Google Scholar] [CrossRef]
- Ding, F.; Sun, K.; Sun, N.; Jiang, Q.; Cao, M.; Wu, Z. iTRAQ-based proteomics reveals SOD2 as a potential salivary biomarker in liver cancer. Int. J. Biol. Markers. 2019, 34, 221–231. [Google Scholar] [CrossRef] [PubMed]
- Shan, J.; Sun, Z.; Yang, J.; Xu, J.; Shi, W.; Wu, Y.; Fan, Y.; Li, H. Discovery and preclinical validation of proteomic biomarkers in saliva for early detection of oral squamous cell carcinomas. Oral Dis. 2019, 25, 97–107. [Google Scholar] [CrossRef]
- Deming, F.P.; Al-Hashimi, I.; Haghighat, N.; Hallmon, W.W.; Kerns, D.G.; Abraham, C.; Rivera-Hidalgo, F. Comparison of salivary calmodulin binding proteins in Sjögren’s syndrome and healthy individuals. J. Oral Pathol. Med. 2007, 36, 132–135. [Google Scholar] [CrossRef]
- Hjelmervik, T.O.; Jonsson, R.; Bolstad, A.I. The minor salivary gland proteome in Sjögren’s syndrome. Oral Dis. 2009, 15, 342–353. [Google Scholar] [CrossRef] [PubMed]
- Tew, M.B.; Reveille, J.D.; Arnett, F.C.; Friedman, A.W.; McNearney, T.; Fischbach, M.; Ahn, C.; Tan, F.K. Glutathione S-transferase genotypes in systemic sclerosis and their association with clinical manifestations in early disease. Genes Immun. 2001, 2, 236–238. [Google Scholar] [CrossRef]
- Morinobu, A.; Kanagawa, S.; Koshiba, M.; Sugai, S.; Kumagai, S. Association of the glutathione S-transferase M1 homozygous null genotype with susceptibility to Sjögren’s syndrome in Japanese individuals. Arthritis. Rheum. 1999, 42, 2612–2615. [Google Scholar] [CrossRef]
- Diebold, Y.; Chen, L.L.; Tepavcevic, V.; Ferdman, D.; Hodges, R.R.; Dartt, D.A. Lymphocytic infiltration and goblet cell marker alteration in the conjunctiva of the MRL/MpJ-Fas(lpr) mouse model of Sjögren’s syndrome. Exp. Eye Res. 2007, 84, 500–512. [Google Scholar] [CrossRef]
- Hillen, M.R.; Kruize, A.A.; Bikker, A.; Wenting-van Wijk, M.; Radstake, T.R.; Hack, C.E.; Lafeber, F.P.; van Roon, J.A. Decreased expression of thymic stromal lymphopoietin in salivary glands of patients with primary Sjögren’s syndrome is associated with increased disease activity. Mod. Rheumatol. 2016, 26, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Yaswen, P.; Smoll, A.; Hosoda, J.; Parry, G.; Stampfer, M.R. Protein product of a human intronless calmodulin-like gene shows tissue-specific expression and reduced abundance in transformed cells. Cell Growth Differ. 1992, 3, 335–345. [Google Scholar] [PubMed]
- Rogers, M.S.; Strehler, E.E. The tumor-sensitive calmodulin-like protein is a specific light chain of human unconventional myosin X. J. Biol. Chem. 2001, 276, 12182–12189. [Google Scholar] [CrossRef] [PubMed]

| Patient Taking Calcium Blocker | Healthy Elderly | |
|---|---|---|
| Unstimulated salivary flow rate (mL/10 min) | 0.500 ± 0.191 * | 4.108 ± 2.707 * |
| Protein concentration (μg/mL) | 4729.63 ± 1642.24 | 1503.17 ± 533.96 |
| Flow rate of protein (μg/mL) | 244.67 ± 77.46 | 577.11 ± 323.01 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mizuhashi, F.; Morita, T.; Toya, S.; Sato, R.; Watarai, Y.; Koide, K. Protein Ingredient in Saliva on Oral Dryness Patients Caused by Calcium Blocker. Geriatrics 2020, 5, 70. https://doi.org/10.3390/geriatrics5040070
Mizuhashi F, Morita T, Toya S, Sato R, Watarai Y, Koide K. Protein Ingredient in Saliva on Oral Dryness Patients Caused by Calcium Blocker. Geriatrics. 2020; 5(4):70. https://doi.org/10.3390/geriatrics5040070
Chicago/Turabian StyleMizuhashi, Fumi, Takao Morita, Shuji Toya, Ritsuko Sato, Yuko Watarai, and Kaoru Koide. 2020. "Protein Ingredient in Saliva on Oral Dryness Patients Caused by Calcium Blocker" Geriatrics 5, no. 4: 70. https://doi.org/10.3390/geriatrics5040070
APA StyleMizuhashi, F., Morita, T., Toya, S., Sato, R., Watarai, Y., & Koide, K. (2020). Protein Ingredient in Saliva on Oral Dryness Patients Caused by Calcium Blocker. Geriatrics, 5(4), 70. https://doi.org/10.3390/geriatrics5040070





